Abstract
Background
About half of first- or second-generation Australians are born overseas, and one-in-five speak English as their second language at home which often are referred to as Culturally and Linguistically Diverse (CALD) populations. These people have varied health needs and face several barriers in accessing health services. Nevertheless, there are limited studies that synthesised these challenges. This study aimed to explore issues and challenges in accessing health services among CALD populations in Australia.
Methods
We conducted a scoping review of the literature published from 1st January 1970 to 30th October 2021 in four databases: PubMed, Scopus, Embase, and the Web of Science. The search strategy was developed around CALD populations and the health services within the Australian context. We used Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines for selection and Arksey and O’Malley framework for analysis of relevant articles. A narrative synthesis of data was conducted using inductive thematic analysis approach. Identified issues and challenges were described using an adapted socioecological model.
Results
A total of 64 studies were included in the final review. Several challenges at various levels were identified to influence access to health services utilisation. Individual and family level challenges were related to interacting social and health conditions, poor health literacy, multimorbidity, diminishing healthy migrants’ effect. Community and organisational level challenges were acculturation leading to unhealthy food behaviours and lifestyles, language and communication problems, inadequate interpretation services, and poor cultural competency of providers. Finally, challenges at systems and policy levels included multiple structural disadvantages and vulnerabilities, inadequate health systems and services to address the needs of CALD populations.
Conclusions
People from CALD backgrounds have multiple interacting social factors and diseases, low access to health services, and face challenges in the multilevel health and social systems. Health systems and services need to focus on treating multimorbidity through culturally appropriate health interventions that can effectively prevent and control diseases. Existing health services can be strengthened by ensuring multilingual health resources and onsite interpreters. Addressing structural challenges needs a holistic policy intervention such as improving social determinants of health (e.g., improving living and working conditions and reducing socioeconomic disparities) of CALD populations, which requires a high level political commitment.
Similar content being viewed by others
Introduction
People who are born overseas and speak other than English are often referred to as Culturally and linguistically diverse (CALD) groups in Australia [1]. In 2016, half of the first or second-generation Australian parents were born overseas; one in five Australians did not speak English at home [2], and nearly two in five (37%) Australians aged > 65 years belonged to CALD population [3]. People from CALD backgrounds are heterogeneous groups, and include temporary migrants (e.g., international students or temporary work-skilled), refugees, and asylum seekers who usually settled through Humanitarian Support Programs (HSP), and permanent residents and citizens of migrant’s backgrounds [1, 4]. They have diverse cultures, languages, religions, social values, and migration trajectories. Among CALD populations, refugees and asylum seekers are the most vulnerable subgroups. People from CALD backgrounds can be categorised as: migrants coming through HSP from conflict-affected countries; migrants coming from Asia, Africa and Latin America; and from high-income countries [5]. Currently, migrations to Australia are the highest from the Asian continent, especially from China and India. Australia’s migration policy emphasises ‘regionalising’ migration within the country; thus, the proportion of CALD populations living in regional areas is increasing [6,7,8].
People from CALD backgrounds in Australia experience multiple social disadvantages and face challenges in health and health care needs [9]. In the early years of post-migration, CALD populations have relatively better physical health (often referred to as Healthy Migrant Effect) than their Australia-born counterparts [10]. They have low rates of all causes of mortality and potentially preventable hospitalisations [11]. However, CALD populations, especially refugees and asylum seekers, face challenges in the new settlement, including inadequate skills and communication for employment [12, 13]. People with low wealth status have a higher burden of diseases and illnesses; they must focus on managing day to day tasks such as working and living conditions rather than health care. For people from CALD backgrounds, this can be exacerbated due to inadequate job skills resulting in fewer employment opportunities [14]. In addition, they usually have sociocultural ties with their country of origin (e.g., food habits), while their growing children acculturation with the Australian lifestyle [15]. Current COVID-19 deaths in Australia revealed three-fold a higher mortality rate among CALD groups than the general population [16]. High rates of COVID-19 hospitalisation and deaths occurred among people with multiple forms of diseases [17]. The high rates of COVID-19 related deaths among these populations suggest they are particularly vulnerable [16]. This is just one example of why we need to address the disadvantages CALD populations face. Such deaths could be due to poor access to health services and severe COVID-19 cases requiring health services at hospitals.
Previous reviews on access to health services among CALD populations were focused on specific health issues of CALD populations [18,19,20,21]. However, there is a dearth of synthesised evidence of available literature on multiple dimensions of CALD populations. To address this gap in research, this study aimed to review issues and challenges in accessing health services among people from CALD backgrounds in Australia. The findings of this study could inform policy and programs for better access to health services and explore potential areas of future research on health and health services in Australia.
Methods
Context of migration and CALD populations in Australia
From World War II to 1970, there was an increase in European migrants coming to Australia as the immigration policy sought migrants from England and Europe [22]. From the mid-70s, the number of migrants from Asia began to increase and has continued over the last four decades [22]. Since the 1990s, the migration policies have become multicultural and included migrants from all regions and nationalities [23]. Currently, permanent migration in Australia occurs through two programs: Skilled Migration Program (for skilled and family migrants) and Humanitarian Program (for refugees and those in refugee-like situations) [24]. Both programs have annual quotas, and the first scheme has a controlled selection process and allows young and healthy persons to immigrate to Australia. In contrast, the later program has no such selection programs but has fixed quotas [6].
Among the top 10 migrants’ countries that came to Australia in 2020, seven were non-English speaking, and six were from South and Southeast Asia [25, 1, 26]. In 2021, the median age of overseas-born Australian was 44 years (compared to 34 years Australian borns), with the highest age of migrants from Europe (England- 58, and Italy-72 years) [25].
Since the late 1990s, there has been a growth in temporary migration and is not subject to quotas or caps by the Government, and this exclusively focuses on improving the short-term economic contribution [27]. Since 2013, there has been a three-fold increase of migrants on temporary visas for more than eight years in Australia. Temporary migrants in Australia have contributed to the national economy by working in essential sectors (e.g., health, agriculture), producing services and goods, and paying taxes and fees to universities [6]. However, welfare restrictions have contributed to temporary migrant workers’ economic and health insecurity because they have no access to income support if they lose their employment, and more vulnerable to underpayment, and are not included in the National Medicare Scheme, and COVID-19 has intensified these insecurities [28].
In 2016, 37.1% of Australia’s 295,324 frontline care workers (childcare, aged and disability and personal) were born overseas, up from 31.2% in 2011, and higher than the proportion of overseas-born workers in the total workforce (30.6%) [29]. This comprised of migrant care workers from non-English-speaking countries (28%), temporary visas (76%), from South Asia (35%) and females ( 85%) [29].
Research design and framework
This study utilised a narrative synthesis of available evidence using a scoping review framework outlined by Arksey and O’Malley [30]. This framework has been previously used in health system and services research [31]. We incorporated the following phases: i) identifying the key research questions through an iterative review/discussion, ii) identifying the initial potential studies based on the discussion, iii) searching literature in major biomedical databases; iv) collating data, synthesising, and reporting of the findings, and v) discussion among experts and utilising their feedback as a required steps in knowledge translation part of a scoping review methodology.
