Abstract
Background
Assertive Community Treatment (ACT) is more successful in reducing hospitalization when baseline use is high. However, with a growing recovery-focus, ACT may be useful for people with severe mental illness who are difficult to engage but not high users of inpatient services. This study investigated hospitalization 2 years before and 2 years after ACT enrollment amongst patients both with and without high inpatient services use before enrollment into ACT.
Methods
This naturalistic observational study included 142 patients from 12 different ACT teams throughout Norway. Of these, 74 (52 %) were high users of inpatient services before ACT. The teams assessed the patients upon enrollment using clinician-rated and self-reported questionnaires. Hospitalization data from 2 years before and 2 years after enrollment into ACT were obtained from the Norwegian Patient Registry. Linear mixed models were used to assess changes in hospitalization and to explore associations between these changes and patient characteristics.
Results
When the participants enrolled into the ACT teams, high users of inpatient care were younger, more often living alone and more often subject to involuntary outpatient treatment than low users. The participants spent significantly fewer days in hospital during the 2 years of ACT follow-up compared to the 2 years before enrollment. The reduction was more evident amongst high users, whereas low users had an initial increase in inpatient days in the first year of ACT and a subsequent decrease in the second year. More severe negative symptoms and previous high use of inpatient care were associated with a reduction in both total and involuntary inpatient days. Additionally, a reduction in involuntary inpatient days was associated with being subject to involuntary outpatient treatment upon enrollment into ACT.
Conclusion
The findings in this study may suggest that ACT contributes to more appropriate use of inpatient care, possibly by reducing the presumably avoidable hospitalization of high users and increasing the presumably needed inpatient care of low users.
Similar content being viewed by others
Background
Hospitalization is considered a proxy for symptom relapse in schizophrenia and is a frequently used measure of treatment effectiveness in studies investigating services that target this population [1, 2]. Assertive Community Treatment (ACT) is a well-documented model of community based care that provides outreach services to people with severe mental illness (schizophrenia, other psychotic disorders or severe bipolar disorder), co-morbidities and poor functioning [3–5]. ACT has been found to successfully reduce hospitalization amongst people with severe mental illness such as schizophrenia and bipolar affective disorder, who have difficulties engaging with standard care and experience recurrent cycles of relapse and readmission to mental hospitals [6, 7]. The ACT approach provides more flexible and intensive support, including evidence-based and individually tailored services in the community, than generic mental health services [7, 8].
One of the primary aims of ACT is to reduce the extent and associated cost of inpatient service use [3] but the setting in which ACT is more appropriate for implementation and effective is debatable [9, 10]. ACT has a superior effect on hospitalization over standard mental health services where there is less overlap between the support delivered by services [11, 12] and when it is focused on high users of inpatient care [6, 12]. Conversely, patients with low inpatient service use prior to ACT may experience an increase in hospitalization once under the care of ACT [13, 14]. Indeed, Mortimer and colleagues concluded that ACT is appropriate for patients with a range of needs, not only those who are high users of inpatient services [15].
ACT is intended for persons with mental illness with the most severe symptoms and disabilities who are prone to frequent or long admissions. This includes patients with poor community functioning who are not successfully engaged by less intensive and assertive services [7, 10]. Some of these patients may have limited contact with services [7] with few or no hospital admissions. In this scenario, hospitalization may help stabilize a difficult situation that might easily be overlooked by traditional, office-based mental health services. With the growing focus on recovery-oriented practices in ACT [8], these teams may offer benefits for patients with severe mental illness and high needs, even if their problems have not led to high use of inpatient services.
Identification of differences between high users and low users of inpatient care and factors associated with changes in hospitalization is therefore important to increase the understanding of the impact that ACT may have on these subgroups. However, different criteria have been used to define high use of inpatient care, either based on the number of admissions [13, 16, 17] or total inpatient days over a fixed time period [14, 18]. Definitions using only frequency exclude patients with few but long admissions while those using only duration exclude patients with frequent but short admissions. To our knowledge, the REACT study from the UK is the only ACT trial that applied criteria that accounted for both frequency and duration [19].
