Abstract
Background
Mental health legislation permits involuntary care of patients with severe mental disorders who meet set legal criteria. The Norwegian Mental Health Act assumes this will improve health and reduce risk of deterioration and death. Professionals have warned against potentially adverse effects of recent initiatives to heighten involuntary care thresholds, but no studies have investigated whether high thresholds have adverse effects.
Aim
To test the hypothesis that areas with lower levels of involuntary care show higher levels of morbidity and mortality in their severe mental disorder populations over time compared to areas with higher levels. Data availability precluded analyses of the effect on health and safety of others.
Methods
Using national data, we calculated standardized (by age, sex, and urbanicity) involuntary care ratios across Community Mental Health Center areas in Norway. For patients diagnosed with severe mental disorders (ICD10 F20-31), we tested whether lower area ratios in 2015 was associated with 1) case fatality over four years, 2) an increase in inpatient days, and 3) time to first episode of involuntary care over the following two years. We also assessed 4) whether area ratios in 2015 predicted an increase in the number of patients diagnosed with F20-31 in the subsequent two years and whether 5) standardized involuntary care area ratios in 2014–2017 predicted an increase in the standardized suicide ratios in 2014–2018. Analyses were prespecified (ClinicalTrials.gov NCT04655287).
Results
We found no adverse effects on patients’ health in areas with lower standardized involuntary care ratios. The standardization variables age, sex, and urbanicity explained 70.5% of the variance in raw rates of involuntary care.
Conclusions
Lower standardized involuntary care ratios are not associated with adverse effects for patients with severe mental disorders in Norway. This finding merits further research of the way involuntary care works.
Similar content being viewed by others
Background
Involuntary care is not uncommon in the treatment of persons diagnosed with severe mental disorders (SMDs). It remains a controversial aspect of psychiatric practice due to its obvious implications for patients’ autonomy and liberty. The use of involuntary care is regulated by mental health legislation, which specifies permitted forms of such care with criteria and safeguards. Involuntary care is usually restricted to those suffering from SMDs who are deemed to need involuntary care or considered a danger to themselves or others when there are no viable, less restrictive options [1]. The Norwegian Mental Health Act (NMHA) [2], like similar legislation in elsewhere, is founded on the assumption that involuntary care reduces risks to patients’ health or life or to the safety and lives of others [3].
Involuntary care is increasing in several countries, both in terms of inpatient [4, 5] and outpatient care [6,7,8]. The scientific evidence regarding benefits to patients of inpatient involuntary care is unclear. A limited number of effect studies, many of which suffered from methodological problems, used a multitude of relevant outcomes and showed mixed results [9,10,11], but overall, the benefits of involuntary admissions have not been firmly established. For Community Treatment Orders (CTOs), which oblige patients to adhere to treatment while living in the community, often with injections of long acting antipsychotic medication, there is a larger evidence base, and meta-analyses of effect studies have concluded that such orders do not prevent admissions or confer other patient benefits [12, 13]. A recent study indicated fewer suicides among patients under CTOs than among comparable patients discharged from hospital without a CTO [14].
Substantial variation has been observed in the use of involuntary care both between [4] and within [15, 16] jurisdictions. In Norway, a recent longitudinal population study found that the average rates of patients under involuntary care from 2014–2018 varied more than threefold between specialist Community Mental Health Center (CMHC) areas, while within-area rates remained relatively stable over time [17]. Age, deprivation, and urbanicity explain parts of the variance between areas, as shown in the United Kingdom [15], but a sizeable proportion of the variation remains unexplained, possibly reflecting differing thresholds for using involuntary care.
Observed variation in the use of involuntary care, along with persistent opposition to coercion by service user organizations, have triggered a number of policy initiatives, campaigns, and programs to reduce involuntary care in various countries [18,19,20,21,22,23,24]. Concerns have been raised, however, that a higher threshold for permitting involuntary care might have adverse effects on patients’ health by failing to alleviate heavy symptom burden or to reduce severe risks [25,26,27,28]. These seem to be relevant concerns, as many patients with psychotic disorders experience relapse [29], chronicity [30], and because patients with SMDs on average die 10–30 years younger than their peers [31]. We have not found empirical studies that have examined whether the lower use of involuntary care is associated with these forms of poor outcomes for patients.
Aims
We present an analysis designed to address this gap in the literature. We hypothesize that if areas with lower levels of involuntary care do not achieve the legislative goals for involuntary care, this would, over time, manifest in higher levels of morbidity and mortality in the area’s population of people with SMDs compared to areas with higher levels of involuntary care. Specifically, we aim to answer the following research questions, using longitudinal national population data from Norway:
-
1.
Do patients with SMDs who live in areas with a lower level of involuntary care have increased case fatality compared to those in areas with a higher level?
-
2.
Do patients with SMDs who receive only voluntary care in the index year and live in areas with lower levels of involuntary care have a higher use of inpatient care in the two subsequent years compared to patients in areas with higher levels?
-
3.
Do patients with SMDs who receive only voluntary care in the index period and live in areas with lower levels of involuntary care experience shorter times until an episode of involuntary care?
-
4.
Does the number of patients with an SMD diagnosis increase over time in areas with lower levels of involuntary care?
-
5.
Is the number of suicides per population higher in areas with lower levels of involuntary care compared to areas with higher levels?
Method
Setting
Norway is a sparsely populated country of five million inhabitants. Four Regional Health Authorities commission 21 health trusts to deliver specialist mental health care from hospitals and CMHCs. In 2016, 71 CMHC areas – the unit used in our analyses – ranged in size from 9,000–125,000 inhabitants aged 18 years and above. Their combined catchment areas covered the entire national population. The NMHA permits involuntary care for observation and treatment of both inpatients and outpatients [2]. A small number of patients are also committed to involuntary care by the criminal courts. Compared internationally, the Norwegian population rates of involuntary care are toward the higher end, with 151 involuntary hospitalized patients per 100,000 adult population in 2015 [4] and a point prevalence of 47.4 patients under a CTO per 100,000 adult population in 2012 [7]. In 2015, the review board rejected 66 of 7824 instances of initiated involuntary care after mandatory document control. In addition, 21 patients successfully appealed against an involuntary observation, and 156 against involuntary care [32].
