Abstract
Background
Previous research has demonstrated a correlation between chronic stress and chronic pain (CP). However, there have been few studies examining the prospective association of allostatic load (AL)—the biological processes related to stress—with CP.
Methods
We firstly conducted latent class analysis to identify phenotypes of AL using a community-dwelling sample, the Midlife in the United States. Multinomial logistic regression models were used to examine the prospective association between phenotypes of AL at MIDUS 2 biomarker project and the presence of CP, CP interference and the number of CP sites at MIDUS 3.
Results
Three phenotypes of AL, low biological dysregulation, parasympathetic dysregulation and metabolic dysregulation, were identified. Compared to low biological dysregulation group, participants experiencing metabolic dysregulation phenotype of AL at MIDUS 2 had higher risks of having high-interference CP (RRR = 2.00, 95% CI: 1.06, 3.79, P < 0.05) and 3 or more CP sites (RRR = 2.03, 95% CI: 1.08, 3.83, P < 0.05) at MIDUS 3.
Conclusion
The findings indicate that focusing on mitigating the metabolic dysfunction phenotype of AL has the potential to be an efficacious strategy for alleviating future CP bodily widespreadness and high CP interference.
Similar content being viewed by others
Introduction
Chronic pain (CP) is pain that lasts or recurs for more than 3 months [1]. CP is becoming a major health issue worldwide. In the US, an estimated 20.5% of adults suffer from CP each year, causing significant burden to the healthcare system and costing over $296 billion in lost productivity [2]. The pathological progression of CP has been linked to chronic stress-related physiological dysregulation across multiple systems [3,4,5]. Such dysregulation has been well described by the framework of allostatic load (AL). AL is defined as the physiological ‘wear and tear’ resulting from repeated adaptations to chronic stressors [6]. Long-term response to chronic stress leads to prolonged activation of the hypothalamus-pituitary-adrenal (HPA) axis and sympathetic nervous system, resulting in elevated levels of glucocorticoids and catecholamines [7, 8]. Over time, over-accumulation of these substances can have downstream consequences and contribute to subclinical conditions across cardiovascular, metabolic, and immune systems.
In the past few decades, there has been substantial evidence indicating the association between AL and various chronic diseases and symptoms [9], however, the examination of the association between AL and CP is still in its preliminary stage. CP is closely associated with chronic stress and may involve abnormalities in several biological systems. Notably, CP patients commonly present dysregulations in the HPA axis, the autonomic nervous system, and the immune system [5, 10]. Furthermore, CP patients often exhibit a range of maladaptive stress responses, including an inability to habituate to repeated similar stressors, a failure to turn off stress responses, and altered or inefficient responses to stress [3, 7]. These dysregulations significantly align with the conditions of the AL. Therefore, some scholars suggest that CP may represent an AL disease [3].
Mixed results regarding the association between AL and CP were found among clinical samples. Research indicates that pediatric patients with pain exhibit a greater risk of experiencing AL, and AL is associated with pain-related functional impairments [11]. A prospective association between AL and CP has been suggested. A one-year longitudinal study reported a mild correlation between the AL index and pain severity among chronic low back pain patients [12]. Specifically, a set of biomarkers encompassing norepinephrine, interleukin-6, triglycerides, waist-to-hip ratio, and resting pulse rate, that demonstrated significant predictive value for chronic low back pain. However, another 6-year longitudinal study reported no association between stress response systems and chronic widespread pain (CWP) improvement [13]. While the use of validated CP assessments helped to control measurement errors, the paradoxical results may be due to inconsistencies in operationalizing chronic stress response dysregulation and in measuring CP outcomes. Additionally, the clinical samples limits the applicability of these findings to the general population.