The ACT model was recently introduced to Norway to improve services to patients with severe mental illness (schizophrenia, other psychotic disorders or severe bipolar disorder) who were difficult to reach and engage by existing services. The Norwegian mental health service system is divided into two organizational levels, with primary health and social care provided at the municipal level and specialized mental health services provided by state-owned health authorities. The primary mental health care comprises general practitioners, individual or group therapy, self-help groups, day centers, and supported housing with full or partial supervision. The specialized mental health services comprise community mental health centers (CMHCs) and psychiatric departments in hospitals. The CMHCs comprise outpatient clinics, psychosis rehabilitation teams, substance abuse clinics day units, crisis resolution teams, and local inpatient facilities.
The key principles of ACT, including outreach, delivery of services in the community, holistic and integrated services, and continuity of care [20] may have been incorporated in standard mental health care internationally but this is not the case in many mental health care settings in Norway. The services are often fragmented and office-based, and the complexity of the service configuration may present impediments to access appropriate treatment for people with severe mental illness.
Estimates from 2008 suggested that more than 4000 persons with severe mental illness in Norway (approximately 1/1000 inhabitants) did not receive appropriate mental health services [21]. In 2009, the National Health Authorities decided to fund implementation of ACT teams across Norway to improve services for this population. Between December 2009 and February 2011, 12 ACT teams were established throughout the country. A history of high inpatient service use was not an inclusion criterion, and this provided an opportunity to investigate possible differences between high users and low users of hospitalization, applying the criteria used in the REACT study. Based on the existing ACT literature, we expect that high users would experience a decrease in hospitalization during ACT follow-up while hospitalization would increase among the low users.
Aims and research questions
This study aimed to investigate hospitalization (new admissions, total inpatient days, involuntary inpatient days) amongst high and low inpatient service users in the 2 years before and 2 years after enrollment into Norwegian ACT teams, and to explore factors associated with change in hospitalization. Our specific research questions were: are there significant socio-demographic or clinical differences between high users and low users of inpatient care upon ACT enrollment? Are there differences in hospitalization in the 2 years before ACT compared to the 2 years during ACT in the two groups? Are changes in hospitalization in the 2 years before ACT compared to the 2 years after enrollment associated with patient characteristics upon enrollment?
Methods
Design
This paper is based on data from the naturalistic observational study on ACT teams in Norway. Cross-sectional socio-demographic and clinical data from 142 patients of 12 ACT teams upon enrollment and longitudinal hospitalization data in the 2 years before and 2 years after ACT enrollment were used in this paper. Due to the nature of the funding and the implementation of the ACT model in Norway, it was not possible to conduct a randomized trial. However, a naturalistic observational study was designed to investigate patient outcomes in a real-life, clinical world.
Recruitment and sample
The ACT teams used inclusion criteria defined by the National Health Authorities which are similar to criteria used in international ACT studies: 18 years or older; severe mental illness (schizophrenia, schizoaffective, other psychotic disorder, bipolar affective disorder); impaired level of functioning; in need of long-term and comprehensive follow-up by mental health and social welfare services.
Patients with co-occurring substance misuse were included if this was not the primary diagnosis.
During the ACT teams’ first year of operation 337 patients enrolled in the 12 teams and they were all invited to participate in the study. A total of 202 patients (60 %) gave written informed consent to participate after the procedure was fully explained. Of these, 142 (42 %) received ACT services for at least 2 years, and were considered eligible for this study (participants n = 142). Data on inpatient service use was not available for the non-participants (n = 195).
Compared to the non-participants, fewer participants had problematic substance misuse (n = 83 versus 128, 59 % versus 70 %, p = 0.034). Participants had less severe symptoms (mean score ± standard deviation (SD) Global Assessment of Functioning-Symptom Scale (GAF-S), 41.4 ± 10.2 versus 38.8 ± 10.0, p = 0.028) and better functioning (mean score ± SD Global Assessment of Functioning-Function Scale (GAF-F), 39.7 ± 8.3 versus 37.6 ± 8.9, p = 0.036). There were no differences in age, gender, diagnosis of severe mental illness, or number of people subject to involuntary outpatient treatment.
