Abstract
Background
The aim of this study was to examine the association between multimorbidity and (i) loneliness, (ii) social exclusion and (iii) network size, respectively.
Methods
Cross-sectional data from a German representative sample of community-dwelling adults aged 40 and over was used (N = 7604). Multimorbidity was indicated with the presence of two or more diseases. Self-rated loneliness was assessed with a short form of the validated De Jong Gierveld Loneliness Scale and social exclusion was measured with a validated scale developed by Bude and Lantermann. Counts of important people in regular contact represented the network size of respondents.
Results
Multimorbidity was present in 68% of the sample. While controlling for potential confounders, multiple linear regression analysis yielded that multimorbidity was associated with increased loneliness (b = 0.08; p < 0.001) and increased social exclusion (b = 0.10; p < 0.01). Multimorbidity was also associated with an increased network size (b = 0.27; p < 0.001).
Conclusion
While there was an association between multimorbidity and increased social exclusion as well as increased loneliness, regressions also revealed an association between multimorbidity and an increased network size. Although the association between multimorbidity and our outcome measures is weak, its complex nature should be investigated further using a longitudinal approach.
Similar content being viewed by others
Introduction
Among adults with chronic illnesses, having only a single illness condition is less common than multimorbidity [1]. Widely used, one method to describe multimorbidity is to simply count the present illness conditions within a person [2]. As proposed by van den Akker et al., multimorbidity is defined as ‘the co-occurrence of multiple chronic or acute diseases and medical conditions within one person’, resulting in a disease count of two or more diseases that defines multimorbidity [3].
As much as 50 million Europeans are estimated to live with multimorbidity [4]. For German adults the prevalence of having two or more chronic illnesses is estimated 43.9% for women and 36.3% for men, respectively. Increasing age is associated with even higher prevalence rates [5]. Hence, in the light of the ageing society in Europe, an overall increase of prevalence can be expected.
Indeed, the consequences of multimorbidity are wide-ranging. The risk of mortality in people with multimorbidity is greater compared to those people with no such condition [6]. Moreover, a dose-response relationship between multimorbidity and mortality has been demonstrated [7]. Alongside the physical consequences, multimorbidity is associated with reduced health-related quality of life at midlife in the general population [8]. Besides an individual financial hardship that is linked to having multiple diseases [9], multimorbidity is associated with a vast overall economic burden [10, 11] and is thus considered to be one of the major challenges in the future for health systems [12].
Over the last 15 years research interest in multimorbidity has rapidly grown [13]. However, little attention has been given to the relationship between multimorbidity and aspects of social relationships.
Loneliness, the social network and social exclusion are related but distinguishable concepts. Loneliness refers to the perception that the quality and quantity of one’s social network is deficient [14], and the size reflects one structural aspect of the social network which can also be characterized by its density, accessibility, and reciprocity [15]. With roots in coping theory, social exclusion is the subjective perception of being excluded from mainstream society as a whole. Among other, it is influenced by the objective precarity of one’s situation which also involves the quality and quantity of one’s social network and the individual state of health, the inherent resources, and a personal evaluation of the precarity [16].
Although previous studies have demonstrated a link between the size of a social network and loneliness, a large social network does not rule out the presence of loneliness and vice versa [15]. Likewise, one might perceive to be socially excluded because of loneliness or a limited social network but this does not always have to be the case [16].
Only a few studies have investigated the association of multimorbidity and loneliness. Stickley and Koyanagi have shown that a higher number of physical diseases is associated with elevated odds of loneliness in the general population in England [17]. Similar results were reported for populations in Israel as well as Canada and Australia [18, 19]. Another study found that the number of illnesses is significantly associated with loneliness in U.S. adults [20].