Search strategy and selection criteria
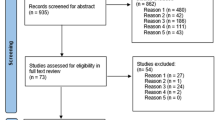
Four databases were searched: PubMed, Embase, Scopus, and the Web of Science. Search terms were identified and organised under three domains (supplementary material; Appendix 1): Health and health services and health systems; population groups; locations (Australia, states/territories). We included quantitative, qualitative, and mixed methods studies published in English from 1st January 1970 to 30th October 2021. We excluded study protocols and letters to the editors. The first author (RBK) developed the search strategy, and the second author (YA) reviewed and verified it independently. Then RBK searched records in databases, and assessed titles and abstracts of selected studies to evaluate their eligibility. Next, full-text studies were evaluated, discussed with the second author (YA). After consensus among the authors, studies were included in the final full-text review (Fig. 1). We presented this paper as a scoping review, following some components of the Preferred Reporting of Systematic Reviews and Meta-Analysis extension for Scoping Review (PRISMA-ScR) Checklist (see Supplementary material Appendix 2). The McGill Mixed Methods Appraisal Tool (MMAT) was used as a guiding framework to assess the quality of each study included in this scoping review [32]. We assessed the quality of the included studies in the context of our review's purpose, not in the context of the primary studies themselves and focused on the ability of the studies to answer our review questions.
Data extraction and synthesis
Based on scoping review framework [30], themes on health issues and challenges and access to health services among people, CALD backgrounds were identified. We analysed data using an inductive approach and generated themes [33]. We adopted a multilevel socioecological model to explain and interpret the findings [34, 35]. This model helps explain the complex interplay between individual, relationship, community, and societal factors that influence health and diseases. For this study, we framed findings at the individual/family level issues that operate at the micro-level of the system, community and organisations challenges that operate and influence at the meso-level of the systems, and policy and systems-level challenges that influence at the macro-level [36]. At the individual and family level, people from CALD backgrounds experience social disadvantages, and high exposure to diseases that lead to multiple forms of diseases and illness. At the community and organisational level, lack of cultural competency, communication difficulties, cultural differences and lack of health awareness can influence the access and provision of health services. Finally, stigma and structural disadvantages can hinder access to health services among CALD groups and are systematic challenges.
Results
Figure 1 shows the flow chart of the selected studies for this review. A total of 64 studies were included in the review.
Multilevel issues and challenges of access to health services
Figure 2 describes the major challenges of accessing health services among CALD populations in Australia. Firstly, CALD groups experience problems at the individual and family level (e.g., multiple forms of interacting diseases including NCDs, infectious diseases, malnutrition). Secondly, they experienced challenges at the community and organisational level (e.g., change in lifestyle and food habits, low level of literacy and communication problems, supply of health services). Finally, people from CALD backgrounds face systemic challenges (e.g., structural disadvantages contribute to vulnerabilities).
Individual and family level issues and challenges
Interacting social conditions and diseases
Generally, CALD populations suffer from multiple diseases and illnesses (e.g., infectious diseases, nutritional and environmental problems, and NCDs). Among them, recently arrived CALD migrants had risky sexual behaviour and shared injecting drug equipment [37], while adult people of CALD backgrounds had a high risk of multiple chronic conditions (MCCs) (e.g., obesity and smoking, anxiety, depressed mood, and poor sleep) [38]. They had an increased risk of cardiovascular diseases (CVDs) [39], and children born from the parents of Middle Eastern backgrounds had a higher prevalence of overweight (53.0%) than non-CALD children (36.7%) in Victoria [40]. Among CALD populations of older age, females, born in CALD Middle Eastern countries had increased traumatic evidence, MCCs, and poor self-rated health [41].
Issues of CALD people of African descent: Infectious diseases, maternal and child health
The CALD women of African backgrounds had complex issues and health needs. For instance, people of Sub-Saharan African backgrounds had infectious diseases (e.g., chronic hepatitis B, schistosomiasis, and strongyloidiasis), female circumcision, and micronutrient deficiency (e.g., anaemia vitamin D, iron deficiency, thrombocytopenia) [42, 43]. In addition, women born in the East African countries had poor perinatal health outcomes; for example, women born in Sudan, Eritrea, Somali and Ethiopia had elevated odds of perinatal mortality, small gestational age, low birth weight, preterm birth, and increased obstetric complications [43, 44].
People of Asian backgrounds: Infectious diseases and risk of NCDs
Asian migrants had a high prevalence of chronic hepatitis B (CHB) than their African counterparts (54.3% vs 36.7%; n = 478); they were at risk of cirrhosis unless treated and increased cost over ten years [45]. Women born in Afghanistan, Bhutan, Iraq, and Myanmar, had poor maternal health, poor pregnancy care attendance, and late booking of visits [46]. People arriving through HSPs aged 35–44 years from Asia (e.g., Iraq and Middle Eastern countries) had higher triglycerides, hypertension, and smoking than their Australian-born counterparts [47].
Diminishing healthy migrant effects over time
First-generation CALD populations have better physical health than their Australian born counterparts. However, this advantage does not apply to mental health and diminishes once migrants spend some decades in Australia [48]. After a decade of stay in Australia, native-born Australians showed a clear health advantage over CALD groups [49]. In addition, there was an association between the length of stay and health and the gross domestic product (GDP) of the birth country, and the healthy migrant effect was negatively associated with CALD groups who were from low GDP countries than those from high GDP countries [50].
Multimorbidity of refugees and asylum seekers
Broadly, refugees and asylum seekers have multiple diseases and health needs. Evidence suggested that these people experienced several health challenges such as maternal and child health (MCH) and nutritional problems, higher exposure to risk factors of MCCs, and several infectious diseases. Refugees from Syria and Afghanistan had anaemia, teenage pregnancy, and a high prevalence of vitamin and micronutrient deficiencies [38, 46]. These CALD groups had more likely to have latent infection of tuberculosis, vitamin deficiencies, parasitic infections, and hepatitis B [51]. Additionally, they usually had a high burden of mental health disorders due to difficult migration journeys and conflict in the country of origin, which varied by generation and racial and ethnic disparities. A study reported nearly half of the study participants (48.8%) had probable post-traumatic stress disorder (PTSD) among refugees resettled in regional areas [52]. Another study reported that half of Melbourne's refugees had psychiatric disorders, while 22.9% and 31.3% of participants screened positive for PTSD symptoms in the previous month and lifetime, respectively [53]. Region of birth, age, high numbers of trauma events and living difficulties post-migration predicted depression and somatic symptoms among humanitarian entrants [54]. Anxiety, depression, and somatisation were higher among recently arrived refugee women from conflict-affected countries (e.g., Iraq, Lebanon, Sudan, and Burma) [54, 55], and recently arrived refugee women experienced high levels of psychological and financial distress, intimate partner violence [54,55,56].
Community and organisational level
Acculturation leading unhealthy food habits and lifestyles
In the early years of migration, they have good physical health; over time, migrants were exposed to risk factors of several NCDs (often referred to as the Exhaust Migrant Effect) due to access to a wide variety of food (e.g., takeaway food) and increased consumption of high energy take way foods and sedentary lifestyles that resulted in weight gain and obesity [57]. A higher proportion of Middle Eastern and South Asian children had consumed nutrient-poor snacks, transformed into family diets and physical activities, and sugar-sweetened beverages as takeaway foods [15, 40]. Length of stay and age of arrival also influence the development of risk factors, such as migrants from China aged < 18 years or who lived in Australia > 30 years were more likely to have diabetes and CVD risk factors [39].
