Abstract
Background
In 2020/2021 in Germany, several non-pharmacological interventions were introduced to lower the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). We investigated to what extent knowledge of prior infection with SARS-CoV-2 or vaccination status influenced the use of personal protection measures (PPM). Further, we were interested in the effect of compliance with PPM on SARS-CoV-2 serostatus.
Methods
Data was based on a sequential, multilocal seroprevalence study (MuSPAD), carried out in eight locations from July 2020 to August 2021. We estimated the association between a known SARS-CoV-2 serostatus (reported positive PCR test or vaccination) and self-reported PPM behavior (hand hygiene, physical distancing, wearing face mask), just as the association of PPM compliance with seropositivity against nucleocapsid (NC), receptor-binding domain (RBD), and spike protein (S) antigens. We identified relevant variables and deduced adjustment sets with directed acyclic graphs (DAG), and applied mixed logistic regression.
Results
Out of the 22,297 participants (median age: 54 years, 43% male), 781 were classified as SARS-CoV-2-infected and 3,877 had a vaccinated immune response. Vaccinated individuals were less likely to keep 1.5 m distance [OR = 0.74 (95% CI: 0.57–0.97)] and only partly physically distanced [OR = 0.71 (95% CI: 0.58–0.87)]. Participants with self-reported positive PCR test had a lower chance of adhering partly to physical distancing [OR = 0.70 (95% CI: 0.50–0.99)] in comparison to the reference group. Higher odds of additionally wearing a face mask was observed in vaccinated [OR = 1.28 (95% CI: 1.08–1.51)] even if it was not obligatory. Overall, among unvaccinated participants, we found little evidence of lower odds of seropositivity given mask wearing [OR: 0.91 (95% CI: 0.71–1.16)], physical distancing [OR: 0.84 (95% CI: 0.59–1.20)] and no evidence for completely adhering to hand cleaning [OR: 0.97 (95% CI: 0.29–3.22)].
Conclusions
A known confirmed prior infection and vaccination may have the potential to influence adherence to PPM.
Similar content being viewed by others
Introduction
In Germany, the first SARS-CoV-2 case was registered in January 2020 [1]. The seroprevalence measured by antibodies against Spike antigens of SARS-CoV-2 in the unvaccinated population in Germany was estimated from July-December 2020 to be 1.3%–2.8% and increased in February-May 2021 to 4.1–13.1% [2].
During the pandemic and in the absence of vaccines or effective medication within the first 12 months, personal protection measures (PPM), such as physical distancing, use of face masks, adequate indoor ventilation, avoiding crowded indoor spaces, hand hygiene, and cleaning the environment were important protective measures [3, 4]. In Germany as of March 2020 lockdowns, curfews and contact bans were imposed, and various facilities, such as schools were closed and events canceled [5, 6]. The requirement of wearing face masks in public transport and for shopping was implemented on April 29, 2020, followed by lockdowns lasting from November 2020 until March 2021 [5, 6]. The vaccination campaign started at the end of December 2020 [7]. The first policy measures were eased at the beginning of March 2021, with regional differences in the opening of stores with strict hygiene measures, and citizens could get tested free of charge at test centers [5, 6].
Wearing masks, performing social distancing, having close contact for less than 15 min, and frequent hand washing were independently associated with a lower risk of a positive polymerase chain reaction (PCR) test after having had contact to a SARS-CoV-2 index case [8]. Reduced incidences of COVID-19 were associated with increased handwashing, face mask wearing, and physical distancing [9]. In addition, a combination of social distancing, testing for SARS-CoV-2, contact tracing, and quarantine could lower pressure on the health care systems [10].
In Germany, the number of newly reported infections with SARS-CoV-2 decreased between 15 to 75%, depending on the region, after the introduction of mandatory face masks, and the overall daily growth rate of reported infections decreased by 47% [11]. The requirement to wear masks in educational institutions reduced the number of infections both within and outside educational settings [11, 12].
Many of the studies performed were of ecological nature and assessed the association between recommendations or mandates and population-level infection indicators [11, 13]. The relationship between individual compliance with PPM and its impact on SARS-CoV-2 serostatus remains unclear in real-life settings. Additionally, how PPM are related to individual knowledge of vaccination and prior infection has not been assessed in larger studies – which could generate transferable knowledge to improve parametrization of future infectious disease models.
