Abstract
Background
Previous studies have revealed that single physical chronic condition was associated with suicidal ideation/plans, but few studies have examined the relationship between multimorbidity and suicidal ideation/plans, and no studies have explored the underlying potential mechanism on this relationship in China. This study aimed to explore association between physical multimorbidity and suicidal ideation as well as plans, and further examine the mediating role of psychological distress (PD) on this relationship.
Methods
This study was based on the data from a survey about the health service of rural elderly household in Shandong, China. A total of 3242 adults aged 60 years and older were included in this study. PD was measured by Kessler Psychological Distress Scale (K10). Ordinal and binary logistic regression analyses were employed to explore the association between physical multimorbidity, PD and suicide ideation/plans. Bootstrapping analysis was further used to examine the mediation effect of PD on the association of multimorbidity and suicidal ideations/plans.
Results
The prevalence of multimorbidity, lifetime suicidal ideation, and suicidal plan in rural older adults was 35.2, 10.6 and 2.2%, respectively. Older adults living in rural areas with two or more chronic physical conditions experienced significantly higher risk of suicidal ideation and suicidal plans. The association between multimorbidity and suicidal ideations/plans was partially mediated by PD, of which, the mediating effect of PD accounted for 31.7 and 25.5% of the total effect, respectively.
Conclusion
This study demonstrated the associations between physical multimorbidity and suicidal ideation/plans, and the mediating role of PD on this relationship among Chinese rural elderly. Healthcare providers in rural community should provide regular surveillance for the mental health status among the rural elderly with multimorbidity, and carry out various effective intervention measures to improve the mental health status, so as to reduce the risk of suicide.
Similar content being viewed by others
Background
Suicide is a serious public health issue worldwide and nearly 800,000 people died from suicide every year. Although the overall suicide rate in China has decreased over the past few decades [1, 2], it remains high among the elderly in China [3]. A recent study indicated that suicide rate among the elderly aged 65–85 years was 2.75–7.08 times higher than that of the general population in China [4]. According to World Health Organization (WHO) report, the suicide rate was highest in population aged over 70 years across different regions in the world. Currently, the suicide rate is about 51.5 per 100,000 people among the elderly in China [5, 6]. This rate was found to be significantly higher among older people in rural than that in urban areas [7, 8]. A study revealed that the mean annual suicide rate among the elderly aged 60–84 years in rural and urban areas was 82.8 per 100,000 people and 16.7 per 100,000 people, respectively [9]. With a rapid increase of elderly population, there is an urgent need to prevent suicide among the older adults, especially in rural areas.
Previous studies have shown that suicidal ideation, plans, and attempts were important predicators of later suicide [10,11,12,13]. The early detection of suicidal ideation and plans is one of the critical primary prevention measures for suicide [14]. However, the current prevention measures mainly focus on the secondary prevention (suicide attempts) and the tertiary prevention (suicide) [15, 16]. Therefore, to identify potential influencing factors for suicidal ideation and plans is of priority.
Physical chronic conditions were found to be related with higher odds of reporting suicidal behaviors among the elderly [17, 18]. Moreover, more and more people were found to be affected by more than one physical condition, especially among the elderly [19, 20]. The existence of two or more physical chronic conditions in an individual was known as multimorbidity [19]. Previous studies in some other countries further found that multimorbidity was associated with suicidal related behaviors. A study by Scott and colleagues revealed that the risk of suicidal outcomes was increased with the increase of the number of physical chronic conditions [21]. Another study in Korea showed that the adults with multimorbidity experienced higher prevalence of suicide thoughts and plans [22]. Although previous studies have demonstrated that the relationship between multimorbidity and suicidal ideation/plans, few studies have explored this association among the elderly, and the underlying potential mechanism or pathways on this relationship is still rarely explored.