Conflicting sociocultural values of the country of origin and host country
Some people of CALD backgrounds hold strong religio-cultural values and beliefs on health and illness of the country of origin. As a result, they struggled to adapt to new culture and health behaviours once they arrived in the host country. For instance, parents were strict with their values and culture, while their children preferred to eat high energy and processed foods [15]. Asian CALD communities were unwilling to access help from mainstream services because of their beliefs. Stigma and shame were key factors of reluctance and were not aligned with Western care approaches [58, 59]. South Asian women felt 'losing control over their pregnancy' because of their preoccupied diet and exercise to control their blood glucose levels [60]. Bhutanese migrants had cultural motivations and strong faith in doctors [61]. Women of African descent perceived concerns about the gender of the service providers, lack of privacy, and cultural and religious beliefs on screening of cancers [62].
High unmet needs of health services
People of CALD backgrounds had low utilisation of health services, experienced unmet healthcare needs, and faced barriers in accessing health services [63]. Women from Afghani backgrounds experienced negative side effects of hormone-based contraception. They expressed difficulty negotiating condom use with their husbands as an alternative, leading to inconsistent contraceptive practices and unintended pregnancy [64]. The new parents arriving with young children were not formally notified of MCH services, and there were disparities in service utilisation especially paediatric specialist services [63, 65]. Additionally, CALD groups had poor access to health services for chronic diseases, including mental health disorders. A study reported only 46.9% of migrants had sought professional help to mitigate mental health problems [52]. Women of South Asian backgrounds had not met their expectations in treating gestational diabetes practices [60].
Multiple barriers and poor utilisation of health services among refugees and asylum seekers
Newly arrived refugees and asylum seekers were faced with many difficulties in accessing effective health care. Prior to migration, refugees had complex health needs and experiences, and the challenges which contributed to social, financial, and psychological stress during resettlement in the host country [66, 67]. Humanitarian entrants had inadequate access to GP services and dental, mental, and maternity care [67, 68]. Women of refugees had a decrease in the first ANC visit at less than 16 weeks' gestation, inequalities in MCH services persist, and high unmet need for child health services [63, 69]. Refugees experienced poor access to PHC services, including preventive healthcare for cervical or breast cancer screening [66, 70]. These people generally had poor health than Australia born populations and had remained limited PHC services affecting their health conditions [67, 71].
Asylum seekers had poor access to PHC services due to Medicare ineligibility, health care costs, and experienced social, financial, and psychological stress [67]. Unaccompanied and separated children, and those in detention experienced additional challenges in accessing health care [68]. In addition, refugees from Afghan, Rohingya, and Sudanese backgrounds had low risk perceptions, a lack of information on routine services (e.g., immunisation) [72], lack of knowledge of the hepatitis B virus [73].
Providers and parent’s awareness of health needs
Health care providers (HCPs) recognise sexual and reproductive health (SRH) as a complex issue among CALD backgrounds that require unique skills to deliver optimal health care [74]. There were issues of health services among children of CALD groups that included parents’ awareness of availability of PHC services, their beliefs on an understanding of children's development and choices of service providers of proximity and continuity, purpose of visit, language spoken by the provider and experience of services [75]. South Asian women with gestational diabetes felt self-management information provided was inadequate and inappropriate to their needs [60].
Low literacy on health and health care
CALD people of Chinese backgrounds had poor health literacy, especially people who migrated at an older age, recent immigrants, and those with low educational levels [76]. Thus, inadequate health literacy was identified in most first-generation Chinese immigrants who had poorer self-rated health [76, 77]. Likewise, people of African backgrounds had poor health literacy and knowledge of health and diseases [78]. In addition, studies found a lack of knowledge about cervical cancer and pap smear and had low food, and health literacy among CALD groups [62, 79, 80], and those living in regional areas experienced difficulties searching and understanding health information and seeking the right services at the right time [81, 82].
Humanitarian entrants had poor health literacy that influenced their health care seeking, including poor knowledge of quality medicine [83]. They faced challenges in navigating health services due to a lack of necessary information [18, 82]. Displaced migrants found low knowledge of STIs and HIV [37]. Lack of information and low literacy among Bhutanese refugees’ care-seeking behaviours was associated with no symptoms-no check-up [61].
Language and communication problems
CALD groups of refugee backgrounds faced language and communication problems among people of Chinese backgrounds with limited English proficiency that increased the risk of chronic heart diseases and had difficulties navigating health care systems/resources, especially older, and those with poor proficiency in English [76, 77]. Misinformation and poor availability of multilingual health materials also influenced poor utilisation of health services and health screening in regional areas among CALD groups [81, 82]. Communication difficulties further challenged self-recognition and care-seeking of mental health problems among members of separated families [52]. In addition, Vietnamese people had access barriers influencing health-seeking behaviours, including language difficulties and lack of health information in their language [77, 83]. Sometimes language barriers created culturally unresponsive interactions and challenge accessing and utilising quality PHC services [79, 80, 84]. Poor understanding of English contributed to difficulties in making phone bookings for MCH services and care for infectious diseases [65, 73].
Poor cultural competency of health care providers
Poor cultural competency of healthcare providers (HCPs) was also a barrier to delivering health services among CALD populations, especially around knowledge and engagement and care provision. HCPs discussed the impact of accessing SRH care in women's country of origin and the influence of resettlement contexts [34]. GPs and pharmacists had poor competency in understanding service users' language, which influenced access to PHC services [85]. The health care provider’s language and cultural competence influenced medicines and pharmacy services utilisation among CALD population [86]. The gestational diabetes practices could not meet consumer expectations among women of South Asian backgrounds due to insufficient culturally appropriate care [60]. Furthermore, the role of reception staff and recording of the language and interpreter's needs was well defined but lacked effective systems to share the information with clinicians [87]. Providers' lack of cultural and spiritual awareness, culturally inappropriate and inadequate information influenced to the provision of mental health services [88].
Inadequate interpreter services
Accessing PHC services was influenced by a lack of interpreter services or low utilisation. Interpreter service was available, but provision was insufficient, especially in regional areas [81, 85]. For example, a study found that 40% of refugee women giving birth in Australia required interpreter services [69], and only 48% reported using the government-funded translating and interpreting service [87]. Lack of interpreter services and poor availability of multilingual health materials further challenged getting necessary information on health, diseases, and services [81, 88]. Current interpretation policy does not allow family members and relatives as interpreters. Thus, extra time was required to arrange interpreters because of the lack of onsite interpreters. In addition, minimal interpreting support for diagnostic services and emergencies (e.g., labour and delivery) was found major barriers to accessing health services [87, 89]. Low availability of interpreter services made it difficult in negotiating GPs services, especially among humanitarian entrants and asylum seekers [67].
Systems and policy level
Poor health system responses for CALD populations
CALD populations experienced barriers to accessibility (e.g., shortage and turnover of staff, distance, travel time, time constraints), acceptability (e.g., poor access to female-specific services, lack of privacy, cultural and religious beliefs), affordability (e.g., cost of services financial costs, high cost of services) and contextual factors (e.g., poor housing and unemployment) in regional areas [62, 65, 81, 83, 85]. They had poor knowledge and understanding of the health system [34, 53, 90, 91]. Current healthcare provisions were culturally inappropriate to African mental health patients, not considering the pre-existing cultural knowledge resulting in disempowerment and loss of autonomy [18, 88]. The health system lacked culturally appropriate service provision and recognition of sociocultural and religious during services delivery [78]. In the post-migration settlement phase, childhood obesity prevention program was influenced by targeted junk food advertising to children, and the lack of mandatory weight checks in schools [79].