Study design and data
The study is a retrospective, longitudinal register study, with data from 2014–2018, where the involuntary care ratio in the area a patient lives is studied as a predictor of subsequent outcomes. We registered the analysis plan prospectively (Clinicaltrials.gov identifier NCT04655287).
We obtained patient data on patients aged 18–65 from the Norwegian Patient Registry (NPR), to which all Health Trusts are required to report all specialist inpatient or outpatient health service use. This means that those diagnosed with an SMD in one year but with no specialist service contact in the following year would not be counted for that second year. This registry provides reliable, patient-identifiable, national data with a good degree of completeness [33], including valid diagnoses for severe mental disorders [34]. From 2015 onward, data completeness for inpatient status (voluntary/involuntary) is considered adequate [35]. The population at risk for SMD and involuntary care was defined as all adults ages 18–65 in Norwegian municipalities and city districts (hereafter called local authorities), and data were acquired at Statistics Norway’s online table generator [36, 37]. We acquired data on suicides for men and women ages 18–65 years in CMHC catchment areas from the Norwegian Cause of Death Registry (NCDR). These could only be released aggregated to local authority level and could not be linked to individuals from the NPR data. Data availability precluded analyses of the effect on health and safety of others.
Inclusion and exclusion criteria
The patient sample comprised all persons with an SMD diagnosis and all those with an episode of involuntary care (defined below) within the study period. We excluded those over 65 years to reduce a potential bias from involuntary care resulting (partly) from dementia.
Homeless persons (75 per 100,000 population) [38] were included as their home area is specified in the registers. We excluded persons without a Norwegian Identification number because they could not be followed over time or allocated to a CMHC area (ca. 1% of patients under involuntary care) and, for the same reason, those with unknown or missing data for residing local authority in 2015 (< 0.001% of persons under involuntary care).
Variables
We based our operationalization of severe mental disorder (SMD) on the NMHA [39], which restricts the major diagnostic prerequisite for involuntary care to psychoses or psychotic symptoms. The law discourages involuntary care for mental health disorders without such symptoms [39]. Therefore, we defined an SMD as a diagnosis on the schizophrenia spectrum (F20-29) or bipolar disorder with psychosis (F30-31) as either the primary or secondary diagnosis, as classified following the ICD-10 system [40]. For patients with more than one recorded diagnosis during a year, we used the following hierarchical order to select each patient’s diagnosis: bipolar, schizophrenia spectrum, substance abuse (F10-19), personality disorder (F60-69), and depressive (F32) and other disorders.
For the purposes of the present study, involuntary care was defined as involuntary inpatient or outpatient care or observation sanctioned by the NMHA, including those in forensic care and those sentenced to care by a criminal court. A patient with such a care episode was classified as under involuntary care for that year.
Mental health inpatient days for a patient was the term we used for the combined number of days in hospital for that patient during the calendar year in question, regardless of care formality and including inpatient days in mental health institutions outside the patient’s CMHC area.
Area of residence represented the local authority in which the patient’s registered address belonged, aggregated to the appropriate CMHC area. For those who moved during the period, we used the address at the beginning of the last episode of mental health care during the year in question. For analyses that studied effects over time, the area of residence in the index year was used as the area of residency throughout.
Urbanicity was classified as one of five levels of urbanicity as described in Table 1, which were assigned to each local authority area. This was based on Statistics Norway’s classification [41] as modified in a previous study [42]. An urbanicity value was assigned to each patient based on his or her area of residence.
Area deprivation. We used Statistics Norway’s continuous living condition index for 2008 as a measure of deprivation in the local community. The index is based on averaged deciles of unemployment, welfare benefits, educational level, mortality, etc., resulting in a number between 1 and 10 [43] and was updated every eight years until 2008.
CMHC areas consist of one or more local authorities. Several CMHCs and local authorities merged during the study period (2014–2018). In order to have a fixed area structure in the analyses, we analyzed all data using the area structure from 2016. In two cities, CMHC areas deviated from local authority borders, and in these two cases, we combined CMHC areas, thereby reducing the number of areas from 71 to 69.
The standardized involuntary care area ratio (SIAR) was used as the primary covariate in our analyses. First, raw involuntary care rates were calculated by dividing the number of people experiencing involuntary care during a given year by the population at risk during that year. We prepared the standardization by estimating a linear regression model with the raw rate of persons experiencing involuntary care in the local authority as the outcome and with age (six groups), sex (two groups), urbanicity (five classes), and deprivation (range) as covariates. We did not include SMD rates into the standardization to reduce the risk of bias from differing diagnostic thresholds. We reasoned that a lower threshold for setting SDM diagnoses would mean more patients with less severe symptoms – and therefore unlikely to be treated involuntarily – would be diagnosed. If used in standardization, areas with lower threshold for setting SMD diagnosis could therefore have their rate of involuntary care adjusted downwards, whereas for areas with a higher diagnostic threshold this would adjust their level upwards. If service capacity or paternalism is associated with the threshold for involuntary care and SMD diagnosis setting, including SMD rates in the standardization could bias the analyses in the direction of null-results.
The variables that were significant in the regression model, which were age, sex, and urbanicity, were then used for indirect standardization. For each local authority, we calculated the expected number of patients under involuntary care for each age and sex stratum in the area’s urbanicity and aggregated this to the CMHC area population. We then divided the observed number of persons under involuntary care by the expected number of persons under involuntary care. The resulting SIAR values (range 0.58–1.46) have 1 as the reference, where SIAR values below 1 indicate fewer persons than expected under involuntary care in the CMHC area. Each patient was assigned a SIAR value based on his or her area of residency in 2015.
Statistical analyses
To answer our research questions about possible negative effects of low levels of involuntary care, we predefined five models [44] (see Table 2). The first four were estimated using longitudinal data at the patient (Models 1–3) or CMHC area level (Model 4). In Model, 5 which used area suicides as outcome, we aggregated suicide numbers for five years in order to increase power. It is therefore a cross-sectional analysis.
Data were not available in advance to prespecify any cut-off value of high/low SIAR or to decide between non-linear and linear associations between SIAR and the outcomes. Therefore, we examined each outcome for non-linear associations and for adequacy of a linear model with suitable tests and estimated the latter when appropriate.