This is why we assessed participants’ behavior in the population-based study MuSPAD. The primary aim was to estimate the effect of a reported positive PCR test of SARS-CoV-2 (since the onset of the pandemic) or vaccination against SARS-CoV-2 on specific self-reported PPM behavior. The secondary aim was to evaluate the effect of self-reported adherence with PPM on seropositivity of SARS-CoV-2.
Methods
Study design and study population
The MuSPAD study is a German population-based seroepidemiologic cross-sectional study to assess the prevalence of antibodies against SARS-CoV-2 [2]. The data collection period was July 2020 to August 2021. The study was developed according to the WHO protocol for SARS-CoV-2 seroprevalence studies [14] and STROBE [15], and has been described before [2].
A random sample was drawn from population registration offices, stratified by age groups, gender, and spatial distribution to be representative in these aspects. Participants were 18 years or older. Included in the current analyses is a subset of the MuSPAD study comprising eight districts in Germany (Reutlingen, Freiburg, Aachen, Osnabrueck, Chemnitz, Magdeburg, Hannover (NAKO participants) and Greifswald-Vorpommern), and excluding mutations of SARS-CoV-2 and longitudinal observations. To answer the second research question, we excluded participants who were vaccinated against SARS-CoV-2 based on multiplex immunoassay (MultiCoV-Ab) [16]. Further details of the MuSPAD study were published previously [2].
Measurements and definitions
Specimen collection and serological testing
In each region, study centers followed standardized operating procedures when collecting blood samples. The serums were aliquoted and adequately stored at the Hannover Unified Biobank [2].
To distinguish between SARS-CoV-2 vaccinations, natural immunity after SARS-CoV-2 infection and no immunity, further analyses were performed by the MultiCoV-Ab [16]. This assay shows an improved sensitivity (88.3%) and specificity (100%) compared to other commercial tests and included analysis of using SARS-CoV-2 trimeric full-length spike protein (S), receptor-binding domain (RBD), and full-length nucleocapsid (NC) of SARS-CoV-2 and the endemic human coronaviruses [2]. A previous infection with SARS-CoV-2 was assumed before December 2020 in those with cut-offs by S > 1 and RBD > 1. From January 2021 to August 2021, the cut-off for previous infection with SARS-CoV-2 was set to S > 1, RBD > 1, and NC > 1. Vaccination against SARS-CoV-2 was based on the following values determined by the test: S > 1, RBD > 1 and NC ≤ 1. If participants were infected with SARS-CoV-2 after vaccination, they were counted as infected with SARS-CoV-2. More information is shown in the supplement (Supplement Table 2). Whether a participant had a known previous infection with SARS-CoV-2 was confirmed by a self-reported positive PCR test since the onset of the pandemic.
Selection and measurement of variables
All relevant PPM were identified based on the recommendations of the government and health authorities [3, 4, 17]. In the analysis, we defined PPM as physical distancing, hand cleaning, and face mask wearing.
Compliance with PPM were measured via self-administered questionnaires and interviews. Physical distancing (1.5 m) and hand cleaning were assessed by the question whether participants were able to adhere “Yes, completely,” “Yes, partly” or “No, not at all”. To capture face mask compliance, participants were asked to state where and whether they wore their face masks on mandatory occasions or on mandatory plus additional occasions.
For the outcome hand cleaning, we merged the two lower categories due to the low number of observations (No, not at all: n = 91; Yes, partly: n = 6,100). We assumed that participants who do not or only partially comply with the rules do not differ too much in this context. For the outcome physical distancing, we tested each category against each other and built up three models, as we deemed all categories as distinct. For the second research question, where these variables were independent variables, we analyzed all three categories so as not to lose any information. The variable gender was included as a binary variable, distinguishing between “male” and “female” – due to a low number of observations (n = 4) the category “diverse” had to be excluded for the regression. More information about data preparation can be found in the supplement (Supplement data preparation).
Statistical analysis
Descriptive statistics were used to explore the sample characteristics using median and interquartile range (IQR) for continuous variables, absolute and relative frequencies for categorical variables.