Systematic challenges of humanitarian entrants and asylum seekers
There were several systemic challenges for humanitarian entrants and asylum seekers. For example, newly arrived refugees had had difficulty negotiating services and faced complexities in the new system and resettlement [67, 68]. In addition, studies reported that humanitarian entrants from Afghan, Rohingya, and South Sudanese backgrounds perceived challenges in the treatment of hepatitis B that included previous experiences, time constraints, divergent views about treatment decisions and perceived inadequate clinical support [73, 92].
Refugees with mental health had dual vulnerabilities: the stigmatisation associated with mental illnesses and the access and utilisation of services [58]. They faced social disadvantages such as financial hardships, unstable housing, discrimination, social exclusion, stigma from providers, and logistical difficulties that influenced their existing problems [41, 90, 93]. Refugees had a high prevalence of mental health issues in the initial years of settlement. They had health systems challenges in accessing mental health (e.g., fear of family members, being judged by treatment providers, fear of hospitalisation) [41, 90, 93]. Some refugees had a strong faith in health service providers, especially doctors; however, the health system lacked opportunistic screening for cancers during routine visits [61]. Nonetheless, they faced challenges from HCPs a lack of training knowledge resources and targeted services to address sexual and relationship issues [34, 71], and had poor accessibility to GPs services [66].
Inadequate inclusion of migrants and refugees’ health in regional organisations
Needs assessment documents of Medicare Locals (MLs) and Primary Health Networks (PHNs) identified that the health of CLAD populations included 46% of MLs and 74% of PHNs. But 48% of MLs and 55% of PHNs did not report any activities on migrant health, while 78% and 62% did not report any activities for refugees [94]. Factors associated with little attention for refugees and migrants’ health in MLs and PHNs included lack of local priority areas, funding, collaboration with the organisations working with CALD communities [94]. Moreover, current systems collect limited information about CALD groups (e.g., maternal country of birth, year of arrival in Australia, a requirement for an interpreter, and women’s preferred language) [95].
Multiple structural disadvantages and vulnerabilities
People from CALD backgrounds experienced several challenges at the micro-level from both supply and demand sides of the systems. However, these were the systemic challenges that influenced services delivery and utilisation. Their perceived challenges included stigma, embarrassment, fear, racism and discriminatory practices, poor knowledge and understanding of the health system, and difficulties in navigating the systems [53, 62, 78, 90, 91]. Those CALD groups with mental health issues experienced more vulnerabilities, including low self-esteem, lack of friends and relatives, poor understating of the health care systems [78, 84], shame and stigma, and lack of collaboration in health care [59]. Additionally, HIV related stigma and discrimination influenced non-disclosure, reduced social support, delayed testing and service access, and impacted treatment adherence [96]. Furthermore, they experienced embarrassment and difficulties adapting to a new cultural context [62, 81]. In addition, people from CALD groups faced financial stress, low socioeconomic status, poor housing, and unemployment, especially in regional areas [78, 81, 83]. Still, some migrants lacked social security services, including the Medicare scheme [88]. Moreover, high cost of care, long waiting time in case of MCCs, and the dissonance between providers and CALD services users in preference of alternative intentions [84, 91].
Discussion
This review identified several challenges in accessing and utilising health services among CALD populations in Australia. These vulnerable groups face challenges in access to health services at individual and family level (e.g., interacting social conditions and diseases, infectious diseases, NCDs, and multimorbidity). At the community and organisational level, challenges include acculturation leading to an unhealthy lifestyle and food habits, diminishing healthy migrant effect, high unmet needs of health services, poor access to health services among humanitarian entrants, poor health literacy on health and health needs, language, and communication problems, and inadequate or low utilisation of interpreter services. Finally, system and policy level challenges include multiple structural disadvantages and vulnerabilities and inadequate inclusions of migrants’ health in regional public health organisations. Several strategies could be adopted to address these challenges at the multiple levels of the systems.
Individual/family level strategies
Implementing tailored and context-specific program approaches and interventions can address issues and challenges at the individual level. People of CALD backgrounds have a higher risk of diseases and experience interacting adverse social conditions and multimorbidity. Targeted behaviour changes approaches can reduce potential risk factors of NCDs. Potential strategies include promoting a low-calorie diet and physical activity. Treatment of multimorbidity needs comprehensive assessment and treatment mechanisms than episodic treatment of disease. For instance, if any ill persons of CALD backgrounds visit GPs to treat common illnesses, GPs need to assess other associated disease conditions and illnesses and advise care seekers of any potential risk factors [97]. Previous background of individuals and country of origin is important as individuals’ belief and perceptions can affect the uptake of behaviour and daily practices [98]. Health and diseases conditions of CALD groups depend on their migration journey and their social-cultural backgrounds. Thus, individual program interventions need to focus on factors contributing to individuals’ social conditions and the progression of diseases. The aggravating causes of multiple diseases among CALD populations are interaction of diseases and social conditions [99]. Therefore, prevention and management of diseases among CALD groups need to have a holistic lens of social determinants of health.
Community and organisational level strategies
Addressing individual/family level challenges also depend on community and organisational level strategies from both supply and demand perspectives. For instance, post-migration CALD populations generally suffer from many NCDs because of unhealthy food behaviours and sedentary lifestyles. Community factors, such as bicultural playgroups, ethnic community groups, and school-based healthy lunch box initiatives, can improve the reduction of childhood obesity, health literacy, and health promotion for NCDs [79]. Patients’ social networks and supports, religious beliefs and individual resilience were coping strategies, while common ethnic social support was positively associated with improved health problems [41, 92]. Family factors and social networks were positively influenced information-acquisition, health-seeking, and preventive behaviours [52].
Furthermore, improving health literacy and awareness of health, diseases, and needs are essential for behaviour changes. Studies reported that functional health literacy of younger-educated women improved care-seeking due to changing awareness [61] and creating a supportive health care environment (culturally responsive care, using trained interpreters) [80]. CALD parents had diverse experiences with service providers influenced by their awareness of available services during their stay in Australia [75]. Phone ownership indicated mHealth solutions acceptable to improve healthcare access, literacy, and autonomy among refugees in Melbourne [70]. Therefore, improving health literacy is vital for accessing health services among CALD populations.
Additionally, adequate, and timely language interpreter services could address language and communication barriers. Health education and communication resources materials need to be developed in participants' (service users') languages. A study reported that the implementation of reminder systems facilitated the uptake of health services and a range of GP practices [72]. The use of family members and relatives effectively interpreted GPs’ prescriptions [87], but they cannot act as interpreters. The feasibility study on the use of family members and friends as interpreters can ensure the provision of timely and uninterrupted interpretation services. Engaging bicultural workers and onsite interpreting services can improve trust and explain refugees' experiences [18, 71] and educate women on maternity care [43]. Community engagement can play a vital role in sharing of information. Studies reported that community organisations played a pivotal for disseminating culturally meaningful information on immunisation [72], and engaged refugee women in health screening programs and services [82].
Not only demand-side community factors, but provision of supply of health services also can improve the utilisation of health services. For instance, timely referral, awareness of risk factors, and appointment reminders can improve access to health services. Previous studies revealed that pre-arranged group appointments by MCH nurses increased engagement and participation with the health system and provided culturally appropriate services among newly arrived migrants [65, 100]. A study reported practice nurses’ supportive roles offer practical strategies for improving community knowledge about safe medicines [101]. Opportunistic screening (e.g., screening of breast and cervical cancers) in GPs clinics and advice about follow-up were found effective to identify multimorbidity [100]. Professional training and development of providers and the ability to recognise the role of medicine (e.g., mental health) enhanced health care-seeking and cultural responsiveness [43, 56].
