Abstract
Background
This report describes two L. monocytogenes outbreak investigations that occurred in March and September of 2018 and that linked illness to a food premises located in an Ontario cancer centre. The cancer centre serves patients from across the province.
Methods
In Ontario, local public health agencies follow up with all reported laboratory-confirmed cases of listeriosis to identify possible sources of disease acquisition and to carry out investigations, including at suspected food premises. The Canadian Food Inspection Agency (CFIA) is notified of any Listeria-positive food product collected in relation to a case. The CFIA traces Listeria-positive product through the food distribution system to identify the contamination source and ensure the implicated manufacturing facility implements corrective measures.
Results
Outbreaks one and two each involved three outbreak-confirmed listeriosis cases. All six cases were considered genetically related by whole genome sequencing (WGS). In both outbreaks, outbreak-confirmed cases reported consuming meals at a food premises located in a cancer centre (food premises A) before illness onset. Various open deli meat samples and, in outbreak two, environmental swabs (primarily from the meat slicer) collected from food premises A were genetically related to the outbreak-confirmed cases. Food premises A closed as a result of the investigations.
Conclusions
When procuring on-site food premises, healthcare facilities and institutions serving individuals with immuno-compromising conditions should consider the potential health risk of foods available to their patient population.
Similar content being viewed by others
Background
Listeriosis is a bacterial infection caused by the pathogen Listeria monocytogenes. In healthy individuals, infection with L. monocytogenes is typically asymptomatic or a mild, self-limited illness such as febrile gastroenteritis. However, listeriosis in individuals with immuno-compromising conditions can result in severe or potentially fatal illness, including septicemia or meningitis. Pregnant women are at increased risk for Listeria infections which can result in stillbirth or miscarriage [1]. Disease surveillance data from Ontario, Canada, from 2011 to 2019 indicates approximately 62 individuals (0.40 cases per 100,000 population) are reported with listeriosis yearly [2]. Further, the proportion of reported cases with severe outcomes is high. Based on data from 2019, 75.3% of Ontario cases were reported as hospitalized and a fatal outcome was reported for 19.2% of cases [2].
L. monocytogenes is primarily acquired through consuming contaminated food. Internationally, outbreaks have been linked to ready-to-eat meats, soft cheese, and other dairy products [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Additional sources of L. monocytogenes outbreaks have also been identified, including whole apples, smoked fish, ready-to-eat salads, and cantaloupes [23,24,25,26,27]. Also, in 2015-16, an outbreak confined to Ontario, which resulted in 34 cases and 4 deaths, was attributed to pasteurized chocolate milk [28].
Listeriosis outbreaks affecting institutions, such as hospitals and long-term care homes, have also been described. In 2008, a large Canadian outbreak involving 57 laboratory-confirmed cases and 24 deaths, mainly from Ontario, was linked to ready-to-eat deli meats purchased primarily by institutions [29]. Similarly, in Denmark an outbreak was linked to spiced meat rolls served in hospitals and long-term care homes [30]. Hospital-acquired outbreaks have also been linked to soft cheese, diced celery, and pasteurized ice cream mix [31,32,33,34]. In particular, several hospital outbreaks in the United Kingdom were associated with pre-made sandwiches with mixed fillings [35,36,37]. The sandwiches were produced off-site in these outbreaks and contaminated at the production facilities.
This report aims to describe two L. monocytogenes outbreak investigations that linked illness to a food premises located in a cancer centre in Ontario (food premises A). The on-site food premises was open to the public and the in- and out-patient population seeking medical care at the cancer centre. The report will highlight issues raised from the investigations, including policy considerations for healthcare facilities and institutions, particularly those serving individuals with immuno-compromising conditions, about the type of food premises permitted on-site.
Methods
Listeria surveillance and outbreak investigations
Laboratories and health care providers in Ontario are required under provincial legislation to report laboratory-confirmed and clinical cases of designated diseases of public health significance, including listeriosis. Laboratory-confirmed cases of listeriosis are considered invasive as confirmation requires the isolation of L. monocytogenes from a normally sterile site (e.g., blood). Cases are reported through the Ontario Ministry of Health (MOH) integrated Public Health Information System (iPHIS), the reportable disease database for the province, and monitored provincially by Public Health Ontario (PHO) for surveillance and outbreak detection. When a multi-jurisdictional outbreak (i.e., an outbreak involving two or more local public health units) within Ontario is detected, PHO leads the investigation. Local public health officials routinely follow up with reported cases of listeriosis using a national standardized questionnaire to identify possible sources of disease acquisition and to conduct case management. Details collected during routine follow up include cases’ food histories and food premises at which the case dined four weeks prior to illness onset. Food premises reported by cases are typically investigated and, if warranted, samples of suspect food items consumed by the case and environmental swabs are collected. Food samples and environmental swabs are tested at the PHO Laboratory, Ontario’s public health reference laboratory.
