Abstract
Background
Cardiovascular disease (CVD), one of the most common comorbidities of coronavirus disease 2019 (COVID-19), has been suspected to be associated with adverse outcomes in COVID-19 patients, but their correlation remains controversial.
Method
This is a quantitative meta-analysis on the basis of adjusted effect estimates. PubMed, Web of Science, MedRxiv, Scopus, Elsevier ScienceDirect, Cochrane Library and EMBASE were searched comprehensively to obtain a complete data source up to January 7, 2021. Pooled effects (hazard ratio (HR), odds ratio (OR)) and the 95% confidence intervals (CIs) were estimated to evaluate the risk of the adverse outcomes in COVID-19 patients with CVD. Heterogeneity was assessed by Cochran’s Q-statistic, I2test, and meta-regression. In addition, we also provided the prediction interval, which was helpful for assessing whether the variation across studies was clinically significant. The robustness of the results was evaluated by sensitivity analysis. Publication bias was assessed by Begg’s test, Egger’s test, and trim-and-fill method.
Result
Our results revealed that COVID-19 patients with pre-existing CVD tended more to adverse outcomes on the basis of 203 eligible studies with 24,032,712 cases (pooled ORs = 1.41, 95% CIs: 1.32-1.51, prediction interval: 0.84-2.39; pooled HRs = 1.34, 95% CIs: 1.23-1.46, prediction interval: 0.82-2.21). Further subgroup analyses stratified by age, the proportion of males, study design, disease types, sample size, region and disease outcomes also showed that pre-existing CVD was significantly associated with adverse outcomes among COVID-19 patients.
Conclusion
Our findings demonstrated that pre-existing CVD was an independent risk factor associated with adverse outcomes among COVID-19 patients.
Similar content being viewed by others
Introduction
Since December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a global outbreak of coronavirus disease 2019 (COVID-19). Currently, the pandemic has affected more than 127,319,002 people in more than 200 countries and killed more than 2,785,838 people (https://www.who.int/emergencies/diseases/novel-coronavirus-2019). Previous studies have reported that several pre-existing medical conditions, such as hypertension, diabetes and so on, might accelerate disease progression of COVID-19 [1,2,3]. Cardiovascular disease (CVD), one of the most common comorbidities of COVID-19, has been observed to be associated with adverse outcomes among COVID-19 patients by Li et al. in a meta-analysis study [4]. Nevertheless, it is worth noting that the results of Li et al.’s study were based on the unadjusted effect estimates [4]. It is reported that age, sex, and co-existing diseases are known to affect the outcomes of COVID-19 patients [5,6,7], which may modulate the association between CVD and adverse outcomes in COVID-19 patients. Moreover, Zhou et al. observed that coronary heart disease (CHD), one of CVD, was strongly correlated with an increased risk of in-hospital mortality among COVID-19 patients in univariable analysis (odds ratio (OR) = 21.4, 95% confidence interval (CI): 4.64-98.76), but no significant correlation was observed in multivariable analysis (OR = 2.14, 95% CI: 0.26-17.79) [8]. The similar results were also observed by Robilotti et al. [9] and Louapre et al. [10]. Therefore, it is necessary to clarify whether pre-existing CVD was an independent risk factor associated with adverse outcomes in COVID-19 patients. In this study, we performed a quantitative meta-analysis on the basis of adjusted effect estimates.
Methods
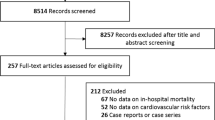
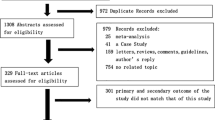
This is a quantitative meta-analysis on the basis of adjusted effect estimates. Admittedly, our study was not registered, but our meta-analysis was made in strict accordance with the process of systematic evaluation (Fig. 1). Moreover, our study is less likely to be biased by artificial bias because this study was carried out rigorously in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (Online supplemental Table A1) [11].
Literature search strategy
The databases of PubMed, Web of Science, MedRxiv, Scopus, Elsevier ScienceDirect, Cochrane Library and Embase were searched to obtain a complete data source up to January 7, 2021. The search strategies were as follows: (“COVID-19” OR “coronavirus disease 2019” OR “SARS-CoV-2” OR “2019-nCoV”) AND (“cardiovascular disease” OR “coronary heart disease” OR “cardiac disease” OR “heart disease” OR “heart failure” OR “coronary artery disease”) AND (“outcome” OR “severe” OR “critical” OR “severity” OR “fatality” OR “mortality” OR “death” OR “adverse outcome” OR “poor outcome” OR “clinical characteristics”). All the terms matched the MesH browser. Beyond that, the relevant references of preceding studies were also taken into account.
Eligibility criteria
The criteria for including studies were: (1) Subjects should be laboratory-confirmed COVID-19 patients; (2) Studies should report the correlation between CVD and COVID-19 patients and the data are available; (3) Studies should be published in English; (4) Studies should include the multivariate analysis. The studies with the largest sample size were selected for inclusion when studies were conducted in the same hospital and the overlapping period. There was no restriction for region of study. The exclusion criteria included case reports, review papers, comments, errata, repeated studies, studies only reporting the characteristics of COVID-19 patients with CVD, and studies without available full text.
Data extraction and quality assessment
Data were extracted independently by two investigators (J.X. and W.X.), including the following information: the first author, source of data, country, date of data collection, number of patients, mean/median age, the percent of males, study design, the percent of COVID-19 patients with CVD, adjusted effect estimates (hazard ratio (HR) or OR) and adjusted risk factors. When both OR and HR existed in the same article, it was preferred to include HR because cox regression took time into account. Two researchers negotiated to resolve it in case of any issues not covered by the criteria and Y.W. acted as arbiter. The quality of the included studies was evaluated by investigators according to the Newcastle-Ottawa Scale [12]. High-quality studies referred to studies with a score above 7.
Data synthesis
The major information such as study design and effect estimates were directly extracted from original articles. The research type of some articles was not clear and some articles provided both OR and HR. Besides, the calculation methods of HR and OR are different. The calculation of HR takes into account the concept of time, and OR is the approximate value of risk ratio. Therefore, pooled HR, OR and 95% confidence intervals (CIs) were separately calculated to address the risk of adverse outcomes in COVID-19 patients with a history of CVD. Heterogeneity was assessed by Cochran’s Q-statistic and I2 test, if no significant heterogeneity was observed (I2 ≤ 50%, P > 0.1), a fixed-effects model was adopted; otherwise, a random-effects model was applied [13]. In addition, we also provided the prediction interval, which was helpful for assessing whether the variation across studies was clinically significant [14, 15]. The robustness of the results was evaluated by sensitivity analysis which omitted one study at a time. Publication bias was assessed by Begg’s test [16], Egger’s test [17] and trim-and-fill method [18]. Subgroup analysis and meta-regression were conducted to determine the source of heterogeneity. Data analyses were conducted using Stata, version 12.0 (meta-program) and R, version 3.6.1 (netmeta package). A two-tailed P-value < 0.05 was regarded as significant.
Results
The flow chart of selection process is shown in Fig. 1. 5,025 records were retrieved after removing 23,826 duplicates, of which 245 studies were full-text assessed. Eventually, a total of 203 eligible studies with 24,032,712 patients were enrolled in our meta-analysis [2, 3, 8, 9, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210, 212,213,214,215,216,217,218]. 81 studies originated from Europe, 54 studies came from North America, 61 from Asia, 2 from Australia, and the remained 5 were not just from one country (Table 1). Among these studies, cardiac disease was mentioned in 63 studies, HF was involved in 35 studies, and CAD was involved in 35 studies (Table 2). Adjusted HR was reported in 65 studies and adjusted OR was reported in 138 studies (Table 2). The main characteristics of the selected studies are summarized in Table 1.