Several population-based studies have consistently demonstrated a positive association between AL and CP in cross-sectional analyses. For example, higher levels of AL are correlated with an increased likelihood of reporting CP, especially widespread bodily pain, among adults in the U.S [14]. However, this study only computed AL based on metabolic, inflammatory, and cardiovascular biomarkers, disregarding primary mediators such as biomarkers in the HPA axis and in sympathetic nervous system [7]. Among a sample of adults over the age of 50 in England, severe CP has been associated with a high level of AL, which encompassed HPA axis biomarkers, after adjusting for sociodemographic factors, health behaviors, and chronic conditions [15]. However, the measurement of CP duration was vague, using the term ‘often’ without specific time frames. Furthermore, the cross-sectional nature limits the ability to establish causal direction between AL and CP or to account for baseline confounders that might influence CP. Additionally, the AL index in previous research primarily relied on a summative score. This computation lacks the ability to discern AL differences within each biological system or across systems [16].
Our study aimed to investigate the prospective relationship between AL and CP using a community-dwelling sample. We utilized latent class analysis (LCA) to capture the nuances of AL phenotypes [17, 18]. Additionally, we used CP measures that adheres to the definition of CP in terms of pain duration [19], thereby enhancing the validity of our pain assessments. Our examination was also adjusted for a range of factors including sociodemographic characteristics, health-related behaviors, multiple chronic conditions, and detailed medication information. We hypothesized that AL phenotypes would be prospectively associated with increased risk of experiencing CP, increased number of pain locations, and greater pain interference after seven years.
Methods
Data
This study used the Midlife in the United States (MIDUS) from 2004 to 2014, including two main survey waves (MIDUS 2 and MIDUS 3) and a Biomarker Project of MIDUS 2. MIDUS is a national longitudinal study focusing on individual social status, psychological profiles, and biological processes of aging, initiated between 1995 and 1996 and followed 7,108 non-institutionalized Americans aged 25 to 74 in the contiguous United States. The main survey collected data by phone interviews and self-administered questionnaires.
Of the participants, 1,255 were involved in the Biomarker Project of MIDUS 2, conducted from 2004 to 2009. Samples meeting the following criteria were incorporated into the analyses (see Fig. 1): (1) samples that participated in the biomarker program and the MIDUS 3 follow-up survey, (2) samples that provided complete information on the major variables (AL and CP). The MIDUS is publicly accessible secondary data. More details of the study are available on the MIDUS website (Available at: http://midus.wisc.edu/).
Measures
Allostatic load
AL biomarkers were collected from the Biomarker Project of MIDUS 2. The project collected 12-hour urine samples, fasting blood samples, as well as nervous system function data from respondents during a one-day stay at a General Clinical Research Center (GCRC) of either UCLA, University of Wisconsin, or Georgetown University, depending on the residence of respondents [20].
Following previous studies [7, 16, 21], AL was constructed into seven physiological systems from 27 biomarkers (shown in Table 1). A high-risk quartile of biomarkers were used [22]. Dehydroepiandrosterone sulfate (DHEA-S) and cortisol in the upper or lower 25th quartile were regarded as at high risk. When high-frequency heart rate variability (HFHRV), low-frequency heart rate variability (LFHRV), root mean square of successive differences (RMSSD), standard deviation of heart beat to heart beat intervals (SDRR), and high-density lipoprotein (HDL) cholesterol strength fell within their lower 25th quartile ranges, individuals were classified as high risk. Other biomarkers falling into their upper 25th quartile were assigned to the high-risk range. Then, biomarkers in their high-risk quartile were coded as 1; otherwise, 0. The high-risk thresholds are detailed in Table 1.
Then, LCA was used to capture the phenotypes of AL (package “poLCA” in R). The binary biomarkers were fitted into 1–7 clusters, and the selection of the optimum number of cluster was based on log-likelihood, Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), entropy, and interpretability of classification. Regarding entropy, an ideal value is close to 1, and above 0.8 is acceptable [23]. As for AIC and BIC, lower values indicate a better fit [24]. However, BIC tends to favor simpler models in larger samples due to its complexity penalty, while AIC may lean towards more complex models. Given these considerations, seeking points of inflection or plateauing for BIC and AIC can balance model complexity against the risk of overfitting [24]. Also, the classification should be meaningful from a clinical or a biological perspective [24]. Additionally, each cluster should have at least 10% of the sample [23, 24]. 5000 iterations were set to generate convergent estimation for each LCA model.