The Canadian Food Inspection Agency (CFIA) is notified of any Listeria-positive food product collected by local public health officials in relation to a case of listeriosis. Following notification of a Listeria-positive food product, the CFIA conducts a food safety investigation. The CFIA traces back Listeria-positive food through the distribution system to manufacturing facilities, reviews records and processes at facilities, and conducts representative sampling and analysis of intact food units (i.e., closed samples) and environmental swabbing to determine a possible source and the extent of environmental contamination. CFIA also traces the implicated food product forward to determine if a product that poses a health risk to Canadians is available on the market. Risk mitigating action may be requested whereby the responsible regulated party conducts a recall and withdraws the affected product from the market. Following a recall, the CFIA verifies its effectiveness, requests that the firm identify the cause of the contamination, and ensures that corrective actions are implemented to prevent similar issues from occurring in the future.
Outbreak case definitions
The first outbreak was declared in March 2018, and a confirmed case was defined as a resident or visitor to Ontario with laboratory confirmation of L. monocytogenes with the PulseNet Canada whole genome sequencing (WGS) cluster code 1803LMWGS-1ON and symptom onset on or after 1 January 2018. An outbreak-probable case was defined as a resident or visitor to Ontario with laboratory confirmation of L. monocytogenes with an epidemiological link to food premises A and symptom onset on or after 1 January 2018. For the second outbreak, which was declared in September 2018, a confirmed case was defined as a resident or visitor to Ontario with laboratory confirmation of L. monocytogenes with the PulseNet Canada WGS cluster code 1810LMWGS-1ON and symptom onset on or after 15 August 2018. An outbreak-probable case was defined as a resident or visitor to Ontario with laboratory confirmation of L. monocytogenes with an epidemiological link to food premises A and symptom onset on or after 15 August 2018.
PHO laboratory testing methods
Clinical isolates of L. monocytogenes identified in hospital and private laboratories are submitted to the PHO Laboratory for molecular subtyping and surveillance purposes. Food samples and environmental swabs collected by public health unit officials in relation to a L. monocytogenes clinical case are also submitted to the PHO Laboratory, and testing is performed according to the Health Canada method MFHPB-30 [38]. During the outbreak investigations molecular subtyping by both pulsed field gel electrophoresis (PFGE) and WGS was performed in accordance with PulseNet Canada standard operating procedures; both methods were used as the PHO Laboratory was transitioning methods during this time. During the first outbreak, PFGE was performed for the clinical, food and environmental L. monocytogenes isolates at the PHO Laboratory and WGS was performed at the National Microbiology Laboratory (NML) in Winnipeg, Manitoba, Canada. PFGE and WGS for the second outbreak were both performed at the PHO Laboratory. Comparisons were generated using BioNumerics version 7.6 and nodes were calculated using UPGMA (Unweighted Pair Group Method with Arithmetic Mean), which is the standard analytical process for PulseNet Canada laboratories. Comparative analysis of WGS results from both outbreaks one and two were performed by the NML.
CFIA laboratory testing methods
Food samples from retail and production facilities collected for testing by the CFIA were analyzed at CFIA laboratories according to Health Canada methods MFLP-28 and MFHPB-30, and environmental samples from production facilities were analyzed according to methods MFLP-15 and MFHPB-30 [38]. L. monocytogenes positive food samples were enumerated according to the Health Canada method MFLP-74 [38]. Molecular subtyping by both PFGE and WGS for the food and environmental L. monocytogenes isolates was performed at CFIA laboratories in accordance with PulseNet Canada standard operating procedures.
