Abstract
Listeriosis, caused by Listeria spp., presents varying clinical manifestations among individuals, from moderate fecal infections such as diarrhea to severe infections such as septicemia, meningitis and abortion or newborn listeriosis in perinatal patients. In Africa, listeriosis is attributed to poor sanitation and cross-contamination in food processing environments, particularly ready to eat (RTE) foods including dairy products, leafy vegetables, fish and meat. Despite the global increase in reported cases and research on listeriosis, data from Africa remains scarce and this could lead to possible underestimation of the importance of listeriosis on the continent. This paper therefore presents a comprehensive overview of currently available reports on Listeria spp. in Africa with emphasis on molecular characteristics, antimicrobial susceptibility, and prevalence in food, animal and environmental samples. The majority of studies on Listeria spp. in Africa have so far focused on the prevalence and antibiotic susceptibility of L. monocytogenes isolated from RTE foods and raw meat but rarely from humans, animals, and the environment. The overall calculated average prevalence values from the available reports are 23.7 and 22.2% for Listeria spp. and L. monocytogenes, respectively. Listeria spp. isolated from different parts of Africa are generally sensitive to ciprofloxacin, but resistant to penicillin. The majority of these studies employed conventional culture and biochemical tests to characterize Listeria spp. However, the use of modern molecular techniques such as PCR and whole-genome sequencing is on the rise. Most of the studies employing molecular tools were carried out in South Africa and Nigeria, with the predominant strain reported in South Africa being ST6. In order to provide a better understanding of the importance of listeria in Africa, there is the need for extensive and coordinated studies using modern molecular-based techniques to characterize the various Listeria species, and to assess the disease epidemiology using the one health concept.
Similar content being viewed by others
Background
Listeriosis is predominantly a foodborne infection associated with microorganisms of the genus Listeria. Listeria mostly affects the elderly, immunocompromised individuals, pregnant women, and newborns [1, 2]. The World Health Organization (WHO) estimates the global burden of listeriosis to be 172,823 disability adjusted life years (DALYs) from 23,150 illnesses [3]. This estimate is based on several data sources from high-income and middle-income subregions, and arbitrary assumptions on regions with data gaps such as WHO African regions (WHO – AFRO) that had 3624 listeriosis incidences, 955 deaths and 27,045 DALYs.
Listeria spp. are gram-positive, catalase-positive bacteria that are motile at least at 30 °C, persist for long periods in the environment, and can grow in a wide range of temperatures. There are currently seventeen (17) identified Listeria species. However, L. ivanovii and L. monocytogenes remain the most important species that cause listeriosis in animals and humans [4, 5]. These species are globally distributed with varying prevalence rates in the different regions. Currently, a comprehensive review on listeriosis in Africa is unavailable, except for very few isolated reports [3]. Thus, the epidemiology of listeriosis in Africa is less understood, and can lead to underestimation of the disease burden on the continent. Meanwhile, a comprehensive overview of the existing published data on epidemiology, prevalence, antimicrobial resistance, and molecular characteristics of Listeria spp. from various countries would provide an outlook of the disease in Africa and highlight areas of urgent research needs.
In this narrative review, we have presented, in context, the currently available literature on the prevalence and molecular diversity of Listeria spp. in Africa. In addition, the resistance of Listeria spp. to common antibiotics, major epidemiological hypotheses and areas of urgent research needs are highlighted. All observational studies reporting on the prevalence, antimicrobial resistance/susceptibility, or characterization of Listeria species in Africa were searched on PubMed, Web of Science, EMBASE, Google Scholar and the Cochrane Library for this review.
Epidemiology
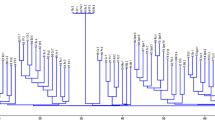
The epidemiology of listeria in Africa is often marked by sporadic cases or major outbreaks. The 2017/2018 South African listeriosis outbreak awakened the world to the possible wide-spread of the disease in Africa [6, 7]. Humans risk multiple exposures to infection via contact with carriers of listeria. Listeria, the causative agent for listeriosis, can colonize up to 5% of healthy adults [7]. Adults with invasive listeriosis can present symptoms such as fever, stillbirth, and convulsion among others. The risk of infection is further exacerbated by the ubiquitous nature of the pathogen, making it difficult to get rid of listeriosis [4]. In Africa, Listeria spp., particularly L. monocytogenes, has been isolated from various food, animal and environmental sources in countries such as Nigeria, South Africa, Ghana, Ethiopia, Egypt and Botswana. Table 1 summarizes the prevalence of Listeria spp. in various food and environmental samples from different African countries (Fig. 1).