Psychological distress (PD) is largely defined as a state of emotional suffering, typically characterized by depressive and anxiety symptoms. PD is an important and widely-used indicator in evaluating the psychological health of the population [23,24,25], which was assessed by Kessler Psychological Distress Scale (K10) in the present study. The relationship between single chronic conditions (such as cancer, diabetes, hypertension) and mental disorder has been well established [26]. Recently, more and more studies have focused on the relationship between multimorbidity and PD. A study conducted in Australia showed that the risk of PD increased with the number of chronic conditions in adults [27]. Another study further showed that three or more chronic conditions conferred a 2.30-fold increase in elevated anxiety among the older adults [28]. Furthermore, a number of studies have examined the association between PD and suicidal related behaviors and revealed that PD was correlated with suicidal ideation, plans and attempts [29, 30]. Similarly, PD was also found to be the strongest predicator of suicidal ideation across different age groups [31]. About 90% of suicides were found to have mental disorders before their death [32]. Thus, PD might be a mediator between the association between chronic conditions and suicidal ideations or plans.
The aim of the present study is to investigate the prevalence of suicidal ideations/plans and further examine the association between physical multimorbidity and suicidal ideation and suicidal plans, as well as to explore the mediating role of PD on this relationship among rural elderly in China. The main hypotheses of this study are as follows: First, there is a significant association between physical multimorbidity and suicidal ideations as well as suicidal plans in rural older adults; Second, PD is a mediator between multimorbidity and suicidal ideations as well as suicidal plans in rural older adults.
Methods
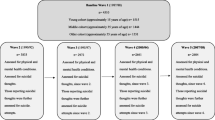
Data source and sample
Data of this study were from a survey about the health status of rural elderly in Shandong, China, which was conducted in 2019. Shandong is the second most populous province of China with a number of 107 million people in 2018, and also the province with largest number of elderly population in China.
This study used a three-stage stratified cluster method to select the participants, which was explained in detail elsewhere [33]. Finally, 3242 elderly living in the study sites were interviewed, with a respondent rate of 90.05%.
Measurements
Lifetime suicidal ideation/plans
In this study, suicidal ideation was measured by a widely used question of “Have you ever seriously considered about suicide/killing yourselves?” For those who answered “Yes”, they would be further asked “Have you ever make a plan for suicide?” to measure suicidal plans. This question is from the US National Comorbidity Survey (NCS) [34], and many previous studies conducted in China also used this question to measure suicidal ideation, which was proved to be of high reliability and validity [35].
Physical multimorbidity
Physical chronic condition was measured by using the self-reported question that “Have you ever been diagnosed with a chronic condition by a physician?” The answer contained “Yes” or “No”, and if the answer was “Yes”, they would be further asked “How many chronic conditions have you ever been diagnosed by a doctor?” The chronic conditions in this study only refer to physical chronic illness. In order to ensure the accuracy of the interview information, the interviewers would further ask the interviewees about their medication details and also sought help from the village doctors to validate the physical chronic conditions information in the health management system in the sampling villages. One person with two or more chronic conditions was defined as physical multimorbidity. This study used the ordinal forms of multimorbidity (0, 1, 2, 3, 4+) to better show the relationship between chronic conditions and other main variables.
Psychological distress
PD was measured by K10, which was used to evaluate the respondents’ psychological conditions that characterized by depression and anxiety [25]. Previous study in China has demonstrated the reliability and validity of the K10 [36]. This scale scored from 10 to 50 points, and the lower scores reflected the better psychological health status. Based on the nature of data, the PD was divided into four categories: low (scores range from 10 to 15), moderate (scores range from 16 to 21), high (scores range from 22 to 29), and very high PD (scores range from 30 to 50).
Other controlling variables
Sleep disturbance was measured by the Pittsburgh sleep quality index (PSQI) [37]. The PSQI was the self-reported questionnaire that used to assess the sleep quality/disturbance during the 1-month period, which included seven components that scoring from 0 to 21 and higher scores reflect the worse sleep quality. In this study, PSQI was dichotomized into without sleep disturbance and with sleep disturbance; the cut-off of PSIQ of 7 has received good sensitivity and specificity in China [38]. Household income was classified into four categories according to quartile, including Q1, Q2, Q3, and Q4. Among them, Q1, Q2, Q3, and Q4 represented the lowest, middle-low, middle-high, and highest economic status group, respectively. Marital status was categorized into single and married, of which, singles included the never married, the widowed, and the divorced, and married included the first marriage and re-marriage. In addition, the controlling variables also included gender, age, education, alcohol drinking, cigarette smoking, and physical exercise.