Model 1 – Cox proportional hazards (PHs) regression analysis. We assessed the effect of SIAR on case fatality over time, adjusted for age and sex, by following all SMD patients over four years, which allowed for observing delayed deaths. Schoenfeld’s residuals were used to assess the PHs assumption, while potential non-linear associations were tested by martingale residuals. Cluster effects on CMHC, Health Trust, and regional health authority levels were assessed by intra-class correlation (ICC), which showed no effects or negligible effects, and hence, no adjustment was needed. Models 2 and 3 assessed whether SMD patients in voluntary care in 2015 deteriorated over the subsequent two years in areas with low SIAR. As we here wanted test deterioration (into more inpatient days in Model 2 and into involuntary care in Model 3), we included only those in voluntary care in the baseline year. It is also among voluntary patients with SMD that we could expect to find those whose needs for protection against deterioration may not be met where there is a high threshold for using involuntary care. Model 2 was a linear mixed model, which assessed the trend in inpatient days as a function of SIAR. The model contained random intercepts for CMHCs and fixed effects for time dummy, SIAR, and interactions between time and SIAR. A model with SIAR as a non-linear covariate was considered; however, no non-linear associations were detected. The residuals were inspected graphically to assess the assumptions of normality and homoscedasticity. Post-hoc analyses were performed to explore the interaction further. Model 3 – a Cox PH model – assessed time to involuntary care as a function of SIAR. Death was included as a competing risk. The model assumptions were assessed in the same way as for Model 1.
Model 4 – a linear mixed model – assessed whether low SIAR in a CMHC area was followed by an increased number of people treated for SMDs in the area in the following two years, suggesting differential rates of improvement or deterioration. As this is an area characteristic it was analyzed at area level, and different baseline levels of SMDs were controlled for by investigating changes in SMD rates. The model included fixed effects for time as a second-order polynomial to account for non-linear effects, SIAR, and interaction between the two. The model without the interaction term was chosen based on the Bayesian information criterion (BIC). The model assumptions were assessed in the same way as for Model 2.
Model 5 was based on cross-sectional data for SIAR and suicides; scatter plot and correlation analysis was employed to assess whether a low SIAR is associated with more suicides. For the smallest CMHC areas, the expected number of suicides per year (based on the national count of ca. 600 suicides per year [45]) was around 1 per year. Therefore, we aggregated suicide numbers for 2014–2018 in order to increase power. This required a cross-sectional design, and we therefore observed and averaged involuntary care for the years 2014–2017, to observe suicides that might happen some time after discharge from involuntary care. We considered an area level measure of suicide to be a relevant outcome for the SMD population, even if it might introduce some noise in that it includes suicides that are not SMD related.
For all analyses, we set the threshold for significance at 0.05. We prepared data for analyses using R 3.6.1 [46] with data.table 1.12.8 [47], tidyverse 1.3.0 [48], and lubridate 1.7.4 [49], and we used Stata 16 for standardization and regression models. Figures were drawn with Stata, ggplot2 [50] and MATLAB R2020b.
Changes to the analysis plan
For technical reasons, we needed to make minor alterations to the registered analysis plan for Model 5. Due to several municipality mergers, the NCDR could not map data on suicides from 2019 to the local authority structure of 2018 and earlier; therefore, we moved the periodization from the planned period of 2015–2019 to 2014–2018. In addition, because the NCDR could not allocate suicides to city districts, we merged several CMHCs in cities for the model with suicides as the outcome. Due to the registry’s privacy requirements, a minimum cell size was required in order to release area data for suicides per urbanicity stratum, and therefore, we combined level 4 (the smallest stratum) and level 5. In 2014, four health trusts had < 85% data completeness on care formality. Thus, we ran Model 5 with and without data from nine CMHC areas in these four health trusts.
Ethics
The study analyzed data from the NPR that was collected prior to and independently of this study. The Norwegian Research Ethics Committee granted permission to obtain and analyze de-identified data from the NPR without individual consent (ref: 2018/795). The NPR de-identifies patients’ ID numbers before release in accordance with relevant regulations. The study and the Data Protection Impact Assessment (DPIA) were approved by the Privacy Ombudsman at Akershus University Hospital (ref: 2018–090).
Results
In Table 3, we provide details of the 21,481 included patients in 2015. One-third (6,853 patients) experienced involuntary care that year, 5,096 (74.3%) of whom were diagnosed with SMD. Of the remaining patients, 621 (9.1%) were diagnosed with addiction disorders and 246 (3.6%) with personality disorders. For all variables with available data for patients with only voluntary care in 2015, the difference between this group and patients under involuntary care had P-values lower than 0.001. There were significantly more men than women under involuntary care, and more urban areas had higher proportions of patients under involuntary care.
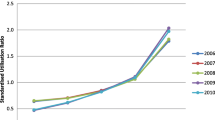
The raw rate of persons under involuntary care in the CMHC areas varied from 92 to 338 per 100,000, with an extremal quotient of 3.7. In bivariate models, age explained 19.5% of this variance, sex 8.8%, urbanicity 42.1%, and deprivation 0.8%. The multiple regression model that included the statistically significant variables (age, sex, and urbanicity) as explanatory variables explained 70.5% of the variance in involuntary care between local authorities. In the indirect standardization, the SIAR in CMHC areas with a mainly urban population was lower compared to raw rates and vice versa. The raw and standardized rates for each CMHC area are shown in Fig. 1. The lowest and highest SIAR observed in 2015 was 0.58 and 1.46 (mean = 1.0), respectively, with an extremal quotient of 2.5.
Models
In Model 1, we investigated case fatality for patients with SMDs dependent on SIAR. Of the 19,724 patients with SMDs in contact with specialist services in 2015, 739 died within the study period. The regression coefficients from the model with case fatality as the outcome are shown in Table 4. There was no significant effect of SIAR on case fatality. Men (p < 0.001) and older patients (p < 0.001) had a significantly higher rate of case fatality.