Prevalence of Listeria monocytogenes in selected African countries. *Average from single study; CMA: Calculated Mean Average (See Table 1.); Calculated Mean Average (CMA) = (Sum of prevalence rates/number of prevalence) × 100
To date, the listeriosis outbreak in South Africa remains the largest in the world with over 1000 laboratory-confirmed cases and over 200 fatalities [24]. This unprecedented outbreak has been attributed to changes in food production and distribution processes in South Africa [25]. Before this outbreak, a marked increase in listeriosis cases was recorded in June 2017 with the source of infection being RTE processed meat product [25]. Following identification of the source of the outbreak, recalls of the affected products were made in South Africa and 15 other African countries [26]. Other reports from South Africa described the presence of L. monocytogenes in various food items [27]. In 2015, L. monocytogenes ST6 affecting humans were reported in Western Cape Province of South Africa [25]. From 2014 to 2016, the overall prevalence of L. monocytogenes in meat and meant products in South Africa was reported to be 14.7% (296/2017), with meats from local markets and ports of entry recording prevalence rates of 15.0% (264/1758) and 12.4% (32/259), respectively [8]. On the other hand, the prevalence of L. monocytogenes recovered from irrigation water and agricultural soil samples in South Africa were 6.8% (8/117) and 6.6% (12/183), respectively [9]. Other studies have also reported that municipal wastewater effluent is a possible reservoir and transporter of pathogenic Listeria in South Africa and this is of public health concern [28]. Taking into account that approximately 77% of South Africans depend on surface water for their daily activities, the reported prevalence of Listeria in irrigation water and agricultural soil could be potential source for infections [29]. From available data, the calculated mean prevalence of L. monocytogenes in South African is 17.9%. Despite the few recent reports on the prevalence of listeriosis in South Africa, comprehensive historic data on prevalence, epidemiology and outbreaks associated with L. monocytogenes is still lacking [25].
In Northern Africa, Listeria spp. was detected in 32% of luncheon, 32% of minced frozen beef, 52% of frozen chicken leg and 56% of frozen chicken fillet in Assiut, Egypt [22]. Additionally, the incidence of Listeria spp. in stool samples of children with underlying health conditions at Assiut University hospital was reported to be 7.14% (2/28). The data demonstrate a potential infection linked to consumption of listeria-containing meat and chicken products in Assiut city, Egypt [22].
In East Africa, the prevalence rate of L. monocytogenes among pregnant women in northern Ethiopia was reported to be 8.5% [20]. Also, 4.4% prevalence of L. monocytogenes was reported in beef and fomites [18]. In another study, a 26.1% prevalence of Listeria spp. was reported in food of animal origin [30]. Furthermore, a prevalence of 25 and 6.25% for Listeria species and L. monocytogenes, respectively, was reported from ready-to eat food of animal origin in Ethiopia [19].
In an investigation to assess the occurrence of L. monocytogenes in Gaborone, Botswana in Central Africa, Morobe et al., [21] analyzed food samples collected from five geographical areas. In their report, the overall prevalence of L. monocytogenes was 4.3% (57/1324). Out of the 57 L. monocytogenes isolates, 12.3% were derived from cheese while the highest L. monocytogenes prevalence of 33.3% was recorded in Gaborone South [21].
In West Africa, the Nigerian meat industry has been implicated in the transmission of Listeria spp. [10]. In Rivers State, South-South Nigeria, 7% prevalence of L. monocytogenes in raw meat samples was reported [10] while 91.8% prevalence of L. monocytogenes in chicken flocks and meat was reported in Oyo state, Nigeria [11]. In Lafia, Nigeria, the reported prevalence of Listeria spp. in beef and chevon were 58.2% (78/134) and 41.8% (56/134), respectively. Of these isolates, 64.4% (67/104) were confirmed to be L. monocytogenes [5]. In Enugu state, Nigeria, the frequency of Listeria spp. isolated from chicken meat, pork, and beef samples was 27.1, 13.2 and 45.8% respectively [12], while in Zaria, Nigeria, the prevalence of L. monocytogenes in raw meat and meat products was 4.0% [13]. Other studies in Nigeria reported the prevalence of L. monocytogenes in vegetables including in cabbage, carrot, cucumber, lettuce, and tomatoes to be, 28.28, 9.02, 23.36, 19.67, and 19.67%, respectively [15]. Additionally, the prevalence of Listeria spp. in locally made soft cheeses (wara) was 78%. Out of which 12.4% were identified as L. monocytogenes [31]. From this review, the calculated mean average prevalence of L. monocytogenes for Nigeria is 43.5%.