The classification of high use of inpatient services prior to ACT were based on the inclusion criteria applied in the REACT study [19]: five or more psychiatric admissions in mental health hospitals or at least 100 consecutive inpatient days during the last 2 years, or three or more admissions or at least 50 consecutive inpatient days during the last year [19]. Of the 142 participants, 74 (52 %) were high users of inpatient services prior to ACT and 68 (48 %) were not.
Measures
Clinician-rated instruments
Socio-demographic data were collected using a form developed by the research group. Global level of functioning was assessed with the Global Assessment of Functioning (GAF) scale [22]. Psychiatric symptoms were assessed with the expanded version of the Brief Psychiatric Rating Scale (BPRS, version 4) [23, 24]. The BPRS-4 comprises 24 items, giving four subscales (i.e., positive symptoms, negative symptoms, agitation mania, and anxiety/depressive symptoms) [25]. Each item is given a score from 1 (not present) to 7 (extremely severe). Everyday functioning was measured with the revised version of the Practical and Social Functioning Scale (PSF) [26], consisting of 32 items. The mean total score ranges from 0 to 8, where higher scores indicate better functioning. An adapted version of the Homeless Engagement and Acceptance Scale (HEAS) [27] measured participants’ quality of engagement with services. The HEAS consists of four items, three rated from 0 to 4 and one from 0 to 3, giving a total score between 0 and 15. Higher scores indicate better service engagement.
Self-reported questionnaires
The alcohol use disorder identification test (AUDIT) [28] and the drug use disorder identification test (DUDIT) [29] are self-report instruments that screen for problematic substance use in the last 12 months. The AUDIT comprises ten and the DUDIT comprises eleven items, with total scores ranging from 0 to 40 (AUDIT) and 0 to 44 (DUDIT). Scores above specific cut-offs (AUDIT: men 8, women 6; DUDIT: men 6, women 2) indicate problematic substance use and higher score indicates greater severity.
Data-collection
Data on number of new admissions, total and involuntary inpatient days in mental health hospitals for the 142 participants in the 2 years before and the 2 years after enrollment into ACT was obtained from the Norwegian Patient Registry. Socio-demographic and clinical data were collected by the ACT teams when the participants enrolled into the teams. Both clinician-rated and self-reported questionnaires were used. Information was obtained through interviews with patients, care givers, and professionals, from direct observations and case-note reviews. The self-reported questionnaires were filled in by the participants alone or together with a team member.
Fidelity of Norwegian ACT teams
The Norwegian teams’ fidelity to the ACT model was assessed using the Tool for Measurement of Assertive Community Treatment (TMACT) [8]. The TMACT comprises 47 items, giving six subscales; organization and structure (OS), core team (CT, including team leader, nursing staff and psychiatric care provider), specialist team (ST, including substance abuse specialist, vocational specialist, and peer specialist), core practices (CP), evidence-based practices (EP) and person-centered planning and practices (PP). Each of the 47 items is rated on a 5-point scale from 1 (not implemented) to 5 (fully implemented). The fidelity was measured at 12 and 30 months after the teams were established. The mean TMACT scores at 12 months ranged from 2.7 to 3.7, indicating low to moderate fidelity and at 30 months the scores ranged from 3.1 to 4.1, indicating moderate to high fidelity. At 30 months, the mean scores on the different subscales showed low implementation on ST, moderate fidelity on CP, EP and PP, and high implementation on OS and CT.
Statistical analysis
Differences in socio-demographic and clinical characteristics between high and low users were assessed with Fisher’s exact test for dichotomous variables, Chi square test for categorical variables, Student’s T test for symmetrically distributed continuous variables, and Mann-Whitney U test for skewed continuous variables.
Total and involuntary inpatient days for four periods [time period (TP) 1: 24–12 months pre-ACT enrollment and TP2: 12–0 months pre-enrollment, TP3: 0–12 months post-enrollment and TP4: 12–24 months post-enrollment] were presented as means and 95 % confidence intervals (CI).
To assess changes in hospitalization the difference between the number of new admissions, total inpatient days and involuntary inpatient days in the 2 years before and the 2 years after ACT enrollment were defined as dependent variables.