Totally, our results revealed that COVID-19 patients who suffered from CVD tended more to adverse outcomes (pooled ORs = 1.41, 95% CIs: 1.32-1.51, prediction interval: 0.84-2.39; pooled HRs = 1.34, 95% CIs: 1.23-1.46, prediction interval: 0.82-2.21 Fig. 2). Subgroup analysis by sample size showed consistent results (pooled HRs = 1.16, 95% CIs: 1.03-1.32, prediction interval: 0.66-2.04; pooled ORs = 1.41, 95% CIs: 1.32-1.51, prediction interval: 0.84-2.39 for sample size >= 1000; pooled HRs = 1.63, 95% CIs: 1.41-1.88, prediction interval: 0.86-3.10; pooled ORs: 1.57, 95% CIs: 1.40-1.77, prediction interval: 0.84-2.95 for sample size < 1000; Table 2 and Fig. A1). The positive association between pre-existing CVD and adverse outcomes in COVID-19 patients was also observed in subgroup analysis by disease types (Table 2 and Fig. A2): cardiac disease (pooled HRs = 1.40, 95% CIs: 1.17-1.69, prediction interval: 0.68-2.90; pooled ORs = 1.43, 95% CIs: 1.25-1.64, prediction interval: 0.80-2.55), HF (pooled HRs = 1.23, 95% CIs: 1.05-1.44, prediction interval: 0.63-2.39; pooled ORs = 1.46, 95% CIs: 1.31-1.62, prediction interval: 1.01-2.10), and CAD (pooled HRs = 1.48, 95% CIs: 1.14-1.93, prediction interval: 0.67-3.29; pooled ORs = 1.17, 95% CIs:1.02-1.35, prediction interval: 0.75-1.83). In addition, subgroup analyses stratified by age, the proportion of males, region, disease outcomes and study design supported the above positive associations (Table 2 and Fig. A3-7). Sensitivity analysis indicated that our result was robust (Fig. 3A and B). There was no publication bias was detected by Begg’s test (OR: P = 0.233, HR: P = 0.054; Fig. 4A and B), while significant publication bias was found by Egger’s test (OR: P = 0.000, HR: P = 0.000; Fig. 4C and D). Therefore, the trim-and-fill method was adopted for further analysis. The results for HR showed that with the addition of 21 more studies, the results of the meta-analysis would be more robust but not reversed (pooled HRs = 1.11, 95% CIs: 1.01-1.14, fixed-effects model; pooled HRs = 1.16, 95% CIs: 1.06-1.26, random-effects model), and the OR results (pooled ORs: 1.18, 95% CIs: 1.16-1.20, fixed-effects model; pooled ORs: 1.21, 95% CIs: 1.12-1.30, random-effects model) showed that the results would be equally robust after adding 29 studies. However, there was high heterogeneity in our study. To find sources of heterogeneity, we conducted a meta-regression. However, adjustments for multivariate regression coefficients for sample size, age, proportion of males, study design, region, disease types, disease outcomes were not statistically significant (Table 3), suggesting that these were not sources of heterogeneity identified.
Discussion
Many countries have been hit by the pandemic caused by SARS-CoV-2, numerous people lost their lives because of this. Meanwhile, health systems in every country were under so unprecedented strain that it was very important to find an effective marker to help implement bed grading management. What called for special attention was that earlier studies have shown COVID-19 patients with at least one underlying conditions, such as chronic kidney disease, HIV, diabetes and other comorbidities, have a poor disease course [2, 29, 211, 219, 220], which means that those patients with underlying diseases should be monitored more carefully in case of disease getting worse. Furthermore, it was reported that the risk of primary respiratory syndrome severity and adverse outcomes was increased in Middle East respiratory syndrome (MERS) patients with pre-existing CVD. The research by Li et al. [8] with unadjusted effect estimates showed that there was a positive association between CVD and adverse outcomes in patients with COVID-19, but the association might be confounded by other factors such as age, gender and comorbidities. Thus, we performed a quantitative meta-analysis on the basis of adjusted effect estimates to clarify whether pre-existing CVD was an independent risk factor associated with adverse outcomes in COVID-19 patients.
Our results based on adjusted effect estimates revealed that pre-existing CVD was significantly related to adverse outcomes in COVID-19 patients on the basis of 203 eligible studies with 24,032,712 cases. The significant association between pre-existing CVD and adverse outcomes in COVID-19 patients was still existent in further subgroup analyses stratified by the proportion of males, study design, disease types, sample size, region and disease outcomes, which suggests that our findings are relatively stable.
Similar to other meta-analyses, several limitations should be acknowledged in this present study. Firstly, data on drug and supportive treatments are not clear in the selected studies presently, thus, we could not evaluate the effects of treatments on the association between co-existing CVD and adverse outcomes in COVID-19 patients. Secondly, statistically significant results were more likely to be accepted and published than non-statistically significant results in similar studies, but in fact, the data of the meta-analysis mainly derived from the studies which have been published, which may lead to publication bias. Thirdly, the causal relationship of CVD and adverse outcomes in patients with COVID-19 cannot be confirmed on account of the inherent limitation of the observational study. Therefore, well-designed studies with larger sample sizes are needed for further verification.
Conclusions
In conclusion, our findings indicated that pre-existing CVD was an independent risk factor associated with adverse outcomes among COVID-19 patients. COVID-19 patients with a history of CVD might need more attention.
Availability of data and materials
All data relevant to the study are included in the article or uploaded as supplementary information.
Abbreviations
- CVD:
-
Cardiovascular disease
- COVID-19:
-
Coronavirus disease 2019
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- HR:
-
Hazard ratio
- CHD:
-
Coronary heart disease
- CAD:
-
Coronary artery disease
- HIV:
-
Human immunodeficiency virus
- MesH:
-
Medical Subject Headings
- HF:
-
Heart failure
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analysis
References
Liang X, Shi L, Wang Y, Xiao W, Duan G, Yang H, et al. The association of hypertension with the severity and mortality of COVID-19 patients: evidence based on adjusted effect estimates. J Infect. 2020; https://doi.org/10.1016/j.jinf.2020.1006.1060.
Cen Y, Chen X, Shen Y, Zhang XH, Lei Y, Xu C, et al. Risk factors for disease progression in patients with mild to moderate coronavirus disease 2019-a multi-centre observational study. Clin Microbiol Infect. 2020; https://doi.org/10.1016/j.cmi.2020.1005.1041.
Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet (London, England). 2020;395(10239):1763–70.
Li X, Guan B, Su T, Liu W, Chen M, Waleed KB, et al. Impact of cardiovascular disease and cardiac injury on in-hospital mortality in patients with COVID-19: a systematic review and meta-analysis. Heart. 2020;106(15):1142–7.
Borghesi A, Zigliani A, Masciullo R, Golemi S, Maculotti P, Farina D, et al. Radiographic severity index in COVID-19 pneumonia: relationship to age and sex in 783 Italian patients. Radiol Med. 2020;125(5):461–4.
Jones J, Sullivan PS, Sanchez TH, Guest JL, Hall EW, Luisi N, et al. Similarities and Differences in COVID-19 Awareness, Concern, and Symptoms by Race and Ethnicity in the United States: Cross-Sectional Survey. J Med Int Res. 2020;22(7):e20001.
Mustafa NM. L AS: Characterisation of COVID-19 Pandemic in Paediatric Age Group: A Systematic Review and Meta-Analysis. J Clin Virol. 2020;128:104395.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England). 2020;395(10229):1054–62.
Robilotti EV, Babady NE, Mead PA, Rolling T, Perez-Johnston R, Bernardes M, et al. Determinants of COVID-19 disease severity in patients with cancer. Nat Med. 2020;26(8):1218–23.
Louapre C, Collongues N, Stankoff B, Giannesini C, Papeix C, Bensa C, et al. Clinical characteristics and outcomes in patients with coronavirus disease 2019 and multiple sclerosis. JAMA Neurol. 2020;77(9):1079.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol Rev. 1987;9:1–30.
IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7):e010247.
Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I(2) is not an absolute measure of heterogeneity. Res Synth Methods. 2017;8(1):5–18.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Schwarzer G, Carpenter J, Rücker G. Empirical evaluation suggests Copas selection model preferable to trim-and-fill method for selection bias in meta-analysis. J Clin Epidemiol. 2010;63(3):282–8.
Yu X, Sun X, Cui P, Pan H, Lin S, Han R, et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai, China. Transbound Emerg Dis. 2020;67(4):1697–707.