In Ghana, data on the prevalence of L. monocytogenes remains scarce. However, 5.5% (14/254) prevalence of L. monocytogenes in traditional milk products was reported [17]. Individual prevalence for raw cow milk, boiled milk and spontaneously fermented milk (nunu) were 8.8% (10/114), 0% (0/114), and 13.1% (11/84), respectively [17]. Additionally, Listeria was identified in fresh milk [32] and smoked fish [33]. Listeria spp. was not recorded when pregnancy related infections in rural communities was investigated [34].
Antimicrobial resistance
Antimicrobial resistance has become a global public health issue. Several studies across Africa have reported the antimicrobial resistance profiles of Listeria species, specifically L. monocytogenes. Table 2 summarizes reported studies on antibiotic resistance profiles of listeria isolates in Africa.
In Ethiopia, resistance of L. monocytogenes was reported for the following antibiotics: penicillin 66.7% (16/24), nalidixic acid 50% (12/24), tetracycline 37.5% (9/24) and chloramphenicol 16.6% (4/24). Furthermore, 16.6% were found to be multi-drug resistant [19]. In a different study, L. monocytogenes isolated from pregnant women in Ethiopia showed that isolates were resistant to clindamycin (66.7%), penicillin G (66.7%), vancomycin (50%) and amoxicillin (50%). However, isolates were sensitive to erythromycin (75%), ciprofloxacin (75%), trimethoprim/sulphamethaxazole (66.7%) and chloramphenicol (60%) [20]. Whereas, Listeria spp. isolated from wastewater treatment plants in Durban, South Africa, demonstrated 100% resistance to penicillin, nalidixic acid and erythromycin. Furthermore, these isolates were also resistant to ampicillin (83.33%), trimethoprim (67.95%), nitrofurantoin (64.10%) and cephalosporin (60.26%) [35].
Similarly, L. monocytogenes isolates recovered from irrigation water and agricultural soil from Eastern Cape Province, South Africa, were resistant to tetracycline (90%), doxycycline (85%), penicillin (80%), cefotaxime (80%), chloramphenicol (70%), linezolid (65%), erythromycin (60%) and trimethoprim/sulfamethoxazole (55%) [9]. The isolates were also reported to harbor tetA, tetB, tetC, sulI, sulII, aadA, aac (3)-IIa resistance genes and extended-spectrum beta-lactamase (ESBLs) including blaTEM, blaCTX-M group 9, blaVEB as well as ampC. However, none of the isolates carried the carbapenemase resistance genes [9].
In South Africa, another study reported that 1.7% L. monocytogenes isolated from meat showed multiple resistance to 13 of the 19 test antibiotics. Resistance was recorded for streptomycin (99.0%), clindamycin (97.3%), fusidic acids (95.6%), nitrofurantoin (79.7%), and gentamycin (74.4%). However, the isolates were sensitive to ampicillin (85.6%), kanamycin (84.6%), amikacin (77.6%), vancomycin (74.2%), and tetracycline (62.5%) [8].
In Botswana, L. monocytogenes isolated from RTE/meat showed multiple resistance against penicillin G (42.1%), sulphamethaxozole/trimethoprim (29.8%), chloramphenicol (28.3%), and tetracycline (22.8%). Resistance against penicillin G and tetracycline was a common pattern in all L. monocytogenes isolated from food products. However, the isolates were generally susceptible to fusidic acid, erythromycin, methicillin, ampicillin and cephalothin [21].
In Enugu State, South-East Nigeria, L. monocytogenes isolated from beef, chicken, and pork were examined against penicillin, cephalothin, amoxicillin, ampicillin, nitrofurantoin, vancomycin, tetracycline, gentamicin (aminoglycosides), gentamicin (macrolides), ciprofloxacin, sulphamethoxazole/trimethoprim and rifampicin. All L. monocytogenes showed 100% resistance against penicillin. Interestingly, only L. monocytogenes recovered from pork showed 100% resistance to more than one antibiotic, i.e., penicillin, cephalothin, sulphamethoxazole/ trimethoprim and ciprofloxacin [12]. The high and multidrug resistance of isolates from pork is a public health concern and could be attributed to the misuse of antibiotics in pig farming. Also, L. monocytogenes isolated from beef, pork and chicken recorded resistance to amoxicillin, tetracycline, augmentin and cloxacillin but sensitivity to erythromycin and gentamicin [16].