The importance of disentangling the association of multimorbidity and loneliness lies in the severe and wide-ranging consequences of both conditions. Similar to multimorbidity, loneliness has been linked to all-cause mortality [21,22,23] and has been identified as risk factor for myocardial infarction and strokes [24]. In addition, loneliness seems to worsen cardiovascular and mental health outcomes [21] and also quality of life is negatively affected by loneliness [25]. Likewise, social networks and social exclusion have been linked to health outcomes. Social exclusion is associated with poor self-rated health and depression in old age [26]. Furthermore, a longitudinal study by Cantarero-Prieto and colleagues showed that socially isolated people have a higher probability of being diagnosed with three or more chronic conditions [27]. A larger social network, a somewhat more objective measure [28], is associated with a reduced risk of subsequent mortality in older women [29]. Compared to loneliness, very little literature exists that investigates the association between multimorbidity and social exclusion or network size. It has been reported that individuals with four or more chronic illnesses are more likely to have limited social networks compared to individuals with one or less chronic conditions [30] and some studies have shown that deteriorated health is associated with social exclusion [31, 32]. Due to the serious health consequences of loneliness, social exclusion and lacking social networks it is important to identify those who are affected. By assessing potential risk factors it is possible to gain more insight on populations at risk. Studies examining the relationship of multimorbidity and loneliness, social exclusion or network size are scarce. Hence, it is the aim of this study to examine the association between multimorbidity and loneliness, social exclusion and network size in a nationally representative sample.
By including additional outcomes of social relationships, compared to solely examining loneliness, this study provides a more detailed insight to the association of multimorbidity and inter-personal outcomes.
Methods
Sample
This study used data from the German Ageing Survey (DEAS) which is a national representative longitudinal survey of community-dwelling Germans aged over 40. With a cohort sequential design the first survey wave took place in 1996 covering 4838 individuals. Subsequent waves followed in 2002, 2008, 2011 and 2014, which are referred to as second, third, fourth and fifth wave, respectively. Second, third and fifth waves included panel samples, following up on individuals who have previously been interviewed as well as newly recruited baseline samples. As an exception, the fourth wave only followed up on respondents from the previous waves and did not recruit new respondents. The response rate for the baseline sample in 2014 was 27.1%. For the first, second and third wave the retention rates for the year 2014, i.e. the valid interviews in the panel year as a proportion of valid interviews in baseline wave, were 18.3, 28.1 and 41.4%, respectively. For more information see Klaus et al. [33]. The analytical sample included individuals who responded to the fifth DEAS wave (2014). Both previously interviewed respondents (panel sample, n = 4322) and newly recruited participants (baseline sample, n = 6002) were included. The final analytical sample comprised 7604 individuals, excluding those participants with missing data for loneliness, social exclusion and/or network size.
This study has a cross-sectional study design as perceived social exclusion was only measured in the fifth survey wave (2014).
All study participants gave informed written consent. The German Centre of Gerontology in Berlin, who is responsible for DEAS, did not apply for an ethic vote because according to criteria an ethical statement was not needed.
Measures
Dependent variables
Loneliness was assessed using a modified version of the De Jong Gierveld short scales for loneliness [34]. Respondents indicate the extent to which six statements apply to their current situation. Scale scores are based on four answering options for each statement (1 = “strongly agree”, 2 = “agree”, 3 = “disagree” and 4 = “strongly disagree”) from which a mean is derived. At least half of the items have to contain valid answers. A higher score indicates a higher perceived level of loneliness. In our study, Cronbach’s alpha was .82. Overall, this instrument has been found to be a valid and reliable instrument with good psychometric characteristics [34, 35].
Perceived social exclusion was measured with a scale developed by Bude and Lantermann [16] that consists of four items with answer options ranging from 1 to 4 (1 = “strongly agree” to 4 = “strongly disagree”). The scale represents the average of the item values of at least 50% of items. A higher value reflects a stronger subjective feeling of social exclusion. In our study, Cronbach’s alpha was .88 for this scale.
Furthermore, the network size was assessed, defined as the number of important people who are in regular contact with the respondent, ranging from 0 to 9. The wording of the question was as follows: “We now want to look at people who are important to you and who you maintain regular contact with. These can include co-workers, neighbours, friends, acquaintances, relatives, and members of your household. Which people are important to you? If there are several, please just name the eight most important. Please give me these people’s first names and the first letters of their last names.” In order to avoid a high questionnaire load, this question only referred to eight persons, as additional information was collected for each nominated network member. Respondents could name their actual network size in an additional question, however any network size > 8 was coded as 9.