Statistical analysis
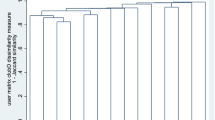
IBM SPSS version 22.0 and Stata 14.0 were employed for analysis. The present study described the basic characteristics of respondents with mean (standard deviation) or frequencies (percentage). According to the mediation testing technology proposed by Baron and Kenny [39], the ordinal logistic regression model was firstly performed to examine the relationship between physical multimorbidity and PD. Secondly, the binary logistic regression model was performed to explore the association between physical multimorbidity and suicidal ideation as well as suicidal plans. Thirdly, the binary logistic regression model was used to further explore the association between physical multimorbidity and suicidal ideation as well as suicidal plan when PD included in this model. The statistically significant threshold was based on two-sided and 0.05-level tests. Moreover, spearman coefficient was used to determine the correlation between main variables, and nonparametric bootstrapping (with 5000 bootstrap samples) was employed to validate the mediation effect, and if the 95% CI excluded zero was regarded as statistically significant.
Results
Socio-demographic characteristics
The basic characteristics of the respondents were presented in Table 1. Among the 3242 participants, the majority of them were female (63.5%), with the education level of primary school or below (80.5%), married (74.5%), and had sleep disturbance (47.4%). The average age was 70.1 ± 6.2 years.
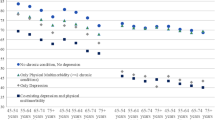
Description of physical multimorbidity, PD and suicidal ideation/plans
Regarding the suicidal ideation/plans, of the respondents, 10.6 and 2.2% reported lifetime suicidal ideation and suicidal plans, respectively. As for the chronic conditions, 35.2% of participants had more than two chronic physical illnesses, with 24.7% reporting two illnesses, 8.8% reporting three illnesses, and 1.7% reporting four and above illnesses. In the aspect of PD, 23.5% of respondents experienced high/very high level of PD.
Association between physical multimorbidity and psychological distress
As shown in Table 2, after adjusting for sex, age, education, marital status, alcohol drinking, household income, cigarette smoking, physical exercise, and sleep disturbance, chronic conditions were significantly related with PD. The odds of reporting PD increased with the number of chronic conditions.
PD mediated the association between physical multimorbidity and suicidal ideation/plans. As shown in Tables 3 and 4, when PD was included in model 2, the result showed that the increasing number of chronic conditions was still significantly correlated with suicidal ideations as well as suicidal plans. Moreover, bootstrap results showed that the direct effect, indirect effect, and total effect were also statistically significant, and the total effect of physical multimorbidity on suicidal ideation as well as suicidal plans were partially explained by PD, of which, the indirect effect accounting for 31.7 and 25.5% of total effect, respectively.
Discussion
This population-based study found that physical multimorbidity was associated with lifetime suicidal ideation as well as suicidal plans in rural older adults. For the first time, this study tried to explore the potential mediating effect of PD on this relationship, and the results showed that PD was associated with suicidal ideation as well as suicidal plans, and partially mediated the association between multimorbidity and suicidal ideation/plans.
The present study found the prevalence of lifetime suicidal ideation and suicidal plans in rural elderly (60+) was 10.6 and 2.2%, respectively. The prevalence of suicidal ideation in present study was much higher than the 4.8% among rural elderly (65+) in Beijing reported by Ma et al. [40], the 5.2% in rural older adults (65+) in Shandong reported by Ge et al. [41], and the 9.4% among U.S. Chinese elderly (60+) reported by Dong and colleagues [42]. Meanwhile, the prevalence of suicidal plans in this study was higher than the 0.51% among elderly (65+) in Spain reported by Miret and colleagues. The lifetime prevalence of suicidal ideation and suicide plans in present study were both lower than 34.5 and 10.3% of elderly (65+) in a remote rural area of China that found by Chiu et al. [11]. One possible reason for such difference is that the sample size of Chiu et al.’ s study was relatively small and only 87 participants were included in the study. Another possible reason is that, the prevalence of suicidal ideation/plans was age-related. The older the elderly, the higher the prevalence. The age inclusion criteria by Chiu et al.’ s study was 65 years and above, which was older than the current study.