In Ekiti, South-West Nigeria, Listeria spp. isolated from soft cheese (wara) showed 90 and 89% resistance against ampiclox (ampicillin/cloxacillin) and amoxicillin, respectively. However, the isolates were susceptible to ciprofloxacin and septrin (co-trimoxazole) [31]. L. monocytogenes isolated from beef and chevon in North-Central Nigeria were reported to be resistant to streptomycin (58.2%), sparfloxacin (55.2%), ampicillin (34.3%), and gentamicin (20.9%) [5]. L. monocytogenes has also been reported to be resistant to ampicillin and erythromycin, but susceptible to gentamicin and ciprofloxacin [14]. In another study, L. monocytogenes strains were resistant (100%) to both ampicillin-cloxacillin and cefuroxime but susceptible to amoxicillin clavulanate (86.1%) ciprofloxacin (43.8%), cloxacillin (36.1%), ceftriaxone (32.5%), gentamicin sulphate (27.8%), streptomycin sulphate (25.0%), pefloxacin (17.5%), erythromycin 5 μg (16.7%), co-trimoxazole (12.5%), erythromycin 10 μg (12.5%), and amoxicillin (6.3%) [11]. Similarly, 100% resistance to augmentin, erythromycin, tetracycline, rifampicin, and cloxacillin was recorded, with some isolates demonstrating a varying degree of resistance to norfloxacin (57.2%), levofloxacin (71.4%), and ciprofloxacin (71.4%). On the contrary, all L. monocytogenes isolates from retail meats were (100%) susceptible to chloramphenicol, gentamicin, ampiclox, clotrimoxazole, and streptomycin [10].
In Ghana, L. monocytogenes resistance against neomycin (61.3%) and tetracycline (24.2%) was observed. While intermediate susceptibilities were recorded for chloramphenicol, ciprofloxacin, clindamycin, doxycycline, kanamycin, neomycin, streptomycin, and tetracycline, general susceptibility (100%) to amoxicillin, ampicillin, erythromycin, gentamycin, penicillin, rifampicin, and vancomycin was observed [17].
Although antibiotics remain the conventional protocol for the treatment of listeriosis, some studies have also shown the potential of plant extracts in listeriosis chemotherapy. The effect of plant triterpenes: 3β-hydroxylanosta-9,24-dien-21-oic acid, methyl-3β-hydroxylanosta-9,24-dien-21-oate and 3β-acetylursolic acid, against L. monocytogenes, L. ivanovii and L. grayi species was investigated. The triterpenes’ minimum inhibitory concentration (MIC) values ranged from 0.185 to 1.67 mg/ml while the minimum bactericidal concentration (MBC) determination assay revealed that the triterpenes were bacteriostatic against Listeria spp. [36]. In summary, listeria isolates from Africa are generally susceptible to ampicillin and ciprofloxacin. However, the emergence of multidrug resistant strains is of serious public health concern in Africa.
Molecular characterization
Genomic studies have been employed to elucidate the global circulation of L. monocytogenes [37]. In Africa, the serotypes of circulating strains of L. monocytogenes are largely unknown [38]. In epidemiological studies, rapid detection of listeriosis outbreaks is often by phenotypic and molecular characterizations [39]. Subtyping of L. monocytogenes isolates is essential for epidemiological investigation and for identification of the source of contamination [1]. Table 3 provides a summary of molecular tools employed in the characterization of Listeria spp. in Africa.
Multilocus Sequence Typing (MLST) has been used to prove that the 2015 and 2017 listeriosis outbreaks in South Africa were mainly due to contamination of meat products by L. monocytogenes ST6 [25]. L. monocytogenes ST6 is often associated with high fatality cases. Whole-genome sequencing approach, MLST, was used to demonstrate that L. monocytogenes ST6 was the most common serotype of L. monocytogenes detected in human listeriosis cases in Western Cape Province in South Africa [6].
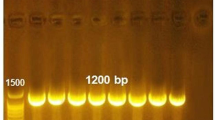
Four different STs (ST1, ST121, ST204, and ST876) belonging to lineage I (serogroup 4b) and lineage II (1/2a) were identified using whole genome sequencing (WGS) to characterize six L. monocytogenes isolated from RTE meat products in South Africa [40]. From their report, the majority of the serogroup 4b (lineage I) strains clustered together while two isolates of serogroup 1/2a (lineage II) were apart compared to the other strains using core genome and average nucleotide identity (ANI) phylogenetic analyses. Additionally, twenty-four different prophages were identified using PHAge Search Tool Enhanced Release (PHASTER) software [40]. The National Center for Biotechnology Information- Nucleotide Basic Local Alignment Search Tool (NCBI-BLAST) showed that the investigated L. monocytogenes strains shared some major virulence genes encoded in the pathogenicity islands 1 and 3 of listeria [40]. All isolates harbored resistant genes against food antiseptics. Overall, all strains of L. monocytogenes isolated from ready to RTE meat products showed similar resistance profiles against heavy metal, and antibiotic [40]. Polymerase chain reaction (PCR) was also employed to demonstrate that most of the L. monocytogenes isolates harbored inlJ (98.7%) and ipa (95.6%) genes with at least one other internalin genes (inlB, inlC, or inlA) [40]. Using PCR, 26.92% of Listeria spp. isolated from the effluent of wastewater in Durban, South Africa, were found to contain virulence genes, with 14.10, 5.12, and 21% harboring the actA, plcA and iap genes, respectively. Additionally, the study employed enzymatic hydrolysis to characterize gelatinase, protease, and haemolysin [35]. Similarly, PCR was used to confirm that all L. monocytogenes isolates recovered from irrigation water and agricultural soil in Eastern Cape Province, South Africa harbored nine virulence genes (inlA, inlB, inlC, inlJ, actA, hlyA, plcA, plcB, and iap) [9].