Moreover, providers of similar backgrounds to service users can identify cultural variations and recognising such cultural differences is important for effective service provision that can address stigma and discrimination [78]. Such as recruiting health workers from CALD communities to adequately elicit and address patients' needs [91]. Furthermore, continuity of care nurses and interpreters from cross cultural groups were preferred for increasing client-provider trust and ongoing engagement in aged care facilities [65, 102]. Integrating CALD staff into the workforce can assist new migrants in transitioning into the wider Australian society and enriching the care of older persons [102]. The perception of gender roles and the involvement of male partners were integral to SRH decision-making and women-centred care [34]. Thus, the provision of culturally competent providers and cross-cultural health force is vital for delivering health services among CALD populations.
From both the demand and supply side of community and organisation level, humanitarian entrants and asylum seekers had multiple health problems and needs and poor access to health services, which suggests the need for targeted program interventions. Possible approaches could be providing friendly services during the first consultation visit, friendly staff, and connection with the refugees’ communities with similar social and ethnic backgrounds. Evidence revealed that these approaches were found effective for clinical assessments and prescriptions among Afghan refugees in Melbourne [68] and addressed their needs for family planning services [64]. Health providers need training on refugee health that could improve access to and quality use of medicines [101], and be able to provide services for women’s health (e.g., sexual and reproductive health) [74]. Refugee families established early connections with the community and religious groups with cultural, social their ethnic backgrounds [103]. The recruitment of cross cultural health workers is crucial to delivering services to this vulnerable subsection of CALD groups. Such health providers can provide culturally responsive care and improve the healthcare experience by providing people-centred care [34], and can build trust among users and providers [77]. Furthermore, the collection of basic information can help to address the health needs of humanitarian migrants and asylum seekers [95].
System and policy level strategies
Macro-level strategies can address policy and systems-level challenges; however, they require political commitment and leadership. Structural interventions can influence the operationalisation of macro-policies at the organisational/ institutional level and implementation targeting the individual level. To address the policy and system level, a range of interventions can be adopted. For instance, the inclusion of CALD issues in the pre-service training or academic curriculum can be important for future HCPs for delivery of culturally appropriate services. Organisational ethics and values influence the human resource diversity management strategies and impact the quality of care provided to residents [102]. The current information system lacks important longitudinal health data of CALD population groups post migration in Australia. Ongoing monitoring of quality improvement initiatives needs such data on CALD groups to identify the vulnerable section of CALD groups and their health needs [69]. The inclusion of migrants' and refugees' health in PHNs and MLs is important for implementing public health programs.
Additionally, increasing the scope of the Medicare program can reduce the financial barriers of temporary migrants in accessing health services in Australia [28]. Low hostility towards migrants and refugees is a constant cultural force that can reduce such structural discrimination [102]. Rural resettlement of migrants was a mixture of settlement experiences and opportunity for integration, a sense of safety, and social connectedness [104]. Thus, integrated settlement can address the social discrimination and societal harmony of multicultural communities.
Implications for policy and research
This review has identified some program and research implications for CALD populations. Firstly, CALD populations often experience disadvantages and vulnerabilities leading to MCCs. Thus, health system efforts require addressing MCCs and their interacting social conditions. Secondly, there is a need to strengthen existing interpretation services by providing onsite timely interpreter services. Providers of the same ethnic backgrounds and multilingual education materials can improve access to health services. Thirdly, to address structural vulnerabilities, there is a need of policy interventions that can address systemic challenges. This research has identified some research agendas. Firstly, there are waves of migrations from different subcontinents and travel using different routes, have multimorbidity and health needs, health care experience and service utilisation and interacting social and diseases conditions. Exploring the status of multimorbidity and its social and cultural aspects is necessary, including the process of acculturation and behaviour changes. Secondly, there are interpretation services to address the language and communication barrier, but the use of these services is inadequate. Thus, family members and relatives can provide interpretation services timely and fill the need of inadequacy of interpretation services; this can be one of the research agendas to explore its feasibility and address language and communication barriers among CALD groups.
Thirdly, a significant proportion of CALD populations work in health care sectors, including aged, disability, and community care. However, access to health services among these care providers is inadequately explored; therefore, future research can address these research gaps. Fourthly, there are several cohorts of migrants settled in Australia. Longitudinal studies are required that can examine health problems which emerge in different cohorts across their lifecycle since arrival in Australia. Such a study can explore the health and diseases of CALD populations. Finally, CALD populations can face challenges in accessing health care at multiple stages, such as at the stage of seeking care and reaching care and receiving care at facilities. Therefore, further research is necessary that can explore delaying care at different stages and potential strategies to mitigate those delays for improved health services utilisation.
Strengths and limitations
This study systematically reviewed the available evidence on access to health services among CALD groups. The evidence was thematically synthesised and presented in a multilevel socioecological framework. The findings of this study could provide research, policy, and program insights to deliver the health services for the improved health status of CALD populations. Addressing access barriers is important to realise universal health coverage and achieve SDG3. Nonetheless, health services utilisation and delivery issues are complex and depend on health systems and social contexts. Therefore, findings from this study could signal which factors to consider and what levels of the system are vital for system performance. Identifying challenges could be the beginning steps toward further research agendas for access to health services for CALD groups in Australia. The CALD populations are heterogenous groups, and thematic synthesis provides important perspectives on issues and challenges in multilevel health systems in line with the research question; however, such analysis can miss the details of the individual study findings and issues of specific subsections of diverse groups.
Conclusions
Despite the Australia’s national universal health care program (Medicare), some populations, such as people from CALD backgrounds, have poor access to quality health services. They experienced multiple challenges that could operate in multilevel health systems and had poor access to health services. Health services providers need to incorporate the care, prevention, and treatment mechanisms. Moreover, program approaches need to focus on preventing the risk behaviours of NCDs, and modification of lifestyle and unhealthy food behaviours. Program and policy efforts need to focus on vulnerable groups such as refugees and asylum seekers. Language and communication problems can be improved by strengthening existing interpretation services and ensuring multilingual information and communication materials. Recruiting health care providers of similar ethnic backgrounds can provide culturally appropriate care for a disadvantaged segment of CALD populations. High-level policy interventions can address the structural challenges, such as the provision of Medicare for CALD populations (e.g., temporary migrants) and the inclusion of migrants’ health in regional health organisations. Addressing structural challenges needs a holistic policy intervention such as improving social determinants of health (e.g., improving living and working conditions, improving socioeconomic status, reducing racial discrimination) of CALD populations, which requires a high level political commitment.
Availability of data and materials
All relevant data are available within the paper and its supplementary material file.
References
Pham TTL, Berecki-Gisolf J, Clapperton A, O’Brien KS, Liu S, Gibson K. Definitions of Culturally and Linguistically Diverse (CALD): a literature review of epidemiological research in Australia. Int J Environ Res Public Health. 2021;18(2):737.
Shepherd SM, Masuka G. Working with at-risk culturally and linguistically diverse young people in Australia: risk factors, programming, and service delivery. Crim Justice Policy Rev. 2021;32(5):469–83.
Khadka J, Lang C, Ratcliffe J, Corlis M, Wesselingh S, Whitehead C, Inacio M. Trends in the utilisation of aged care services in Australia, 2008–2016. BMC Geriatr. 2019;19(1):1–9.