Congruent with our hypothesis, we found that the presence of two or more physical chronic conditions were significantly associated with suicidal ideation and suicidal plans. In the fully adjusted model, the elderly with two or more chronic conditions had higher odds of experiencing suicidal ideation and plans compared to those without any physical condition. This finding was consistent with a previous study, which demonstrated that the increasing number of chronic conditions were related with higher risks of suicidal ideation and plans in US population [43]. Huh et al. reported elderly (65+) with multimorbidity had higher prevalence of suicidal thoughts than those without multimorbidity in Korea [22]. Some previous studies showed that compared with those with no physical conditions, the elderly with multimorbidity were more likely to have disability, poor physical and mental health-related quality of life [44, 45], and it is intolerable for some older adults when these adverse consequences have accumulated to a certain extent. That was to say, multimorbidity may cause more seriously adverse health outcomes, thus increased the likelihood of suicidal ideation/plans of the patients.
Furthermore, we found that PD were independently associated with both multimorbidity and suicidal ideation/plans, and partially mediated the association between them. Although there was no study to explore the mediating role of PD in the association between multimorbidity and suicidal ideation/plans, a previous study conducted in China suggested that depression partly mediated the association between multimorbidity and health-related quality of life in older adults [46]. As mentioned above, the possible interpretation of this finding might be that the multiple adverse outcomes caused by multimorbidity may directly or indirectly increase the risk of PD, which in turn further stimulates the occurrence of the suicidal ideation/plans. A review suggested that the patients with multimorbidity were twice as likely to experience depression than those without multimorbidity [47]. A study conducted in Canada indicated that people with obesity and multimorbidity had higher probability of reporting mental disorders [48]. In addition, multimorbidity was associated with increased risk of loneliness, social exclusion, function limitations, and economic burden, all of which may negatively affect the PD [49,50,51]. Several previous studies also found that PD was one of the strongest influencing factors of suicidal related behaviors [52, 53]. Thus, multimorbidity may have indirect effect on suicidal ideation as well as suicidal plans via inducing the PD. Some previous studies demonstrated that health care utilization and spending increased with the number of chronic conditions among the elderly [54,55,56], and a large proportion of the healthcare cost for multimorbidity was out-of-pocket paid by the rural elderly themselves, which may be more economically disadvantaged and impose financial hardship for their households. Moreover, as the origin of the Confucius culture, the elderly in rural Shandong were more traditional and conservative [57]. For those with multiple chronic conditions, they were fear of becoming a burden to their families and bearing higher level of PD for a long time. This existence of mental disorders may be one of the triggers of stressful life events, and ultimately increase the risk of suicide [58].
The findings in this study implied for the healthcare providers in rural communities to strengthen the regular screening and management of chronic conditions among the elderly to prevent or retard the presence of the multimorbidity, and further to reduce the chronic condition burden. More importantly, a regular surveillance for the mental health status should be taken among the rural elderly with multimorbidity, and various effective intervention measures should be carried out to improve the mental health status, so as to reduce the risk of suicide.
This study had several limitations. First, the information about number of physical chronic conditions and suicidal ideation/plans was self-reported, which might lead to recall basis. Second, although the US National Comorbidity Survey (NCS) and many previous studies have used the question “Have you ever seriously considered about suicide/killing yourselves?” to measure suicidal ideation, this question cannot be used as a standard instrument for assessing suicidal ideation. In addition, although previous studies have found that older adults who committed suicide were more likely to have antidepressants detected in the blood [59], the information about diagnosed mental illness and medication (e.g., antidepressant use information) was not collected in our study, which would be remedied in the follow-up studies. Third, based on the availability of data, we only examined the relationship between the number of chronic conditions and suicidal ideation/plans, further studies would investigate whether the pattern, length, or severity of chronic conditions were associated with suicidal ideation/plans. Fourth, the present study was based on cross-sectional design, so we could not infer the casual relationship between multimorbidity, PD, and suicidal ideation as well as plans, prospective studies were needed in the future to elucidate the causal association.