Results
Outbreak One
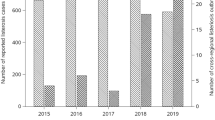
In early March 2018, local public health officials received a report of a laboratory-confirmed case of L. monocytogenes. During routine case follow-up, it was determined that the case was receiving cancer treatment at an Ontario cancer centre and had consumed a meal at food premises A during their incubation period (i.e., the four weeks before illness onset). Food premises A was part of a chain of restaurants with locations throughout Ontario, one of which was in the cancer centre. As food premises reported by any confirmed listeriosis case during their incubation period are typically investigated, control samples of menu items consumed by the case were collected for testing. Seven days later, local public health officials were notified that the control sample of sliced corned beef collected from food premises A was presumptive positive for Listeria (Fig. 1). Four days following the presumptive positive finding, the open control sample of corned beef was confirmed to be a PFGE-match to the case and food premises A was closed on the same day. The public health unit in whose jurisdiction food premises A was located issued a media release to inform the public of the investigation; as well, targeted communications were sent to health care providers to assist with prompt diagnosis and treatment of cases. PHO also issued a communication to all public health units in Ontario requesting they share information about the outbreak with health care providers in their jurisdiction.
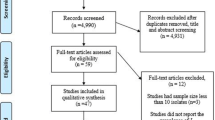
A total of four laboratory-confirmed (three outbreak-confirmed and one outbreak-probable) cases from three different public health units in southern Ontario were included in the investigation. The three outbreak-confirmed cases were considered genetically related by WGS (within 0 to 10 alleles; Table 1; Fig. 2) and symptom onset ranged from mid-January to mid-March 2018. All three outbreak-confirmed cases were cancer patients receiving treatment at the cancer centre and were hospitalized due to listeriosis, and no deaths were reported during the course of the investigation. All three outbreak-confirmed cases reported consuming sandwiches at food premises A during their incubation period. The outbreak-probable case was a cancer patient with a symptom onset in late March but was not considered genetically related to the outbreak-confirmed cases by WGS (over 200 alleles different). The proxy for the outbreak-probable case reported that the case consumed meals at food premises A, however, further details could not be confirmed.
Local public health officials collected 14 open control samples of various types of deli meat that had been sliced on-site at food premises A and 42 environmental swabs from the food premises. A total of five different open deli meat samples (a sample of roast beef, salami, and black forest ham, and two samples of corned beef) tested positive for L. monocytogenes and all L. monocytogenes isolates were genetically related to the outbreak-confirmed cases by WGS (within 0 to 10 alleles) (Table 2). L. monocytogenes was not detected in any environmental swabs, including swabs from the slicer, however, the environmental swabs were taken from the slicer following supervised cleaning and sanitization. Despite this, the slicer was a suspect source of cross-contamination as all the positive open samples had been sliced on-site with the same slicer and it was determined that the slicer was not being routinely dismantled, cleaned, and sanitized as required per the manufacturer’s specifications.
The CFIA conducted a traceback of the five different L. monocytogenes-positive open deli meat samples from food premises A. Two different manufacturing facilities were identified, however the manufacturing facility for one of the L. monocytogenes-positive open samples (black forest ham) could not be determined due to a lack of packaging details. The CFIA collected and tested a roast beef sample and a corned beef sample still intact in the original packaging from the same lots of product as the L. monocytogenes-positive open samples. Closed samples of the other deli meat products (salami, black forest ham, and the other lot of corned beef) from the same lots as the L. monocytogenes-positive open samples were either no longer available or could not be identified due to lack of packaging details. L. monocytogenes was not detected in the closed corned beef sample tested, but was detected in the closed roast beef sample. Additional lots of closed roast beef products were also tested and environmental swabs were taken from the associated production line at manufacturing facility Y. L. monocytogenes was detected in additional lots of product and on the associated production line (slicer and cooler/snap chiller). As a result of these findings, production on the affected line stopped. Several voluntary product recalls and public warnings were issued, the first of which occurred in late March 2018 and continued until all potentially affected product within shelf life was recalled in mid-April 2018.
Multiple strains of L. monocytogenes (both within a sample and across samples) were identified by WGS in the closed roast beef samples and environmental swabs collected at manufacturing facility Y. However, none of the L. monocytogenes isolates detected in the closed roast beef samples or environmental swabs from the facility were genetically related by WGS to the open samples from food premises A, outbreak cases, or other confirmed cases of listeriosis. Further, enumeration results indicated very low levels of Listeria contamination (< 5 CFU/g) in the closed roast beef samples, which were tested towards the end of their shelf life. After implementing corrective measures, the manufacturing facility resumed operations at the end of April 2018. Food premises A re-opened in late March after all food safety requirements were met, including more frequent slicer cleaning and sanitization (deep cleaning every four hours), staff education on Listeria, re-training of staff on slicer cleaning and sanitizing procedures, and 15 Listeria-negative environmental swabs (including swabs from the slicer).