Renzaho A, Polonsky M, Mellor D, Cyril S. Addressing migration-related social and health inequalities in Australia: call for research funding priorities to recognise the needs of migrant populations. Aust Health Rev. 2015;40(1):3–10.
Wilson T, McDonald P, Temple J, Brijnath B, Utomo A. Past and projected growth of Australia’s older migrant populations. Genus. 2020;76(1):20.
Boese M, Moran A. The regional migration-development nexus in Australia: what migration? Whose development? Front Sociol. 2021;6:9.
Hawkes C, Norris K, Joyce J, Paton D. resettlement stressors for women of refugee background resettled in regional Australia. Int J Environ Res Public Health. 2021;18(8):3942.
Forbes-Mewett H, Hegarty K, Wickes R. Regional migration and the local multicultural imaginary: the uneasy governance of cultural difference in regional Australia. J Ethn Migr Stud. 2021;6:1–18.
Georgeou N, Schismenos S, Wali N, Mackay K, Moraitakis E. A scoping review of ageing experiences among culturally and linguistically diverse people in Australia: towards better ageing policy and cultural well-being for migrant and refugee adults. Gerontologist. 2021;191:1–18.
Anikeeva O, Bi P, Hiller JE, Ryan P, Roder D, Han G-S. The health status of migrants in Australia: a review. Asia Pac J Public Health. 2010;22(2):159–93.
Australian Institute of Health and Welfare 2018. Australia’s health 2018. Australia’s health series no. 16. AUS 221. Canberra: AIHW.
Kavian F, Mehta K, Willis E, Mwanri L, Ward P, Booth S. Migration, stress and the challenges of accessing food: an exploratory study of the experience of recent Afghan women refugees in Adelaide, Australia. Int J Environ Res Public Health. 2020;17(4):1379.
Udah H, Singh P, Chamberlain S. Settlement and employment outcomes of black African immigrants in Southeast Queensland Australia. Asian Pac Migr J. 2019;28(1):53–74.
Montayre J, Montayre J, Thaggard S. Culturally and linguistically diverse older adults and mainstream long-term care facilities: integrative review of views and experiences. Res Gerontol Nurs. 2018;11(5):265–76.
Zulfiqar T, Strazdins L, Banwell C. How to Fit In? Acculturation and Risk of Overweight and Obesity. Experiences of Australian Immigrant Mothers From South Asia and Their 8- to 11-Year-Old Children. SAGE Open. 2021;11(3):21582440211031800.
ABS. COVID-19 Mortality in Australia. 2022.
Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, Hosein Z, Padda I, Mangat J, Altaf M. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020;2(8):1069–76.
Au M, Anandakumar AD, Preston R, Ray RA, Davis M. A model explaining refugee experiences of the Australian healthcare system: a systematic review of refugee perceptions. BMC Int Health Hum Rights. 2019;19(1):22.
Chen JR, Cross WM, Plummer V, Lam L, Tang SY. A systematic review of prevalence and risk factors of postpartum depression in Chinese immigrant women. Women Birth. 2019;32(6):487–92.
Alam Z, Shafiee Hanjani L, Dean J, Janda M. Cervical cancer screening among immigrant women residing in Australia: a systematic review. Asia Pac J Public Health. 2021;33(8):816–27.
Joshi C, Russell G, Cheng IH, Kay M, Pottie K, Alston M, Smith M, Chan B, Vasi S, Lo W, et al. A narrative synthesis of the impact of primary health care delivery models for refugees in resettlement countries on access, quality and coordination. Int J Equity Health. 2013;12:88.
Australian Institute of Health and Welfare: Culturally and linguistically diverse populations. In: Australia’s health series no 16 AUS 221 Canberra: AIHW; 2018.
1990 and Beyond | Australia's migration history timeline | NSW Migration Heritage Centre [https://www.migrationheritage.nsw.gov.au/exhibition/objectsthroughtime-history/1990-and-beyond/index.html]
Davis RM. The ‘bad’ and exceptionally ‘good’: constructing the African refugee. Media Int Aust. 2020;179(1):113–26.
Migration, Australia [https://www.abs.gov.au/statistics/people/population/migration-australia/latest-release]
Microdata: Personal Income of Migrants, Australia [https://www.abs.gov.au/statistics/microdata-tablebuilder/available-microdata-tablebuilder/personal-income-migrants-australia]
Phillips J, Simon-Davies o: Migration to Australia: a quick guide to the statistics. In: RESEARCH PAPER SERIES, 2016–17. 2017.
Clibborn S, Wright CF. COVID-19 and the policy-induced vulnerabilities of temporary migrant workers in Australia. J Aust Political Econ. 2020;85:62–70.
Christine Eastman, Charlesworth S, Hill E: Migrant Workers in Frontline Care. In: FACT SHEET 1. 2016.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Adhikari B, Mishra SR, Schwarz R. Transforming Nepal’s primary health care delivery system in global health era: addressing historical and current implementation challenges. Global Health. 2022;18(1):8.
Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Mengesha ZB, Perz J, Dune T, Ussher J. Refugee and migrant women’s engagement with sexual and reproductive health care in Australia: a socio-ecological analysis of health care professional perspectives. PLoS One. 2017;12(7):e0181421.
White K, Ocampo M, Scarinci IC. A socio-ecological approach for examining factors related to contraceptive use among recent Latina immigrants in an emerging Latino state. Women Health. 2017;57(7):872–89.
Smith T, McNeil K, Mitchell R, Boyle B, Ries N. A study of macro-, meso- and micro-barriers and enablers affecting extended scopes of practice: the case of rural nurse practitioners in Australia. BMC Nurs. 2019;18:14–14.
Dean J, Mitchell M, Stewart D, Debattista J. Sexual health knowledge and behaviour of young Sudanese Queenslanders: a cross-sectional study. Sex Health. 2017;14(3):254–60.
Maldari T, Elsley N, Rahim RA. The health status of newly arrived Syrian refugees at the Refugee Health Service, South Australia, 2016. Aust J Gen Pract. 2019;48(7):480–6.
Jin K, Gullick J, Neubeck L, Koo F, Ding D. Acculturation is associated with higher prevalence of cardiovascular disease risk-factors among Chinese immigrants in Australia: evidence from a large population-based cohort. Eur J Prev Cardiol. 2017;24(18):2000–8.
Scott B, Bolton KA, Strugnell C, Allender S, Marks J. Weight status and obesity-related dietary behaviours among culturally and linguistically diverse (CALD) children in Victoria, Australia. BMC Pediatr. 2019;19(1):511.
Cooper S, Enticott JC, Shawyer F, Meadows G. Determinants of mental illness among humanitarian migrants: longitudinal analysis of findings from the first three waves of a large cohort study. Front Psychiatry. 2019;10:545.
Gibney KB, Mihrshahi S, Torresi J, Marshall C, Leder K, Biggs BA. The profile of health problems in African immigrants attending an infectious disease unit in Melbourne. Australia Am J Trop Med Hyg. 2009;80(5):805–11.
Correa-Velez I, Ryan J. Developing a best practice model of refugee maternity care. Women Birth. 2012;25(1):13–22.
Belihu FB, Davey MA, Small R. Perinatal health outcomes of East African immigrant populations in Victoria, Australia: a population based study. BMC Pregnancy Childbirth. 2016;16:86.