Relevant variables and their associations were determined by subject matter knowledge. Directed acyclic graphs (DAG) were used to visualize these associations and to deduce the minimal adjustment sets with the online tool DAGitty [18]. Mixed logistic regression models were applied to estimate the effect of self-reported positive SARS-CoV-2 PCR test since the onset of the pandemic or vaccination against SARS-CoV-2 on PPM compliance, just as the effect of PPM on seropositivity after an infection with SARS-CoV-2. All models included random intercepts for time and geographical region and were based on available cases. Derived odds ratio (OR) estimates were reported along with 95% confidence intervals (CI).
Data were analyzed with the statistics software R (Version 4.13), just as R packages lme4, gtsummary, and tidyverse [19,20,21,22].
Ethics and data protection
MuSPAD complies with all relevant laws and declarations – EU Charter of Fundamental Rights, Biomedical Convention of the Council of Europe and additional protocols, the Council for International Organizations of Medical Sciences guidelines, and the Helsinki Declaration. Ethical approval was obtained on June 21, 2020 by the Ethics Committee of the Hannover Medical School (No 9086_BO_S_2020) and ethics committees for NAKO (Bavarian Medical Association “Bayerische Landesärztekammer” (1302313031) and Medical Association of Lower Saxony “Ärztekammer Niedersachen” (Grae/067/2013)). Furthermore, the study complies with the requirements of the General Data Protection Regulation and the Federal Data Protection Act and Recommendations for Ensuring Good Epidemiological Practice of the German Society for Epidemiology e.V. [23].
Results
Characteristics of the study population
The subsample included 22,927 participants from the original MuSPAD study (N = 25,712) who were eligible, offered a blood sample, and completed the PPM questionnaire. Of these, 781 were classified as infected with SARS-CoV-2, and 3,877 showed a vaccinated immune response (Table 1). Overall, the median age was 54 years (IQR = 39, 65), the same as for SARS-CoV-2-infected participants (IQR = 40, 64). Among participants vaccinated against SARS-CoV-2, the median age was 59 years (IQR = 48, 69). Of the study population, 57% were female, 60% of women were vaccinated, 41% of men were classified as naturally infected with SARS-CoV-2, and 43% had no immune response. More detailed study sample characteristics are shown below (Table 1).
Self-reported compliance with PPM
During the observation period, 32% of participants reported full compliance with the PPM physical distancing. Stratified by serostatus, 39% of those vaccinated, 33% of those infected, and 30% of those without antibodies against SARS-CoV-2 fully adhered to physical distancing. 63% partially complied with the recommended distance of 1.5 m and 4.9% were unable to comply at all. Overall, 71% fully complied with hand cleaning, while 28% complied partly, whereby the highest compliance with hand cleaning was seen in vaccinated participants with 76%. Face masks were worn on occasions only when mandatory by 13% and on occasions when mandatory plus other occasions by 87% of the participants (Table 2). The highest compliance with face masks wearing of 88% was reported by those with no antibodies against SARS-CoV-2.
Association of a self-reported positive SARS-CoV-2 PCR test and SARS-CoV-2 vaccination with PPM
To assess the relationship of SARS-CoV-2 vaccination with compliance to PPM, we deduced the following minimal adjustment sets, visualized with DAGs in Supplementary Figs. 1 and 2: age, education, gender, occupation, and pre-existing medical condition. Where known prior infection was the primary exposure, household size and smoking status were added.
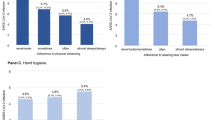
The odds of full adherence to physical distancing versus non-adherence were 26% decreased in vaccinated compared to unvaccinated participants [OR: 0.74 (95% CI: 0.57–0.97), n = 7,052] and 11% decreased in participants having a self-reported positive PCR test since the onset of the pandemic [OR: 0.89 (95% CI: 0.60–1.32), n = 7,281]. Vaccinated participants had lower odds of partial compliance to physical distancing [OR: 0.71 (95% CI: 0.58–0.87), n = 13,268], just as participants with a self-reported positive PCR test [OR: 0.70 (95% CI: 0.50–0.99), n = 13,666]. Vaccinated and unvaccinated did not relevantly differ regarding their odds of full compliance to physical distancing [OR: 1.00 (95% CI: 0.89–1.14), n = 18,382], but participants with a self-reported positive PCR test had higher odds to fully comply [OR: 1.18 (95% CI: 0.97–1.45), n = 18,917] (Fig. 1).