Outbreak two
Towards the end of September 2018 public health officials were notified of a L. monocytogenes laboratory-confirmed case who reported consuming a meal during their incubation period at food premises A (Fig. 1). Five days later laboratory results indicated the case had the same first enzyme PFGE pattern as the outbreak-confirmed cases from the first outbreak. Local public health officials collected open food samples and environmental swabs from food premises A. Food premises A was closed following Listeria presumptive positive results from the open food samples and environmental swabs. The closure occurred one day after the case was identified as having the same first enzyme PFGE pattern as the first outbreak.
A total of three outbreak-confirmed cases from three different public health units in southern Ontario were included in the investigation. All three outbreak-confirmed cases were considered genetically related by WGS and were also genetically related to outbreak-confirmed cases from the first investigation (within 0 to 10 alleles) (Table 1; Fig. 2). Symptom onset dates ranged from late August to mid-September 2018. All three cases were cancer patients hospitalized as a result of listeriosis. No deaths were reported during the course of the investigation. All three outbreak-confirmed cases reported consuming meals at food premises A during their incubation period. No outbreak-probable cases were identified. Similar to the first investigation, the public health unit in whose jurisdiction food premises A was located issued a public media release and a communication to health care providers. PHO also issued a communication to all public health units in Ontario requesting they share information about the outbreak with health care providers in their jurisdiction.
Local public health officials collected 12 open control food samples and 92 environmental swabs from food premises A. Seven food samples (all various types of deli meat that had been sliced using the on-site slicer) and eight environmental swabs were positive for Listeria and were genetically related to the outbreak-confirmed cases by WGS (Table 2). All but one of the L. monocytogenes-positive environmental swabs were collected from the slicer – the same slicer that was the suspect source of cross-contamination in the first outbreak. Public health officials permanently removed the slicer from use at food premises A. Food premises A closed due to the investigations.
The same facility as in the previous investigation, manufacturing facility Y, was identified as the L. monocytogenes-positive open deli meat manufacturer. As no product labels were available from the Listeria monocytogenes positive open product, traceback activities identified what was likely the same lots of product. Closed samples were collected and tested from those lots. Listeria was not detected in any of the closed deli meat samples tested. Further, manufacturing facility Y and the CFIA did not report any Listeria positive samples during the routine product or environmental testing in the previous three months, which had been scaled up as a result of the first outbreak. No corrective action was required at manufacturing facility Y.
Discussion
The report describes two L. monocytogenes outbreaks that occurred within six months and were linked to the same on-site food premises in an Ontario cancer centre. The centre serves a large in- and out-patient population from across Ontario who visit the centre for medical care. During the outbreaks, the on-site food premises was open to the public and the cancer centre in- and out-patient populations.
Environmental swab results identified the slicer at food premises A as a source of cross-contamination in the second outbreak, and the slicer was the suspected source in the first outbreak. Slicers are known to be a source of growth of Listeria that can result in cross-contamination in food premises, as these devices can harbour bacteria (particularly if damaged). Food premises operators must adhere to cleaning and sanitizing requirements to reduce the risk of contamination [39]. Before the first outbreak, proper slicer cleaning and sanitation procedures were not followed. Despite corrective measures, the slicer design did not allow for complete disassembly which likely precluded adequate cleaning and sanitizing. This likely led to the re-emergence of the same genetic strain months later causing the second outbreak. As a result of the two Ontario outbreaks, food premises A in the cancer centre closed.
Listeria has been known to persist in the environment for years, particularly on food equipment surfaces that cannot be adequately cleaned and sanitized, leading to foodborne illness outbreaks [40]. Two listeriosis outbreaks in a hospital setting in the United States (US) similarly highlighted the challenge of cleaning and sanitizing inaccessible food contact surfaces, and the environmental persistence of L. monocytogenes [33, 34]. These US outbreaks were linked to milkshakes produced in a commercial-grade freezer machine that remained contaminated following the first outbreak, despite repeated cleaning and sanitization, causing a second outbreak of the same strain of L. monocytogenes a year later.