The level of clustering within the team was assessed by an intra-class coefficient (ICC). Only a weak cluster effect was present but nevertheless, the difference in hospitalization between high and low users was analyzed by a linear mixed model with random effects at the ACT level, to correctly adjust the estimates for possible intra-ACT correlations. Fixed effect for variable identifying high and low users was entered into the model.
A multivariate linear mixed model was built with clinical variables [involuntary outpatient treatment (Y/N), the four BPRS subscales, AUDIT, DUDIT, HEAS, PSF, and high inpatient service use (Y/N)] as fixed effects to assess possible predictors for change in hospitalization. Random effects at the ACT level were included. The Akaike’s information criteria (AIC) (the smaller the better) [30] was applied for model reduction, but according to the AIC, none of the predictors could be eliminated. The final model was adjusted for age, gender and fidelity score (TMACT mean score at 30 months as this score was thought to best represent the 2 year follow-up period of the participants).
We imputed missing values on PSF items (n = 14, 0.3 % of cases), HEAS items (n = 2, 0.4 %), AUDIT (n = 14, 9.9 %) and DUDIT (n = 18, 12.7 %) by generating the empirical distribution for each variable and drawing a random number from that distribution to replace the missing value. The process was repeated until all missing values were imputed. The GAF scores were close to normally distributed, and missing values (n = 4, 2.8 % of cases) were imputed by drawing a random number from the corresponding normal distribution. The BPRS was completed for 98.6 % of the participants and thus we imputed no scores.
Linear mixed models were estimated by Statistical Analysis System version 9.3 (SAS Institute, Cary, NC USA). Other statistical analyses were performed with the Statistical Package for Social Science version 22 (SPSS, Chicago, IL USA). All tests were two-sided. p values below 0.05 were considered statistically significant. No correction for multiple hypothesis testing was performed as the study was exploratory.
Ethics, consent and permission
The study was approved by the Regional Committee for Medical and Health Research Ethics Health region South-East (ID: 2010/1196a). All participants gave written informed consent to participate in the study after the procedure of the study had been explained to them by the ACT teams.
Results
Characteristics of the groups
Upon ACT enrollment, the high users were younger, more likely to be subject to involuntary outpatient treatment, more likely to live in supported accommodations, be in prison or homeless, and less likely to live alone, as compared to the low users (Table 1). There were no significant differences in scores on clinical rating assessments between the groups.
Hospitalization
There were few differences between the 12 ACT teams regarding patients’ inpatient service use before ACT [total inpatient days (ICC = 7.4 %), involuntary inpatient days (ICC = 6.2 %)]. There were also only small differences between the teams regarding change in total inpatient days (ICC = 2.8 %) and involuntary days (ICC = 1.1 %).
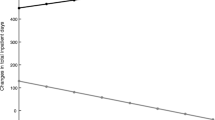
For the total sample, the mean number of new admissions was the same before and after ACT enrollment; on average, patients had three admissions in the 2 years before and three admissions in the 2 years after enrollment (Table 2). However, both total and involuntary inpatient days were halved in the 2 years after ACT enrollment compared to the 2 years before. There were significant differences in the changes in inpatient service use between the high and the low users. Total and involuntary inpatient days reduced amongst the high users, whilst the low users experienced an increase in the same period.
When comparing the three hospitalization outcomes in the four time periods (TP1, TP2, TP3, TP4, Table 3), the high users experienced an increase in all outcomes before ACT (TP1–TP2) and a decrease after ACT enrollment (TP2–TP4). However, the low users experienced an increase in new admissions throughout the period (TP1–TP4). Total and involuntary inpatient days were stable before ACT amongst the low users (TP1–TP2) but both outcomes increased in the first year after ACT enrollment (TP2–TP3) and subsequently decreased during the second year (TP 3–TP4). Non-overlapping confidence intervals between to consecutive periods indicate significant change between these two periods.