The odds of adhering completely to hand cleaning compared to no and partial adherence were similar in vaccinated and unvaccinated participants [OR: 1.03 (95% CI: 0.91–1.16), n = 18,415] and in participants having a self-reported positive PCR test compared to those who reported not having had a prior infection [OR: 0.97 (95% CI: 0.79–1.19), n = 18,985] (Fig. 1).
Odds of wearing face masks on mandatory plus other occasions compared to only when mandatory were 28% increased [OR: 1.28 (95% CI: 1.08–1.51), n = 19,353] in the vaccinated, and increased by 13% in participants having a self-reported positive PCR test compared to the reference group [OR: 1.13 (95% CI: 0.83–1.54), n = 19,927] (Fig. 1).
Association of PPM with serostatus of SARS-CoV-2
Investigating the effect of PPM on serostatus in the unvaccinated, we adjusted for age, education, gender, household size, occupation, pre-existing medical condition, and smoking (Supplement Fig. 3). For the adjustment set, we identified the grade of restrictions in Germany over the course of the pandemic as causing confounding and therefore used the Health and Containment Index to account for it [24, 25].
Among the unvaccinated MuSPAD participants, the odds of being seropositive were reduced by 22% and 16%, respectively in the group that partly [OR: 0.78 (95% CI: 0.56–1.09), n = 15,228] and completely adhered to physical distancing [OR: 0.84 (95% CI: 0.59–1.20), n = 15,228] compared to non-compliance (Fig. 2).
The odds of being seropositive were similar in the group that partly [OR: 1.03 (95% CI: 0.31–3.43), n = 15,228] and completely [OR: 0.97 (95% CI: 0.29–3.22), n = 15,228] adhered to adequate hand cleaning, compared to the group reporting no compliance with hand cleaning (Fig. 2).
The odds of being seropositive in the unvaccinated participants were decreased by 9% [OR: 0.91 (95% CI: 0.71–1.16), n = 15,228] when wearing face masks on mandatory plus other occasions compared to those reporting wearing face masks only on mandatory occasions (Fig. 2).
Discussion
Among MuSPAD participants in Germany the adherence to personal protection measures was rather high. Participants who were vaccinated against SARS-CoV-2 were older and had the highest compliance with physical distancing as well as hand cleaning. Those participants without an immune response against SARS-CoV-2 showed the highest percentage of additional face mask wearing. Our data indicated that self-reported positive SARS-CoV-2 PCR test since the onset of the pandemic or vaccination against SARS-CoV-2 decreased the odds of adhering more strictly to hand cleaning and physical distancing, but increased the odds of wearing face masks on mandatory occasions. In addition, we found that among unvaccinated participants, a higher adherence to PPM reduced the odds of being seropositive for SARS-CoV-2.
Overall, a high adherence to hand cleaning (67%) and additional face mask wearing (87%) was reported by the study population. In contrast, MuSPAD participants complied more partially (63%) with physical distancing. A high acceptance of PPM was also reported from an online survey (N = 9,796) conducted in March 2020 in various countries [26]. Researchers concluded that the prevention measures implemented by the government, for example avoiding gatherings, closure of public places, and hand hygiene were accepted by 95.0%–99.7% of the respondents [26].
Previous research has shown that being female, of older age, part of a risk group, suffering from impaired physical and mental health, having a positive perception of government communications, and mostly a higher socio-economic status were characteristics positively associated with acceptance of PPM [27,28,29,30]. In our study, we found that vaccinated participants were older and showed the highest compliance with hand cleaning and physical distancing. Further, we found that a known serostatus of antibodies against SARS-CoV-2 due to a self-reported positive PCR test or vaccination might be associated with adherence to PPM. The odds of not adhering to physical distancing were generally increased in vaccinated participants compared to those unvaccinated or not having a positive PCR test. A Study has shown that moods, such as anxiety, can enhance preventive behavior toward a SARS-CoV-2 infection [31]. Thus, a known protection with antibodies against SARS-CoV-2 could improve individuals’ moods and conversely affect compliance with PPM. Moods were not investigated in our analysis, but can be an unobserved factor, which needs to be considered in future studies.