The source of the introduction of Listeria contamination at food premises A was not determined. Multiple genetic strains of L. monocytogenes were identified in closed deli meat samples, and in the environment of the associated production line at manufacturing facility Y. Studies elsewhere have also reported multiple L. monocytogenes isolates at production facilities [30, 41]. However, the same genetic outbreak strain found in the laboratory-confirmed cases as well as at food premises A was not identified at manufacturing facility Y. Further, in the first outbreak, closed samples of the Listeria positive salami (produced at another manufacturing facility) and black forest ham (where the manufacturing facility could not be determined) could not be obtained to determine if they were contaminated with the outbreak strain.
Conclusions
Similar to recommendations raised in outbreaks investigations elsewhere, the two outbreak investigations raised a number of considerations for health care facilities and institutions serving individuals with immuno-compromising conditions [33,34,35]. Health care facilities and institutions should consider the potential health risk of foods available to their patient population when procuring on-site food premises. This may require policies promoting greater collaboration between medical and administrative branches of health care facilities in the procurement process for on-site food premises. During the two Ontario investigations, additional health care facilities and institutions in Ontario were identified with on-site premises (including other locations belonging to the same chain as food premises A) that served foods known to be high-risk for those with immuno-compromising conditions. Excluding high risk foods from being served in settings that care for patients with immuno-compromising conditions may reduce the risk of listeriosis for these patients.
Counselling provided by health care providers to patients at increased risk for listeriosis (those with immuno-compromising conditions, pregnant women and the elderly) regarding the health risks associated with foods that are more likely to be contaminated with Listeria is an important preventive measure [31, 35, 36]. However, patients may not necessarily adhere to clinical advice. Out-patients who would not have meals prepared by a medical care centre may be more likely to visit on-site food premises. In the two outbreak investigations described in this paper, a number of the outbreak-confirmed cases were out-patients seeking treatment at the cancer centre. To further reduce the risk to these individuals, it is recommended that high risk foods not be served in settings that care for patients at increased risk for listeriosis. Further, recognizing that those at increased risk for listeriosis consume and purchase high risk foods from many food premises in the community, signage at these premises to alert these individuals of the risk of Listeria infection associated with these foods could also be considered. In addition, food handlers at any food premises with an onsite slicer should be appropriately educated on proper cleaning and sanitizing techniques and on the importance of frequent slicer cleaning [42]. Routine public health inspections of food premises should monitor and re-enforce proper cleaning and sanitizing of slicers.
Data Availability
Case data is closed, and reported in the Ontario Ministry of Health’s integrated Public Health Information System (iPHIS). Public Health Ontario (PHO) cannot disclose the underlying data. Doing so would compromise individual privacy contrary to PHO’s ethical and legal obligations. Restricted access to the data may be available under conditions prescribed by the Ontario Personal Health Information Protection Act, 2004, the Ontario Freedom of Information and Protection of Privacy Act, the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans (TCPS 2 (2018)), and PHO privacy and ethics policies. Data are available for researchers who meet PHO’s criteria for access to confidential data. Information about PHO’s data access request process is available on-line at https://www.publichealthontario.ca/en/data-and-analysis/using-data/data-requests.
The whole genome sequencing datasets generated during and/or analyzed during the current study are available in the National Centre for Biotechnology Information repository within BioProject PRJNA563085, https://www.ncbi.nlm.nih.gov/.
Abbreviations
- MOH:
-
Ontario Ministry of Health
- iPHIS:
-
Integrated Public Health Information System
- PHO:
-
Public Health Ontario
- CFIA:
-
Canadian Food Inspection Agency
- WGS:
-
Whole genome sequencing
- PFGE:
-
Pulsed field gel electrophoresis
- NML:
-
National Microbiology Laboratory
References
De Noordhout CM, Devleesschauwer B, Angulo FJ, Verbeke G, Haagsma J, Kirk M, et al. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(11):1073–82.
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Reportable disease trends in Ontario, 2017: technical notes. Toronto, ON: Queen’s Printer for Ontario; 2020.
Gelbicova T, Zobanikova M, Tomastikova Z, Van Walle I, Ruppitsch W, Karpiskova R. An outbreak of listeriosis linked to turkey meat products in the Czech Republic, 2012–2016. Epidemiol Infect. 2018;146(11):1407–12.