Zhao M, Wang M, Zhang J, Gu J, Zhang P, Xu Y, et al. Comparison of clinical characteristics and outcomes of patients with coronavirus disease 2019 at different ages. Aging. 2020;12(11):10070–86.
Sabri A, Davarpanah AH, Mahdavi A, Abrishami A, Khazaei M, Heydari S, et al. Novel coronavirus disease 2019: predicting prognosis with a computed tomography-based disease severity score and clinical laboratory data. Pol Arch Intern Med. 2020;130(7-8):629–34.
Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. JAm Coll Cardiol. 2020;76(5):533–46.
Ciceri F, Castagna A, Rovere-Querini P, De Cobelli F, Ruggeri A, Galli L, et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol. 2020;217:108509.
Barman HA, Atici A, Sahin I, Alici G, Tekin EA, Baycan OF, et al. Prognostic significance of cardiac injury in COVID-19 patients with and without coronary artery disease. Coron Artery Dis. 2020; Publish Ahead of Print.
Bravi F, Flacco ME, Carradori T, Volta CA, Cosenza G, De Togni A, et al. Predictors of severe or lethal COVID-19, including angiotensin converting enzyme inhibitors and angiotensin II receptor blockers, in a sample of infected Italian citizens. PLOS ONE. 2020;15(6):e0235248.
Deiana G, Azara A, Dettori M, Delogu F, Vargiu G, Gessa G, et al. Deaths in SARS-Cov-2 positive patients in Italy: the influence of underlying health conditions on lethality. Int J Environ Res Public Health. 2020;17(12):4450.
Zhang C, Qin L, Li K, Wang Q, Zhao Y, Xu B, et al. A novel scoring system for prediction of disease severity in COVID-19. Front Cell Infect Microbiol. 2020;10:318.
Nie Y, Li J, Huang X, Guo W, Zhang X, Ma Y, et al. Epidemiological and clinical characteristics of 671 COVID-19 patients in Henan Province, China. Int J Epidemiol. 2020;49(4):1085–95.
Hashemi N, Viveiros K, Redd WD, Zhou JC, McCarty TR, Bazarbashi AN, et al. Impact of chronic liver disease on outcomes of hospitalized patients with COVID‐19: a multicentre United States experience. Liver Int. 2020;40(10):2515–21.
Lanza E, Muglia R, Bolengo I, Santonocito GO, Lisi C, Angelotti G, et al. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Euro Radiol. 2020;30(12):6770–8.
Zeng Z, Ma Y, Zeng H, Huang P, Liu W, Jiang M, et al. Simple nomogram based on initial laboratory data for predicting the probability of ICU transfer of COVID‐19 patients: multicenter retrospective study. J Med Virol. 2021;93(1):434–40.
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell LF, Chernyak Y, et al. Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York City. BMJ. 2020;369:m1966.
Arshad S, Kilgore P, Chaudhry ZS, Jacobsen G, Wang DD, Huitsing K, et al. Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19. IJID. 2020;97:396–403.
San Roman JA, Uribarri A, Amat-Santos IJ, Aparisi A, Catala P, Gonzalez-Juanatey JR. The presence of heart disease worsens prognosis in patients with COVID-19. Rev Esp Cardiol. 2020;73(9):773–5.
Cheng B, Hu J, Zuo X, Chen J, Li X, Chen Y, et al. Predictors of progression from moderate to severe coronavirus disease 2019: a retrospective cohort. Clin Microbiol Infect. 2020;26(10):1400–5.
Oussalah A, Gleye S, Urmes IC, Laugel E, Callet J, Barbé F, et al. Long-term ACE inhibitor/ARB use is associated with severe renal dysfunction and acute kidney injury in patients with severe COVID-19: results from a referral center cohort in the Northeast of France. Clin Infect Dis. 2020.
Kim DW, Byeon KH, Kim J, Cho KD, Lee N. The correlation of comorbidities on the mortality in patients with COVID-19: an observational study based on the Korean national health insurance big data. J Korean Med Sci. 2020;35(26).
Chen J, Bai H, Liu J, Chen G, Liao Q, Yang J, et al. Distinct clinical characteristics and risk factors for mortality in female inpatients with coronavirus disease 2019 (COVID-19): a sex-stratified, large-scale cohort study in Wuhan, China. Clin Infect Dis. 2020;71(12):3188–95.
Ferrante G, Fazzari F, Cozzi O, Maurina M, Bragato R, D’Orazio F, et al. Risk factors for myocardial injury and death in patients with COVID-19: insights from a cohort study with chest computed tomography. Cardiovasc Res. 2020;116(14):2239–46.
Rastad H, Karim H, Ejtahed HS, Tajbakhsh R, Noorisepehr M, Babaei M, et al. Risk and predictors of in-hospital mortality from COVID-19 in patients with diabetes and cardiovascular disease. Diabetol Metab Syndr. 2020;12:57.
Hwang JM, Kim JH, Park JS, Chang MC, Park D. Neurological diseases as mortality predictive factors for patients with COVID-19: a retrospective cohort study. Neurol Sci. 2020;41(9):2317–24.
Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Int Med. 2020;180(10):1345.
Deng P, Ke Z, Ying B, Qiao B, Yuan L. The diagnostic and prognostic role of myocardial injury biomarkers in hospitalized patients with COVID-19. Int J Clin Chem. 2020;510:186–90.
Al‐Salameh A, Lanoix AP, Bennis Y, Andrejak C, Brochot E, Deschasse G, et al. Characteristics and outcomes of ‐19 in hospitalized patients with and without diabetes. Diab/Metab Res Rev. 2021;37(3).
Atkins JL, Masoli JAH, Delgado J, Pilling LC, Kuo CL, Kuchel GA, et al. Preexisting comorbidities predicting COVID-19 and mortality in the UK biobank community cohort. J Gerontol Ser A. 2020;75(11):2224–30.
Yao JS, Paguio JA, Dee EC, Tan HC, Moulick A, Milazzo C, et al. The minimal effect of zinc on the survival of hospitalized patients with COVID-19. Chest. 2021;159(1):108–11.
Pinto C, Berselli A, Mangone L, Damato A, Iachetta F, Foracchia M, et al. SARSCoV-2 positive hospitalized cancer patients during the Italian Outbreak: the cohort study in Reggio Emilia. Biology. 2020;9(8):181.
Chilimuri S, Sun H, Alemam A, Mantri N, Shehi E, Tejada J, et al. Predictors of mortality in adults admitted with COVID-19: retrospective cohort study from New York City. Western J Emerg Med. 2020;21(4):779–84.
Lian J, Jin C, Hao S, Zhang X, Yang M, Jin X, et al. High neutrophil-to-lymphocyte ratio associated with progression to critical illness in older patients with COVID-19: a multicenter retrospective study. Aging. 2020;12(14):13849–59.
Zhao Z, Chen A, Hou W, Graham JM, Li H, Richman PS, et al. Prediction model and risk scores of ICU admission and mortality in COVID-19. PloS one. 2020;15(7):e0236618.
Wang L, Foer D, Bates DW, Boyce JA, Zhou L. Risk factors for hospitalization, intensive care, and mortality among patients with asthma and COVID-19. J Allergy Clin Immunol. 2020;146(4):808–12.
Garcia-Azorin D, Martinez-Pias E, Trigo J, Hernandez-Perez I, Valle-Penacoba G, Talavera B, et al. Neurological comorbidity is a predictor of death in Covid-19 disease: a cohort study on 576 patients. Front Neurol. 2020;11:781.
Alkhatib AL, Kreniske J, Zifodya JS, Fonseca V, Tahboub M, Khatib J, et al. BMI is associated with coronavirus disease 2019 intensive care unit admission in African Americans. Obesity. 2020;28(10):1798–801.
Hernández-Galdamez DR, González-Block MÁ, Romo-Dueñas DK, Lima-Morales R, Hernández-Vicente IA, Lumbreras-Guzmán M, et al. Increased risk of hospitalization and death in patients with COVID-19 and pre-existing noncommunicable diseases and modifiable risk factors in Mexico. Arch Med Res. 2020;51(7):683–9.