In Nigeria, the first L. monocytogenes genome sequence was of three isolates recovered from fresh leaves and vegetables in South-Eastern Nigeria. The size of the draft genome was between 2.93 to 3.06 Mb, with 37.9% GC content. Isolates were found to belong to ST155 and ST5 using MLST, while CT2050 and CT2051 were defined as new cgMLST types [37]. In South-East Nigeria, 23(30.67%) and 41(54.67%) Listeria spp. were isolated from a cereal-based food (fura), and a RTE fermented milk (nunu), respectively. Using PCR, the isolates were classified as human pathogenic serogroup 1/2a and 4b, with some strains harboring virulence genes hlyA and iap [41]. Similarly, L. monocytogenes isolates from raw meat and meat products in Kaduna, Nigeria was characterized using uniplex PCR to detect the hylA gene [13].
Multiplex PCR was employed to identify virulence-associated genes (prfA, inlA, hlyA, actA, and iap) in L. monocytogenes from milk in Nigeria [42]. The study further compared the 16S rRNA sequence of the isolates to the reference L. monocytogenes ATCC 19155 and a phylogenetic analysis enabled the clustering of the isolates into two lineages; lineage A (responsible for epidemic listeriosis) and lineage B (responsible for sporadic cases of listeriosis). The categorization of the L. monocytogenes isolates into the two lineages provides better overview of potential risk of listeriosis outbreak by these isolates [42]. The Nigerian L. monocytogenes isolates (NGA 34A, NGA 35A, and NGA 41A) were phylogenetically closer to J1776; N1-011A; R2–502; J1816; and J2–031, whereas isolate (NGA 38A) was closer to EDG; J1–220; J1926; J1817; and J2–1091 [42].
In Ghana, multiplex PCR was used to identify virulence-associated genes, plcA, actA, hlyA, iap and prfA, as well as inlA, inlB, inlC, and inlJ in L. monocytogenes isolates from raw and fermented cow milk product [17]. The presence of single or multiple genes enable categorization of isolates into serogroups 1/2a-3a (32/62, 51.6%), 1/2b-3b-7 (14/62, 22.6%), 4b-4d-4e (9/62, 14.5%) and 1/2c-3c (7/62, 11.3%) [17].
In summary, PCR techniques have been used in a few studies to identify and characterize the virulence potential of L. monocytogenes in Africa. However, the use of whole-genome sequencing to enhance characterization is gradually emerging in Africa, particularly in South Africa and Nigeria.
Conclusion and future perspective
Listeria spp., particularly L. monocytogenes, is generally reported to have a low prevalence rate but a high fatality rate. The possible explanations for the epidemiological differences of Listeria spp. across Africa could be attributed to the variation in study groups, sampling source, microbial diversity, and geographic location. Currently, information on the prevalence, antimicrobial susceptibility profiles, and molecular characteristics of Listeria spp. in Africa is limited and disconnected. Here the highest calculated mean average of Listeria spp. was recorded in Nigeria, followed by South Africa. Although, L. monocytogenes isolates are generally susceptible to many antibiotics, the observed single and multiple antibiotics resistant strains detected are a cause for concern. Our review shows that, the majority of the African Listeria isolates are resistant to penicillin, erythromycin, tetracycline, and amoxicillin, while most isolates are susceptible to gentamicin, amikacin, ampicillin and ciprofloxacin.
While studies on the prevalence and antibiotic susceptibility profile of Listeria spp. are considered limited globally, molecular characterization of Listeria spp. in Africa remains very scarce. Genomic sequences are often employed to decipher population structure, pathogen evolution and transmission networks. Although there has been an increase in the use of PCR and MLST to study listeriosis since 2018, most of the studies were limited to L. monocytogenes isolates from RTE foods in South Africa and Nigeria.
To develop effective preventive and control measures against potential Listeria spp. outbreaks, it is crucial to actively research the molecular epidemiology of listeriosis. To understand the dynamics of listeria infection in Africa, other African countries should contribute to studies aimed at a complete overview of the prevalence of listeria in Africa. There is also the need to elucidate the link between the epidemiological patterns of Listeria spp. from various sources (animals, humans and environment), by adapting the one health concept to study not only L. monocytogenes in RTE food but also study other Listeria spp. in humans, animals, and the environment.