Dahl V, Sundqvist L, Hedenstrom I, Lofdahl M, Alm E, Ringberg H, et al. A nationwide outbreak of listeriosis associated with cold-cuts, Sweden 2013–2014. Infect Ecol Epidemiol. 2017;7(1):1324232.
Heiman KE, Garalde VB, Gronostaj M, Jackson KA, Beam S, Joseph L, et al. Multistate outbreak of listeriosis caused by imported cheese and evidence of cross-contamination of other cheeses, USA, 2012. Epidemiol Infect. 2016;144(13):2698–708.
Magalhaes R, Almeida G, Ferreira V, Santos I, Silva J, Mendes MM, et al. Cheese-related listeriosis outbreak, Portugal, March 2009 to February 2012. Euro Surveill. 2015;20(17):1–6.
McIntyre L, Wilcott L, Naus M. Listeriosis outbreaks in British Columbia, Canada, caused by soft ripened cheese contaminated from environmental sources. Biomed Res Int. 2015;131623:1–12.
Okpo E, Leith J, Smith-Palmer A, Bell J, Parks D, Browning F, et al. An outbreak of an unusual strain of Listeria monocytogenes infection in North-East Scotland. J Infect Public Health. 2015;8(6):612–8.
Choi MJ, Jackson KA, Medus C, Beal J, Rigdon CE, Cloyd TC, et al. Notes from the field: multistate outbreak of listeriosis linked to soft-ripened cheese-United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(13):294–5.
De Castro V, Escudero J, Rodriguez J, Muniozguren N, Uribarri J, Saez D, et al. Listeriosis outbreak caused by latin-style fresh cheese, Bizkaia, Spain, August 2012. Euro Surveill. 2012;17(42):1–3.
Centers for Disease Control and Prevention (CDC). Outbreak of invasive listeriosis associated with the consumption of hog head cheese-Louisiana, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(13):401–5.
Jackson KA, Biggerstaff M, Tobin-D’Angelo M, Sweat D, Klos R, Nosari J, et al. Multistate outbreak of Listeria monocytogenes associated with Mexican-style cheese made from pasteurized milk among pregnant, hispanic women. J Food Prot. 2011;74(6):949–53.
Fretz R, Pichler J, Sagel U, Much P, Ruppitsch W, Pietzka AT, et al. Update: multinational listeriosis outbreak due to ‘Quargel’, a sour milk curd cheese, caused by two different L. monocytogenes serotype 1/2a strains, 2009–2010. Euro Surveill. 2010;15(16):1–2.
Bille J, Blanc DS, Schmid H, Boubaker K, Baumgartner A, Siegrist HH, et al. Outbreak of human listeriosis associated with tomme cheese in northwest Switzerland, 2005. Euro Surveill. 2006;11(6):91–3.
Gianfranceschi M, D’Ottavio MC, Gattuso A, Pourshaban M, Bertoletti I, Bignazzi R, et al. Listeriosis associated with gorgonzola (italian blue-veined cheese). Foodborne Pathog Dis. 2006;3(2):190–5.
Gottlieb SL, Newbern EC, Griffin PM, Graves LM, Hoekstra RM, Baker NL, et al. Multistate outbreak of listeriosis linked to turkey deli meat and subsequent changes in US regulatory policy. Clin Infect Dis. 2006;42(1):29–36.
Althaus D, Jermini M, Giannini P, Martinetti G, Reinholz D, Nuesch-Inderbinen M, et al. Local outbreak of Listeria monocytogenes serotype 4b sequence type 6 due to contaminated meat pate. Foodborne Pathog Dis. 2017;14(4):219–22.
Duranti A, Sabbatucci M, Blasi G, Acciari VA, Ancora M, Bella A, et al. A severe outbreak of listeriosis in central Italy with a rare pulsotype associated with processed pork products. J Med Microbiol. 2018;67(9):1351–60.
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED). Outbreak of Listeria Infections Linked to Deli Ham (Final Update). 2018. https://www.cdc.gov/listeria/outbreaks/countryham-10-18/index.html. Accessed 06 Oct 2022.
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED). Multistate Outbreak of Listeriosis Linked to Soft Raw Milk Cheese Made by Vulto Creamery (Final Update). 2017. https://www.cdc.gov/listeria/outbreaks/soft-cheese-03-17/index.html. Accessed 06 Oct 2022.