Bellmann-Weiler R, Lanser L, Barket R, Rangger L, Schapfl A, Schaber M, et al. Prevalence and predictive value of anemia and dysregulated iron homeostasis in patients with COVID-19 infection. J Clin Med. 2020;9(8):2429.
Berenguer J, Ryan P, Rodríguez-Baño J, Jarrín I, Carratalà J, Pachón J, et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin Microbiol Infect. 2020;26(11):1525–36.
Gottlieb M, Sansom S, Frankenberger C, Ward E, Hota B, Jang T. Clinical course and factors associated with hospitalization and critical illness among COVID‐19 patients in Chicago, Illinois. Acad Emerg Med. 2020;27(10):963–73.
Agarwal S, Schechter C, Southern W, Crandall JP, Tomer Y. Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019. Diabetes Care. 2020;43(10):2339–44.
Shang Y, Liu T, Wei Y, Li J, Shao L, Liu M, et al. Scoring systems for predicting mortality for severe patients with COVID-19. E Clin Med. 2020;24:100426.
Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802.
Posso M, Comas M, Román M, Domingo L, Louro J, González C, et al. Comorbidities and mortality in patients with COVID-19 aged 60 years and older in a University Hospital in Spain. Arch Bronconeumol. 2020;56(11):756–8.
Shu L, Wang X, Li M, Chen X, Ji N, Shi L, et al. Clinical characteristics of moderate COVID‐19 patients aggravation in Wuhan Stadium Cabin Hospital: A 571 cases of retrospective cohort study. J Med Virol. 2021;93(2):1133–40.
Parra-Bracamonte GM, Lopez-Villalobos N, Parra-Bracamonte FE. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann Epidemiol. 2020;52:93–98.e2.
Pablos JL, Galindo M, Carmona L, Lledó A, Retuerto M, Blanco R, et al. Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study. Ann Rheum Dis. 2020;79(12):1544–9.
Zhang B, Liu S, Lu Z, Dong Y, Zhang S. Previous cardiovascular surgery significantly increases the risk of developing critical illness in patients with COVID-19. J Infect. 2021;82(2):282–327.
Fox T, Ruddiman K, Lo KB, Peterson E, DeJoy R, Salacup G, et al. The relationship between diabetes and clinical outcomes in COVID-19: a single-center retrospective analysis. Acta Diabetol. 2021;58(1):33–8.
Vena A, Giacobbe DR, Di Biagio A, Mikulska M, Taramasso L, De Maria A, et al. Clinical characteristics, management and in-hospital mortality of patients with coronavirus disease 2019 in Genoa, Italy. Clin Microbiol Infect. 2020;26(11):1537–44.
Ng JH, Hirsch JS, Wanchoo R, Sachdeva M, Sakhiya V, Hong S, et al. Outcomes of patients with end-stage kidney disease hospitalized with COVID-19. Kidney Int. 2020. https://doi.org/10.1016/j.kint.2020.1007.1030.
He F, Luo Q, Lei M, Fan L, Shao X, Huang G, et al. Risk factors for severe cases of COVID-19: a retrospective cohort study. Aging. 2020;12(15):15730–40.
Gupta A, Madhavan MV, Poterucha TJ, DeFilippis EM, Hennessey JA, Redfors B, et al. Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Res Sq [Preprint]. 2020:rs.3.rs-56210.
Czernichow S, Beeker N, Rives-Lange C, Guerot E, Diehl JL, Katsahian S, et al. Obesity doubles mortality in patients hospitalized for severe acute respiratory syndrome coronavirus 2 in Paris hospitals, France: a cohort study on 5,795 patients. Obesity. 2020;28(12):2282–9.
Sisó-Almirall A, Kostov B, Mas-Heredia M, Vilanova-Rotllan S, Sequeira-Aymar E, Sans-Corrales M, et al. Prognostic factors in Spanish COVID-19 patients: a case series from Barcelona. PloS one. 2020;15(8):e0237960.
Brenner H, Holleczek B, Schöttker B. Vitamin D insufficiency and deficiency and mortality from respiratory diseases in a cohort of older adults: Potential for limiting the death toll during and beyond the COVID-19 pandemic? Nutrients. 2020;12(8):1–11.
De Rossi N, Scarpazza C, Filippini C, Cordioli C, Rasia S, Mancinelli CR, et al. Early use of low dose tocilizumab in patients with COVID-19: a retrospective cohort study with a complete follow-up. E Clin Med. 2020;25:100459.
Nimkar A, Naaraayan A, Hasan A, Pant S, Durdevic M, Suarez CN, et al. Incidence and risk factors for acute kidney injury and its effect on mortality in patients hospitalized from COVID-19. Mayo Clin Proc Innov Qual Outcomes. 2020;4(6):687–95.
Klang E, Soffer S, Nadkarni G, Glicksberg B, Freeman R, Horowitz C, et al. Sex differences in age and comorbidities for COVID-19 mortality in urban New York City. SN Compr Clin Med. 2020;2(9):1319–22.
Emami A, Javanmardi F, Akbari A, Kojuri J, Bakhtiari H, Rezaei T, et al. Survival rate in hypertensive patients with COVID-19. Clin Exper Hypertens. 2021;43(1):77–80.
Liu D, Cui P, Zeng S, Wang S, Feng X, Xu S, et al. Risk factors for developing into critical COVID-19 patients in Wuhan, China: a multicenter, retrospective, cohort study. EClinicalMedicine. 2020;25:100471.
Rossi PG, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R, et al. Characteristics and outcomes of a cohort of COVID-19 patients in the Province of Reggio Emilia, Italy. PLOS ONE. 2020;15(8):e0238281.
Feng X, Li P, Ma L, Liang H, Lei J, Li W, et al. Clinical characteristics and short-term outcomes of severe patients with COVID-19 in Wuhan, China. Front Med. 2020;7:491.
Li G, Deng Q, Feng J, Li F, Xiong N, He Q. Clinical characteristics of diabetic patients with COVID-19. J Diab Res. 2020;2020:1652403.
Seiglie J, Platt J, Cromer SJ, Bunda B, Foulkes AS, Bassett IV, et al. Diabetes as a risk factor for poor early outcomes in patients hospitalized with COVID-19. Diab Care. 2020;43(12):2938–44.
Tural Onur S, Altın S, Sokucu SN, Fikri B, Barça T, Bolat E, et al. Could ferritin level be an indicator of COVID-19 disease mortality? J Med Virol. 2021;93(3):1672–7.
Anzola GP, Bartolaminelli C, Gregorini GA, Coazzoli C, Gatti F, Mora A, et al. Neither ACEIs nor ARBs are associated with respiratory distress or mortality in COVID-19 results of a prospective study on a hospital-based cohort. Intern Emerg Med. 2020;15(8):1477–84.
Ioannou GN, Locke E, Green P, Berry K, O'Hare AM, Shah JA, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US veterans with SARS-CoV-2 infection. JAMA Netw Open. 2020;3(9):e2022310.
Bahl A, Van Baalen MN, Ortiz L, Chen NW, Todd C, Milad M, et al. Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort. Intern Emerg Med. 2020;15(8):1485–99.
Rafi K, Patrik Brodin N, Maron MI, Guha C, Kalnicki S, Garg MK, et al. Association of race and ethnicity with comorbidities and survival among patients with COVID-19 at an Urban Medical Center in New York. JAMA Network Open. 2020;3(9):e2019795.
Jackson BR, Gold JAW, Natarajan P, Rossow J, Fanfair RN, da Silva J, et al. Predictors at admission of mechanical ventilation and death in an observational cohort of adults hospitalized with coronavirus disease 2019. Clin Infect Dis. 2020.
Desai A, Voza G, Paiardi S, Teofilo FI, Caltagirone G, Pons MR, et al. The role of anti-hypertensive treatment, comorbidities and early introduction of LMWH in the setting of COVID-19: A retrospective, observational study in Northern Italy. Int J Cardiol. 2021;324:249–54.
Wang X, Liu Z, Li J, Zhang J, Tian S, Lu S, et al. Impacts of type 2 diabetes on disease severity, therapeutic effect, and mortality of patients with COVID-19. J Clin Endocrinol Metab. 2020;105(12):e4219–29.