Independent variable of interest: multimorbidity
Respondents were asked to name which out 13 illnesses they were currently having at the time of assessment. The self-report question included following illnesses: cardiac and circulatory disorders; bad circulation; joint, bone, spinal or back problems; respiratory problems, asthma, or shortness of breath; stomach and intestinal problems; cancer; diabetes; gall bladder, liver or kidney problems; bladder problems; eye problems or vision impairment; ear problems or hearing problems; and other illnesses or health problems. As multimorbidity was not assessed directly through an index or scale, disease counts were used. Disease counts weight all conditions equally and do not take the duration into account. However, it has been shown that simple disease counts perform comparably well as more complex measures [36, 37]. Multimorbidity was defined as “the co-occurrence of multiple diseases and medical conditions within one person” [3] and was hence indicated by the presence of ≥2 illnesses.
Covariates
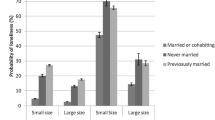
Based on findings of former research on determinants of multimorbidity and loneliness, a number of covariates was controlled for. Sociodemographic control variables included age [38, 39], gender [38, 40], monthly net equivalence income [38, 41, 42] and marital status (married, living together with spouse; married, living separated from spouse; divorced; widowed; single) [43]. Moreover, previous research has shown associations between multimorbidity and depression [44] as well as loneliness and depression or depressive symptoms [39, 40, 45]. To measure depressive symptoms the German 15 item version of the Center for Epidemiological Studies Depression Scale (CES-D) was administered. On a scale from 0 to 45, higher scores indicate higher depressive symptoms [46]. Cronbach’s alpha for the CES-D was .86 in this sample.
Furthermore, a list of potentially confounding lifestyle factors was included. Smoking, categorized as daily, occasional, former and never smokers [40, 42, 47], alcohol consumption (daily; several times a week; once a week; 1–3 times per month; less often (than 1–3 times per month); never) [48, 49], physical activity (daily; several times a week; once a week; 1–3 times per month; less often (than 1–3 times per month); never) [47, 50] as well as the body mass index (BMI) as an indicator of obesity (dichotomized into BMI ≤ 30 and BMI > 30) [42, 47] were included as control variables.
Statistical analysis
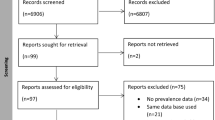
Missing data in the final analytical sample was checked for all variables used. The percentage of missing data in all variables varied between 0 and 5.4%. Initially, sample characteristics were analysed using descriptive statistics stratified by the presence and absence of multimorbidity, indicated by < 2 and ≥ 2 illnesses. Chi2- or t-tests were applied according to the level of measurement. The same procedure was repeated for loneliness, social exclusion and network size that were dichotomized with a median split.
Model assumptions for linear regression models were checked beforehand for each model. The variance inflation factor was < 3 for all independent variables (including the additional sensitivity analysis covariate), indicating no problem with multicollinearity. Multivariate normality was checked with normal probability plots of the residuals and yielded approximate normal distributions. The White’s test statistic for homoscedasticity yielded significant values (for loneliness =373.32 p < 0.001; for social exclusion =291.47 p < 0.001; and for network size =145.64 p < 0.01). As a result, the null hypothesis of homoscedasticity had to be rejected. Hence, robust standard errors were used in the regression models. Univariate regression coefficients were calculated for each of the three dependent variables and each independent variable used in the multivariate analysis. Then, three separate multiple linear regression models estimated the relationship between multimorbidity and the dependent variables while controlling for the covariates named above. Categorical variables were dummy coded in the regression analysis. Survey weights were not applied in the analysis as it has previously been pointed out that survey weights can influence estimates negatively in their efficiency [51]. In sensitivity analyses, the threshold was altered to three or more illnesses to see whether this could change the results. To further check the robustness of our results, functional limitation measured with the SF-36 functional limitation subscale [52] (ranging from 0 = worst to 100 = best) was an additional covariate in sensitivity analysis. Moreover, interaction effects of the educational level expressed by the International Standard Classification of Education (ISCED; 1 = low, 2 = middle, 3 = high) and gender with multimorbidity were explored. To our knowledge, no studies have investigated possible interaction effects in the association of multimorbidity and social relations to date.