Outcome: chronic pain
CP interference and the number of CP sites from MIDUS 3 were utilized. Respondents were first asked “Do you have chronic pain, that is do you have pain that persists beyond the time of normal healing and has lasted from anywhere from a few months to many years?” An affirmative response indicated the presence of CP and the respondents were then asked about CP interference. A pain interference index was generated by calculating a mean score of how much pain interfered with respondents’ activity, mood, relations, sleep, and enjoyment, ranging from 0 to 10 [25, 26]. Then, the pain interference index was further categorized into no pain, low interference pain (≤ 4), and high interference pain (> 4) as categorical variable [25]. In addition, if respondents reported having CP, they were asked about the location of the pain, including head, neck, back, arms, legs, shoulders, hips, knees, and other sites. We summed up the pain sites into an index and then categorized it into no pain, 0–2 sites, or 3 or more sites as a categorical variable [26, 27].
Covariates
Covariates were selected by current knowledge about the association between AL and CP [14, 15, 28]. Sociodemographic covariates were obtained from the MIDUS 2 main survey and were coded as categorical variables except for the age variable, which was treated as continuous. Sociodemographic covariates included gender (ref: males), age, ethnicity (ref: White), educational attainment (i.e., the highest educational certificate a respondent had obtained, ref: high school or less), marital status (ref: Married), and the income-to-needs ratio (INR, ref: Affluent) [29] which was computed by dividing total household income by Federal Poverty Threshold [30]. Additionally, behavior factors from the MIDUS 2 Biomarker Project were considered. They were alcohol intake status (ref: Moderate + drinker), smoking status (ref: Current smokers), and categories of the metabolic equivalent of task (MET, ref: Between 500 and 1000 min per week) minutes per week [26, 31]. Also, the time gap between the two data collections was controlled for. Finally, adverse childhood experiences (ACEs) also possibly confound the relationship between AL and CP [32, 33]. In this case, we considered emotional abuse and physical abuse from parents. The ACE data were retrospectively collected in the MIDUS 1 and were treated as ordinal variables.
Multimorbidity was also adjusted for [28, 34]. The chronic condition index summed up a count of “Yes” responses to the chronic conditions-related questions [20]. Then, the index was coded as a binary variable (Ref: <2) and the index more than 2 was regarded as multimorbidity. Since mental health conditions were already incorporated in this variable, there were no extra adjustments for depression and anxiety.
MIDUS 2 Biomarker Project enhanced medication reports by linking medication names and IDs to Generic Names and Lexi-Data database and asking respondents for their reasons for taking medications [20]. A binary variable was created to represent whether a participant had taken any medication from a selection of antihyperlipidemic agents, beta adrenergic blocking agents, antihypertensive combinations, analgesics, anxiolytics sedatives and hypnotics, antidiabetic agents, sex hormones, thyroid hormones, antidepressants, and analgesics, including opioids and non-opioids.
Analysis
Statistical methods
Regression models were chosen according to types of CP variables. For a binary CP variable, logistic regressions were used. The number of pain location and pain interference were categorical variables, therefore, multinomial logistic regressions were utilized. All main analyses presented were fully adjusted for relevant confounders to reduce spurious associations and were generated from the complete cases.
Three sensitivity analyses were applied. Firstly, data missingness can lead to biased estimation [35, 36]. Multiple imputation (MI) using the R package “MICE” [37] was employed to address item nonresponse, based on the assumption of missing at random (MAR). Missing covariates were imputed in accordance with the specific distribution of each item, as recommended [36]. Twenty imputed datasets were generated, and the coefficients from all statistical models were combined using Rubin’s rules. ANOVA tests and chi-squared tests were performed respectively for continuous variables and categorical variables to check the similarity of imputed datasets and the observed dataset. Secondly, bootstrapping method was used to estimate the variability and robustness of coefficients [38]. A total of 5000 bootstrap samples were generated with replacement, each with the same sample size as the original dataset. The bootstrapping process was conducted by R. Finally, CP status at MIDUS 2 was incorporated into the model and the binary measure of medication intake at MIDUS 2 was substituted with specific individual medications.