Patient characteristics associated with changes in inpatient days
The exploratory regression analyses showed that fidelity was not associated with changes in new admissions, total inpatient days or involuntary days. There were also no significant associations between change in new admissions and patient characteristics. However, more severe negative symptoms and high use of inpatient services before ACT were significantly associated with reduction in both total and involuntary inpatient days after ACT enrollment (Table 4). Being subject to involuntary outpatient treatment upon enrollment was also significantly associated with a reduction in involuntary inpatient days after ACT enrollment.
Discussion
Our study documented a decrease in total and involuntary inpatients days over the 2 years of ACT follow-up but no change in number of admissions. The decrease in inpatient days was more evident for the high users whilst for the low users there was an initial increase and a subsequent decrease in inpatient days after ACT enrollment. More severe negative symptoms upon ACT enrollment and high inpatient service use before ACT were significantly associated with a reduction in both total and involuntary inpatient days after ACT enrollment. Additionally, a reduction in involuntary inpatient days was significantly associated with being subject to involuntary outpatient treatment upon ACT enrollment.
Characteristics of the groups
Our findings that the high users were younger, more often subject to involuntary outpatient treatment and less likely to be living independently compared to the low users upon ACT enrollment is corroborated by previous studies [16, 17]. The fact that there were no differences in ratings of clinical problems between the groups may support the hypothesis of Mortimer and colleagues that ACT could be appropriate for patients with severe mental illness who are not high users of inpatient services [15]. According to the NICE guidelines, in addition to reducing the use of hospitalization, ACT teams should ensure continuous contact with services and improve psychosocial outcomes [3]. Intensive case management, including ACT, has been shown to have a significant advantage over other services in reducing the number of people who drop-out of contact with services [6]. It may be that the increase in hospitalization experienced by the low users represented an appropriate response to unmet clinical needs, or it may have shown a negative impact of ACT involvement. The fact that inpatient days reduced in the second year of ACT in this group perhaps gives more weight to the first explanation, suggesting that admission was necessary to attend to specific problems in order that the person could progress. Additionally, a recovery approach is an important part of ACT [14] and ACT may therefore provide a basis for recovery-oriented, assertive, and intensive services to patients with significant clinical needs who historically have not been high users of inpatient services.
Hospitalization
We found that the participants spent significantly fewer days in hospital during the 2 years of ACT follow-up compared to the 2 years before they enrolled into the teams. This is in contrast to findings from recent European randomized trials of ACT [19, 31], but is in line with several non-randomized studies [14, 15, 32, 33]. That the reduction in inpatient days was mainly found amongst the high users, supporting findings by Burns and colleagues [12] and Dietrich and colleagues [6].
Previous studies have suggested that ACT has most impact on hospitalization where there is less overlap with standard care services [11, 12]. In England, Crisis Resolution Teams (CRTs) and ACT teams were implemented simultaneously as part of a national policy and the subsequent reduction in use of hospitalization was attributed to the CRTs more than ACT [34], although this finding has been questioned [35]. In contrast, the CRTs in Norway were established before the ACT teams and serve a population with less severe symptoms [36]. This suggests that the presence of CRTs and ACT in the same catchment area is an unlikely explanation for the reduction in hospitalization found in our study.
When inpatient service use is already low, the effect of interventions aiming to reduce hospitalization is less likely to succeed [12, 37]. National data from 2009 [38] and 2013 [39] show that high users of inpatient services, of whom the majority suffer severe mental illness like schizophrenia, spend an average of 75–83 days in hospital per year. This is similar to the level of total inpatient days per year we found in our study in the 2 years before ACT but it is almost twice as high as the number of total inpatient days per year in the 2 years of ACT follow-up. This may indicate that, although the design of our study does not allow us to draw conclusions regarding the effect of ACT on hospitalization, it is unlikely that regression to the mean can fully explain the reduction found amongst high users in our study.
However, national policies on hospital bed availability can also influence use of inpatient services. Between 2009 and 2013 there was a 13 % reduction in the number of inpatient beds, a 15.3 % reduction in total inpatient days [39], and minor fluctuations in the use of involuntary inpatient treatment in Norway [40]. Although these figures include all patients, not only those with severe mental illness, they are unlikely to support the possibility that changes in inpatient services explain the much larger reduction in inpatient service use found in this study (reduction in total inpatient days for all participants 59.46 days, p < 0.001, reduction in involuntary inpatient days for all participants 44.20 days, p < 0.001). Furthermore, although total inpatient days were reduced during ACT follow-up, there was no increase in involuntary inpatient treatment. This could indicate that patients experiencing deterioration were identified at an earlier stage of relapse by ACT, prior to requiring involuntary admission.