Conclusions
This study demonstrated the significant associations between physical multimorbidity and suicidal ideation/plans, and the mediating role of PD on this relationship among Chinese rural elderly. In rural areas, policy makers and healthcare providers should strengthen the prevention and management of chronic conditions among the elderly, to prevent or retard the presence of chronic conditions, especially the multimorbidity. In addition, a regular surveillance for the mental health status should be taken among the rural elderly with multimorbidity, and various effective intervention measures should be carried out to improve the mental health status, so as to reduce the risk of suicide.
Availability of data and materials
Our data may not be shared directly, because it is our teamwork. Informed consent should be attained from all the team members. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PD:
-
Psychological distress
- WHO:
-
World Health Organization
- PSQI:
-
Pittsburgh sleep quality index
References
Jiang H, Niu L, Hahne J, Hu M, Fang J, Shen M, Xiao S. Changing of suicide rates in China, 2002–2015. J Affect Disorders. 2018;240:165–70.
World Health Organization. World health statistics 2016: monitoring health for the SDGs sustainable development goals. Geneva: World Health Organization; 2016.
Li Y, Li Y, Cao J. Factors associated with suicidal behaviors in mainland China: a meta-analysis. BMC Public Health. 2012;12(1):524.
Lien SS, Kosik RO, Fan AP, Li W, Jiang Y, Huang L, Zhao X, Chen Q. Injury and suicide in people aged 60 years and over in China: an analysis of nationwide data. Lancet. 2018;392:S41.
World Health Organization. Preventing suicide: A global imperative. Geneva: World Health Organization; 2014.
Li X, Xiao Z, Xiao S. Suicide among the elderly in mainland China. Psychogeriatrics. 2009;9(2):62–6.
Li M, Katikireddi SV. Urban-rural inequalities in suicide among elderly people in China: a systematic review and meta-analysis. Int J Equity Health. 2019;18(1):2.
World Health Organization: China country assessment report on ageing and health. 2015.
Phillips MR, Li X, Zhang Y. Suicide rates in China, 1995–99. Lancet. 2002;359(9309):835–40.
Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. Jama. 2005;293(20):2487–95.
Chiu H, Dai J, Xiang YT, Chan S, Leung T, Yu X, Hou ZJ, Ungvari GS, Caine ED. Suicidal thoughts and behaviors in older adults in rural China: a preliminary study. Int J Geriatr Psych. 2012;27(11):1124–30.
Cao X, Zhong B, Xiang Y, Ungvari GS, Lai KY, Chiu HF, Caine ED. Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. Int J Psychiatry Med. 2015;49(4):296–308.
Zhang D, Yang Y, Sun Y, Wu M, Xie H, Wang K, Zhang J, Jia J, Su Y. Characteristics of the Chinese rural elderly living in nursing homes who have suicidal ideation: a multiple regression model. Geriatr Nurs. 2017;38(5):423–30.
Harris KM, Syu J, Lello OD, Chew YE, Willcox CH, Ho RH. The ABC’s of suicide risk assessment: applying a tripartite approach to individual evaluations. PLoS One. 2015;10(6):e127442.
Vilhjálmsson R, Sveinbjarnardottir E, Kristjansdottir G. Factors associated with suicide ideation in adults. Soc Psych Psych Epid. 1998;33(3):97–103.
Kye S, Park K. Suicidal ideation and suicidal attempts among adults with chronic diseases: a cross-sectional study. Compr Psychiat. 2017;73:160–7.
HTT V, Nguyen TX, HTT N, Le TA NTN, Nguyen AT, TTH N, Nguyen HL, Nguyen CT, Tran BX. Depressive symptoms among elderly diabetic patients in Vietnam. Diabetes Metab Syndr Obes. 2018;11:659.
Ng A, Tam WW, Zhang MW, Ho CS, Husain SF, McIntyre RS, Ho RC. IL-1β, IL-6, TNF-α and CRP in elderly patients with depression or Alzheimer’s disease: systematic review and meta-analysis. Sci Rep-UK. 2018;8(1):1–12.
Mercer S, Furler J, Moffat K, Fischbacher-Smith D, Sanci L. Multimorbidity: technical series on safer primary care. Geneva: World Health Organization; 2016.
MacMahon S. Multimorbidity: a priority for global health research. London: The Academy of Medical Sciences; 2018.