Results
Descriptive statistics
Table 2 displays the descriptive statistics of the analytic sample (N = 781). 62.7% of participants reported no CP and 37.3% of participants reported the presence of CP. 24.6% of participants had low-interference pain, and 12.7% of participants had high-interference pain. In terms of the number of pain locations, 23.8% of participants reported 0–2 pain sites and 13.4% of participants reported 3 or more pain sites. The majority of respondents were females, non-Hispanic whites, affluent, and married, with over 48% of respondents being highly educated (above high school degree). Additionally, there were no significant differences between observed dataset and imputed datasets, supporting the validity of the imputation process.
Supplement Table 1 presents the fit statistics for latent class model with 1–7 clusters, the 3-cluster model was considered the optimal clustering. Despite the continuous reduction in AIC and BIC, along with the progressive improvement in log-likelihood, the enhancement in the fitness of the model with 4 and 5 clusters was rather moderate. On the other hand, the 3-cluster model exhibited the best entropy, suggesting a good classification. Additionally, the 3-cluster model had an ample number of observations within each cluster and presented meaningful separation. Therefore, the 3-cluster model was adopted.
According to Supplement Table 2, class 1 is designated as ‘Baseline’ due to its association with a low risk across most biomarkers. Class 2, termed ‘Parasympathetic Dysregulation,’ is distinguished by significantly lower values in HFHRV, LFHRV, RMSSD, and SDRR, suggesting potential impairments in parasympathetic system functioning. Class 3 is characterized by marked increases in fasting glucose, HbA1c, HOMA-IR, triglycerides, WHR, and BMI, coupled with a notable decrease in HDL concentrations. These characteristics are consistent with the physiological patterns commonly observed in metabolic dysregulation. Figure 2 shows the phenotypes of AL. 51.6% of the participants were classified as low AL risk group, 24.2% of participants were in the phenotype of parasympathetic dysregulation, and an additional 24.2% demonstrated signs of metabolic dysregulation.
Model results
Table 3 presents regression results. In the fully adjusted binary logistic regression models, there was no statistically significant association between any AL dysregulation phenotype and CP status compared to the low AL risk phenotype.
In the multinomial logistic regression models (Table 4), the prospective association between the metabolic dysregulation phenotype and high-interference CP was significant (RRR = 2.00, 95% CI: 1.06, 3.79, P < 0.05), compared to the baseline phenotype. In the prospective association between the number of pain sites and biological dysregulation phenotypes, metabolic dysregulation was significantly associated with 3 or more CP sites (RRR = 2.03, 95% CI: 1.08, 3.83, P < 0.05). There were no other significant associations found. In the sensitivity analyses, the results remained similar. The similar results generated from the imputed datasets indicated that data missingness did not significantly biased the estimates. Also, the results generated from the bootstrapping samples were similar to the main analyses, indicating that the association was expected to persist even when accounting for potential uncertainties. Finally, after extra adjusting for medication intakes as separate factors and CP status at MIDUS 2, the results remained stable. Supplement Table 3 displays the full models for examining the relationship between AL phenotypes and CP status, CP interference, and the number of CP locations.