We found that vaccinated participants and those with a known prior infection had increased odds of compliance regarding additional face mask wearing. In both exposures the odds were increased (vaccinated: OR: 1.28; self-reported positive PCR test OR: 1.13).
The extent to which PPM behavior was associated with SARS-CoV-2 seropositivity among unvaccinated MuSPAD participants was subject of the second research question. Results indicated that keeping physical distancing, hand cleaning, and wearing face masks on mandatory occasions decreased the odds of being identified as seropositive. Point estimates of the exposures of physical distancing (adhering partly OR: 0.78; adhering completely: OR: 0.84), hand cleaning (adhering partly: OR: 1.03; adhering completely: OR: 0.97), and additional face mask wearing (OR: 0.91) on seropositivity were shown to be protective. Other studies confirmed that PPM reduced the transmissions of SARS-CoV-2 [32,33,34]. A systematic review of 25,697 participants showed that the transmission of SARS-CoV-2 was reduced when keeping physical distance of more than 1 m [pooled adjusted OR 0.18 (95% CI: 0.09–0.38)]. Wearing face masks in addition to appropriate physical distancing can reduce SARS-CoV-2 infection by up to 85% [OR: 0.15 (95% CI: 0.07–0.34)], with a difference between respirators and disposable surgical or similar masks [33].
Strengths and limitations
This study provided a presentation of the behavioral patterns of MuSPAD participants across Germany, based on a population level, rather than focusing only on hotspots. Data collection allowed depicting PPM adherence across Germany and at different times. Another strength was the measurement of SARS-CoV-2 serostatus using multiplex immunoassay to distinguish between vaccinated, recovered, and individuals without antibodies against SARS-CoV-2. Compared with commercial assays, this test already demonstrated its improved sensitivity [16] in comparison to case identification based on (self-reported) PCR tests used in previous studies [8]. To capture relevant confounding, adjustment sets were derived from expertise, visualized with DAGs, and evaluated jointly in the research group.
Due to the sequential cross-sectional nature of the MuSPAD, the temporal sequence of the relationship between exposure and outcome is uncertain. In addition, response bias due to self-report questionnaires may result in overestimation [35]. Due to mandatory mask wearing, social desirability is an important factor that may influence our estimates [36], too. The Health and Containment Index to control for restrictions in Germany [25] was only available on a country and not on a communal level, limiting the accuracy of adjustment.
Another aspect that needs to be discussed is that the large overall sample size of our study may result in confidence intervals being very narrow, suggesting high precision in the effect estimates, resulting in more statistically significant findings. Therefore, in the interpretation of our findings we focused on precision estimated based on confidence intervals.
In addition, we would like to point out that for each outcome and exposure, a specific regression model was built to adequately control for confounding factors for each research question. Therefore, there is a possibility that some of our results are false positives due to multiple testing. In our questionnaire, compliance was measured in three categories (“No, not at all,” “Yes, partly,” “Yes, completely”). Therefore misclassification might have occurred, as adherence to PPM could not be captured accurately and thus differences between individuals could not be validly measured. In our categorization of vaccinated and infected due to serological status we did not account for those who were both, which potentially overestimated the association between personal protective measures and infections according to serological status. However for the time period assessed here this misclassification cannot be large as the proportion of those infected before vaccination was small.
Conclusion
A prior known infection of SARS-CoV-2 confirmed with a positive PCR test and vaccination against SARS-CoV-2 may have influenced compliance with certain PPM behaviors during the pandemic in Germany. Furthermore, similar to previous research, we confirmed that compliance to PPM can reduce the odds of SARS-CoV-2 seropositivity in unvaccinated participants.