Availability of data and materials
Not applicable.
Abbreviations
- L:
-
Listeria
- Spp:
-
species (spp)
- RTE:
-
Ready to Eat
- WHO:
-
World Health Organization
- DALYs:
-
Disability adjusted life daily
- AFRO:
-
African regions
- CMA:
-
Calculated mean Average
- ND:
-
Not determined
- ESBL:
-
Extended-spectrum beta-lactamase
- MIC:
-
Minimum inhibitory concentration
- MBC:
-
Minimum bactericidal concentration
- PGAP:
-
Prokaryotic Genome Annotation Pipeline
- RNA:
-
Ribonucleic acid
- ANI:
-
Average nucleotide identity
- PHASTER:
-
PHAge Search Tool Enhanced Release
- NCBI-BLASTn:
-
National Center for Biotechnology Information-NucleotideBasic Local Alignment Search Tool
- PCR:
-
Polymerase chain reaction
- MLST:
-
Multilocus Sequence Typing
- ST(s):
-
Serotype(s)
- WGS:
-
Whole Genome Sequencing (WGS)
References
Jamshidi A, Zeinali T. Significance and characteristics of Listeria monocytogenes in poultry products. Int J Food Sci. 2019;2019:1–7. https://doi.org/10.1155/2019/7835253.
De Luca C, Donati L, D’oria L, Licameli A, Pellegrino M, De Santis M. Listeria infection in pregnancy: a review of literature. Open Infect Dis J. 2015;9(1):20–5. https://doi.org/10.2174/1874279301509010020.
De Noordhout CM, Devleesschauwer B, Angulo FJ, Haagsma J, Kirk M, Havelaar A, et al. The global burden of listeriosis : a systematic review and meta- analysis. Lancet Infect Dis. 2015;14(11):1073–82.
Kayode AJ, Igbinosa EO, Okoh AI. Overview of listeriosis in the southern African hemisphere—review. J Food Saf. 2020;40(1):1–22.
Chuku A, Obande GA, Eya SB. Original Article Listerial contamination of raw beef and chevon in north-central Nigeria. IMC J Med Sci. 2020;13(2):1-8.
Allam M, Tau N, Smouse SL, Mtshali PS, Mnyameni F, Khumalo ZTH. Whole-genome sequences of Listeria monocytogens sequence type 6 isolates associated with a large foodborne outbreak in South Africa, 2017 to 2018. Genome Announc. 2018;6(25):2017–8.
Tchatchouang CDK, Fri J, De Santi M, Brandi G, Schiavano GF, Amagliani G, et al. Listeriosis outbreak in south africa: A comparative analysis with previously reported cases worldwide. Microorganisms. 2020;8(1):135. https://doi.org/10.3390/microorganisms8010135.
Matle I, Mbatha KR, Lentsoane O, Magwedere K, Morey L, Madoroba E. Occurrence, serotypes, and characteristics of Listeria monocytogenes in meat and meat products in South Africa between 2014 and 2016. J Food Saf. 2019;39(4):1–14.
Iwu CD, Okoh IA. Characterization of antibiogram fingerprints in Listeria monocytogenes recovered from irrigation water and agricultural soil samples. PLoS One. 2020 10;15(2):e0228956. https://doi.org/10.1371/journal.pone.0228956.
Odu NN, Okonko IO. Prevalence and antibiotic susceptibility of Listeria monocytogenes in retailed meats in Port Harcourt Metropolis. Nigeria Public Heal Res. 2017;7(4):91–9.
Ishola OO, Mosugu JI, Adesokan HK. Prevalence and antibiotic susceptibility profiles of Listeria monocytogenes contamination of chicken flocks and meat in Oyo State , south-western Nigeria. J Prev Med Hyg. 2016;57(3):157–63.
Okorie-Kanu OJ, Anyanwu MU, Ezenduka EV, Mgbeahuruike AC, Okorie-Kanu CO, Ugwuijem EE, et al. Occurrence and antibiogram of Listeria species in raw pork, beef, and chicken meats marketed in Enugu state, Southeast Nigeria. Vet World. 2020;13(2):317–25. https://doi.org/10.14202/vetworld.2020.317-325.
Ndahi MD, Kwaga JKP, Bello M, Kabir J, Umoh VJ, Yakubu SE, et al. Prevalence and antimicrobial susceptibility of Listeria monocytogenes and methicillin-resistant Staphylococcus aureus strains from raw meat and meat products in Zaria, Nigeria. Lett Appl Microbiol. 2014;58(3):262–9. https://doi.org/10.1111/lam.12183.