Predicted probabilities
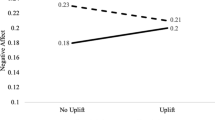
Table 5 presents the adjusted prevalence for CP outcomes grouped by AL phenotypes. Using the average adjusted predicted probabilities from the models, we calculated the probability of CP outcomes by AL phenotypes. The metabolic dysregulation phenotype was significantly associated with high-interference pain and 3 or more CP sites as shown in Table 4. Respondents with the metabolic dysregulation phenotype were more likely to experience a higher degree of CP conditions than those with a low AL risk profile. Specifically, those with metabolic dysregulation driven AL had a 4.88% adjusted probability of reporting high pain interference and had a 4.58% adjusted probability of reporting more than 3 pain locations. In contrast, these probabilities were lower, at 2.48% and 2.29% respectively, among respondents with a baseline AL profile.
Discussion
The present study identified three phenotypes of AL through LCA, encompassing low levels of biological dysregulation, AL driven by parasympathetic dysregulation, and AL driven by metabolic dysregulation. Also, consistent with previous research [14, 15, 39, 40], we found that AL driven by metabolic dysregulation is associated with more severe CP interference and a greater number of CP sites. For instance, a cross-sectional study based on a sample of population aged over 50 in the UK revealed that, after controlling for sociodemographic factors and comorbid conditions, high-risk biomarker, defined by the upper quartile and including HDL, HBA1c, and WHR, are related to increased severity of CP [15]. Similarly, in American adults, higher BMI and triglyceride levels are associated with a higher prevalence of widespread bodily pain [14].
Compared to previous studies, our research offers several advantages. Firstly, we employed a more comprehensive set of biomarkers, including those from the HPA axis, and the sympathetic and parasympathetic nervous systems, to construct a more valid AL measurement [7]. Moreover, our use of LCA to identify AL phenotypes captured the common variability of biomarkers, while previous studies that used single biomarkers for regression with CP to examine the AL driving systems of CP overlooked the interrelationships among biomarkers within the AL framework [14, 15]. On the other hand, prior operationalizations of AL, based on summative computation that assigns equal weight to each biomarker, may obscure the specific impacts of different AL components on CP. In summary, LCA offers a nuanced method for exploring the specific components of AL that drive CP.
Furthermore, this study’s strengths include its prospective design, community-dwelling sample, adjustments for early confounders, and the substantial avoidance of trivial and recent pain in measurement by adhering to the definition of CP in terms of pain duration. Thus far, this research may be the first community-dwelling study to examine the prospective association between AL and CP.
However, this study also has limitations. Firstly, the measurement of pain is self-reported. Even when controlling for potential reporting biases from relevant sociodemographic factors, unobserved factors can still introduce biases in pain assessment. Furthermore, the variability in CP measures across various surveys partly limits the comparability of findings. For instance, the MIDUS survey assesses pain interference, which differs from the pain severity measurements used in other studies. While pain interference is associated with pain severity, the association is affected by patients’ beliefs about pain, their tendency towards catastrophizing, and their pain coping strategies. These factors can alter the relationship between pain interference and pain severity [41]. Therefore, there is a need for further prospective research to explore the link between AL and CP severity in more depth.
Additionally, the available data on AL was only collected in MIDUS 2 during our research, however, the upcoming biomarker data present opportunities for future research on the association between AL trajectories and the development of CP. Also, the sample composition is predominantly white people, and future studies focusing on ethnic minorities are encouraged. Moreover, our findings from the U.S. data may not generalize to other countries due to differences in health care systems, lifestyle choices, and the impact of sociocultural variables on the reporting and perception of pain. Lastly, this study only examined the prospective association in one direction and future research on the reverse association may be beneficial elucidate the causal direction.
While the underlying mechanism remains undetermined, several potential explanations could account for the prospective positive association between the metabolic dysregulation phenotype of allostatic load and both high-interference pain as well as an increased number of pain sites. The AL model proposes, when undergoing repeated stress adaptation, the prolonged secretion of stress hormones and inflammatory cytokines can disrupt the normal regulation of downstream physiological systems, such as the metabolic system [7]. Dyslipidemia and high BMI may be associated with upregulation of cytokines, leading to low-grade inflammation, a condition frequently observed in patients with fibromyalgia [42]. Additionally, a high waist-to-hip ratio may be related to structural changes in intervertebral discs and being consistently subjected to high biomechanical loads [43]. This highlights the significant role that metabolic dysregulation related to adiposity may play in low back pain. Meanwhile, elevated blood glucose is associated with peripheral neuropathy or synergistically interacts with high BMI and the sequential inflammation, thereby potentially increasing the likelihood of experiencing daily pain [44]. Also, metabolic dysregulation could potentially reduce the pain activation threshold via its interplay with inflammatory mechanisms. This interaction may intensify pain response by increasing synaptic strength and reducing inhibition, allowing even low-threshold stimuli to activate pain pathways [45, 46].
