Abstract
Background
To improve knowledge on endoscopic retrograde cholangiopancreatography (ERCP) in children, we aimed to study the proportion of indications, success rate and complication of ERCP.
Methods
We performed a systematic search of all articles published up to December 2022 in the following databases: Cochrane Library, PubMed (MEDLINE) and Scopus. The meta-analysis was performed using a random-effects model. Heterogeneity was determined by the I2 statistics and the Cochrane Q test. The included data were analyzed to identify the proportion of indications, success rate and complications of ERCP in children.
Results
Based on data from 52 studies with a total of 5624 participants, the most common indications for ERCP in children were biliary [48% (95% CI: 0.40 - 0.57; I2 = 98.17%, P < 0.001)] and both biliary and pancreatic [41% (95% CI: 0.33 - 0.49; I2 = 98.27%, P < 0.001)]. The success rate of ERCP was 95% (95% CI: 0.94 - 0.96; I2 = 82.53%, P < 0.001) with the overall complication rate of 7% (95% CI: 0.05 - 0.09; I2 = 82.06%, P < 0.001). The pooled estimate for the incidence of post ERCP pancreatitis was 4% (95% CI: 0.03 - 0.06; I2 = 85.46%, P < 0.001) and the bleeding was 0% (95% CI: 0.0 - 0.0; I2 = 28.21%, P = 0.03).
Conclusions
ERCP appears to be performed safely in children with a similar success rate as in the adult population.
Similar content being viewed by others
Introduction
Advanced endoscopy, traditionally associated with endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS), continues to evolve as new technology and techniques become available [1, 2]. Advanced endoscopists now have a variety of capabilities, including ERCP, balloon enteroscopy, Capsule Endoscopy, EUS and transabdominal ultrasonography (TUS) and deep small bowel enteroscopy [3]. Pediatric indications differ from adults for ERCP while it is comparable in adolescents such as choledocholithiasis, liver-transplantation related disorders, and malignancy. In contrast, the main indication for ERCP in newborns was diagnostic workup of neonatal cholestasis and suspected pancreaticobiliary maljunction [4, 5]. Considering the rise in the incidence of ERCP in children, an increased risk of complications was also reported in this sub-population [6]. A few authors have expressed their opinion that ERCP could be successfully carried out in children with a similar success rate as observed in adults provided, they are performed by an experienced endoscopist in children, but the evidence is inadequate [7,8,9]. Considering the dearth of data, a systematic in-depth review and analysis of published literature is essential. We focus the discussion on advanced endoscopic methods that have already been developed and are more widely accepted in practice, but it is worth noting that there is an explosion of new endoscopic methods that continue to expand the frontiers of endoscopic treatment.
Method
Search strategy
The study protocol was developed complying the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) checklist. An independent systematic search was implemented in the Cochrane Library, PubMed (MEDLINE), Scopus and Web of Science until April 2023 by two authors (M.H.S. and S.F). The combination of following keywords and Medical Subject Heading (MeSH) terms were used in the search strategies: [“Cholangiopancreatography, Endoscopic Retrograde” OR Endoscopic Retrograde Cholangiopancreatography OR ERCP] AND [indication OR outcome OR outcomes OR success rate OR efficacy OR patient safety OR complications OR] AND [Child OR Adolescent OR Pediatrics OR Pediatric* OR youth* OR teen* OR infant]. We also hand searched the bibliographies of retrieved reviews to find potentially relevant original articles. No language or time limits were imposed in the literature search.
Eligibility criteria
After the elimination of duplicate records, titles and abstracts of identified papers were screened and studies meeting the following criteria were included: (1) the articles were case series, prospective/retrospective cohort studies, case-control studies, or randomized) (2) the studies enrolled pediatric/children/adolescents (aged < 18 years); and (3) the articles reported indication, success rate or complication of ERCP. Duplicate data, studies with unclear information, studies involving animals, reviews and studies whose corresponding author did not offer any feedback after several emails were excluded.
Data extraction
A detailed full-text review was independently performed by two authors (E.Sh. and AH.H.) and the following data were abstracted using standardized pre-piloted forms: reference (first author's name and year of publication), study location, sample size, type of study, participants' characteristics (gender, age), indication, success rate and complication of procedure.