Results
Sample characteristics
In total, 7604 participants reported on their loneliness, social exclusion and network size. For these participants, the mean age was 64.37 (SD 11.22) and the overall proportion of females was 50.92%. The mean loneliness score for the total sample was 1.77 (SD 0.54), the mean social network size was 5.23 (SD 2.70), and the mean social exclusion score was 2.60 (SD 0.59). Sample characteristics, stratified by presence of multimorbidity, are shown in Table 1. 68% of the sample (N = 5140) reported to have two or more physical illnesses whereas the remaining 32% (N = 2464) reported to have one or none of the listed illnesses. Respondents with two or more illnesses differed significantly from respondents with one or less in all characteristics except number of important contacts in regular contact. Results of the sample characteristics stratified by loneliness, social exclusion and network size, respectively, can be seen in Table 4 in Appendix.
Regression analysis
The crude regression coefficients for multimorbidity were b = 0.14 (p < 0.001) for loneliness, b = 0.19 (p < 0.001) for social exclusion, and b = − 0.08 (p = 0.232) for network size, respectively. Table 2 shows the results of the univariate regression analysis, while Table 3 reports the multiple regression analysis results for loneliness, social exclusion and number of important people in regular contact, while controlling for potential confounders. The explained variance in loneliness and social exclusion was R2 = 0.16 and R2 = 0.15 for the main model. For the number of important people in regular contact, the explained variance for the main model was R2 = 0.07.
While controlling for the potential confounders multimorbidity was associated with increased loneliness (b = 0.08; p < 0.001), increased social exclusion (b = 0.09; p < 0.001) but also with increased numbers of important people in regular contact (b = 0.27; p < 0.001). Apart from multimorbidity, only depressive symptoms, gender, marital status and monthly net equivalent income in Euro were significantly associated with all three variables.
In further analyses, the threshold for multimorbidity was altered and set at three or more physical illnesses, resulting in similar regression coefficients of b = 0.08 (p < 0.001) for loneliness, b = 0.11 (p < 0.001) for social exclusion and b = 0.18 (p < 0.01) for number of important people in regular contact. The inclusion of functional limitation as additional covariate did not change the association between multimorbidity and the three outcomes considerably. To investigate whether interaction effects of gender and education with multimorbidity were present, the interaction terms were included in the regression analyses. However, no interaction effect for neither of the two variables was observed.
Discussion
Main findings
This study examined the association between multimorbidity and loneliness, social exclusion and network size in a representative sample of Germans aged 40+. Even though the effect sizes are small, our results indicate that multimorbidity is associated with increased loneliness and social exclusion scores. Conversely, the positive association between multimorbidity and the number of important people in contact suggests that multimorbidity is associated with a larger network size.
Relation to previous research
Our results are in line with findings from previous research indicating an association between multimorbidity and loneliness. A conceptual model of loneliness might assist in explaining our findings in this study, namely why individuals with multimorbidity feel lonelier. It is assumed that distal social structure factors through more proximal factors, including health, can explain individual differences in loneliness and social exclusion by affecting relationship characteristics such as quantity and quality. Particularly relationship quality is mentioned as key determinant of loneliness which, however, can be altered by other factors such as poor health [53]. Another possible explanation could be offered by the possible impact of functional limitation. It is conceivable that an individual who suffers from several medical conditions might experience limited functionality that could have an influence on the quality of social relations. However, in additional analysis, it was adjusted for functional limitation with the SF-36 functional limitation subscale and virtually no difference in the association between multimorbidity and loneliness as well as social exclusion was seen.