Subramaniam K, Flexman J, Tarquinio L, Thambiran A, Hopkins S, Cheng W. Hepatitis B status in migrants and refugees: increasing health burden in Western Australia. Intern Med J. 2012;42(8):880–6.
Gibson-Helm M, Boyle J, Cheng IH, East C, Knight M, Teede H. Maternal health and pregnancy outcomes among women of refugee background from Asian countries. Int J Gynaecol Obstet. 2015;129(2):146–51.
Chandra M, Duri A, Smith M. Prevalence of chronic disease risk factors in 35- to 44-year-old humanitarian arrivals to New South Wales (NSW). Australia Aust J Prim Health. 2019;25(1):19–23.
Biddle N, Kennedy S, McDonald JT. Health assimilation patterns amongst Australian Immigrants. Economic Record. 2007;83(260):16–30.
Lee R. Does the healthy immigrant effect apply to mental health? Examining the effects of immigrant generation and racial and ethnic background among Australian adults. SSM Popul Health. 2019;7:011–011.
Song H, Booth JM, Kim BJ. Decomposing the Healthy Immigrant Effect: The Role of GDP of Birth Country in Immigrant Health. J Immigr Minor Health. 2021;17:1–7.
Masters PJ, Lanfranco PJ, Sneath E, Wade AJ, Huffam S, Pollard J, Standish J, McCloskey K, Athan E, O’Brien DP, et al. Health issues of refugees attending an infectious disease refugee health clinic in a regional Australian hospital. Aust J Gen Pract. 2018;47(5):305–10.
Hamrah MS, Hoang H, Mond J, Pahlavanzade B, Charkazi A, Auckland S. The prevalence and correlates of symptoms of post-traumatic stress disorder (PTSD) among resettled Afghan refugees in a regional area of Australia. J Ment Health. 2020;30(3):1–7.
Shawyer F, Enticott JC, Block AA, Cheng IH, Meadows GN. The mental health status of refugees and asylum seekers attending a refugee health clinic including comparisons with a matched sample of Australian-born residents. BMC Psychiatry. 2017;17(1):76.
Schweitzer RD, Vromans L, Brough M, Asic-Kobe M, Correa-Velez I, Murray K, Lenette C. Recently resettled refugee women-at-risk in Australia evidence high levels of psychiatric symptoms: individual, trauma and post-migration factors predict outcomes. BMC Med. 2018;16(1):149.
Rees SJ, Fisher JR, Steel Z, Mohsin M, Nadar N, Moussa B, Hassoun F, Yousif M, Krishna Y, Khalil B, et al. Prevalence and risk factors of major depressive disorder among women at public antenatal clinics from refugee, conflict-affected, and Australian-born backgrounds. JAMA Netw Open. 2019;2(5):e193442.
Slewa-Younan S, Guajardo MGU, Yaser A, Mond J, Smith M, Milosevic D, Smith C, Lujic S, Jorm AF. Causes of and risk factors for posttraumatic stress disorder: the beliefs of Iraqi and Afghan refugees resettled in Australia. Int J Ment Health Syst. 2017;11(1):1–14.
Babatunde-Sowole OO, Power T, Davidson P, Ballard C, Jackson D. Exploring the diet and lifestyle changes contributing to weight gain among Australian West African women following migration: a qualitative study. Contemp Nurse. 2018;54(2):150–9.
Cross W, Singh C. Dual vulnerabilities: mental illness in a culturally and linguistically diverse society. Contemp Nurse. 2012;42(2):156–66.
Wynaden D, Chapman R, Orb A, McGowan S, Zeeman Z, Yeak S. Factors that influence Asian communities’ access to mental health care. Int J Ment Health Nurs. 2005;14(2):88–95.
Bandyopadhyay M. Gestational diabetes mellitus: a qualitative study of lived experiences of South Asian immigrant women and perspectives of their health care providers in Melbourne, Australia. BMC Pregnancy Childbirth. 2021;21(1):500.
Parajuli J, Horey D, Avgoulas MI. Perceived barriers to cervical cancer screening among refugee women after resettlement: a qualitative study. Contemp Nurse. 2020;56(4):363–75.
Anaman-Torgbor JA, King J, Correa-Velez I. Barriers and facilitators of cervical cancer screening practices among African immigrant women living in Brisbane Australia. Eur J Oncol Nurs. 2017;31:22–9.
Guo SJ, Liu MJ, Chong SY, Zendarski N, Molloy C, Quach J, Perlen S, Nguyen MT, O’Connor E, Riggs E, et al. Health service utilisation and unmet healthcare needs of Australian children from immigrant families: a population-based cohort study. Health Soc Care Community. 2020;28(6):2331–42.
Russo A, Lewis B, Ali R, Abed A, Russell G, Luchters S. Family planning and Afghan refugee women and men living in Melbourne, Australia: new opportunities and transcultural tensions. Cult Health Sex. 2020;22(8):937–53.
Riggs E, Davis E, Gibbs L, Block K, Szwarc J, Casey S, Duell-Piening P, Waters E. Accessing maternal and child health services in Melbourne, Australia: reflections from refugee families and service providers. BMC Health Serv Res. 2012;12:117.
Manchikanti P, Cheng IH, Advocat J, Russell G. Acceptability of general practice services for Afghan refugees in south-eastern Melbourne. Aust J Prim Health. 2017;23(1):87–91.
Spike EA, Smith MM, Harris MF. Access to primary health care services by community-based asylum seekers. Med J Aust. 2011;195(4):188–91.
Davidson N, Skull S, Burgner D, Kelly P, Raman S, Silove D, Steel Z, Vora R, Smith M. An issue of access: delivering equitable health care for newly arrived refugee children in Australia. J Paediatr Child Health. 2004;40(9–10):569–75.
Yelland J, Mensah F, Riggs E, McDonald E, Szwarc J, Dawson W, Vanpraag D, Casey S, East C, Biro MA, et al. Evaluation of systems reform in public hospitals, Victoria, Australia, to improve access to antenatal care for women of refugee background: an interrupted time series design. PLoS Med. 2020;17(7):e1003089.
Bartlett R, Robinson T, Anand J, Negussie F, Simons Smith J, Boyle JA. Empathy and journey mapping the healthcare experience: a community-based participatory approach to exploring women's access to primary health services within Melbourne's Arabic-speaking refugee communities. Ethn Health. 2020;27(3):1–17.
McBride J, Block A, Russo A. An integrated healthcare service for asylum seekers and refugees in the South-Eastern Region of Melbourne: Monash Health Refugee Health and Wellbeing. Aust J Prim Health. 2017;23(4):323–8.
Abdi I, Menzies R, Seale H. Barriers and facilitators of immunisation in refugees and migrants in Australia: an east-African case study. Vaccine. 2019;37(44):6724–9.
Sievert K, O’Neill P, Koh Y, Lee JH, Dev A, Le S. Barriers to accessing testing and treatment for chronic hepatitis B in Afghan, Rohingyan, and South Sudanese populations in Australia. J Immigr Minor Health. 2018;20(1):140–6.
Mengesha ZB, Perz J, Dune T, Ussher J. Preparedness of health care professionals for delivering sexual and reproductive health care to refugee and migrant women: a mixed methods study. Int J Environ Res Public Health. 2018;15(1):174.