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED). Multistate Outbreak of Listeriosis Linked to Raw Milk Produced by Miller’s Organic Farm in Pennsylvania (Final Update). 2016. https://www.cdc.gov/listeria/outbreaks/raw-milk-03-16/index.html. Accessed 06 Oct 2022.
Smith AM, Tau NP, Smouse SL, Allam M, Ismail A, Ramalwa NR, et al. Outbreak of Listeria monocytogenes in South Africa, 2017–2018: Laboratory Activities and Experiences Associated with whole-genome sequencing analysis of Isolates. Foodborne Pathog Dis. 2019;16(7):524–30.
Angelo KM, Conrad AR, Saupe A, Dragoo H, West N, Sorenson A, et al. Multistate outbreak of Listeria monocytogenes infections linked to whole apples used in commercially produced, prepackaged caramel apples: United States, 2014–2015. Epidemiol Infect. 2017;145(5):848–56.
Gillesberg Lassen S, Ethelberg S, Bjorkman JT, Jensen T, Sorensen G, Kvistholm Jensen A, et al. Two listeria outbreaks caused by smoked fish consumption-using whole-genome sequencing for outbreak investigations. Clin Microbiol Infect. 2016;22(7):620–4.
Self JL, Conrad A, Stroika S, Jackson A, Burnworth L, Beal J, et al. Notes from the field: outbreak of Listeriosis Associated with consumption of packaged salad - United States and Canada, 2015–2016. MMWR Morb Mortal Wkly Rep. 2016;65(33):879–81.
Stephan R, Althaus D, Kiefer S, Lehner A, Hatz C, Schmutz C et al. Foodborne transmission of Listeria monocytogenes via ready-to-eat salad: A nationwide outbreak in Switzerland, 2013–2014. Food Control [Internet]. 2015;57:14–7. https://www.zora.uzh.ch/id/eprint/122093/. Accessed 06 Oct 2022.
McCollum JT, Cronquist AB, Silk BJ, Jackson KA, O’Connor KA, Cosgrove S, et al. Multistate outbreak of listeriosis associated with cantaloupe. N Engl J Med. 2013;369(10):944–53.
Hanson H, Whitfield Y, Lee C, Badiani T, Minielly C, Fenik J, et al. Listeria monocytogenes associated with pasteurized chocolate milk, Ontario, Canada. Emerg Infect Dis. 2019;25(3):581–4.
Currie A, Farber JM, Nadon C, Sharma D, Whitfield Y, Gaulin C, et al. Multi-province listeriosis outbreak linked to contaminated deli meat consumed primarily in institutional settings, Canada, 2008. Foodborne Pathog Dis. 2015;12(8):645–52.
Kvistholm Jensen A, Nielsen EM, Bjorkman JT, Jensen T, Muller L, Persson S, et al. Whole-genome sequencing used to investigate a nationwide outbreak of Listeriosis caused by ready-to-eat Delicatessen Meat, Denmark, 2014. Clin Infect Dis. 2016;63(1):64–70.
Johnsen BO, Lingaas E, Torfoss D, Strom EH, Nordoy I. A large outbreak of Listeria monocytogenes infection with short incubation period in a tertiary care hospital. J Infect. 2010;61(6):465–70.
Gaul LK, Farag NH, Shim T, Kingsley MA, Silk BJ, Hyytia-Trees E. Hospital-acquired listeriosis outbreak caused by contaminated diced celery–Texas, 2010. Clin Infect Dis. 2013;56(1):20–6.
Rietberg K, Lloyd J, Melius B, Wyman P, Treadwell R, Olson G, et al. Outbreak of Listeria monocytogenes infections linked to a pasteurized ice cream product served to hospitalized patients. Epidemiol Infect. 2016;144(13):2728–31.
Mazengia E, Kawakami V, Rietberg K, Kay M, Wyman P, Skilton C, et al. Hospital-acquired listeriosis linked to a persistently contaminated milkshake machine. Epidemiol Infect. 2017;145(5):857–63.
Shetty A, McLauchlin J, Grant K, O’Brien D, Howard T, Davies EM. Outbreak of Listeria monocytogenes in an oncology unit associated with sandwiches consumed in hospital. J Hosp Infect. 2009;72(4):332–6.