A British study on health and social exclusion supports the results of our study [31]. It was found that poor self-rated health and limiting long-term illnesses predicted subsequent social exclusion. The Precarity-Resource-Model of Exclusion might offer an explanation for these results [16]. The model assumes that the objective precarity, resulting from individual poverty, social network characteristics, and poor health among others, influences the social exclusion through the individual evaluation of the current situation and a subjective appraisal of future developments. Illnesses represented in the disease count in this study were largely of chronic nature (e.g. cardiac problems, diabetes, joint, bone, spinal or back problems). The limited prospect of recovery in combination with old age might lead to a negative appraisal of future developments and thereby contribute to the subjective feeling of social exclusion. A somewhat counterintuitive result in our study, and in contrast to results from Tisminetzky et al. [30], is that multimorbidity is associated with an increased network size when controlling for potential confounders. A possible explanation could be offered by a qualitative study, in which patients with multimorbidity described their social network. Most networks described were diverse and rich. A range of family, friends, community organisations, service providers and health professionals were reported by patients. This highlights the different scope of people supporting patients with multimorbidity [54]. It could be possible that multimorbidity, through an increased need for support, could enlarge the social network reported by people with multimorbidity. Yet, when we controlled for functional limitation, measured with the SF-36 functional limitation subscale, we found that the inclusion of the covariate did not change the association between multimorbidity and network size.
In comparison to existing studies, we were able to extend the perspective on loneliness to the related constructs of social exclusion and network size. To our knowledge, no other studies exist which examined the association between multimorbidity and these constructs.
It is worth noting that the opposite direction, in which loneliness, social exclusion and network size predict multimorbidity, has also been investigated previously and significant associations have been found [27, 55]. In a cross-sectional study Jessen et al. [56] found that people who are exposed to loneliness have increased odds for multimorbidity. In light of this research, a bi-directional relationship seems plausible. This should be investigated in further longitudinal research.
Strength and limitations
One of the major strengths of this study are the outcome measures used. We used established loneliness and social exclusion scales with good psychometric properties. Furthermore, we included a somewhat more objective measure of loneliness which was the network size.
By using data from the DEAS study our results are representative for the German population 40+. Analyses of the cohorts in the DEAS study reveal that selectivity effects are only minor and that central socio-demographic characteristics are very similar to official statistics of the German population [33, 57]. In addition, this study supports previous findings and provides further insight to this rarely investigated field of research.
However, our study results are tied to some limitations. The response rate of the DEAS study was relatively low in 2014 but comparable in magnitude with other German surveys [33]. The cross-sectional nature of our study is a limitation as no conclusions can be drawn towards the temporality of the relationship. In addition, we cannot rule out that other, unmeasured covariates, e.g. coping strategies, have influenced the relationships assessed. Also, we were not able to include the duration of illnesses which could have provided more detailed insight of the relationship. Lastly, the list of diseases that we based the disease count on to indicate multimorbidity, differed somewhat from lists used in other studies. This hampers the comparability of our results.
Conclusion
While there was an association between multimorbidity and increased social exclusion as well as increased loneliness, regressions also revealed an association between multimorbidity and an increased network size. In conclusion, the association between multimorbidity and our outcome measures is complex. Although small effect sizes were observed in our study, results may be helpful for the identification of lonely or socially excluded people.
Analysing different disease patterns could provide further valuable insight for preventive measures. Some literature suggests, that different disease patterns lead to different consequences in loneliness. A study by Penninx et al. found that greater feelings of loneliness were mainly seen in persons with lung disease or arthritis [58]. Even between different types of rheumatic diseases, different intensities of loneliness have been reported [59]. It would be of great interest to further analyse different disease patterns and their effects on loneliness in future studies. In addition, longitudinal research is needed to disentangle the association between multimorbidity and aspects of social relationships.