In Model 2, we investigated the change in mental-health inpatient days for voluntary SMD patients dependent on SIAR. Of the 14,628 patients diagnosed with SMD and no involuntary care episodes in 2015, the mean number of mental-health inpatient days was reduced by one day per year, from 11.5 (SD 32.42) in 2015 to 10.5 (33.72) in 2016 and to 9.7 (32.93) in 2017. The model showed non-significant interactions, indicating no overall differences in the association between SIAR and the change in inpatient days, as shown in Table 5.
Because the P-value for SIAR (= 0.05) was close to our set significance level, we explored data in greater detail in a linear mixed model, showing a mean reduction of 0.92 days per year that was significant (p < 0.001). In this post hoc analysis, the change from 2015 to 2017 was significant for SIAR > 0.7, while the change from 2015 to 2016 was significant for SIAR values 0.85–1.35. The differences in change from 2015 to 2016 and 2015 to 2017, depicted in Fig. 2, are only significant, however, for SIAR > 0.9. Higher SIAR was associated with a higher number of inpatient days in the baseline year, and decreased more over time compared with lower SIAR areas.
In Model 3, we investigated time to involuntary care for voluntary SMD patients, dependent on SIAR. Of the 14,628 patients diagnosed with SMD and with no involuntary care episode in 2015, 1,202 (8.2%) experienced involuntary care at some point during the subsequent two years. The Cox PH regression model with death as a competing risk showed that lower SIAR in 2015 did not predict deterioration into involuntary care (hazard ratio 1.17, 95% CI (0.86; 1.57), p = 0.316). A sensitivity analysis that excluded patients who died showed similar results.
In Model 4, we investigated change in SMD rates in CMHC areas over time, dependent on SIAR. The rate of SMD per 100,000 persons across all CMHC areas varied between 606.5 in 2015 and 620 in 2017.
As presented in Table 6, the linear mixed model showed a significant non-linear time trend for the rate of SMDs, with an overall increase in rates throughout the period and a small reduction in 2018. Lower SIARs in 2015 were associated with lower SMD rates for 2016–2018 (p = 0.024), and this association did not vary between the years (no interaction between time and SIAR). The model predicted that areas with SIAR 1.1 had 2.5% more SMD patients per capita compared to areas with SIAR 1.0. That is, if an area has 20 additional people under involuntary care per 100,000 persons at risk, there would be 15 more people with an SMD in the area.
In Model 5, we studied suicide rate dependent on SIAR. We observed 2,474 suicides between 2014 and 2018, corresponding to a five-year suicide rate of 75.3 per 100,000 persons at risk (46.3 for women and 102.8 for men). The five-year rate varied by age from 65.7 in 18–25-year-olds to 92.2 for those ages 50–57. The correlation between standardized suicide rates for the five-year period and the mean of yearly local SIARs in the period 2014–2017 was -0.11, explaining 1.22% of the variance in suicides. After removing data from nine CMHC areas due to the reported low data completeness on legal status in 2014, the correlation coefficient was -0.15, explaining 2.3% of the variance. The scatter plots did not indicate non-linear relations.
Discussion
We designed this study to investigate whether services in areas with lower ratios of involuntary mental health care fail to achieve legislative ambitions for involuntary care, specifically in regard to restoring health and reducing risks of deterioration or death for persons with SMD. To our knowledge, this is the first empirical study to investigate potentially adverse effects of lower levels of involuntary care within an entire jurisdiction.
Using a continuous, standardized measure of each area’s level of involuntary care (SIAR), we tested five models of possible adverse effects of a lower use of involuntary care and found no statistically significant effect for patients with an SMD. We did not observe significantly more case fatalities, deterioration into involuntary care, or increases in inpatient days for patients with SMDs, nor did we find increased rates of SMDs or notable increases in the numbers of suicides at the area level. In addition to investigating linear effects, we checked all outcomes for non-linear relationships to identify potential cut-off values for high vs low SIARs with differential effect on outcomes but found none. Overall, our findings did not support the hypothesis that areas with low standardized rates of involuntary care place patients with SMD at higher risk.
While none of our results reached statistical significance, the relationship between SIAR and number of inpatient days in Model 2 had a p-value of 0.05. An exploratory post-hoc analysis (depicted in Fig. 2) showed a higher mean number of inpatient days at baseline for voluntary SMD patients in higher SIAR areas. We used inpatient days as a proxy for severity of illness [51]. We had expected that a higher SIAR value reflected a lower threshold for involuntary care, and that voluntary SMD patients in these areas would have reduced illness severity compared to lower SIAR area patients. Contrary to this expectation, Fig. 2 indicated fewer inpatient days in lower SIAR areas and that this inpatient day level was stable throughout the three years.
If SMD patients in areas with low standardized involuntary care rates have unnecessary deterioration and that fewer recover, then the following increased morbidity should lead to more patients under involuntary care. Model 3 and 4 showed no such effect, which is in accordance with the relatively stable involuntary care rates over time at CMHC level [17] as well as health trust level in Norway [52,53,54,55].
The national rate of involuntary care in Norway is relatively high compared to many other Western countries [4]. Rates considered low in Norway may, therefore, not be considered as such in other jurisdictions. Cross-national comparisons of involuntary care are fraught with problems [56], and several factors might be conducive to higher reported levels of involuntary care in Norway. These include good quality registers, relatively few patients in forensic care, inclusion of forensic patients in several coercion estimates, strict conditions for converting a patient’s status from voluntary to involuntary care during an admission, and the guidance from the Directory of Health that patients in need of treatment but without capacity to make treatment decisions should be placed under involuntary care, even if they accept treatment, in order to protect their legal safeguards [39]. Although the range of raw rates in CMHC areas in the data in our study (92–338 per 100,000) covers the national average level of involuntary care in many jurisdictions, several relevant parameters may vary between countries, and studies of the effect of the level of involuntary care in different jurisdictions are merited.
Model assumptions and future areas for research
Our design was based on two main assumptions. First, as implicit in the legislation, involuntary care protects patients from negative outcomes. Second, our standardization procedure made the CMHC areas comparable. However, the results indicate that one or both of these assumptions are inaccurate.