Data synthesis
The statistical analysis was conducted using STATA version 11.0 (Stata Corp, College Station, TX, USA). The pooled estimates for the indications, success rate and complications of ERCP were expressed as proportions with 95% confidence intervals (95% CI) using the random effects model, and presented visually as the Forest plot [10]. Heterogeneity was examined using the I-squared (I2) statistic and the Cochrane Q test in which the heterogeneity was considered significant if the I2 value was ≥ 50%. The significance level for heterogeneity was defined with a significance level of P ≤ 0.10 for Cochran Q. We assessed the presence of publication bias using the Funnel plot and the Egger’s test [11].
Results
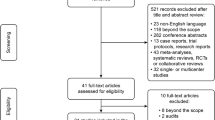
Study selection
Figure 1 displays the flow diagram of the study selection process. A total of 5257 articles were identified from the screening process. After the removal of duplicate records, 4467 articles remained and finally 176 articles were retained for full-text review of which 52 articles [5, 7, 9, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60] were included in this study.
Study characteristics
The key characteristics of the included studies are summarized in Table 1. All except two [46, 50] had retrospective study design. In general, the included studies were published between 1993 and 2022, and were conducted in the United States of America [14, 18, 20, 21, 23,24,25, 29, 30, 33, 36, 40, 42, 44, 45, 48,49,50,51, 53, 57], China [17, 28, 34, 54, 56, 58,59,60], India [12, 16, 37], Netherlands [52], Germany, [5, 22, 32] Pakistan [46], Turkey [19, 55], Czech Republic [27], Italy [9, 35, 41], Canada [7, 38], Japan [43, 47], Korea [15], Bangladesh [39], Bulgaria [13], France [31], and Saudi Arabia [26]. The number of patients enrolled in each study ranged from 5 to 857 and the mean age (year) range of studies' participants varied between 53 days to 16.2 years. Eight studies [9, 12, 25, 28, 35, 40, 54, 59]reported exclusively on pancreatic ERCPs and three studies [27, 32, 57] on biliary ERCPs.
Meta-analysis
Based on the data from 52 studies with a total of 5624 participants, the most common indications for ERCP in pediatric were biliary [48% (95% CI: 0.40 - 0.57; I2 = 98.17%, P < 0.001)] in 3653 patients (Fig. 2) and both biliary and pancreatic [41% (95% CI: 0.33 - 0.49; I2 = 98.27%, P < 0.001)] in 2018 patients (Fig. 3). The success rate of the procedure as 95% (95% CI: 0.94 - 0.96; I2 = 82.53%, P < 0.001) (Fig. 4) with the overall complication rate of 7% (95% CI: 0.05 - 0.09; I2 = 82.06%, P < 0.001) (Fig. 5). To clarify the details of most common complication of ERCP and the source of heterogeneity, we carried out a subgroup analysis based on the Post ERCP pancreatitis and bleeding. Complication of ERCP (pancreatitis and biliary) was observed as a possible source of heterogeneity on the overall effect size. Post ERCP pancreatitis was reported 4% (95% CI: 0.03 - 0.06; I2 = 85.46%, P < 0.001) in 350 and bleeding was 0% (95% CI: 0.0 - 0.0; I2 = 28.21%, P = 0.03) as observed only in 40 patients out of the total 5900 (Fig. 6). Considering the significant heterogeneity to identify the source, further subgroup analyses were performed by age group and the ERCP center. On the basis of subgroup analyses, none of the variables examined represented a source of heterogeneity, but the subgroup analysis showed the overall complication of ERCP was greater 10% [95% CI: 0.06 - 0.14] in children between age 2-10 years compared with the other age groups [ for < 2 years: 8% (95% CI: 0.02 - 0.19) and for > 10 years: 6% (95% CI: 0.05 - 0.09)]. These results were similar for success rate, in that the success rate for the children between age 2-10 years was %97 (95% CI: 0.93 - 1.0) and was higher compared to other age groups [for < 2 years: 0.93 (95% CI: 0.89 - 0.96) and for > 10 years: %95 (95% CI: 0.92 - 0.96)].