Solerte SB, D'Addio F, Trevisan R, Lovati E, Rossi A, Pastore I, et al. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study. Diab Care. 2020;43(12):2999–3006.
Hayek SS, Brenner SK, Azam TU, Shadid HR, Anderson E, Berlin H, et al. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ. 2020;371:m3513.
Chen R, Yang J, Gao X, Ding X, Yang Y, Shen Y, et al. Influence of blood pressure control and application of renin-angiotensin-aldosterone system inhibitors on the outcomes in COVID-19 patients with hypertension. J Clin Hypertens. 2020;22(11):1974–83.
Lee JH, Kim YC, Cho SH, Lee J, You SC, Song YG, et al. Effect of sex hormones on coronavirus disease 2019: an analysis of 5,061 laboratory-confirmed cases in South Korea. Menopause. 2020;27(12):1376–81.
Nachega JB, Ishoso DK, Otokoye JO, Hermans MP, Machekano RN, Sam-Agudu NA, et al. Clinical characteristics and outcomes of patients hospitalized for COVID-19 in Africa: early insights from the Democratic Republic of the Congo. Am J Trop Med Hyg. 2020;103(6):2419–28.
Rozaliyani A, Savitri AI, Setianingrum F, Shelly TN, Ratnasari V, Kuswindarti R, et al. Factors associated with death in COVID-19 patients in Jakarta, Indonesia: an epidemiological study. Acta Med Indones. 2020;52(3):246–54.
Wang Z, Ye D, Wang M, Zhao M, Li D, Ye J, et al. Clinical features of COVID-19 patients with different outcomes in Wuhan: a retrospective observational study. BioMed Res Int. 2020;2020:2138387.
Liu L, Wang W, Yang K, Li S, Yu X, Dong C, et al. Glycemic control before admission is an important determinant of prognosis in patients with coronavirus disease 2019. J Diab Investig. 2021;12(6):1064–73.
Al Kuwari HM, Abdul Rahim HF, Abu-Raddad LJ, Abou-Samra A-B, Al Kanaani Z, Al Khal A, et al. Epidemiological investigation of the first 5685 cases of SARS-CoV-2 infection in Qatar, 28 February–18 April 2020. BMJ Open. 2020;10(10):e040428.
Balbi M, Caroli A, Corsi A, Milanese G, Surace A, Di Marco F, et al. Chest X-ray for predicting mortality and the need for ventilatory support in COVID-19 patients presenting to the emergency department. Eur Radiol. 2021;31(4):1999–2012.
Calmes D, Graff S, Maes N, Frix AN, Thys M, Bonhomme O, et al. Asthma and COPD are not risk factors for ICU stay and death in case of SARS-CoV2 infection. J Allergy Clin Immunol Pract. 2021;9(1):160–9.
Talavera B, García-Azorín D, Martínez-Pías E, Trigo J, Hernández-Pérez I, Valle-Peñacoba G, et al. Anosmia is associated with lower in-hospital mortality in COVID-19. J Neurol Sci. 2020;419:117163.
Zinellu A, Arru F, De Vito A, Sassu A, Valdes G, Scano V, et al. The De Ritis ratio as prognostic biomarker of in‐hospital mortality in COVID‐19 patients. Eur J Clin Investig. 2021;51(1).
Mallow PJ, Belk KW, Topmiller M, Hooker EA. Outcomes of hospitalized COVID-19 patients by risk factors: results from a United States hospital claims database. J Health Econ Outcomes Res. 2020;7(2):165–74.
Abbasi B, Akhavan R, Khameneh AG, Zandi B, Farrokh D, Rad MP, et al. Evaluation of the relationship between inpatient COVID-19 mortality and chest CT severity score. Am J Emerg Med. 2020.
Craig-Schapiro R, Salinas T, Lubetzky M, Abel BT, Sultan S, Lee JR, et al. COVID-19 outcomes in patients waitlisted for kidney transplantation and kidney transplant recipients. Am J Transplant. 2021;21(4):1576–85.
Ryan C, Minc A, Caceres J, Balsalobre A, Dixit A, Ng BKP, et al. Predicting severe outcomes in Covid-19 related illness using only patient demographics, comorbidities and symptoms. Am J Emerg Med. 2020.
Serin I, Sari ND, Dogu MH, Acikel SD, Babur G, Ulusoy A, et al. A new parameter in COVID-19 pandemic: initial lactate dehydrogenase (LDH)/Lymphocyte ratio for diagnosis and mortality. J Infect Public Health. 2020;13(11):1664–70.
Cao Y, Han X, Gu J, Li Y, Liu J, Alwalid O, et al. Prognostic value of baseline clinical and HRCT findings in 101 patients with severe COVID-19 in Wuhan, China. Sci Rep. 2020;10(1):17543.
Gupta S, Coca SG, Chan L, Melamed ML, Brenner SK, Hayek SS, et al. AKI treated with renal replacement therapy in critically ill patients with COVID-19. JASN. 2021;32(1):161–76.
Raparelli V, Palmieri L, Canevelli M, Pricci F, Unim B, Lo Noce C, et al. Sex differences in clinical phenotype and transitions of care among individuals dying of COVID-19 in Italy. Biol Sex Differ. 2020;11(1):57.
Chinnadurai R, Ogedengbe O, Agarwal P, Money-Coomes S, Abdurrahman AZ, Mohammed S, et al. Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting- a cohort study. BMC Geriatr. 2020;20(1):409.
Rajter JC, Sherman MS, Fatteh N, Vogel F, Sacks J, Rajter JJ. Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the ivermectin in COVID nineteen study. Chest. 2021;159(1):85–92.
Naaraayan A, Nimkar A, Hasan A, Pant S, Durdevic M, Elenius H, et al. End-stage renal disease patients on chronic hemodialysis fare better with COVID-19: a retrospective cohort study from the New York Metropolitan Region. Cureus. 2020;12(9):e10373.
Cherri S, Lemmers DHL, Noventa S, Abu Hilal M, Zaniboni A. Outcome of oncological patients admitted with COVID-19: experience of a hospital center in northern Italy. Ther Adv Med Oncol. 2020;12:1758835920962370.
Rodríguez-Molinero A, Gálvez-Barrón C, Miñarro A, Macho O, López GF, Robles MT, et al. Association between COVID-19 prognosis and disease presentation, comorbidities and chronic treatment of hospitalized patients. PloS one. 2020;15(10):e0239571.
Clift AK, Coupland CAC, Keogh RH, Hemingway H, Hippisley-Cox J. COVID-19 mortality risk in down syndrome: results from a cohort study of 8 million adults. Ann Intern Med. 2021;174(4):572–6.
Clift AK, Coupland CAC, Keogh RH, Diaz-Ordaz K, Williamson E, Harrison EM, et al. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ. 2020;371:m3731.
Gamberini L, Tonetti T, Spadaro S, Zani G, Mazzoli CA, Capozzi C, et al. Factors influencing liberation from mechanical ventilation in coronavirus disease 2019: multicenter observational study in fifteen Italian ICUs. J Intensive Care. 2020;8:80.
Omrani AS, Almaslamani MA, Daghfal J, Alattar RA, Elgara M, Shaar SH, et al. The first consecutive 5000 patients with Coronavirus Disease 2019 from Qatar; a nation-wide cohort study. BMC Infect Dis. 2020;20(1):777.
Yahyavi A, Hemmati N, Derakhshan P, Banivaheb B, Behnagh AK, Tofighi R, et al. Angiotensin enzyme inhibitors and angiotensin receptor blockers as protective factors in COVID-19 mortality: a retrospective cohort study. Intern Emerg Med. 2021;16(4):883–93.
Guisado-Vasco P, Valderas-Ortega S, Carralón-González MM, Roda-Santacruz A, González-Cortijo L, Sotres-Fernández G, et al. Clinical characteristics and outcomes among hospitalized adults with severe COVID-19 admitted to a tertiary medical center and receiving antiviral, antimalarials, glucocorticoids, or immunomodulation with tocilizumab or cyclosporine: a retrospective observational study (COQUIMA cohort). EClinicalMedicine. 2020;28:100591.