The assumption that involuntary care protects patients from negative outcomes is not supported by our findings, but neither can it be ruled out. Combined with systematic reviews that demonstrate a lack of evidence for patient benefits of involuntary care [11, 13], this raises the concern that involuntary care may not work entirely as intended by lawmakers and clinicians. This might be because predicting suicides and other rare events is notoriously difficult [57]. We know that previously committed patients have greater likelihood of later involuntary care, which may maintain the patterns of involuntary care without fully taking into account the patient’s symptoms or risks ([58] see Lived experience commentary by Olive & Nyikavaranda). Given the concerns voiced by user organizations [59], the ethical concern surrounding the provision of treatment without a person’s consent [60, 61], and over geographical variations in such treatment [62] there is an urgent need for additional studies that test core assumptions of mental health acts.
To establish comparable areas, we calculated standardized involuntary care area ratios (SIARs) that controlled for age, sex, and urbanicity (deprivation added no explanatory value) as these variables are known to be associated with levels of involuntary care [15, 58]. Our standardization variables explained 70.5% of the variation in rates of involuntary care in 2015, and urbanicity, in particular, explained the observed service variation. Associations with urbanicity have also been found in the Netherlands [63] and England [15], and it was associated with an elevated risk of psychosis in studies from Northern European settings in a recent review [64]. A number of other factors that have been associated with our outcomes are likely to correlate with urbanicity and/or deprivation and, therefore, are to some extent controlled for by our procedure. These include immigrant status, which has been associated with higher levels of SMDs [65]; the proximity to a hospital [66]; and the numbers of hospital beds [67] and of psychiatrists [68], which have been linked to increased admissions. Nonetheless, there may be other factors that could not be fully evaluated in our design that may have affected the comparability of the CMHC areas. These could include variance in morbidity and severity (case mix), care capacity, diagnostic threshold, service paternalism, help-seeking behavior, and SMD recovery rates, among other factors.
The results in Model 4 suggest that confounding factors might have been at play. We found higher rates of SMD patients in areas with higher SIARs and no interaction between SIARs and time. With a higher level of morbidity – which was also suggested by baseline inpatient day use in Model 3 – it is possible that the threshold for using involuntary care was similar across areas. Nevertheless, results from Model 4 indicated that, with an additional 20 patients under involuntary care, there would be 15 additional people with SMD. With roughly one-third of all SMD patients under involuntary care in any given year (see Table 3), as many as 60 additional patients should be registered with SMD to explain why 20 more patients are placed under involuntary care, indicating that high SIAR areas have a lower threshold for involuntary care, a very different case-mix, or differing diagnostic practices.
Future research should seek to control for additional variables related to service context that were not included in our data. We know that the organization and capacity of primary mental health care vary significantly among the CMHC areas in Norway [69], which might have an impact on the use of involuntary care [70]. The availability of comprehensive outpatient treatment approaches, such as assertive community treatment (ACT) or flexible ACT, could also have an impact. Studies of ACT, where it exists in Norway, have found reduced numbers and duration of episodes of involuntary care [71], in addition to improved interaction and rapport between patients and professionals [72, 73]. This is in line with the international evidence on ACT [74]. Common qualities in these types of services may, therefore, have an impact on both the local level of involuntary care and potential adverse patient outcomes and, thereby, could contribute to the lack of difference in outcomes between areas with high and low SIARs as observed in our study.
Strengths and limitations
The study was based on comprehensive and robust longitudinal data encompassing an entire jurisdiction, collected independently of the research aims and with good completeness. All analyses were prespecified and conducted with only minor alterations as explained above. The findings across all models were consistent and supported the null hypotheses. The SIAR comprised persons affected by involuntary inpatient and/or outpatient care, thus reducing possible bias from individuals with many involuntary care episodes during a year and from local differences in substituting admissions with CTOs.
A main limitation of the present study is the observational design. While the hypothesis of adverse outcomes for patients in low SIAR areas did not bear out in our analysis, unmeasured variables may have confounded the results, as discussed above. Our data did not allow us to test a number of alternative predictions regarding other important potential benefits of involuntary care, most notably, risk to others. Additionally, that SIAR did not predict outcomes in our design, does not inform us of the outcomes for patient groups that tend to be under involuntary care also in the low SIAR areas.
We categorized local authority areas into five ordinal classes. These urbanicity classes explained as much as 42.1% of involuntary care rate variation. As the underlying urbanicity dimension is likely to be gradual, a continuous urbanicity index could have improved the design.
To calculate SIAR rates, we looked at persons under involuntary care, but in Models 1–4, we looked at the outcome for persons with SMDs. Of patients under involuntary care in 2015, one-fourth did not have a primary or secondary F20-31 diagnosis, and Models 1–4 did not evaluate the effect for these patients. Future studies should consider more fine-tuned analyses by calculating separate involuntary care rates for prespecified diagnostic groups or should distinguish between involuntary care following, for instance, drug-induced psychoses vs longer-term mental disorders. Norwegian mental health care differs from care in other countries and changes over time, which limits the generalizability of the present study to other contexts.
In conclusion, based on the assumption underpinning the NMHA that involuntary care confers patient benefits by improving health and reducing risk, we hypothesized that areas with lower use of involuntary care would show poorer outcomes than areas of higher use. We found no such effect. Low area rates were not associated with higher case fatality, deterioration into involuntary care, or more inpatient days, nor did we find increased rates of SMDs or suicides at the area level. Services with lower levels of involuntary care, therefore, seem to provide care for those with SMD diagnoses with similar results as areas with higher uses of compulsion. Our results show that it is possible to study specific hypotheses of how involuntary mental health care works with routinely collected register data. More research is needed to examine in greater detail whether or not mental health legislation protects life and health in the ways intended by its core assumptions.
Availability of data and materials
The full dataset analyzed during the current study is not publicly available due to data restrictions demanded by the NPR. Population count data and aggregated suicide data are available from the corresponding author upon reasonable request.
References
Saya A, Brugnoli C, Piazzi G, Liberato D, Di Ciaccia G, Niolu C, Siracusano A. Criteria, procedures, and future prospects of involuntary treatment in psychiatry around the world: a narrative review. Front Psychiatry. 2019;10:271.