Publication bias
The evaluation of publication bias by visual inspection of the funnel plot and Egger’s test demonstrated some evidence for publication bias in the meta-analysis of biliary indication of ERCP (P = 0.040). However, the results of the meta trim and fill analysis did not reveal any presence of additional studies other than those included in this meta-analysis. Egger’s linear regression test for elevated pancreatic indication (P = 0.284), success rate (P = 0.355), and complication rate (P = 0.500) did not reveal presence of any publication bias (Fig. 7).
Discussion
The present meta-analysis was carried out for evaluating the indications, success rate, and complications of ERCP in children. We observed through a total of 5624 participants in 52 studies, the most common indications were biliary and almost 95% of the procedure was successful with a very satisfactory rate of overall complication (7%). Our results are very assuring considering the fact that ERCP provides an opportunity for visualization of the biliary tract in infants and can replace the non-invasive imaging by magnetic resonance cholangiopancreatography (MRCP) [61]. Our study had a much higher success rate compared to the results carried out in adults where the pooled estimates for single-balloon enteroscopy (SBE-) assisted ERCP in biliary interventions revealed with a success rate of 75.8% [62]. Similarly, results from Sun et al. [63], revealed a success rate of 74% and the incidence of side effects as 8% compared to the present study where the success rate and complication rate of 95% and 7%, respectively. Additionally, the previous study was also limited in not revealing the indications for ERCP, unlike the present study, instead, there were interesting results regarding stent placement as the most common method (75%) and the usage proportion of sphincterotomy (ST), stone extraction/removal and bougienage/balloon dilation. Usatin et al [64] evaluated the same outcome measures in a meta-analysis of 32 studies (2612 study participants) where biliary indications contributed to 54% of the cases with an overall complication rate of 6%. The authors have also observed a similar rate of pancreatitis (3%) and bleeding (0.6%) as shown in the present study. Although some studies have observed injection of contrast medium in the pancreatic duct and pancreatic sphincterotomy as the risk factors for post-ERCP pancreatitis [8], we could not evaluate it in the present study owing to data constraints. Additionally, none of the studies have evaluated mortality following ERCP despite 0.11% observed in the adult population [6]. Although the overall complication rates following ERCP were low, it is still significant particularly in terms of the morbidity due to post-ERCP pancreatitis. Due to the limited number of pediatric cases requiring ERCP, in many centers, ERCP is carried out by adult gastroenterologists with a reasonable success rate and low complication rates [24]. It is still debatable whether a pediatric gastroenterologist should only perform the ERCP in children or a trained adult gastroenterologist in the pediatric procedures can be involved in doing so particularly with the limited data in the literature. Post-ERCP pancreatitis has been observed to be 4% in the present study like the rates observed in adult populations [65, 66]. We could not evaluate the complication rate in infants separately although a recent unpublished report in this sub-population revealed a higher incidence (13%) compared to older children [67].
The present meta-analysis has included the maximum number of studies and patients to date. However, the study does have certain limitations. Firstly, there is a varied length of follow-up among participants in the studies, which may lead to the observation of additional complications not documented in long-term follow-up. Additionally, the rate of observed complications may also differ between studies.
Secondly, differences in resources among hospital set-ups may result in variations in the experiences of gastroenterologists who performed ERCP between studies. This could potentially impact the outcomes and conclusions drawn from the analysis. Furthermore, there is a limited number of published studies involving younger children and infants, making it unclear if success rates and complications differ in this age group compared to older children. This lack of data raises questions about generalizability and applicability to pediatric populations. Lastly, none of the included studies have mentioned mortality following ERCP, either immediately after the procedure or due to long-term complications. This information is crucial for a comprehensive understanding of the risks associated with ERCP. Overall, while this meta-analysis provides valuable insights into ERCP outcomes based on existing literature, these limitations should be taken into consideration when interpreting the results and applying them to clinical practice.
Conclusion
ERCP appears to be performed safely in children with similar success rates as in the adult population.
Availability of data and materials
Data is available upon request from the corresponding author for the article due to privacy / ethical restrictions.
References
Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, et al. Quality indicators for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc. 2006;63(4):S29–34.