Scott KM, Hwang I, Chiu W, Kessler RC, Sampson NA, Angermeyer M, Beautrais A, Borges G, Bruffaerts R, De Graaf R. Chronic physical conditions and their association with first onset of suicidal behavior in the world mental health surveys. Psychosom Med. 2010;72(7):712–9.
Huh Y, Nam GE, Kim Y, Lee JH. Relationships between multimorbidity and suicidal thoughts and plans among Korean adults. J Clin Med. 2019;8(8):1094.
Andrews G, Slade T. Interpreting scores on the Kessler psychological distress scale (K10). Aust NZ J Publ Heal. 2001;25(6):494–7.
Drapeau A, Marchand A, Beaulieu-Prévost D. Epidemiology of psychological distress. Mental illnesses-understanding, prediction and control. 2012;69:105–6.
Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76.
Verhaak PF, Heijmans MJ, Peters L, Rijken M. Chronic disease and mental disorder. Soc Sci Med. 2005;60(4):789–97.
Holden L, Scuffham P, Hilton M, Vecchio N, Whiteford H. Psychological distress is associated with a range of high-priority health conditions affecting working Australians. Aust NZ J Publ Heal. 2010;34(3):304–10.
Gould CE, O'Hara R, Goldstein MK, Beaudreau SA. Multimorbidity is associated with anxiety in older adults in the health and retirement study. Int J Geriatr Psych. 2016;31(10):1105–15.
De Beurs D, Ten Have M, Cuijpers P, De Graaf R. The longitudinal association between lifetime mental disorders and first onset or recurrent suicide ideation. BMC Psychiatry. 2019;19(1):345.
O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85.
Miret M, Caballero FF, Huerta-Ramírez R, Moneta MV, Olaya B, Chatterji S, Haro JM, Ayuso-Mateos JL. Factors associated with suicidal ideation and attempts in Spain for different age groups. Prevalence before and after the onset of the economic crisis. J Affect Disorders. 2014;163:1–9.
Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405.
Jing Z, Li J, Wang Y, Ding L, Tang X, Feng Y, Zhou C. The mediating effect of psychological distress on cognitive function and physical frailty among the elderly: evidence from rural Shandong, China. J Affect Disorders. 2020;268:88–94.
Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–26.
Lee S, Fung SC, Tsang A, Liu ZR, Huang Y, He YL, Zhang MY, Shen Y, Nock MK, Kessler RC. Lifetime prevalence of suicide ideation, plan, and attempt in metropolitan China. Acta Psychiat Scand. 2007;116(6):429–37.
Zhou C, Chu J, Wang T, Peng Q, He J, Zheng W, Liu D, Wang X, Ma H, Xu L. Reliability and validity of 10-item Kessler scale (K10) Chinese version in evaluation of mental health status of Chinese population. Chin J Clin Psychol. 2008;16(6):627–9.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Liu X, Tang M, Hu L. Reliability and validity of the Pittsburgh sleep quality index. Chinese J Psychiatry. 1996;29:103–7.
Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173.
Ma X, Xiang Y, Cai Z, Li S, Xiang Y, Guo H, Hou Y, Li Z, Li Z, Tao Y. Lifetime prevalence of suicidal ideation, suicide plans and attempts in rural and urban regions of Beijing, China. Aust NZ J Psychiat. 2009;43(2):158–66.
Ge D, Sun L, Zhou C, Qian Y, Zhang L, Medina A. Exploring the risk factors of suicidal ideation among the seniors in Shandong, China: a path analysis. J Affect Disorders. 2017;207:393–7.
Dong X, Chen R, Wong E, Simon MA. Suicidal ideation in an older US Chinese population. J Aging Health. 2014;26(7):1189–208.
Stickley A, Koyanagi A, Ueda M, Inoue Y, Waldman K, Oh H. Physical multimorbidity and suicidal behavior in the general population in the United States. J Affect Disorders. 2020;260:604–9.
Garin N, Olaya B, Moneta MV, Miret M, Lobo A, Ayuso-Mateos JL, Haro JM. Impact of multimorbidity on disability and quality of life in the Spanish older population. PLoS One. 2014;9(11):e111498.