Nevertheless, we did not find any prospective associations between AL driven by the parasympathetic nervous system and CP. Low parasympathetic nervous system activity may represent low capacity to respond to chronic stress. A meta-analysis, which thoughtfully sieved through 26 moderate-high-quality studies from a pool of 17,350 publications, uncovered that biomarkers relating to the parasympathetic nervous system (LFHRV, HFHRV, RMSSD, R-R interval, and SDRR) exhibited an association with CP [47]. However, the association appears to be predominantly influenced fibromyalgia and its significance may vary across CP conditions [5]. CP may also maladapt parasympathetic nervous system directly. Therefore, future research is encouraged to focus on exploring the potential links between the parasympathetic nervous system and different subtypes of CP to clarify these relationships.
Conclusion
In conclusion, our findings indicate that metabolic dysregulation as a phenotype of AL is prospectively associated with high-interference CP and 3 or more CP sites. Differentiating nuances of biological dysregulation of AL could facilitate the development of precise clinical interventions aimed at specific biological mechanisms, which may alleviate the impacts of AL on the conditions of CP.
Availability of data and materials
MIDUS data are freely available to the public via the Web by opening an Inter-university Consortium for Political and Social Research user account.
References
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of Chronic Pain for the International classification of diseases (ICD-11). Pain. 2019;160(1):19–27.
Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic pain among adults in the United States. Pain. 2022;163(2):e328-332.
Borsook D, Maleki N, Becerra L, McEwen B. Understanding migraine through the Lens of maladaptive stress responses: a model disease of allostatic load. Neuron. 2012;73(2):219–34.
Rabey M, Moloney N. I don’t know why I’ve got this Pain! Allostasis as a possible explanatory model. Phys Ther. 2022;102(5):pzac017.
Woda A, Picard P, Dutheil F. Dysfunctional stress responses in chronic pain. Psychoneuroendocrinology. 2016;71:127–35.
McEwen BS, Stellar E. Stress and the Individual: mechanisms leading to Disease. Arch Intern Med. 1993;153(18):2093–101.
Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16.
McEwen BS. Stress, adaptation, and Disease: Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840(1):33–44.
Guidi J, Lucente M, Sonino N, Fava GA. Allostatic load and its impact on Health: a systematic review. Psychother Psychosom. 2021;90(1):11–27.
Abdallah CG, Geha P. Chronic Pain and chronic stress: two sides of the same Coin? Chronic Stress. 2017;1:247054701770476.
Nelson S, Bento S, Enlow MB. Biomarkers of allostatic load as correlates of Impairment in Youth with Chronic Pain: an initial investigation. Children. 2021;8(8): 709.
Wippert PM, Puerto Valencia L, Drießlein D. Stress and Pain. Predictive (Neuro)Pattern Identification for Chronic Back Pain: a longitudinal observational study. Front Med. 2022;9: 828954.
Generaal E, Vogelzangs N, Macfarlane GJ, Geenen R, Smit JH, de Geus EJCN, et al. Biological Stress Systems, adverse life events, and the improvement of chronic Multisite Musculoskeletal Pain across a 6-Year Follow-Up. J Pain. 2017;18(2):155–65.
Slade GD, Sanders AE, By K. Role of allostatic load in sociodemographic patterns of Pain Prevalence in the U.S. Population. J Pain. 2012;13(7):666–75.