Izzy S, Tahir Z, Cote DJ, Al Jarrah A, Roberts MB, Turbett S, et al. Characteristics and outcomes of latinx patients with COVID-19 in comparison with other ethnic and racial groups. Open Forum Infect Dis. 2020;7(10):ofaa401.
Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, et al. Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019. Anesth Analg. 2021;132(4):930–41.
Raines AM, Tock JL, McGrew SJ, Ennis CR, Derania J, Jardak CL, et al. Correlates of death among SARS-CoV-2 positive veterans: the contribution of lifetime tobacco use. Addict Behav. 2021;113:106692.
Ramos-Rincon JM, Buonaiuto V, Ricci M, Martín-Carmona J, Paredes-Ruíz D, Calderón-Moreno M, et al. Clinical characteristics and risk factors for mortality in very old patients hospitalized with COVID-19 in Spain. J Gerontol Ser A Biol Sci Med Sci. 2021;76(3):e28–37.
Zhang L, Fan T, Yang S, Feng H, Hao B, Lu Z, et al. Comparison of clinical characteristics of COVID-19 between elderly patients and young patients: a study based on a 28-day follow-up. Aging. 2020;12(20):19898–910.
de Souza CD, de Arruda Magalhães AJ, Lima AJ, Nunes DN, de Fátima Machado Soares É, de Castro Silva L, et al. Clinical manifestations and factors associated with mortality from COVID-19 in older adults: retrospective population-based study with 9807 older Brazilian COVID-19 patients. Geriatr Gerontol Int. 2020;20(12):1177–81.
Kolhe NV, Fluck RJ, Selby NM, Taal MW, Remuzzi G. Acute kidney injury associated with COVID-19: a retrospective cohort study. PLOS Med. 2020;17(10):e1003406.
Kim TS, Roslin M, Wang JJ, Kane J, Hirsch JS, Kim EJ. BMI as a risk factor for clinical outcomes in patients hospitalized with COVID-19 in New York. Obesity. 2021;29(2):279–84.
Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, et al. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2043–55.
An C, Lim H, Kim DW, Chang JH, Choi YJ, Kim SW. Machine learning prediction for mortality of patients diagnosed with COVID-19: a nationwide Korean cohort study. Sci Rep. 2020;10(1):18716.
Piazza G, Campia U, Hurwitz S, Snyder JE, Rizzo SM, Pfeferman MB, et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2060–72.
Rao X, Wu C, Wang S, Tong S, Wang G, Wu G, et al. The importance of overweight in COVID-19: A retrospective analysis in a single center of Wuhan, China. Medicine. 2020;99(43):e22766.
Tehrani S, Killander A, Åstrand P, Jakobsson J, Gille-Johnson P. Risk factors for death in adult COVID-19 patients: frailty predicts fatal outcome in older patients. IJID. 2021;102:415–21.
Hyman JB, Leibner ES, Tandon P, Egorova NN, Bassily-Marcus A, Kohli-Seth R, et al. Timing of intubation and in-hospital mortality in patients with coronavirus disease 2019. Crit Care Explor. 2020;2(10):e0254.
Hamilton P, Hanumapura P, Castelino L, Henney R, Parker K, Kumar M, et al. Characteristics and outcomes of hospitalised patients with acute kidney injury and COVID-19. PloS one. 2020;15(11):e0241544.
Liu J, Zhang S, Dong X, Li Z, Xu Q, Feng H, et al. Corticosteroid treatment in severe COVID-19 patients with acute respiratory distress syndrome. J Clin Invest. 2020;130(12):6417–28.
Ganatra S, Dani SS, Redd R, Rieger-Christ K, Patel R, Parikh R, et al. Outcomes of COVID-19 in patients with a history of cancer and comorbid cardiovascular disease. J Natl Compr Canc Netw. 2020:1–10.
Rubio-Rivas M, Corbella X, Mora-Luján JM, Loureiro-Amigo J, López Sampalo A, Yera Bergua C, et al. Predicting clinical outcome with phenotypic clusters in COVID-19 pneumonia: an analysis of 12,066 hospitalized patients from the Spanish registry SEMI-COVID-19. J Clin Med. 2020;9(11).
Mendes A, Serratrice C, Herrmann FR, Genton L, Périvier S, Scheffler M, et al. Predictors of in-hospital mortality in older patients with COVID-19: the COVIDAge study. J Am Med Dir Assoc. 2020;21(11):1546–1554.e1543.
Nemer DM, Wilner BR, Burkle A, Aguilera J, Adewumi J, Gillombardo C, et al. Clinical characteristics and outcomes of non-ICU hospitalization for COVID-19 in a nonepicenter, centrally monitored healthcare system. J Hosp Med. 2021;16(1):7–14.
Guo T, Shen Q, Zhou Z, Li J, Guo W, He W, et al. Combined interventions for severe novel coronavirus disease (COVID-19): experience from 350 patients. Infect Drug Resist. 2020;13:3907–18.
Hilbrands LB, Duivenvoorden R, Vart P, Franssen CFM, Hemmelder MH, Jager KJ, et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration. Nephrol Dial Transplant. 2020;35(11):1973–83.
Wang F, Cao J, Yu Y, Ding J, Eshak ES, Liu K, et al. Epidemiological characteristics of patients with severe COVID-19 infection in Wuhan, China: evidence from a retrospective observational study. Int J Epidemiol. 2021;49(6):1940–50.
Tang O, Bigelow BF, Sheikh F, Peters M, Zenilman JM, Bennett R, et al. Outcomes of nursing home COVID-19 patients by initial symptoms and comorbidity: results of universal testing of 1970 residents. J Am Med Dir Assoc. 2020;21(12):1767–1773.e1761.
Annweiler G, Corvaisier M, Gautier J, Dubée V, Legrand E, Sacco G, et al. Vitamin D supplementation associated to better survival in hospitalized frail elderly COVID-19 patients: the GERIA-COVID quasi-experimental study. Nutrients. 2020;12(11):3377.
Huang Y, Lyu X, Li D, Wang L, Wang Y, Zou W, et al. A cohort study of 676 patients indicates D-dimer is a critical risk factor for the mortality of COVID-19. PloS one. 2020;15(11):e0242045.
Poterucha TJ, Elias P, Jain SS, Sayer G, Redfors B, Burkhoff D, et al. Admission cardiac diagnostic testing with electrocardiography and troponin measurement prognosticates increased 30-day mortality in COVID-19. J Am Heart Assoc. 2021;10(1):e018476.
Li J, Zhang Y, Wang F, Liu B, Li H, Tang G, et al. Cardiac damage in patients with the severe type of coronavirus disease 2019 (COVID-19). BMC Cardiovasc Disord. 2020;20(1):479.
Prado-Galbarro FJ, Sanchez-Piedra C, Gamiño-Arroyo AE, Cruz-Cruz C. Determinants of survival after severe acute respiratory syndrome coronavirus 2 infection in Mexican outpatients and hospitalised patients. Public Health. 2020;189:66–72.
Shah C, Grando DJ, Rainess RA, Ayad L, Gobran E, Benson P, et al. Factors associated with increased mortality in hospitalized COVID-19 patients. Ann Med Surg (2012). 2020;60:308–13.
Botta M, Tsonas AM, Pillay J, Boers LS, Algera AG, Bos LDJ, et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med. 2021;9(2):139–48.
Di Domenico SL, Coen D, Bergamaschi M, Albertini V, Ghezzi L, Cazzaniga MM, et al. Clinical characteristics and respiratory support of 310 COVID-19 patients, diagnosed at the emergency room: a single-center retrospective study. Intern Emerg Med. 2020:1–10.
Ayaz A, Arshad A, Malik H, Ali H, Hussain E, Jamil B. Risk factors for intensive care unit admission and mortality in hospitalized COVID-19 patients. Acute Crit Care. 2020;35(4):249–54.
Hippisley-Cox J, Young D, Coupland C, Channon KM, Tan PS, Harrison DA, Rowan K, Aveyard P, Pavord ID, Watkinson PJ: Risk of severe COVID-19 disease with ACE inhibitors and angiotensin receptor blockers: cohort study including 8.3 million people. Heart 2020, 106(19):1503-1511.