Yousaf MN, Chaudhary FS, Ehsan A, Suarez AL, Muniraj T, Jamidar P, et al. Endoscopic ultrasound (EUS) and the management of pancreatic cancer. BMJ Open Gastroenterol. 2020;7(1):e000408.
Ishigami S, Yoshinaka H, Sakamoto F, Natsugoe S, Tokuda K, Nakajo A, et al. Preoperative assessment of the depth of early gastric cancer invasion by transabdominal ultrasound sonography (TUS): a comparison with endoscopic ultrasound sonography (EUS). Hepato-gastroenterol. 2004;51(58):1202–5.
Pogorelić Z, Lovrić M, Jukić M, Perko Z. The laparoscopic cholecystectomy and common bile Duct Exploration: a single-step treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children. 2022;9(10):1583.
Felux J, Sturm E, Busch A, Zerabruck E, Graepler F, Stüker D, et al. ERCP in infants, children and adolescents is feasible and safe: results from a tertiary care center. United Eur Gastroenterol J. 2017;5(7):1024–9.
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Off J Am Coll Gastroenterol. 2007;102(8):1781–8.
Paris C, Bejjani J, Beaunoyer M, Ouimet A. Endoscopic retrograde cholangiopancreatography is useful and safe in children. J Pediatr Surg. 2010;45(5):938–42.
Troendle DM, Abraham O, Huang R, Barth BA. Factors associated with post-ERCP pancreatitis and the effect of pancreatic duct stenting in a pediatric population. Gastrointest Endosc. 2015;81(6):1408–16.
Kohoutova D, Tringali A, Papparella G, Perri V, Boškoski I, Hamanaka J, et al. Endoscopic treatment of chronic pancreatitis in pediatric population: Long-term efficacy and safety. United Eur Gastroenterol J. 2019;7(2):270–7.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:1–10.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Agarwal J, Reddy DN, Talukdar R, Lakhtakia S, Ramchandani M, Tandan M, et al. ERCP in the management of pancreatic diseases in children. Gastrointest Endosc. 2014;79(2):271–8.
Asenov Y, Akın M, Cantez S, Soysal FG, Tekant Y. Endoscopic retrograde cholangiopancreatography in children: Retrospective series with a long-term follow-up and literature review. Turk J Gastroenterol. 2019;30(2):192–7.
Brown CW, Werlin SL, Geenen JE, Schmalz M. The diagnostic and therapeutic role of endoscopic retrograde cholangiopancreatography in children. J Pediatr Gastroenterol Nutr. 1993;17(1):19–23.
Cho JM, Jeong IS, Kim HJ, Oh SH, Kim KM. Early adverse events and long-term outcomes of endoscopic sphincterotomy in a pediatric population: a single-center experience. Endoscopy. 2017;49(05):438–46.
Dahale AS, Puri AS, Sachdeva S, Srivastava S, Kumar A. Endoscopic retrograde cholangiopancreaticography in children: a single-center experience from Northern India. Indian Pediatr. 2019;56:196–8.
Deng Z, Zeng J, Lv C, Jiang L, Ji J, Li X, et al. Prevalence and factors associated with post-endoscopic retrograde cholangiopancreatography pancreatitis in children. Dig Dis Sci. 2021;66(1):224–30.
Dua K, Miranda A, Santharam R, Ramanujam S, Werlin S. ERCP in the evaluation of abdominal pain in children. Gastrointest Endosc. 2008;68(6):1081–5.
Durakbasa ÇU, Balik E, Yamaner S, Bulut T, Büyükuncu Y, Sökücü N, et al. Diagnostic and therapeutic endoscopic retrograde cholangiopancreatography (ERCP) in children and adolescents: Experience in a single institution. Eur J Pediatr Surg. 2008;18(4):241–4.
Enestvedt BK, Tofani C, Lee DY, Abraham M, Shah P, Chandrasekhara V, et al. Endoscopic retrograde cholangiopancreatography in the pediatric population is safe and efficacious. J Pediatr Gastroenterol Nutr. 2013;57(5):649–54.
Giefer MJ, Kozarek RA. Technical outcomes and complications of pediatric ERCP. Surg Endosc. 2015;29:3543–50.