Graham JC, Lanser S, Bignardi G, Pedler S, Hollyoak V. Hospital-acquired listeriosis. J Hosp Infect. 2002;51(2):136–9.
Dawson SJ, Evans MR, Willby D, Bardwell J, Chamberlain N, Lewis DA. Listeria outbreak associated with sandwich consumption from a hospital retail shop, United Kingdom. Euro Surveill. 2006;11(6):89–91.
Health Canada. HPB Methods for the Microbiological Analysis of Foods -MFHPB-30: Isolation of Listeria monocytogenes and other Listeria spp. from foods and environmental samples. Ottawa: Queen’s Printer for Canada. 2011. www.canada.ca/en/health-canada/services/food-nutrition/research-programs-analytical-methods/analytical-methods/compendium-methods/methods-microbiological-analysis-foods-compendium-analytical-methods.html. Accessed 06 Oct 2022.
Lipcsei LE, Brown LG, Hoover ER, Faw BV, Hedeen N, Matis B, et al. Retail Deli Slicer Inspection Practices: an EHS-Net study. J Food Prot. 2018;81(5):799–805.
Ferreira V, Wiedmann M, Teixeira P, Stasiewicz MJ. Listeria monocytogenes persistence in food-associated environments: epidemiology, strain characteristics, and implications for public health. J Food Prot. 2014;77(1):150–70.
Chasseignaux E, Toquin MT, Ragimbeau C, Salvat G, Colin P, Ermel G. Molecular epidemiology of Listeria monocytogenes isolates collected from the environment, raw meat and raw products in two poultry- and pork-processing plants. J Appl Microbiol. 2001;91(5):888–99.
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Focus on: Practices for cleaning and sanitizing meat slicers to control Listeria. Toronto: Queen’s Printer for Ontario. 2021. https://www.publichealthontario.ca/-/media/Documents/Surveillance-Reports/Infectious/2021/focus-on-listeria-and-slicers.pdf?rev=9fa006b876ad4d19ac599b583a7651c1&sc_lang=en. Accessed 07 Jul 2023.
Acknowledgements
The authors thank the following individuals and organizations: Ontario public health units including Salman Siddiqui and Tom Marjanovich from Toronto Public Health; the Ontario Ministry of Health; Public Health Ontario staff members in the Enteric, Environmental and Molecular Surveillance laboratories; Public Health Ontario staff members of the Enteric, Zoonotic and Vector-Borne Diseases Unit; Canadian Food Inspection Agency Food Microbiology Laboratories; Ontario-Outbreak Investigation Coordinating Committee partners, including the Public Health Agency of Canada, the Canadian Food Inspection Agency, the Ontario Ministry of Agriculture Food and Rural Affairs, Health Canada, and the National Microbiology Laboratory (PulseNet Canada).
Funding
No funding was obtained for any aspect of this study including: data collection, analysis, and interpretation; writing the report; or in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
JLH completed the original draft of the manuscript as well as data interpretation and analysis. CL was involved in the preparation of the manuscript for submission. All authors were actively involved in one or both outbreak investigations. JLH, CL, JC, NB, and BW coordinated the investigations, and interpreted and summarized findings provincially. BT, AA, OO, TP, CN, and VD led the local investigations, including completing case follow up and inspections at the implicated food premises. AK, MG, and KC led the food safety investigations, including carrying out traceback, traceforward, and product sampling. AM, ML, AMM, ALM, MG and ES completed laboratory testing and interpretation of results for clinical, food, and environmental isolates. MG and ES generated the whole genome sequencing figure. All authors edited and critically reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent is waived by (Ontario Agency for Health Protection and Promotion Act, SO 2007, c 10). As per Public Health Ontario’s ethics review process and provincial regulations, this project did not require research ethics committee approval as the activities described in this manuscript were conducted in fulfillment of Public Health Ontario’s legislated mandate “to provide scientific and technical advice and support to the health care system and the Government of Ontario in order to protect and promote the health of Ontarians” (Ontario Agency for Health Protection and Promotion Act, SO 2007, c 10) and are therefore considered public health practice, not research. Methods were carried out following relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have no financial or non-financial competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hobbs, J.L., Lee, C., Thompson, B. et al. Two Listeria monocytogenes outbreaks in a cancer centre: onsite food premises and their potential health risk to patients. BMC Public Health 23, 1443 (2023). https://doi.org/10.1186/s12889-023-16371-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16371-7