Act No. 62 of 2 July 1999 relating to the provision and implementation of mental health care, with later amendments [http://app.uio.no/ub/ujur/oversatte-lover/data/lov-19990702-062-eng.pdf]
Wasserman D, Apter G, Baeken C, Bailey S, Balazs J, Bec C, Bienkowski P, Bobes J, Ortiz MFB, Brunn H, et al. Compulsory admissions of patients with mental disorders: State of the art on ethical and legislative aspects in 40 European countries. Eur Psychiatry. 2020;63(1): e82.
Sheridan Rains L, Zenina T, Dias MC, Jones R, Jeffreys S, Branthonne-Foster S, Lloyd-Evans B, Johnson S. Variations in patterns of involuntary hospitalisation and in legal frameworks: an international comparative study. Lancet Psychiatry. 2019;6(5):403–17.
Sashidharan S, Saraceno B. Is psychiatry becoming more coercive? BMJ. 2017;357:j2904.
Light E. Rates of use of community treatment orders in Australia. Int J Law Psychiatry. 2019;64:83–7.
Riley H, Sharashova E, Rugkåsa J, Nyttingnes O, Christensen TB. Austegard A-TA, Løvsletten M, Lau B, Høyer G. Out-patient commitment order use in Norway: incidence and prevalence rates, duration and use of mental health services from the Norwegian Outpatient Commitment Study. BJPsych open. 2019;5(5):e75.
Trevithick L, Carlile J, Nodiyal S, Keown P. Community treatment orders: an analysis of the first five years of use in England. Br J Psychiatry. 2018;212(3):175–9.
Kallert TW, Glockner M, Schutzwohl M. Involuntary vs. voluntary hospital admission. A systematic literature review on outcome diversity. Eur Arch Psychiatry Clin Neurosci. 2008;258(4):195–209.
Jacobsen TB. Involuntary treatment in Europe: different countries, different practices. Curr Opin Psychiatry. 2012;25(4):307–10.
Luciano M, Sampogna G, Del Vecchio V, Pingani L, Palumbo C, De Rosa C, Catapano F, Fiorillo A. Use of coercive measures in mental health practice and its impact on outcome: a critical review. Expert Rev Neurother. 2014;14(2):131–41.
Kisely SR, Campbell LA, O’Reilly R. OReilly R: Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database Syst Rev. 2017;3(3):CD004408.
Barnett P, Matthews H, Lloyd-Evans B, Mackay E, Pilling S, Johnson S. Compulsory community treatment to reduce readmission to hospital and increase engagement with community care in people with mental illness: a systematic review and meta-analysis. The Lancet Psychiatry. 2018;5(12):1013–22.
Hunt IM, Webb RT, Turnbull P, Graney J, Ibrahim S, Shaw J, Kapur N, Appleby L. Suicide rates among patients subject to community treatment orders in England during 2009–2018. BJPsych Open. 2021;7(6):E180, 1–6.
Keown P, McBride O, Twigg L, Crepaz-Keay D, Cyhlarova E, Parsons H, Scott J, Bhui K, Weich S. Rates of voluntary and compulsory psychiatric in-patient treatment in England: an ecological study investigating associations with deprivation and demographics. Br J Psychiatry. 2016;209(2):157–61.
Gandré C, Gervaix J, Thillard J, Macé J-M, Roelandt J-L, Chevreul K. Geographic variations in involuntary care and associations with the supply of health and social care: results from a nationwide study. BMC Health Serv Res. 2018;18(1):1–10.
Hofstad T, Rugkåsa J, Ose SO, Nyttingnes O, Husum TL. Measuring the level of compulsory hospitalisation in mental health care: The performance of different measures across areas and over time. Int J Methods Psychiatr Res. 2021;30(3):e1881.
Guan L, Liu J, Wu XM, Chen D, Wang X, Ma N, Wang Y, Good B, Ma H, Yu X. Unlocking patients with mental disorders who were in restraints at home: a national follow-up study of China’s new public mental health initiatives. PLoS ONE. 2015;10(4): e0121425.
Fukasawa M, Miyake M, Suzuki Y, Fukuda Y, Yamanouchi Y. Relationship between the use of seclusion and mechanical restraint and the nurse-bed ratio in psychiatric wards in Japan. Int J Law Psychiatry. 2018;60:57–63.
Noorthoorn EO, Voskes Y, Janssen WA, Mulder CL, van de Sande R, Nijman HL, Smit A, Hoogendoorn AW, Bousardt A, Widdershoven GA. Seclusion reduction in Dutch mental health care: Did hospitals meet goals? Psychiatr Serv. 2016;67(12):1321–7.
Zero seclusion: It’s about teamwork. Health Quality & Safety Commission [https://www.hqsc.govt.nz/blog/zero-seclusion-its-about-teamwork/]
Position Statement on Seclusion and Restraint [https://www.nasmhpd.org/content/position-statement-seclusion-and-restraint]
Ministry of Health and Care: Better quality - Increased voluntariness. National strategy for increased voluntariness in mental health care 2012–2015 [Norwegian]. https://www.regjeringen.no/globalassets/upload/hod/bedrekvalitet-okt_frivillighet.pdf; 2012.
Nyttingnes O, Rugkåsa J. The Introduction of Medication-Free Mental Health Services in Norway: An Analysis of the Framing and Impact of Arguments From Different Standpoints. Front Psych. 2021;12(685024):1123.
Torrey EF, Zdanowicz M. Outpatient commitment: what, why, and for whom. Psychiatr Serv. 2001;52(3):337–41.
Appelbaum PS. Protecting the rights of persons with disabilities: an international convention and its problems. Psychiatr Serv. 2016;67(4):366–8.
Freeman MC, Kolappa K, de Almeida JM, Kleinman A, Makhashvili N, Phakathi S, Saraceno B, Thornicroft G. Reversing hard won victories in the name of human rights: a critique of the General Comment on Article 12 of the UN Convention on the Rights of Persons with Disabilities. Lancet Psychiatry. 2015;2(9):844–50.
Larsen TK. Coercion is necessary sometimes - political interference bordering to the scandalous [Norwegian]. Stavanger Aftenblad 2018. https://www.aftenbladet.no/meninger/debatt/i/l1q4vy/rus-psykiatri-noen-ganger-er-tvang-noedvendig-politisk-innblanding-grenser-til-det-skandaloese.