Patient characteristics associated with changes in inpatient days
An increase in total inpatient days during ACT among patients with low baseline use has previously been reported [13, 14] and is not surprising, as reduction in total hospitalization is primarily found if baseline use is high [12]. High use of inpatient services and involuntary outpatient treatment were both associated with reduced inpatient service use, as was having more severe negative symptoms upon ACT enrollment. Although exploratory, our findings may support the hypothesis that hospitalization during ACT can mark the beginning of access to care and recovery for patients with prior low inpatient service use [13], and that ACT may contribute to more appropriate use of inpatient services and involuntary hospitalization amongst patient both with and without high inpatient service use.
Our study showed no associations between the teams’ fidelity score at 30 months and changes in hospitalization after ACT enrollment, in contrast to recent reports that higher TMACT scores were associated with decreased hospital use [41]. However, our study was exploratory so our findings should be interpreted with caution.
Strengths and limitations
A major strength of our study is that we have data from 12 different ACT teams operating in both urban and rural areas, covering all parts of Norway. Instruments with good psychometric properties were used. However, our study is an observational study and not a randomized controlled trial and therefore subject to potential confounders. We cannot conclude that the reduction in hospitalization observed was due to ACT, although the reduction was similar across teams and much higher than the national reduction in inpatient service use. Our sample included only those who gave informed consent and had received ACT for at least 2 years in Norway. Therefore our results may not be generalizable to all ACT patients. Finally, there were fewer participants than non-participants with substance abuse and the participants had statistically better functioning and less severe symptoms. This may have contributed to an overestimation of the reduction in total and involuntary inpatient days found in this study although the difference in symptom and functioning levels between the groups may not have been clinically significant.
Conclusion
This study showed a clear reduction in both total and involuntary inpatient days after the patients enrolled into ACT. The reduction was mainly due to fewer inpatient days amongst the high users. The low users experienced an initial increase in inpatient days, perhaps required to attend to needs that had not been identified by other services. Our results suggest that ACT may contribute to a more appropriate use of inpatient care for both groups, possibly by reducing the presumably avoidable hospitalization of high users and increasing the presumably undetected but needed inpatient care by the low users.
Abbreviations
- ACT:
-
Assertive Community Treatment
- CMHC:
-
Community Mental Health Centers
- GAF:
-
Global Assessment of Functioning
- BPRS:
-
Brief Psychiatric Rating Scale
- PSF:
-
practical and social functioning
- HEAS:
-
Homeless Engagement and Acceptance Scale
- AUDIT:
-
Alcohol Use Disorder Identification Scale
- DUDIT:
-
Drug Use Disorder Identification Scale
- TMACT:
-
tool for measurement of Assertive Community Treatment
- OS:
-
organization and structure
- CT:
-
Core Team
- ST:
-
Specialist Team
- CP:
-
core practices
- EP:
-
evidence-based practices
- PP:
-
person-centered planning and practices
- TP:
-
time period
- CI:
-
confidence interval
- ICC:
-
intra-class correlation coefficient
- AIC:
-
Akaike’s information criteria
- SAS:
-
statistical analysis system
- SPSS:
-
statistical package for social science
- CRT:
-
Crisis Resolution Team
- SD:
-
standard deviation
References
Olivares JM, Sermon J, Hemels M, Schreiner A. Definitions and drivers of relapse in patients with schizophrenia: a systematic literature review. Ann Gen Psychiatry. 2013;12(1):32.
Burns T. Hospitalisation as an outcome measure in schizophrenia. Br J Psychiatry Suppl. 2007;50:s37–41.
Kuipers E, Kendall T, Antoniou J, Barnes T, Bhui K, Bird V, Brabban A, Flanagan E, Garety P, Hopkins S et al. The NICE guidelines on core interventions in the treatment and management of schizophrenia in adults in primary and secondary care—updated edition. In: National Collaborating Centre for Mental Health. 2010: 338.
Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, Lehman A, Tenhula WN, Calmes C, Pasillas RM, et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):48–70.
Mueser KT, Deavers F, Penn DL, Cassisi JE. Psychosocial Treatments for Schizophrenia. Annu Rev Clin Psychol. 2013;9(1):465–97.
Dieterich M, Irving CB, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database Syst Rev (Online). 2010;6(10):CD007906.
Allness DJ, Knoedler WH. A manual for ACT start-up: based on the PACT model of community treatment for persons with severe and persistent mental illnesses. National Alliance for the Mentally III. 2003.
Monroe-DeVita M, Teague GB, Moser LL. The TMACT: a new tool for measuring fidelity to assertive community treatment. J Am Psychiatr Nurses Assoc. 2011;17(1):17–29.
Burns T, Catty J, Watt H, Wright C, Knapp M, Henderson J. International differences in home treatment for mental health problems: results of a systematic review. Br J Psychiatry. 2002;181(5):375–82.
Rosen A, Mueser KT, Teesson M. Assertive community treatment–issues from scientific and clinical literature with implications for practice. J Rehabil Res Dev. 2007;44(6):813–25.
Marshall M, Bond G, Stein LI, Shepherd G, McGrew J, Hoult J, Rosen A, Huxley P, Diamond RJ, Warner R et al. PRiSM psychosis study. Design limitations, questionable conclusions, vol. 175; 1999.
Burns T, Catty J, Dash M, Roberts C, Lockwood A, Marshall M. Use of intensive case management to reduce time in hospital in people with severe mental illness: systematic review and meta-regression. BMJ. 2007;335(7615):336.
Bonsack C, Adam L, Haefliger T, Besson J, Conus P. Difficult-to-engage patients: a specific target for time-limited assertive outreach in a Swiss setting. Can J Psychiatry Revue canadienne de psychiatrie. 2005;50(13):845–50.
Morrissey JP, Domino ME, Cuddeback GS. Assessing the Effectiveness of Recovery-Oriented ACT in Reducing State Psychiatric Hospital Use. Psychiatr Serv (Washington, DC). 2013;64(4):303–11.
Mortimer AM, Shepherd CJ, Fadahunsi A, Jones A, Kumar P, Gangaram P. Assertive outreach: mirror-image study with contemporaneous controls. Psychiatrist. 2012;36(7):245–8.
Graca J, Klut C, Trancas B, Borja-Santos N, Cardoso G. Characteristics of Frequent Users of an Acute Psychiatric Inpatient Unit: a Five-Year Study in Portugal. Psychiatr Serv. 2013;64(2):192–5.
Morlino M, Calento A, Schiavone V, Santone G, Picardi A, de Girolamo G. Use of psychiatric inpatient services by heavy users: findings from a national survey in Italy. Eur Psychiatry. 2011;26(4):252–9.
Domino ME, Morrissey JP, Cuddeback GS. The Effectiveness of Recovery-Oriented ACT in Reducing Hospital Use: do Effects Vary Over Time? Psychiatr Serv (Washington, DC). 2013;64(4):312–7.
Killaspy H, Bebbington P, Blizard R, Johnson S, Nolan F, Pilling S, King M. The REACT study: randomised evaluation of assertive community treatment in north London. BMJ. 2006;332(7545):815–20.
Bond GR, Drake RE. The critical ingredients of assertive community treatment. World Psychiatry. 2015;14(2):240–2.
Huus G, Storm-Olsen B, Herheim Å: Mennesker med alvorlige psykiske lidelser og behov for særlig tilrettelagte tilbud. In.: Helsedirektoratet; 2008.
Goldman HH, Skodol AE, Lave TR. Revising Axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149(9):1148–56.
Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: “The drift busters.”. Int J Methods Psychiatr Res. 1993;3(4):221–44.
Ventura J, Lukoff D. K.H. N, Liberman RP, Green MF, Shaner A: brief Psychiatric Rating Scale (BPRS) expanded version: scales, anchor points, and administration manual. Int J Methods Psychiatr Res. 1993;3:227–43.