Availability of data and materials
The anonymized data for this study will be made available to other academic researchers. To request additional data or information from this study, please contact the author Manuela Harries (Manule.Harries@helmholtz-hzi.de). Institutions can apply for the data via serohub@helmholtz-hzi.de. Regarding data from the NAKO study Hannover researchers have the opportunity to apply for data usage in accordance with the official regulations and specifications. For more detailed information, please visit https://transfer.nako.de.
Change history
23 February 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12889-024-18125-5
Abbreviations
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- DAG:
-
Directed acyclic graph
- ECDC:
-
European Centre for Disease Prevention and Control
- HUB:
-
Hannover Unified Biobank
- HZI:
-
Helmholtz Centre for Infection Research
- MultiCoV-Ab:
-
Multiplex immunoassay
- MuSPAD:
-
Multilocal and Serial Prevalence Study of Antibodies to SARS-2 coronavirus in Germany
- NC:
-
Nucleocapsid
- NMI:
-
Natural and Medical Sciences Institute at the University of Tübingen
- OR:
-
Odds ratio
- PCR:
-
Polymerase chain reaction
- PPM:
-
Personal protection measures
- RBD:
-
Receptor-binding domain
- RKI:
-
Robert Koch Institute
- RNA:
-
Ribonucleic acid
- S:
-
Spike protein
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- WHO:
-
World Health Organization
References
Böhmer MM, Buchholz U, Corman VM, Hoch M, Katz K, Marosevic DV, et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: a case series. Lancet Infect Dis. 2020;20(8):920–8.
Gornyk D, Harries M, Glöckner S, Strengert M, Kerrinnes T, Heise JK, et al. SARS-CoV-2 seroprevalence in Germany. Dtsch Arztebl Int. 2021;118(48):824–31.
Centers for Disease Control and Prevention (CDC). SARS-CoV-2 is transmitted by exposure to infectious respiratory fluids 2021 [cited 2021 10/06]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html.
World Health Organization (WHO). Advice for the public: Coronavirus disease (COVID-19) 2021 [cited 2021 10/07]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
Hansen S, Schäfer N, Kaspar R. Wahrgenommene Auswirkungen der Coronapandemie auf die Lebenssituation älterer Menschen. (D80+ Kurzberichte, 1). 2021 [cited 2022 04/07]. Available from: https://nbn-resolving.org/urn:nbn:de:0168-ssoar-75927-0.
Bundesgesundheitsministeriums. Coronavirus-Pandemie: Was geschah wann? Chronik aller Entwicklungen im Kampf gegen COVID-19 (Coronavirus SARS-CoV-2) und der dazugehörigen Maßnahmen des Bundesgesundheitsministeriums 2022 [Available from: https://www.bundesgesundheitsministerium.de/coronavirus/chronik-coronavirus.html.
Robert Koch-Institut (RKI). Digitales Impfqoutenmonitoring zur COVID-19-Impfung 2021 [cited 2022 04/02]. Available from: https://impfdashboard.de/.
Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-control study of use of personal protective measures and risk for SARS-CoV 2 infection. Thailand Emerg Infect Dis. 2020;26(11):2607–16.
Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ (Clinical research ed). 2021;375:e068302.
Aleta A, Martín-Corral D, Pastore YPA, Ajelli M, Litvinova M, Chinazzi M, et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat Hum Behav. 2020;4(9):964–71.
Mitze T, Kosfeld R, Rode J, Wälde K. Face masks considerably reduce COVID-19 cases in Germany. Proc Natl Acad Sci USA. 2020;117(51):32293–301.
Heinsohn T, Lange B, Vanella P, Rodiah I, Glöckner S, Joachim A, et al. Infection and transmission risks of COVID-19 in schools and their contribution to population infections in Germany: a retrospective observational study using nationwide and regional health and education agency notification data. PLoS Med. 2022;19(12):e1003913.
Baxter A, Oruc BE, Asplund J, Keskinocak P, Serban N. Evaluating scenarios for school reopening under COVID19. BMC Public Health. 2022;22(1):496.
World Health Organization (WHO). Population-based age-stratified seroepidemiological investigation protocol for coronavirus 2019 (COVID-19) infection 2020 [cited 2021 10/08]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Seroepidemiology-2020.2.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Becker M, Strengert M, Junker D, Kaiser PD, Kerrinnes T, Traenkle B, et al. Exploring beyond clinical routine SARS-CoV-2 serology using MultiCoV-Ab to evaluate endemic coronavirus cross-reactivity. Nat Commun. 2021;12(1):1152.