Availability of data and materials
The data used in this study are third-party data. The anonymized data sets of the DEAS (1996, 2002, 2008, 2011, and 2014) are available for secondary analysis. The data has been made available to scientists at universities and research institutes exclusively for scientific purposes. The use of data is subject to written data protection agreements. Microdata of the DEAS is available free of charge to scientific researchers for non-profitable purposes. The FDZ-DZA provides access and support to scholars interested in using DEAS for their research. However, for reasons of data protection, signing a data distribution contract is required before data can be obtained. Please see for further Information (data distribution contract): https://www.dza.de/en/fdz/access-to-data/formular-deas-en-english.html
Abbreviations
- BMI:
-
Body Mass Index
- CES-D:
-
Center for Epidemiological Studies Depression Scale
- DEAS:
-
German Ageing Survey (Deutscher Alterssurvey)
- ISCED:
-
International Standard Classification of Education
References
Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. Journal of the American Board of Family Medicine : JABFM. 2013;26(5):518–24.
Lefèvre T, d’Ivernois JF, De Andrade V, Crozet C, Lombrail P, Gagnayre R. What do we mean by multimorbidity? An analysis of the literature on multimorbidity measures, associated factors, and impact on health services organization. Rev Epidemiol Sante Publique. 2014;62(5):305–14.
van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. Eur J Gen Pract. 1996;2(2):65–70.
Rijken M, Struckmann V, Dyakova M, Melchiorre MG, Rissanen S, van Ginneken E. Improving care for people with multiple chronic conditions in Europe. Eurohealth. 2013;19(3):29–31.
Fuchs J, Busch M, Lange C, Scheidt-Nave C. Prevalence and patterns of morbidity among adults in Germany. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2012;55(4):576–86.
Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–8.
Wei MY, Mukamal KJ. Multimorbidity, mortality, and long-term physical functioning in 3 prospective cohorts of community-dwelling adults. Am J Epidemiol. 2018;187(1):103–12.
Kanesarajah J, Waller M, Whitty JA, Mishra GD. Multimorbidity and quality of life at mid-life: a systematic review of general population studies. Maturitas. 2018;109:53–62.
Temple JB, Williams R. Financial well-being of older Australians with multiple health conditions. Australas J Ageing. 2018.
Wang L, Si L, Cocker F, Palmer AJ, Sanderson K. A systematic review of cost-of-illness studies of multimorbidity. Applied Health Economics and Health Policy. 2018;16(1):15–29.
Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, Riedel-Heller S, König H-H. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420.
Rijken M, Struckmann V, van der Heide I, Hujala A, Barbabella F, van Ginneken E, Schellevis F. How to improve care for people with multimorbidity in Europe? In: Policy Brief. Edited by Richardson E, vol. 23. European Observatory on Health Systems and Policies: Copenhagen, Denmark; 2016.
McPhail SM. Multimorbidity in chronic disease: impact on health care resources and costs. Risk Manag Healthc Policy. 2016;9:143–56.
de Jong GJ, van Tilburg T, Dykstra PA. In: Perlman D, Vangeslisti A, editors. Loneliness and social isolation. In: The Cambridge handbook of personal relationships. Cambridge, UK, Cambridge University Press; 2006. p. 485–500.
Victor C, Scambler S, Bond J, Bowling A. Being alone in later life: loneliness, social isolation and living alone. Rev Clin Gerontol. 2000;10(4):407–17.
Bude H, Lantermann E-D. Soziale exklusion und exklusionsempfinden. KZfSS Kölner Zeitschrift für Soziologie und Sozialpsychologie. 2006;58(2):233–52.
Stickley A, Koyanagi A. Physical multimorbidity and loneliness: a population-based study. PLoS One. 2018;13(1):e0191651.
Wister A, Kendig H, Mitchell B, Fyffe I, Loh V. Multimorbidity, health and aging in Canada and Australia: a tale of two countries. BMC Geriatr. 2016;16:163.
Cohen-Mansfield J, Shmotkin D, Goldberg S. Loneliness in old age: longitudinal changes and their determinants in an Israeli sample. Int Psychogeriatr. 2009;21(6):1160–70.
Theeke LA. Predictors of loneliness in U.S. adults over age sixty-five. Arch Psychiatr Nurs. 2009;23(5):387–96.
Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–71.
Laugesen K, Baggesen LM, Schmidt SAJ, Glymour MM, Lasgaard M, Milstein A, Sørensen HT, Adler NE, Ehrenstein V. Social isolation and all-cause mortality: a population-based cohort study in Denmark. Sci Rep. 2018;8:4731.
Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–14.
Hakulinen C, Pulkki-Raback L, Virtanen M, Jokela M, Kivimaki M, Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart (British Cardiac Society). 2018;104(18):1536-1542.
Musich S, Wang SS, Hawkins K, Yeh CS. The impact of loneliness on quality of life and patient satisfaction among older, Sicker Adults. Gerontol Geriatr Med. 2015;1:2333721415582119.
Feng Z, Jones K, Phillips DR. Social exclusion, self-rated health and depression among older people in China: evidence from a national survey of older persons. Arch Gerontol Geriatr. 2019;82:238–44.
Cantarero-Prieto D, Pascual-Sáez M, Blázquez-Fernández C. Social isolation and multiple chronic diseases after age 50: a European macro-regional analysis. PLoS One. 2018;13(10):e0205062.
Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and social relationships: what are we measuring? A novel framework for classifying and comparing tools. BMJ Open. 2016;6(4):e010799.
Rutledge T, Matthews K, Lui LY, Stone KL, Cauley JA. Social networks and marital status predict mortality in older women: prospective evidence from the study of osteoporotic fractures (SOF). Psychosom Med. 2003;65(4):688–94.
Tisminetzky M, Gurwitz J, McManus DD, Saczynski JS, Erskine N, Waring ME, Anatchkova M, Awad H, Parish DC, Lessard D, et al. Multiple chronic conditions and psychosocial limitations in patients hospitalized with an acute coronary syndrome. Am J Med. 2016;129(6):608–14.
Sacker A, Ross A, MacLeod CA, Netuveli G, Windle G. Health and social exclusion in older age: evidence from understanding society, the UK household longitudinal study. J Epidemiol Community Health. 2017;71(7):681–90.
Finlay JM, Kobayashi LC. Social isolation and loneliness in later life: a parallel convergent mixed-methods case study of older adults and their residential contexts in the Minneapolis metropolitan area, USA. Soc Sci Med. 2018;208:25–33.
Klaus D, Engstler H, Mahne K, Wolff JK, Simonson J, Wurm S, Tesch-Römer C. Cohort Profile: The German Ageing Survey (DEAS). Int J Epidemiol. 2017;46(4):1105–1105g.
de Jong GJ, van Tilburg T. A 6-item scale for overall, emotional, and social loneliness:confirmatory tests on survey data. Res Aging. 2006;28(5):582–98.
de Jong GJ, van Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing. 2010;7(2):121–30.
Di Bari M, Virgillo A, Matteuzzi D, Inzitari M, Mazzaglia G, Pozzi C, Geppetti P, Masotti G, Marchionni N, Pini R. Predictive validity of measures of comorbidity in older community dwellers: the Insufficienza Cardiaca negli Anziani Residenti a Dicomano study. J Am Geriatr Soc. 2006;54(2):210–6.
Perkins AJ, Kroenke K, Unutzer J, Katon W, Williams JW Jr, Hope C, Callahan CM. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57(10):1040–8.
Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, Glynn L, Muth C, Valderas JM. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9(7):e102149.
Dahlberg L, Andersson L, McKee KJ, Lennartsson C. Predictors of loneliness among older women and men in Sweden: a national longitudinal study. Aging Ment Health. 2015;19(5):409–17.
Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, Wiltink J, Wild PS, Münzel T, Lackner KJ, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17:97.
Pathirana TI, Jackson CA: Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health 2018:n/a-n/a.
Katikireddi SV, Skivington K, Leyland AH, Hunt K, Mercer SW. The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: a longitudinal analysis of the Twenty-07 cohort. BMC Med. 2017;15:152.