Ieren II, Bello M, Kwaga JKP. Occurrence and antibiotic resistance profile of Listeria monocytogenes in salad vegetables and vegetable salads sold in Zaria, Nigeria. Afr J Food Sci. 2013;7(9):334–8. https://doi.org/10.5897/AJFS2013.1036.
Ajayeoba TA, Atanda OO, Obadina AO, Bankole MO, Adelowo OO. The incidence and distribution of Listeria monocytogenes in ready- to- eat vegetables in South- Western Nigeria. Food Sci Nutr. 2016;4(1):59–66.
Peter A, Umeh EU, Azua ET, Obande GA. Prevalence and Antimicrobial Susceptibility of Listeria monocytogenes Isolated from Beef , Pork and Chicken Sold in Makurdi Metropolis. MRJI. 2016;14(11):1–7.
Owusu-Kwarteng J, Wuni A, Akabanda F, Jespersen L. Prevalence and characteristics of Listeria monocytogenes isolates in raw milk, heated milk and nunu, a spontaneously fermented milk beverage, in Ghana. Beverages. 2018;13:1–10.
Gebremedhin EZ, Hirpa G, Borana BM, Sarba EJ, Marami LM, Kelbesa KA, Tadese ND, Ambecha HA. Listeria Species Occurrence and Associated Factors and Antibiogram of Listeria monocytogenes in Beef at Abattoirs, Butchers, and Restaurants in Ambo and Holeta in Ethiopia. Infect Drug Resist. 2021;14:1493–504. https://doi.org/10.2147/IDR.S304871.
Garedew L, Taddese A, Biru T, Nigatu S, Kebede E, Ejo M, et al. Prevalence and antimicrobial susceptibility profile of listeria species from ready-to-eat foods of animal origin in Gondar town, Ethiopia. BMC Microbiol. 2015;100(2015):15. https://doi.org/10.1186/s12866-015-0434-4.
Welekidan LN, Bahta YW, Teklehaimanot MG, Abay GK, Wasihun AG, Dejene TA, et al. Prevalence and drug resistance pattern of Listeria monocytogenes among pregnant women in Tigray region, northern Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):1–6. https://doi.org/10.1186/s13104-019-4566-8.
Morobe IC, Obi CL, Nyila MA, Gashe BA, Matsheka MI. Prevalence , antimicrobial resistance profiles of Listeria monocytognes from various foods in Gaborone, Botswana Afr J Biotechnol 2009;8(22):6383–6387, https://doi.org/10.5897/AJB2009.000-9486.
El-Malek AMA, Ali SFH, Hassanein R, Mohamed MA, Elsayh KI. Occurrence of Listeria species in meat, chicken products and human stools in Assiut city, Egypt with PCR use for rapid identification of Listeria monocytogenes. Vet World. 2010;3(8):353–9.
Fall NS, Sarr M, Diagne N, Bassène H, Sokhna C. Listeria monocytogenes detected in vaginal self-samples of 2 women after spontaneous miscarriage, Senegal, West Africa. EJCMID. 2019;39:393–4.
National Institute for Communicable Diseases (NICD). An update on the outbreak of Listeria monocytogenes in South Africa. 2018. [Internet: Accessed Oct 2020]. Available from: http://www.nicd.ac.za/wp-content/uploads/2018/08/An-update-on-the-outbreak-of-Listeria-monocytogenes-South-Africa.pdf.
Smith AM, Tau NP, Smouse SL, Allam M, Ismail A, Ramalwa NR, et al. Outbreak of Listeria monocytogenes in South Africa, 2017-2018: laboratory activities and experiences associated with whole-genome sequencing analysis of isolates. Foodborne Pathog Dis. 2019;16(7):524–30. https://doi.org/10.1089/fpd.2018.2586.
World Health Organisation (WHO). Disease outbreak news. 2018. [Internet: Accessed Apr 2020]. https://www.who.int/csr/don/28-march-2018-liste-riosis-south-africa/en/.
Plessis EMD, Govender S, Pillay B, Korsten L. Exploratory study into the microbiological quality of spinach and cabbage purchased from street vendors and retailers in Johannesburg, South Africa. J Food Prot. 2017;80(10):1726–33.
Odjadjare EEO, Obi LC, Okoh AI. Municipal wastewater effluents as a source of listerial pathogens in the aquatic milieu of the eastern cape province of South Africa: a concern of public health importance. Int J Environ Res Public Health. 2010;7(5):2376–94. https://doi.org/10.3390/ijerph7052376.
Luyt CD, Tandlich R, Muller WJ, Wilhelmi BS. Microbial monitoring of surface water in South Africa: an overview. Int J Environ Res Public Health. 2012;9(8):2669–93. https://doi.org/10.3390/ijerph9082669.