Tomasoni D, Inciardi RM, Lombardi CM, Tedino C, Agostoni P, Ameri P, et al. Impact of heart failure on the clinical course and outcomes of patients hospitalized for COVID-19. Results of the Cardio-COVID-Italy multicentre study. Eur J Heart Fail. 2020;22(12):2238–47.
Elmunzer BJ, Wolf BJ, Scheiman JM, Tierney WM, Taylor JR. Association between preadmission acid suppressive medication exposure and severity of illness in patients hospitalized with COVID-19. Gastroenterology. 2021;160(4):1417–1422.e1414.
Polverino F, Stern DA, Ruocco G, Balestro E, Bassetti M, Candelli M, et al. Comorbidities, cardiovascular therapies, and COVID-19 mortality: a nationwide, italian observational study (ItaliCO). Front Cardiovasc Med. 2020;7.
Sharp AL, Huang BZ, Broder B, Smith M, Yuen G, Subject C, et al. Identifying patients with symptoms suspicious for COVID-19 at elevated risk of adverse events: The COVAS score. Am J Emerg Med. 2020.
Stebbing J, Sánchez Nievas G, Falcone M, Youhanna S, Richardson P, Ottaviani S, et al. JAK inhibition reduces SARS-CoV-2 liver infectivity and modulates inflammatory responses to reduce morbidity and mortality. Sci Adv. 2021;7(1).
Fu L, Li XY, Fei J, Xiang Y, Xiang HX, Li MD, et al. Myocardial injury at early stage and its association with the risk of death in COVID-19 patients: a hospital-based retrospective cohort study. Front Cardiovasc Med. 2020;7:590688.
Sheshah E, Sabico S, Albakr RM, Sultan AA, Alghamdi KS, Al Madani K, et al. Prevalence of diabetes, management and outcomes among Covid-19 adult patients admitted in a specialized tertiary hospital in Riyadh. Saudi Arabia. Diabetes Res Clin Pract. 2021;172:108538.
Bowe B, Cai M, Xie Y, Gibson AK, Maddukuri G, Al-Aly Z. Acute kidney injury in a national cohort of hospitalized US veterans with COVID-19. Clin J Am Soc Nephrol. 2020;16(1):14–25.
Cheng X, Cai G, Wen X, Gao L, Jiang D, Sun M, et al. Clinical characteristics and fatal outcomes of hypertension in patients with severe COVID-19. Aging. 2020;12(23):23436–49.
Neumann-Podczaska A, Chojnicki M, Karbowski LM, Al-Saad SR, Hashmi AA, Chudek J, et al. Clinical characteristics and survival analysis in a small sample of older COVID-19 patients with defined 60-day outcome. Int J Environ Res Public Health. 2020;17(22).
Ken-Dror G, Wade C, Sharma S, Law J, Russo C, Sharma A, et al. COVID-19 outcomes in UK centre within highest health and wealth band: a prospective cohort study. BMJ Open. 2020;10(11):e042090.
Iannelli A, Bouam S, Schneck AS, Frey S, Zarca K, Gugenheim J, et al. The impact of previous history of bariatric surgery on outcome of COVID-19. A nationwide medico-administrative French study. Obes Surg. 2020:1–9.
Sharifpour M, Rangaraju S, Liu M, Alabyad D, Nahab FB, Creel-Bulos CM, et al. C-Reactive protein as a prognostic indicator in hospitalized patients with COVID-19. PloS one. 2020;15(11):e0242400.
Martins-Filho PR, Antunes de Souza Araújo A, Pereira LX, Quintans-Júnior LJ, de Souza Barboza W, Cavalcante TF, et al. Factors associated with mortality among hospitalized patients with COVID-19: a retrospective cohort study. Am J Trop Med Hyg. 2021;104(1):103–5.
Lee SG, Park GU, Moon YR, Sung K. Clinical characteristics and risk factors for fatality and severity in patients with coronavirus disease in Korea: a nationwide population-based retrospective study using the Korean Health Insurance Review and Assessment Service (HIRA) database. Int J Environ Res Public Health. 2020;17(22).
Loffi M, Piccolo R, Regazzoni V, Di Tano G, Moschini L, Robba D, et al. Coronary artery disease in patients hospitalised with Coronavirus disease; 2019. (COVID-19) infection. Open Heart. 2020;7(2).
Grodecki K, Lin A, Razipour A, Cadet S, McElhinney PA, Chan C, et al. Epicardial adipose tissue is associated with extent of pneumonia and adverse outcomes in patients with COVID-19. Metabolism. 2021;115:154436.
Khan A, Althunayyan S, Alsofayan Y, Alotaibi R, Mubarak A, Arafat M, et al. Risk factors associated with worse outcomes in COVID-19: a retrospective study in Saudi Arabia. East Mediterr Health J. 2020;26(11):1371–80.
Rutten JJS, van Loon AM, van Kooten J, van Buul LW, Joling KJ, Smalbrugge M, et al. Clinical suspicion of COVID-19 in nursing home residents: symptoms and mortality risk factors. J Am Med Dir Assoc. 2020;21(12):1791–1797.e1791.
Schuelter-Trevisol F, Raimundo LJ, Soccas HD, Antunes AF, Mohr RLD, Marcon CEM, et al. Assessment of patients with COVID-19 hospitalized in southern Santa Catarina. Rev Soc Bras Med Trop. 2020;53:1–5.
Severity of COVID-19 and survival in patients with rheumatic and inflammatory diseases: data from the French RMD COVID-19 cohort of 694 patients. Ann Rheum Dis. 2021;80(4):527-538.
Nyabera A, Lakhdar S, Li M, Trandafirescu T, Ouedraogo TS. The association between BMI and inpatient mortality outcomes in older adults with COVID-19. Cureus. 2020;12(10):e11183.
Ozturk S, Turgutalp K, Arici M, Odabas AR, Altiparmak MR, Aydin Z, et al. Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. Nephrol Dial Transplant. 2021;35(12):2083–95.
Druyan A, Lidar M, Brodavka M, Levy I, Barzilai A, Pavlotsky F. The risk for severe COVID 19 in patients with autoimmune and/or inflammatory diseases: first wave lessons. Dermatol Ther. 2021;34(1):e14627.
Alguwaihes AM, Al-Sofiani ME, Megdad M, Albader SS, Alsari MH, Alelayan A, et al. Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study. Cardiovasc Diabetol. 2020;19(1):205.
Özdemir İH, Özlek B, Özen MB, Gündüz R, Çetin N, Bilge AR. Hydroxychloroquine/azithromycin treatment, QT interval and ventricular arrhythmias in hospitalised patients with COVID-19. Int J Clin Pract. 2021;75(2):e13896.
Gue YX, Tennyson M, Gao J, Ren S, Kanji R, Gorog DA. Development of a novel risk score to predict mortality in patients admitted to hospital with COVID-19. Sci Rep. 2020;10(1):21379.
Galiero R, Pafundi PC, Simeon V, Rinaldi L, Perrella A, Vetrano E, et al. Impact of chronic liver disease upon admission on COVID-19 in-hospital mortality: findings from COVOCA study. PloS one. 2020;15(12):e0243700.
Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open. 2020;3(12):e2029058.
Rethemiotaki I. A preliminary study of coronavirus disease 2019 in China: the impact of cardiovascular disease on death risk. Arch Med Sci Atherosclerotic Dis. 2020;5:e219–23.
Stoian AP, Pricop-Jeckstadt M, Pana A, Ileanu B-V, Schitea R, Geanta M, et al. Death by SARS-CoV 2: a Romanian COVID-19 multi-centre comorbidity study. Sci Rep. 2020;10(1).
Zhou S, Chen C, Hu Y, Lv W, Ai T, Xia L. Chest CT imaging features and severity scores as biomarkers for prognostic prediction in patients with COVID-19. Ann Transl Med. 2020;8(21):1449.
Stefan G, Mehedinti AM, Andreiana I, Zugravu AD, Cinca S, Busuioc R, et al. Clinical features and outcome of maintenance hemodialysis patients with COVID-19 from a tertiary nephrology care center in Romania. Renal Fail. 2021;43(1):49–57.