Sibille KT, McBeth J, Smith D, Wilkie R. Allostatic load and pain severity in older adults: results from the English Longitudinal Study of Ageing. Exp Gerontol. 2017;88:51–8.
Carbone JT, Clift J, Alexander N. Measuring allostatic load: approaches and limitations to algorithm creation. J Psychosom Res. 2022;163: 111050.
Carbone JT. Allostatic load and mental health: a latent class analysis of physiological dysregulation. Stress. 2021;24(4):394–403.
Forrester SN, Leoutsakos JM, Gallo JJ, Thorpe RJ, Seeman TE. Association between allostatic load and health behaviours: a latent class approach. J Epidemiol Community Health. 2019;73(4):340–5.
Bonica JJ, Hoffman JF. The Management of Pain with special emphasis on the Use of Analgesic blocks in diagnosis, prognosis, and Therapy. Anesth Analgesia. 1954;34(5):57–8.
Ryff CD, Seeman T, Weinstein M. Midlife in the United States (MIDUS 2): Biomarker Project, 2004–2009. Inter-university Consortium for Political and Social Research [distributor]; 2022.
Carbone JT, Holzer KJ, Clift J, Fu Q. Latent profiles of biological dysregulation and risk of mortality: time-to-event analysis using the midlife in the US longitudinal study. J Epidemiol Community Health. 2023;77(3):182–8.
McEwen BS, Seeman T. Protective and Damaging effects of mediators of stress: elaborating and testing the concepts of Allostasis and allostatic load. Ann N Y Acad Sci. 1999;896(1):30–47.
Weller BE, Bowen NK, Faubert SJ. Latent class analysis: a guide to best practice. J Black Psychol. 2020;46(4):287–311.
Sinha P, Calfee CS, Delucchi KL. Practitioner’s guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. 2021;49(1):e63-79.
Jensen MP. Measuring pain interference. In: The pain stethoscope: A clinician’s guide to measuring pain. Tarporley: Springer Healthcare Ltd.; 2011 . p. 23–7. Available from: http://link.springer.com/https://doi.org/10.1007/978-1-908517-43-2_6. Cited 2022 Nov 9.
Li R, Chapman BP, Smith SM. Blood dehydroepiandrosterone and Dehydroepiandrosterone Sulfate as Pathophysiological correlates of Chronic Pain: analyses using a national sample of midlife adults in the United States. Pain Med. 2021;22(2):243–54.
Li R, Kreher DA, Jusko TA, Chapman BP, Bonham AD, Seplaki CL. Prospective Association between Dysmenorrhea and Chronic Pain Development in Community-Dwelling women. J Pain. 2021;22(9):1084–96.
Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273-283.
Diemer MA, Mistry RS, Wadsworth ME, López I, Reimers F. Best practices in conceptualizing and measuring Social Class in Psychological Research: Social Class Measurement. Anal Soc Issues Public Policy. 2013;13(1):77–113.
United States Census Bureau. Poverty Thresholds by Size of Family and Number of Children. 2022. Poverty Thresholds by Size of Family and Number of Children. Available from: https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html.
Office of Disease Prevention and Health Promotion. 2008 Physical Activity Guidelines for Americans. 2008 . Available from: https://health.gov/our-work/nutrition-physical-activity/physical-activity-guidelines/previous-guidelines/2008-physical-activity-guidelines. Cited 2022 Oct 26.
Graves KY, Nowakowski ACH. Childhood socioeconomic status and stress in late adulthood: a Longitudinal Approach to measuring allostatic load. Global Pediatr Health. 2017;4:2333794X1774495.
Misiak B, Stańczykiewicz B, Pawlak A, Szewczuk-Bogusławska M, Samochowiec J, Samochowiec A, et al. Adverse childhood experiences and low socioeconomic status with respect to allostatic load in adulthood: a systematic review. Psychoneuroendocrinology. 2022;136: 105602.
Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic Diseases—A systematic review on existing Multimorbidity indices. The J Gerontol: Series A. 2011;66A(3):301–11.