Gebretsadik S, Kassa T, Alemayehu H, Huruy K, Kebede N. Isolation and characterization of Listeria monocytogenes and other Listeria species in foods of animal origin in Addis Ababa, Ethiopia. J Infect Public Health. 2011;4(1):22–9. https://doi.org/10.1016/j.jiph.2010.10.002.
Oyinloye JMA. Detection and molecular characterization of Listeria species in ‘ Wara ’, a west African local cheese sold in Ekiti state. Int J Curr Microbiol App Sci. 2016;5(6):941–8.
Kunadu AP, Holmes M, Miller EL, Grant AJ. International Journal of Food Microbiology Microbiological quality and antimicrobial resistance characterization of Salmonella spp . in fresh milk value chains in Ghana. Int J Food Microbiol. 2018;277(4):41–9. https://doi.org/10.1016/j.ijfoodmicro.2018.04.025.
Tano-Debrah K, Bediako-Amoa B, Saalia FK, Bomfeh K. Occurrence of Listeria monocytogenes in traditionally processed fish in informal markets in Accra, Ghana. GSA (Conference). 2011:10–5.
Völker F, Cooper P, Bader O, Uy A, Zimmermann O, Lugert R, et al. Prevalence of pregnancy-relevant infections in a rural setting of Ghana. BMC Pregnancy Childbirth. 2017;17(1):1–7.
Olaniran AO, Nzimande SBT, Mkize NG. Antimicrobial resistance and virulence signatures of Listeria and Aeromonas species recovered from treated wastewater effluent and receiving surface water in Durban, South Africa. BMC Microbiol. 2015;15(1):1–10. https://doi.org/10.1186/s12866-015-0570-x.
Penduka D, Mosa R, Simelane M, Basson A, Okoh A, Opoku A. Evaluation of the anti-Listeria potentials of some plant-derived triterpenes. Ann Clin Microbiol Antimicrob. 2014;13(1):1–7.
Nwaiwu O, Moura A, Thouvenot P, Rees C, Leclercq A, Lecuit M. Draft genome sequences of Listeria monocytogenes, isolated from fresh leaf vegetables in Owerri City, Nigeria. Genome Announc. 2017;5(22):5–6.
Odetokun IA, Adetunji VO. Prevalence and persistence of Listeria monocytogens in dairy and other ready-to-eat food products in Africa. In: Garg N, Abdel-Aziz S, Aeron A (eds) Microbes in Food and Health. Cham: Springer; 2016. p. 349–62. https://doi.org/10.1007/978-3-319-25277-3_18.
Koudelka Š, Gelbíčová T, Procházková M, Karpíšková R. Lineage and serotype identification of Listeria monocytogenes by matrix-assisted laser desorption ionization-time of flight mass spectrometry. Czech J Food Sci. 2018;36(6):452–8.
Matle I, Pierneef R, Mbatha KR, Magwedere K, Madoroba E. Genomic diversity of common sequence types of Listeria monocytogenes isolated from ready-to-eat products of animal origin in South Africa. Genes (Basel). 2019;10(12):1–19.
Ezeonu IM, Ononugbo CM, Ike AC. Molecular characterization of Listeria monocytogenes isolated from a ready-to-eat fermented milk and cereal product, Fura-de-Nunu. Afr J Microbiol Res. 2018;12(19):448–55. https://doi.org/10.5897/AJMR2018.8828.
Usman UB, Kwaga JKP, Kabir J, Olonitola OS, Radu S, Bande F. Molecular characterization and phylogenetic analysis of Listeria monocytogenes isolated from Milk and Milk products in Kaduna, Nigeria. Can J Infect Dis Med Microbiol. 2016;2016:1–7. https://doi.org/10.1155/2016/4313827.
Acknowledgements
We thank all the authors whose works were used for the review. We also thank Dr. Neil Oldfield for proofreading the manuscript.
Funding
The work received no funding. All financial burden was from the personal salaries of the authors.
Author information
Authors and Affiliations
Contributions
OAD conceived the idea. MOY collected relevant literature and prepared the first draft. OAD, JO-K and FA analyzed and critically revised the draft into a review synthesis. JOK developed Fig. 1 included in the manuscript. OAD, MOY, JO-K and FA read and approved the final version of the manuscript and agreed to be personally accountable for the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not applicable.
Competing interests
OAD, MOY, JOK, and FA declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dufailu, O.A., Yaqub, M.O., Owusu-Kwarteng, J. et al. Prevalence and characteristics of Listeria species from selected African countries. Trop Dis Travel Med Vaccines 7, 26 (2021). https://doi.org/10.1186/s40794-021-00151-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40794-021-00151-5