Taylor M, Jauhar S. Are we getting any better at staying better? The long view on relapse and recovery in first episode nonaffective psychosis and schizophrenia. Therapeutic advances in psychopharmacology. 2019;9:2045125319870033.
Cohen A, Patel V, Thara R, Gureje O. Questioning an axiom: better prognosis for schizophrenia in the developing world? Schizophr Bull. 2008;34(2):229–44.
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. The Lancet Psychiatry. 2016;3(2):171–8.
Helsedirektoratet. Kontroll av tvangsbruk i psykisk helsevern 2015 [Control of use of coercion in mental health care 2015. Norwegian Directorate of Health]. Report. 2016. Retrieved from: https://www.helsedirektoratet.no/rapporter/kontroll-av-tvangsbruk-i-psykisk-helsevern/Kontroll%20av%20tvangsbruk%20i%20psykisk%20helsevern%202015.pdf/_/attachment/inline/5f0c714c-b4d6-4d18-b867-f6f5936da828:a8fa21d763cbca2534642d17c17d5c8a37fe870f/Kontroll%20av%20tvangsbruk%20i%20psykisk%20helsevern%202015.pdf.
Bakken IJ, Ariansen AMS, Knudsen GP, Johansen KI, Vollset SE. The Norwegian Patient Registry and the Norwegian Registry for Primary Health Care: Research potential of two nationwide health-care registries. Scand J Public Health. 2020;48(1):49–55.
Nesvåg R, Jönsson EG, Bakken IJ, Knudsen GP, Bjella TD, Reichborn-Kjennerud T, Melle I, Andreassen OA. The quality of severe mental disorder diagnoses in a national health registry as compared to research diagnoses based on structured interview. BMC Psychiatry. 2017;17(1):1–8.
Helsedirektoratet. Tvang i psykisk helsevern. Utvikling i perioden 2013 - 2017 [Norwegian Directorate of Health: Involuntary mental health care. Developments in the period 2013 -2017]. Report IS-2812. 2019. Retrieved from: https://www.helsedirektoratet.no/rapporter/tvang-i-psykisk-helsevern--utvikling-i-perioden-20132017/Tvang%20i%20psykisk%20helsevern%20%E2%80%93%20Utvikling%20i%20perioden%202013%E2%80%932017.pdf/_/attachment/inline/4a97f77b-4be9-4b69-ba02-27761cf1baed:5cf5e3f022b9b2ca6548092b70f4ff062579b2c8/Tvang%20i%20psykisk%20helsevern%20%E2%80%93%20Utvikling%20i%20perioden%202013%E2%80%932017.pdf.
Statistics Norway. Population, by sex and one‐year age groups (M) 1986—2020. PX‐Web SSB. 2022. https://www.ssb.no/en/statbank/table/07459.
Statistics Norway. Population, by sex & age (UD) 2001 - 2020. [Four largest cities with city districts] PX-Web SSB. 2022. https://www.ssb.no/en/statbank/table/10826.
Dyb E. Counting homelessness and politics: the case of Norway. Eur J Homelessness. 2017;11(2):15-37.
Norges offentlige utredninger. Økt selvbestemmelse og rettssikkerhet. [Official Norwegian Reports: Increased self-determination and legal protection]. NOU 2011:9, Ministry of Health and Care. 2011. Retrieved from: https://www.regjeringen.no/contentassets/edc9f614eb884f1d988d16af63218953/no/pdfs/nou201120110009000dddpdfs.pdf.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
Statistics Norway. Population in densely and sparsely populated areas, by sex (M) 1990-2021. PX-Web SSB; 2021. https://www.ssb.no/en/statbank/table/05212.
Rugkåsa J, Nyttingnes O, Simonsen TB, Benth JŠ, Lau B, Riley H, Løvsletten M, Christensen TB. Austegard A-TA, Høyer G: The use of outpatient commitment in Norway: Who are the patients and what does it involve? Int J Law Psychiatry. 2019;62:7–15.
Rogstad L. Index for living conditions of deprivation [Norwegian: Indeks for levekårsproblemer]. Samfunnsspeilet. 2002;4–5:106–9.
ClinicalTrials.gov [Internet]: Identifyer NCT04655287. A Register Study of Effects Following Local Variation in Rates of Involuntary Care; 2020.
Norwegian Cause of Death Registry. D10b Suicides, by sex and way of death. 2020. https://statistikkbank.fhi.no/dar/.
R Core Team. R: A language and environment for statistical computing, Version 3.0.2. R Foundation for Statistical Computing, Vienna, Austria. 2019. [https://www.R-project.org/].
Dowle M, Srinivasan A, Gorecki J, Chirico M, Stetsenko P, Short T, Lianoglou S, Antonyan E, Bonsch M, Parsonage H. Package ‘data.table’. Extension of ‘data.frame’. 2019. [https://rdrr.io/cran/data.table/].
Wickham H, Averick M, Bryan J, Chang W, McGowan LDA, François R, Grolemund G, Hayes A, Henry L, Hester J. Welcome to the Tidyverse. J Open Source Softw. 2019;4(43):1686.
Grolemund G, Wickham H. Dates and times made easy with lubridate. J Stat Softw. 2011;40(1):1–25.
Wickham H. ggplot2. Elegant graphics for data analysis. New York: Springer; 2016.
Burns T. Hospitalisation as an outcome measure in schizophrenia. Br J Psychiatry. 2007;191(50):s37–41.
Helsedirektoratet. Bruk av tvang i psykisk helsevern for voksne 2009 [The Norwegian Directorate of Health: Use of Coercion in Norwegian Mental Health Care for adults 2009]. Report IS 1861. 2010. Retrieved from: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/466/Bruk-av-tvang-i-psykisk-helsevern-for-voksne-2010-IS-1941.pdf.
Helsedirektoratet. Bruk av tvang i psykisk helsevern for voksne 2013 [The Norwegian Directorate of Health: Use of Coercion in Norwegian Mental Health Care for adults 2013]. Report IS 2243; 2014.
Helsedirektoratet. Tvang i psykisk helsevern. Status etter lovendringene i 2017 [The Norwegian Directorate of Health: Coercion in mental health care. Status after the legal changes in 2017]. Report IS 2888; 2020.