European Centre for Disease Prevention and Control (ECDC). Guidelines for the use of non-pharmaceutical measures to delay and mitigate the impact of 2019-nCoV. 2020:10.
Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ‘dagitty.’ Int J Epidemiol. 2016;45(6):1887–94.
R-Core-Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; 2021 [Available from: https://www.R-project.org/.
Sjoberg DD, Whiting K, Curry M, Lavery JA, Larmarange JJRJ. Reproducible summary tables with the gtsummary package. 2021;13(1).
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48.
Wickham H, Averick M, Bryan J, Chang W, McGowan L, François R, et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4:1686.
Hoffmann W, Latza U, Baumeister SE, Brünger M, Buttmann-Schweiger N, Hardt J, et al. Guidelines and recommendations for ensuring Good Epidemiological Practice (GEP): a guideline developed by the German Society for Epidemiology. Eur J Epidemiol. 2019;34(3):301–17.
Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. 2021;5(4):529–38.
Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus pandemic (COVID-19): OurWorldInData.org; 2020 [cited 2022 01/07]. Available from: https://ourworldindata.org/coronavirus.
Meier K, Glatz T, Guijt MC, Piccininni M, van der Meulen M, Atmar K, et al. Public perspectives on protective measures during the COVID-19 pandemic in the Netherlands, Germany and Italy: a survey study. PLoS ONE. 2020;15(8):e0236917.
Margraf J, Brailovskaia J, Schneider S. Behavioral measures to fight COVID-19: an 8-country study of perceived usefulness, adherence and their predictors. PLoS ONE. 2020;15(12):e0243523.
Varghese NE, Sabat I, Neumann-Böhme S, Schreyögg J, Stargardt T, Torbica A, et al. Risk communication during COVID-19: a descriptive study on familiarity with, adherence to and trust in the WHO preventive measures. PLoS ONE. 2021;16(4):e0250872.
van Loenhout JAF, Vanderplanken K, Van den Broucke S, Aujoulat I. COVID-19 measures in Belgium: how perception and adherence of the general population differ between time periods. BMC Public Health. 2022;22(1):245.
Lüdecke D, von dem Knesebeck O. Protective behavior in course of the COVID-19 outbreak-survey results from Germany. Front Public Health. 2020;8:572561.
Velikonja NK, Erjavec K, Verdenik I, Hussein M, Velikonja VG. Association between preventive behaviour and anxiety at the start of the COVID-19 pandemic in Slovenia. Zdravstveno varstvo. 2020;60(1):17–24.
Leung NHL, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, Hau BJP, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26(5):676–80.
Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet (London, England). 2020;395(10242):1973–87.
Ingram C, Downey V, Roe M, Chen Y, Archibald M, Kallas KA, et al. COVID-19 prevention and control measures in workplace settings: a rapid review and meta-analysis. Int J Environ Res Public Health. 2021;18(15):7847.
Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5(1):56.
Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res. 2011;2(4):320–32.
Acknowledgements
We would like to express our sincere thanks to the counties and urban districts for supporting our study and their good cooperation. In addition, we thank our former colleague Barbora Kessel for answering data quality questions and concerns. We appreciate the work of our colleagues at the Natural and Medical Sciences Institute at the University of Tübingen (NMI) for analyzing the samples using the muliplex assay. Our deepest gratitude goes to all participants who donated their blood and time.