Ausín B, Muñoz M, Castellanos MA. Loneliness, Sociodemographic and mental health variables in Spanish adults over 65 years old. The Spanish Journal of Psychology. 2017;20:E46.
Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord. 2017;221:36–46.
Ge L, Yap CW, Ong R, Heng BH. Social isolation, loneliness and their relationships with depressive symptoms: a population-based study. PLoS One. 2017;12(8):e0182145.
Hautzinger M, Bailer M. Allgemeine Depressions-Skala. Beltz: Weinheim; 1993.
Jackson CA, Dobson AJ, Tooth LR, Mishra GD. Lifestyle and socioeconomic determinants of multimorbidity patterns among mid-aged women: a longitudinal study. PLoS One. 2016;11(6):e0156804.
Sakib MN, Shooshtari S, St John P, Menec V. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: an analysis of Canadian longitudinal study on aging data. BMC Public Health. 2019;19(1):243.
Shiovitz-Ezra S, Litwin H. Social network type and health-related behaviors: evidence from an American national survey. Social science & medicine (1982). 2012;75(5):901–4.
Dhalwani NN, Zaccardi F, O’Donovan G, Carter P, Hamer M, Yates T, Davies M, Khunti K. Association between lifestyle factors and the incidence of multimorbidity in an older English population. The Journals of Gerontology: Series A. 2017;72(4):528–34.
Solon G, Haider SJ, Wooldridge JM. What are we weighting for? J Hum Resour. 2015;50(2):301–16.
Bullinger M. German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA project. International quality of life assessment. Soc Sci Med. 1995;41(10):1359–66.
Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. J Gerontol Ser B Psychol Sci Soc Sci. 2008;63(6):S375–84.
McKinlay E, McDonald J, Darlow B, Perry M. Social networks of patients with multimorbidity: a qualitative study of patients' and supporters' views. Journal of primary health care. 2017;9(2):153–61.
Smith KJ, Victor C. Typologies of loneliness, living alone and social isolation, and their associations with physical and mental health. Ageing Soc. 2018:1–22.
Jessen MAB, Pallesen AVJ, Kriegbaum M, Kristiansen M. The association between loneliness and health - a survey-based study among middle-aged and older adults in Denmark. Aging Ment Health. 2017:1–6.
Klaus D, Engstler H: Daten und Methoden des Deutschen Alterssurveys. In: Altern im Wandel: Zwei Jahrzehnte Deutscher Alterssurvey (DEAS). edn. Edited by Mahne K, Wolff JK, Simonson J, Tesch-Römer C. Wiesbaden: Springer Fachmedien Wiesbaden; 2017: 29–45.
Penninx BWJH, van Tilburg T, Kriegsman DMW, Boeke AJP, Deeg DJH, van Eijk JTM. Social network, social support, and loneliness in older persons with different chronic diseases. Journal of Aging and Health. 1999;11(2):151–68.
Kool MB, Geenen R. Loneliness in patients with rheumatic diseases: the significance of invalidation and lack of social support. The Journal of Psychology. 2012;146(1–2):229–41.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
KK, HHK, AH: Design and concept of analyses, preparation of data, statistical analysis and interpretation of data, preparing of the manuscript. All authors critically reviewed the manuscript, provided significant editing of the article and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An ethical statement for the DEAS study was not necessary because criteria for the need of an ethical statement were not met (risk for the respondents, lack of information about the aims of the study, examination of patients). This is in accordance with the German Research Foundation-guidelines (Deutsche Forschungsgemeinschaft, DFG) available at: http://dfg.de/foerderung/faq/geistes_sozialwissenschaften/ (only available in German language). The German Centre of Gerontology, who is responsible for the DEAS study did not apply for an ethics vote, based on the recommendation of a standing council of the DEAS that decided no ethics vote to be necessary.
Prior to the interview, written informed consent was given by all participants of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kristensen, K., König, HH. & Hajek, A. The association of multimorbidity, loneliness, social exclusion and network size: findings from the population-based German Ageing Survey. BMC Public Health 19, 1383 (2019). https://doi.org/10.1186/s12889-019-7741-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-7741-x