Statens helsetilsyn. Bruk av tvang i psykisk helsevern. [Norwegian Board of Health Supervision: Use of coercion in mental health care]. Report: 4/2006; 2006. Retrieved from: https://www.helsetilsynet.no/globalassets/opplastinger/publikasjoner/rapporter2006/helsetilsynetrapport4_2006.pdf.
Høyer G. Involuntary hospitalization in contemporary mental health care. Some (still) unanswered questions. J Ment Health. 2008;17(3):281–92.
Mulder R, Newton-Howes G, Coid JW. The futility of risk prediction in psychiatry. Br J Psychiatry. 2016;209(4):271–2.
Walker S, Mackay E, Barnett P, Sheridan Rains L, Leverton M, Dalton-Locke C, Trevillion K, Lloyd-Evans B, Johnson S. Clinical and social factors associated with increased risk for involuntary psychiatric hospitalisation: a systematic review, meta-analysis, and narrative synthesis. Lancet Psychiatry. 2019;6(12):1039–53.
Oaks D. The moral imperative for dialogue with organizations of survivors of coerced psychiatric human rights violations. In: Kallert TW, Mezzich JE, Monahan J, editor. Coercive Treatment in Psychiatry Clinical, Legal and Ethical Aspects. West Sussex: Wiley Blackwell; 2007:187–211.
Saks ER. Refusing care: Forced treatment and the rights of the mentally ill. Chicago: University of Chicago Press; 2002.
Häyry H. The limits of medical paternalism. London: Routledge; 1991.
Hofstad T, Husum TL, Rugkåsa J, Hofmann BM. Geographical variation in compulsory hospitalisation–ethical challenges. BMC Health Serv Res. 2022;22(1):1–12.
Braam AW, van Ommeren OW, van Buuren ML, Laan W, Smeets HM, Engelhard IM. Local geographical distribution of acute involuntary psychiatric admissions in subdistricts in and around Utrecht, the Netherlands. J Emerg Med. 2016;50(3):449–57.
Fett A-KJ, Lemmers-Jansen IL, Krabbendam L. Psychosis and urbanicity: A review of the recent literature from epidemiology to neurourbanism. Curr Opin Psychiatry. 2019;32(3):232.
Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first-and second-generation immigrants. Psychol Med. 2011;41(5):897–910.
Curtis S, Congdon P, Almog M, Ellermann R. County variation in use of inpatient and ambulatory psychiatric care in New York State 1999–2001: Need and supply influences in a structural model. Health Place. 2009;15(2):568–77.
Watts BV, Shiner B, Klauss G, Weeks WB. Supplier-induced demand for psychiatric admissions in Northern New England. BMC Psychiatry. 2011;11(1):1–7.
Kurdyak P, Stukel TA, Goldbloom D, Kopp A, Zagorski BM, Mulsant BH. Universal coverage without universal access: a study of psychiatrist supply and practice patterns in Ontario. Open Medicine. 2014;8(3): e87.
Ose SO, Kaspersen SL. Kommunalt psykisk helse- og rusarbeid 2017 [Municipal work in mental health and addiction 2017]. Report SINTEF. 2017. Retrieved from: https://www.sintef.no/globalassets/sintef-teknologi-og-samfunn/rapporter-sintef-ts/rapport_is24_8_2017.pdf.
Hofstad T, Rugkåsa J, Ose SO, Nyttingnes O, Kjus SHH, Husum TL. Service Characteristics and Geographical Variation in Compulsory Hospitalisation: An Exploratory Random Effects Within–Between Analysis of Norwegian Municipalities, 2015–2018. Front Psychiatry. 2021;12:737698.
Clausen H, Landheim A, Odden S, Benth JŠ, Heiervang KS, Stuen HK, Killaspy H, Ruud T. Hospitalization of high and low inpatient service users before and after enrollment into Assertive Community Treatment teams: a naturalistic observational study. Int J Ment Heal Syst. 2016;10(1):14.
Stuen HK, Rugkåsa J, Landheim A, Wynn R. Increased influence and collaboration: a qualitative study of patients’ experiences of community treatment orders within an assertive community treatment setting. BMC Health Serv Res. 2015;15(1):409.
Stuen HK, Landheim A, Rugkåsa J, Wynn R. Responsibilities with conflicting priorities: a qualitative study of ACT providers’ experiences with community treatment orders. BMC Health Serv Res. 2018;18(1):1–11.
Dieterich M, Irving CB, Bergman H, Khokhar MA, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane database Syst Rev. 2017. Retrived from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007906.pub3/full.
Acknowledgements
We thank the staff at the NPR and at the NCDR for their support in data retrieval for this study. We are grateful for discussions and comments from lived-experience expert Solveig Helene Høymork Kjus during the planning of this study.
Funding
This study was funded by the Research Council of Norway (ref: 273546) as part of the Reducing Coercion in Norway (ReCoN) project. The funder had no role in study design, data collection, analysis or interpretation.
Author information
Authors and Affiliations
Contributions
ON planned the study after discussions and contributions from all co-authors. ON drafted the analysis plan, which was critically revised by JSB and JR. TH prepared and facilitated register data, together with ON. JSB planned and was responsible for statistical analysis in cooperation with ON. JR secured funding for the ReCoN project. ON drafted the manuscript. TH, JSB and JR critically reviewed the manuscript several times, and all authors approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved and the need for informed consent was waived by the Norwegian Regional Committee for Medical and Health Research Ethics (ref: 2018/795). According to Norwegian legislation, permission can be given to obtain and analyze de-identified data from registers without individual consent using data in existing health registers, when participants’ welfare and integrity are maintained. The NPR de-identified patients’ ID numbers before release in accordance with relevant regulations. The study and the Data Protection Impact Assessment (DPIA) were approved by the Privacy Ombudsman at Akershus University Hospital (ref: 2018–090). The authors assert that this work comply with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
Rugkåsa is a member of the editorial board of BMC Psychiatry. Benth, Hofstad and Nyttingnes declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nyttingnes, O., Benth, J.Š., Hofstad, T. et al. The relationship between area levels of involuntary psychiatric care and patient outcomes: a longitudinal national register study from Norway. BMC Psychiatry 23, 112 (2023). https://doi.org/10.1186/s12888-023-04584-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04584-4