List of consortium: MuSPAD Team
Representative: Berit Lange.1
– Dr. rer. nat. Monika Strengert.1
– Dr. med. Stefanie Castell.1
– Jana-Kirstin Heise.1
– Dr. rer. nat. Pilar Hernandez.1
– Daniela Gornyk PhD.1
– Monike Schlüter.1
– Dr. rer. nat. Tobias Kerrines.5
– Dr. rer.nat. Nicole Schneiderhan-Marra.6
– Dr. rer.nat. Alex Dulovic.6
– Dr. med. Gerhard Bojara.7
– Kerstin Frank.8
– Dr. rer. nat. Knut Gubbe.8
– Prof. Dr. med. Torsten Tonn.8
– Dr. med. Oliver Kappert.9
– Prof. Dr. med. Winfried V. Kern.10
– Prof. Dr. rer. nat. Thomas Illig.11
– Dr. rer. nat. Norman Klopp.11
– Dr. med. Gottfried Roller.12
– Dr. phil. Michael Ziemons.13
– Dr. med. Gottfried Rolle.14
1Helmholtz Center for Infection Research, Department of Epidemiology, Braunschweig
5Helmholtz – Institute for RNA-based Infection Research
6Natural and Medical Sciences Institute at the University of Tübingen, Reutlingen, Germany (NMI)
7Public Health Office for the District and City of Osnabrück
8German Red Cross Blood Donation Service North-East gGmbH, Institute of Transfusion Medicine and Immunohematology, Dresden and Plauen
9Department of Health and Care Services, Breisgau-Hochschwarzwald District Office, Freiburg im Breisgau
10Department of Infectious Diseases, Internal Medicine II, University Hospital Freiburg, and Faculty of Medicine, University of Freiburg
11Hanover Unified Biobank (HUB), Hanover School of Medicine (MHH), Clinical Research Center Hanover
12District Health Office Reutlingen
13Department of Social Affairs, Health, and Digitalization, Aachen City Region
14Baden-Wuerttemberg State Health Office, Stuttgart
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Helmholtz Association, the European Union's Horizon 2020 research and innovation program (grant number 101003480) and by internal HZI funds. The Serohub to establish a repository for sharing data from seroprevalence studies for SARS-CoV-2 (www.serohub.net) was supported by the German Center for Infection Research (DZIF) and the Network for University Medicine (NUM).
This research project partially used data from the German National Cohort (NAKO) study site Hannover (www.nako.de). The Federal Ministry of Education and Research (BMBF), the federal states, and the Helmholtz Association, with additional financial support from participating universities and Leibniz Association institutes, funded the NAKO (project funding reference numbers: 01ER1301A/B/C and 01ER1511D).
Author information
Authors and Affiliations
Consortia
Contributions
A.A. (Aigner, A.); M.H. (Harries, M.); B.L. (Lange, B.); O.J. (Ortmann, J.); M.T. (MuSPAD Team); R.K. (Kettlitz, R.); G.K. (Krause, G.). Collaborations: M.T. Conceptualization: B.L. A.A; Data quality: R.K., J.O., M.H.; Formal analyses: R.K., A.A., Visualization: R.K., M.H.; Project administration: M.H.; Writing-original draft: R.K., M.H., A.A, B.L; Funding acquisition: B.L., G.K. Writing-review & editing: R.K., M.H., B.L. A.A; All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
MuSPAD complies with all relevant laws and declarations – EU Charter of Fundamental Rights, Biomedical Convention of the Council of Europe and additional protocols, the Council for International Organizations of Medical Sciences guidelines, and the Helsinki Declaration. Ethical approval was obtained on June 21, 2020 by the Ethics Committee of the Hannover Medical School (No 9086_BO_S_2020) and ethics committees for NAKO (Bavarian Medical Association “Bayerische Landesärztekammer” (13023, 13031) and Medical Association of Lower Saxony “Ärztekammer Niedersachen” (Grae/067/2013)). Furthermore, the study complies with the requirements of the General Data Protection Regulation and the Federal Data Protection Act and Recommendations for Ensuring Good Epidemiological Practice of the German Society for Epidemiology e.V. [23].
Prior to study participation, all participants provided signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been updated to correct the references.
Supplementary Information
Additional file 1.
DAG - variable Selection of adjustment set. Data preparation regression models. Regional distribution of study sample. Self-reported vaccination status and self-reported result of PCR test and by serostatus.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kettlitz, R., Harries, M., Ortmann, J. et al. Association of known SARS-CoV-2 serostatus and adherence to personal protection measures and the impact of personal protective measures on seropositivity in a population-based cross-sectional study (MuSPAD) in Germany. BMC Public Health 23, 2281 (2023). https://doi.org/10.1186/s12889-023-17121-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17121-5