Wei MY, Mukamal KJ. Multimorbidity and mental health-related quality of life and risk of completed suicide. J Am Geriatr Soc. 2019;67(3):511–9.
She R, Yan Z, Jiang H, Vetrano DL, Lau JT, Qiu C. Multimorbidity and health-related quality of life in old age: role of functional dependence and depressive symptoms. J Am Med Dir Assoc. 2019;20(9):1143–9.
Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disorders. 2017;221:36–46.
Romain AJ, Marleau J, Baillot A. Association between physical multimorbidity, body mass index and mental health/disorders in a representative sample of people with obesity. J Epidemiol Community Health. 2019;73(9):874–80.
Kristensen K, König H, Hajek A. The association of multimorbidity, loneliness, social exclusion and network size: findings from the population-based German ageing survey. BMC Public Health. 2019;19(1):1383.
Jindai K, Nielson CM, Vorderstrasse BA, Quiñones AR. Multimorbidity and Functional Limitations Among Adults 65 or Older, NHANES 2005–2012. Prev Chronic Dis. 2016;13:160174.
Zhao Y, Zhang L, Zhao S, Zhang L. Impact of multimorbidity on health service use and catastrophic health expenditure in China: an analysis of data from a nationwide longitudinal survey. Lancet. 2019;394:S69.
Batty GD, Kivimäki M, Bell S, Gale CR, Shipley M, Whitley E, Gunnell D. Psychosocial characteristics as potential predictors of suicide in adults: an overview of the evidence with new results from prospective cohort studies. Transl Psychiat. 2018;8(1):1–15.
Handley TE, Hiles SA, Inder KJ, Kay-Lambkin FJ, Kelly BJ, Lewin TJ, McEvoy M, Peel R, Attia JR. Predictors of suicidal ideation in older people: a decision tree analysis. Am J Geriatr Psychiatry. 2014;22(11):1325–35.
Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15(1):23.
Picco L, Achilla E, Abdin E, Chong SA, Vaingankar JA, McCrone P, Chua HC, Heng D, Magadi H, Ng LL. Economic burden of multimorbidity among older adults: impact on healthcare and societal costs. BMC Health Serv Res. 2016;16(1):173.
Kuo RN, Lai M. The influence of socio-economic status and multimorbidity patterns on healthcare costs: a six-year follow-up under a universal healthcare system. Int J Equity Health. 2013;12(1):69.
Li LW, Long Y, Essex EL, Sui Y, Gao L. Elderly Chinese and their family caregivers' perceptions of good care: a qualitative study in Shandong, China. J Gerontol Soc Work. 2012;55(7):609–25.
San Too L, Spittal MJ, Bugeja L, Reifels L, Butterworth P, Pirkis J. The association between mental disorders and suicide: a systematic review and meta-analysis of record linkage studies. J Affect Disorders. 2019;259:302–13.
Ho RC, Ho EC, Tai BC, Ng WY, Chia BH. Elderly suicide with and without a history of suicidal behavior: implications for suicide prevention and management. Arch Suicide Res. 2014;18(4):363–75.
Acknowledgments
We thank the officials of health agencies, all participants and staffs at the study sites for their cooperation.
Funding
This study was supported by the National Science Foundation of China (71774104, 71974117), the China Medical Board (16–257), Cheeloo Youth Scholar Grant, Shandong University (IFYT1810, 2012DX006) and NHC Key Laboratory of Health Economics and Policy Research (NHC-HEPR2019014). The funding organizations had no role in the design of the study and collection, analysis and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
CZ conceived, designed the study and revised and reviewed the manuscript. ZJ conducted the literature search, performed the analysis and wrote the draft manuscript. JL, PF, YW, YY, DZ, WH and CY conducted the fieldwork and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol for this study was approved by the Ethical Committee of School of Public Health, Shandong University (approval number, 20181228). All participants gave their informed written consent for participation prior to the face-to-face interview. The data used in this study was anonymized before its use.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jing, Z., Li, J., Fu, P.P. et al. Physical multimorbidity and lifetime suicidal ideation and plans among rural older adults: the mediating role of psychological distress. BMC Psychiatry 21, 78 (2021). https://doi.org/10.1186/s12888-021-03087-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-021-03087-4