Ahnach M, Zbiri S, Nejjari S, Ousti F, Elkettani C. C-reactive protein as an early predictor of COVID-19 severity. J Med Biochem. 2020;39(4):500–7.
Eshrati B, Baradaran HR, Erfanpoor S, Mohazzab A, Moradi Y. Investigating the factors affecting the survival rate in patients with COVID-19: a retrospective cohort study. Med J Islamic Repub Iran. 2020;34:88.
Özyılmaz S, Ergün Alış E, Ermiş E, Allahverdiyev S, Uçar H. Assessment of the relationship between mortality and troponin I levels in hospitalized patients with the novel coronavirus (COVID-19). Medicina. 2020;56(12).
Tan X, Zhang S, Xu J, Zhou M, Huang Q, Duan L, et al. Comparison of clinical characteristics among younger and elderly deceased patients with COVID-19: a retrospective study. Aging. 2020;13(1):16–26.
Ling SF, Broad E, Murphy R, Pappachan JM, Pardesi-Newton S, Kong M-F, et al. High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study. Nutrients. 2020;12(12):3799.
Zhong Y, Zhao L, Wu G, Hu C, Wu C, Xu M, et al. Impact of renin-angiotensin system inhibitors use on mortality in severe COVID-19 patients with hypertension: a retrospective observational study. J Int Med Res. 2020;48(12):300060520979151.
Izurieta HS, Graham DJ, Jiao Y, Hu M, Lu Y, Wu Y, et al. Natural history of coronavirus disease 2019: risk factors for hospitalizations and deaths among >26 million US medicare beneficiaries. J Infect Dis. 2021;223(6):945–56.
Burrell AJ, Pellegrini B, Salimi F, Begum H, Broadley T, Campbell LT, et al. Outcomes for patients with COVID-19 admitted to Australian intensive care units during the first four months of the pandemic. Med J Aust. 2021;214(1):23–30.
Li Y, Shang K, Bian W, He L, Fan Y, Ren T, et al. Prediction of disease progression in patients with COVID-19 by artificial intelligence assisted lesion quantification. Sci Rep. 2020;10(1).
Caliskan T, Saylan B. Smoking and comorbidities are associated with COVID-19 severity and mortality in 565 patients treated in Turkey: a retrospective observational study. Rev Assoc Med Bras (1992). 2020;66(12):1679–84.
Moradi EV, Teimouri A, Rezaee R, Morovatdar N, Foroughian M, Layegh P, et al. Increased age, neutrophil-to-lymphocyte ratio (NLR) and white blood cells count are associated with higher COVID-19 mortality. Am J Emerg Med. 2021;40:11–4.
The first wave of the COVID-19 pandemic in Spain: characterisation of cases and risk factors for severe outcomes, as at 27 April 2020. Eurosurveillance. 2020;25(50)
Rashidi F, Barco S, Kamangar F, Heresi GA, Emadi A, Kaymaz C, et al. Incidence of symptomatic venous thromboembolism following hospitalization for coronavirus disease 2019: prospective results from a multi-center study. Thromb Res. 2021;198:135–8.
Chaudhri I, Koraishy FM, Bolotova O, Yoo J, Marcos LA, Taub E, et al. Outcomes associated with the use of renin-angiotensin-aldosterone system blockade in hospitalized patients with SARS-CoV-2 infection. Kidney 360. 2020;1(8):801–9.
Huh K, Ji W, Kang M, Hong J, Bae GH, Lee R, et al. Association of prescribed medications with the risk of COVID-19 infection and severity among adults in South Korea. IJID. 2021;104:7–14.
Orioli L, Servais T, Belkhir L, Laterre PF, Thissen JP, Vandeleene B, et al. Clinical characteristics and short-term prognosis of in-patients with diabetes and COVID-19: A retrospective study from an academic center in Belgium. Diab Metab Syndr. 2021;15(1):149–57.
Gude-Sampedro F, Fernández-Merino C, Ferreiro L, Lado-Baleato Ó, Espasandín-Domínguez J, Hervada X, et al. Development and validation of a prognostic model based on comorbidities to predict COVID-19 severity: a population-based study. Int J Epidemiol. 2021;50(1):64–74.
Monteiro AC, Suri R, Emeruwa IO, Stretch RJ, Cortes-Lopez RY, Sherman A, et al. Obesity and smoking as risk factors for invasive mechanical ventilation in COVID-19: A retrospective, observational cohort study. PloS one. 2020;15(12):e0238552.
Lano G, Braconnier A, Bataille S, Cavaille G, Moussi-Frances J, Gondouin B, et al. Risk factors for severity of COVID-19 in chronic dialysis patients from a multicentre French cohort. Clin Kidney J. 2020;13(5):878–88.
Lanini S, Montaldo C, Nicastri E, Vairo F, Agrati C, Petrosillo N, et al. COVID-19 disease—Temporal analyses of complete blood count parameters over course of illness, and relationship to patient demographics and management outcomes in survivors and non-survivors: a longitudinal descriptive cohort study. PLOS ONE. 2020;15(12):e0244129.
Schwartz KL, Achonu C, Buchan SA, Brown KA, Lee B, Whelan M, et al. Epidemiology, clinical characteristics, household transmission, and lethality of severe acute respiratory syndrome coronavirus-2 infection among healthcare workers in Ontario, Canada. PloS one. 2020;15(12):e0244477.
Sun Y, Guan X, Jia L, Xing N, Cheng L, Liu B, et al. Independent and combined effects of hypertension and diabetes on clinical outcomes in patients with COVID-19: A retrospective cohort study of Huoshen Mountain Hospital and Guanggu Fangcang Shelter Hospital. J Clin Hypertens. 2021;23(2):218–31.
McGurnaghan SJ, Weir A, Bishop J, Kennedy S, Blackbourn LAK, McAllister DA, et al. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. Lancet Diab Endocrinol. 2021;9(2):82–93.
Cetinkal G, Kocas BB, Ser OS, Kilci H, Yildiz SS, Ozcan SN, et al. The association between chronic use of renin-angiotensin-aldosterone system blockers and in-hospital adverse events among COVID-19 patients with hypertension. Sisli Etfal Hastanesi tip bulteni. 2020;54(4):399–404.
Xu M, Yang W, Huang T, Zhou J. Diabetic patients with COVID-19 need more attention and better glycemic control. World J Diab. 2020;11(12):644–53.
Lv Z, Lv S. Clinical characteristics and analysis of risk factors for disease progression of COVID-19: a retrospective cohort study. Int J Biol Sci. 2021;17(1):1–7.
Guerra Veloz MF, Cordero Ruiz P, Ríos-Villegas MJ, Del Pino BP, Bravo-Ferrer J, Galvés Cordero R, et al. Liver manifestations in COVID-19 and the influence of pre-existing liver disease in the course of the infection. Rev Esp Enferm Dig. 2021;113(2):103–9.
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–15.
Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. IJID. 2016;49:129–33.
Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HHX, Mercer SW, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8(8):e1003–17.
Guan W-j, Liang W-h, Zhao Y, Liang H-r, Chen Z-s, Li Y-m, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547.
Acknowledgements
We would like to thank Jian Wu, Yang Li and Hongjie Hou (All are from Department of Epidemiology, School of Public Health, Zhengzhou University) for their kind help in searching articles and collecting data, and valuable suggestions for data analysis.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (No. 81973105). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
H.Y. and Y.W. designed the study; J.X., W.X., X.L. and P.Z. searched literature and extracted the data; J.X., L.S. and Y.W. contributed to the statistical analyses and interpretation; J.X. drafted the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not required.
Consent for Publication
Not applicable
Competing interests
The authors declare not any potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table A1.
Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines. Fig. A1. Subgroup analysis stratified by sample size. Fig. A2. Subgroup analysis stratified by type of disease. Fig. A3. Subgroup analysis stratified by age. Fig. A4. Subgroup analysis stratified by the proportion of male. Fig. A5. Subgroup analysis stratified by study design. Fig. A6. Subgroup analysis stratified by region. Fig. A7. Subgroup analysis stratified by outcome of disease.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, J., Xiao, W., Liang, X. et al. A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity. BMC Public Health 21, 1533 (2021). https://doi.org/10.1186/s12889-021-11051-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-11051-w