Garg P, Ha MT, Eastwood J, Harvey S, Woolfenden S, Murphy E, Dissanayake C, Jalaludin B, Williams K, McKenzie A, et al. Explaining culturally and linguistically diverse (CALD) parents’ access of healthcare services for developmental surveillance and anticipatory guidance: qualitative findings from the “Watch Me Grow” study. BMC Health Serv Res. 2017;17(1):228.
Zhang L, Ding D, Neubeck L, Gallagher R. Health literacy as a predictor of emergency department visits and self-rated health among Chinese immigrants: findings from an Australian survey. Patient Educ Couns. 2020;103(11):2353–60.
Jin K, Neubeck L, Koo F, Ding D, Gullick J. Understanding prevention and management of coronary heart disease among Chinese immigrants and their family carers: a socioecological approach. J Transcult Nurs. 2020;31(3):257–66.
Fauk NK, Ziersch A, Gesesew H, Ward P, Green E, Oudih E, Tahir R, Mwanri L. Migrants and Service Providers’ Perspectives of Barriers to Accessing Mental Health Services in South Australia: A Case of African Migrants with a Refugee Background in South Australia. Int J Environ Res Public Health. 2021;18(17):8906.
Cyril S, Nicholson JM, Agho K, Polonsky M, Renzaho AM. Barriers and facilitators to childhood obesity prevention among culturally and linguistically diverse (CALD) communities in Victoria, Australia. Aust N Z J Public Health. 2017;41(3):287–93.
Murray L, Elmer S, Elkhair J. Perceived barriers to managing medications and solutions to barriers suggested by bhutanese former refugees and service providers. J Transcult Nurs. 2018;29(6):570–7.
Javanparast S, Naqvi SKA, Mwanri L. Health service access and utilisation amongst culturally and linguistically diverse populations in regional South Australia: a qualitative study. Rural Remote Health. 2020;20(4):5694.
Babatunde-Sowole OO, Power T, Davidson PM, DiGiacomo M, Jackson D. Health screening and preventative health care in refugee women: A qualitative analysis. Contemp Nurse. 2020;56(1):62–79.
Stewart DE, Do BN. Health needs of migrant Vietnamese women in south-west Brisbane: an exploratory study. Aust J Soc Issues. 2003;38(2):247–61.
Wohler Y, Dantas JA. Barriers Accessing Mental Health Services Among Culturally and Linguistically Diverse (CALD) immigrant women in Australia: policy implications. J Immigr Minor Health. 2017;19(3):697–701.
Clark A, Gilbert A, Rao D, Kerr L. “Excuse me, do any of you ladies speak English?” Perspectives of refugee women living in South Australia: barriers to accessing primary health care and achieving the Quality Use of Medicines. Aust J Prim Health. 2014;20(1):92–7.
Bellamy K, Ostini R, Martini N, Kairuz T. Insights from the coalface: barriers to accessing medicines and pharmacy services for resettled refugees from Africa. Aust J Prim Health. 2019;25(2):118–24.
Saito S, Harris MF, Long KM, Lewis V, Casey S, Hogg W, Cheng IH, Advocat J, Marsh G, Gunatillaka N, et al. Response to language barriers with patients from refugee background in general practice in Australia: findings from the OPTIMISE study. BMC Health Serv Res. 2021;21(1):921.
Wamwayi MO, Cope V, Murray M. Service gaps related to culturally appropriate mental health care for African immigrants. Int J Ment Health Nurs. 2019;28(5):1110–8.
Yelland J, Riggs E, Szwarc J, Casey S, Duell-Piening P, Chesters D, Wahidi S, Fouladi F, Brown S. Compromised communication: a qualitative study exploring Afghan families and health professionals’ experience of interpreting support in Australian maternity care. BMJ Qual Saf. 2016;25(4):e1.
Valibhoy MC, Szwarc J, Kaplan I. Young service users from refugee backgrounds: their perspectives on barriers to accessing Australian mental health services. Int J Hum Rights in Healthc. 2017;10(1):68–80.
Komaric N, Bedford S, van Driel ML. Two sides of the coin: patient and provider perceptions of health care delivery to patients from culturally and linguistically diverse backgrounds. BMC Health Serv Res. 2012;12:322.
Mude W, Fisher C, Richmond J, Wallace J, Le Gautier R. A qualitative investigation of barriers, support-seeking and coping among South Sudanese people with chronic hepatitis B in Australia. Aust J Prim Health. 2019;25(3):264–74.
Drummond PD, Mizan A, Brocx K, Wright B. Barriers to accessing health care services for West African refugee women living in Western Australia. Health Care Women Int. 2011;32(3):206–24.
Ziersch A, Freeman T, Javanparast S, Mackean T, Baum F. Regional primary health care organisations and migrant and refugee health: the importance of prioritisation, funding, collaboration and engagement. Aust N Z J Public Health. 2020;44(2):152–9.
Yelland J, Riggs E, Szwarc J, Vanpraag D, Dawson W, Brown S. Improving the ascertainment of refugee-background people in health datasets and health services. Aust Health Rev. 2018;42(2):130–3.
Ziersch A, Walsh M, Baak M, Rowley G, Oudih E, Mwanri L. “It is not an acceptable disease”: a qualitative study of HIV-related stigma and discrimination and impacts on health and wellbeing for people from ethnically diverse backgrounds in Australia. BMC Public Health. 2021;21(1):779.
American Geriatrics Society Expert Panel on the Care of Older Adults with M. Patient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics Society: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012;60(10):1957–68.
Zeng L, Perry L, Xu X. Self-care behaviours and related cultural factors among Chinese immigrants with cardiovascular disease in western countries: an integrative review. J Clin Nurs 2021, n/a(n/a).
Chuah FL, Tan ST, Yeo J, Legido-Quigley H. Health system responses to the health needs of refugees and asylum-seekers in Malaysia: a qualitative study. Int J Environ Res Public Health. 2019;16(9):1584.
Parajuli J, Horey D, Avgoulas MI. Best practice models recommended by Bhutanese refugee women for cervical and breast cancer screening in Australia: a qualitative study. Health Promot J Austr. 2020;31(3):381–90.
Kay M, Wijayanayaka S, Cook H, Hollingworth S. Understanding quality use of medicines in refugee communities in Australian primary care: a qualitative study. Br J Gen Pract. 2016;66(647):e397-409.
Willis E, Xiao LD, Morey W, Jeffers L, Harrington A, Gillham D, De Bellis A. New migrants in residential aged care: managing diversity in not-for-profit organisations. J Int Migr Integr. 2018;19(3):683–700.
Sheikh-Mohammed M, Macintyre CR, Wood NJ, Leask J, Isaacs D. Barriers to access to health care for newly resettled sub-Saharan refugees in Australia. Med J Aust. 2006;185(11–12):594–7.
Ziersch A, Miller E, Baak M, Mwanri L. Integration and social determinants of health and wellbeing for people from refugee backgrounds resettled in a rural town in South Australia: a qualitative study. BMC Public Health. 2020;20(1):1700.
Acknowledgements
The first author thank his public health research colleagues from CALD backgrounds for their opinions in the early draft of this manuscript.
Funding
The University of Queensland funded the research. However, the University had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
RBK and YA conceived the idea of the research. RBK collected and analysed the data, and prepared the first and subsequent drafts. RBK and YA provided comments in subsequent drafts. YA supervised the study process. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khatri, R.B., Assefa, Y. Access to health services among culturally and linguistically diverse populations in the Australian universal health care system: issues and challenges. BMC Public Health 22, 880 (2022). https://doi.org/10.1186/s12889-022-13256-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13256-z