Kopelowicz A, Ventura J, Liberman RP, Mintz J. Consistency of Brief Psychiatric Rating Scale factor structure across a broad spectrum of schizophrenia patients. Psychopathology. 2008;41(2):77–84.
Rishovd Rund B, Ruud T. Måling av funksjonsnivå og funksjonsendring i psykiatrisk behandling. Oslo: Statens helsetilsyn; 1994.
Park MJ, Tyrer P, Elsworth E, Fox J, Ukoumunne OC, MacDonald A. The measurement of engagement in the homeless mentally ill: the Homeless Engagement and Acceptance Scale–HEAS. Psychol Med. 2002;32(5):855–61.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT - The Alcohol Use Disorder Identification Test: Guidelines for use in primary care. Geneva: World Health Organization; 2001.
Berman AH, Bergman H, Palmstierna T, Schlyter F. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res. 2005;11(1):22–31.
Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19(6):716–23.
Sytema S, Wunderink L, Bloemers W, Roorda L, Wiersma D. Assertive community treatment in The Netherlands: a randomized controlled trial. Acta Psychiatr Scand. 2007;116(2):105–12.
Commander M, Sashidharan S, Rana T, Ratnayake T. North Birmingham assertive outreach evaluation. Patient characteristics and clinical outcomes. Soc Psychiatry Psychiatr Epidemiol. 2005;40(12):988–93.
Davidson G, Campbell J. An Examination of the Use of Coercion by Assertive Outreach and Community Mental Health Teams in Northern Ireland. Br J Soc Work. 2007;37(3):537–55.
Glover G, Arts G, Babu KS. Crisis resolution/home treatment teams and psychiatric admission rates in England. Br J Psychiatry. 2006;189:441–5.
Jacobs R, Barrenho E. Impact of crisis resolution and home treatment teams on psychiatric admissions in England. Br J Psychiatry. 2011;199(1):71–6.
Hasselberg N, Grawe RW, Johnson S, Ruud T. An implementation study of the crisis resolution team model in Norway: are the crisis resolution teams fulfilling their role? BMC Health Serv Res. 2011;11:96.
Burns T. End of the road for treatment-as-usual studies? vol. 195; 2009.
Pedersen PB, Sitter M, Lilleeng SE, Bremnes R. Pasienter i det psykiske helsevernet 2009 [Patients in Norwegian adult mental health services 2009]. In. Oslo: Helsedirektoratet; 2009.
Helsedirektoratet: SAMDATA Spesialisthelsetjenesten 2013 [Specialized health care in Norway 2013]. In. Trondheim: Helsedirektoratet; 2014.
Helsedirektoratet: Bruk av tvang i psykisk helsevern for voksne 2013 [Use of Coercion in Norwegian Mental Health Care for adults 2013]. In. Oslo: Helsedirektoratet; 2014.
Cuddeback GS, Morrissey JP, Domino ME, Monroe-Devita M, Teague GB, Moser LL. Fidelity to Recovery-Oriented ACT Practices and Consumer Outcomes. Psychiatric Serv. 2013;64(4):318–23.
Authors’ contribution
TR, AL designed the national evaluation on ACT teams in Norway with significant support from SO, HKS, KSH, HK and HC. The research questions were formulated by TR, AL, HK and HC. Literature search was performed by HC and the statistical analyses were conducted and interpreted by JSB and HC with substantial support from TR, AL and HK. HC wrote the manuscript which was substantially revised by TR, AL and HK. The final version was prepared and revised by all authors and all authors approved for submission. All authors read and approved the final manuscript.
Acknowledgements
This report is based on data from a national evaluation of ACT in Norway, which is funded by the Norwegian Directorate of Health. The authors thank the ACT teams for collecting data.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Clausen, H., Landheim, A., Odden, S. et al. Hospitalization of high and low inpatient service users before and after enrollment into Assertive Community Treatment teams: a naturalistic observational study. Int J Ment Health Syst 10, 14 (2016). https://doi.org/10.1186/s13033-016-0052-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13033-016-0052-z