He Y. Missing Data Analysis using multiple imputation. Circulation: Cardiovasc Qual Outcomes. 2010;3(1):8.
Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338(jun29 1):b2393-2393.
van Buuren S, Groothuis-Oudshoorn K. MICE: Multivariate Imputation by Chained Equations in R. J Stat Soft. 2011 ;45(3). Available from: http://www.jstatsoft.org/v45/i03/. Cited 2023 Mar 25.
Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Statist Med. 2000;19(9):1141–64.
Loevinger BL, Muller D, Alonso C, Coe CL. Metabolic syndrome in women with chronic pain. Metabolism. 2007;56(1):87–93.
Sibille KT, Steingrímsdóttir ÓA, Fillingim RB, Stubhaug A, Schirmer H, Chen H, et al. Investigating the Burden of Chronic Pain: an inflammatory and metabolic composite. Pain Res Manage. 2016;2016:1–11.
Jensen MP, Tomé-Pires C, de la Vega R, Galán S, Solé E, Miró J. What determines whether a Pain is rated as mild, moderate, or severe? The Importance of Pain beliefs and Pain Interference. Clin J Pain. 2017;33(5):414–21.
Ghafouri B, Edman E, Löf M, Lund E, Leinhard OD, Lundberg P, et al. Fibromyalgia in women: association of inflammatory plasma proteins, muscle blood flow, and metabolism with body mass index and pain characteristics. PAIN Rep. 2022;7(6):e1042.
Hussain SM, Urquhart DM, Wang Y, Shaw JE, Magliano DJ, Wluka AE, et al. Fat mass and fat distribution are associated with low back pain intensity and disability: results from a cohort study. Arthritis Res Ther. 2017;19(1):26.
Mäntyselkä P, Miettola J, Niskanen L, Kumpusalo E. Chronic pain, impaired glucose tolerance and diabetes: a community-based study. PAIN®. 2008;137(1):34–40.
Veldhuijzen DS, van Middendorp H, Evers AWM. Stress and Sensitization in Chronic Pain. In: Karoly P, Crombez G, editors. Motivational Perspectives on Chronic Pain [Internet]. Oxford University Press; 2018 [cited 2022 Oct 29]. https://doi.org/10.1093/oso/9780190627898.003.0005.
Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3):2–15.
Tracy LM, Ioannou L, Baker KS, Gibson SJ, Georgiou-Karistianis N, Giummarra MJ. Meta-analytic evidence for decreased heart rate variability in chronic pain implicating parasympathetic nervous system dysregulation. Pain. 2016;157(1):7–29.
Acknowledgements
The authors acknowledge the MIDUS study coordinators and MIDUS participants for their contribution to this research.
Since 1995 the MIDUS study has been funded by the following: John D. and Catherine T. MacArthur Foundation Research Network, National Institute on Aging (P01-AG020166), National institute on Aging (U19-AG051426).
Biomarker data collection was further supported by the NIH National Center for Advancing Translational Sciences (NCATS) Clinical and Translational Science Award (CTSA) program as follows: UL1TR001409 (Georgetown), UL1TR001881 (UCLA), 1UL1RR025011 (UW).
Funding
The authors declare that this work was not funded by any external sources.
Author information
Authors and Affiliations
Contributions
Y. L. and C. B. contributed to the conceptualization. Y. L. wrote the main manuscript, prepared all figures and tables, and conducted the formal analysis. All authors reviewed and edited the manuscript. C. B. contributed to supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
MIDUS data collection is reviewed and approved by the Education and Social/Behavioral Sciences and the Health Sciences IRBs at the University of Wisconsin-Madison.
Consent for publication
All participants provided written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liang, Y., Booker, C. Allostatic load and chronic pain: a prospective finding from the national survey of midlife development in the United States, 2004–2014. BMC Public Health 24, 416 (2024). https://doi.org/10.1186/s12889-024-17888-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17888-1