Goetz M, Andersen P, Bergman J, Frei N, Schmidt A, Kähler G, et al. ERCP in babies: Low risk of post-ERCP pancreatitis–results from a multicentre survey. United Eur Gastroenterol J. 2020;8(1):77–80.
Green J, Scheeres D, Conrad H, Cloney D, Schlatter M. Pediatric ERCP in a multidisciplinary community setting: experience with a fellowship-trained general surgeon. Surg Endosc. 2007;21:2187–92.
Halvorson L, Halsey K, Darwin P, Goldberg E. The safety and efficacy of therapeutic ERCP in the pediatric population performed by adult gastroenterologists. Digest Dis Sci. 2013;58:3611–9.
Hsu RK, Draganov P, Leung JW, Tarnasky PR, Yu AS, Hawes RH, et al. Therapeutic ERCP in the management of pancreatitis in children. Gastrointest Endosc. 2000;51(4 Pt 1):396–400.
Issa H, Al-Haddad A, Al-Salem AH. Diagnostic and therapeutic ERCP in the pediatric age group. Pediatr Surg Int. 2007;23:111–6.
Keil R, Snajdauf J, Rygl M, Pycha K, Kotalová R, Drábek J, et al. Diagnostic efficacy of ERCP in cholestatic infants and neonates a retrospective study on a large series. Endoscopy. 2010;42(2):121–6.
Li ZS, Wang W, Liao Z, Zou DW, Jin ZD, Chen J, et al. A long-term follow-up study on endoscopic management of children and adolescents with chronic pancreatitis. Am J Gastroenterol. 2010;105(8):1884–92.
Limketkai BN, Chandrasekhara V, Kalloo AN, Okolo PI. Comparison of performance and safety of endoscopic retrograde cholangiopancreatography across pediatric age groups. Digest Dis Sci. 2013;58:2653–60.
Lin TK, Pathak SJ, Hornung LN, Vitale DS, Nathan JD, Abu-El-Haija M. Clinical outcomes following therapeutic endoscopic retrograde cholangiopancreatography in children with pancreas divisum. J Pediatr Gastroenterol Nutr. 2021;72(2):300–5.
Mercier C, Pioche M, Albuisson E, Ponchon T, Gonzalez J-M, Barthet M, et al. Safety of endoscopic retrograde cholangiopancreatography in the pediatric population: a multicenter study. Endoscopy. 2021;53(06):586–94.
Negm AA, Petersen C, Markowski A, Luettig B, Ringe KI, Lankisch TO, et al. The role of endoscopic retrograde cholangiopancreatography in the diagnosis of biliary atresia: 14 years’ experience. Eur J Pediatr Surg. 2018;28(03):261–7.
Otto AK, Neal MD, Slivka AN, Kane TD. An appraisal of endoscopic retrograde cholangiopancreatography (ERCP) for pancreaticobiliary disease in children: our institutional experience in 231 cases. Surg Endosc. 2011;25:2536–40.
Pan G, Yang K, Gong B, Deng Z. Analysis of the efficacy and safety of endoscopic retrograde cholangiopancreatography in children with symptomatic pancreas divisum. Front Pediatr. 2021;9:761331. https://doi.org/10.3389/fped.2021.761331.
Perrelli L, Nanni L, Costamagna G, Mutignani M. Endoscopic treatment of chronic idiopathic pancreatitis in children. J Pediatr Surg. 1996;31(10):1396–400.
Pfau PR, Chelimsky GG, Kinnard MF, Sivak MV Jr, Wong RC, Isenberg GA, et al. Endoscopic retrograde cholangiopancreatography in children and adolescents. J Pediatr Gastroenterol Nutr. 2002;35(5):619–23.
Poddar U, Yachha SK, Borkar V, Srivastava A, Saraswat VA. Clinical profile and treatment outcome of chronic pancreatitis in children: a long-term follow-up study of 156 cases. Scand J Gastroenterol. 2017;52(6–7):773–8.
Prasil P, Laberge J-M, Barkun A, Flageole H. Endoscopic retrograde cholangiopancreatography in children: a surgeon’s perspective. J Pediatr Surg. 2001;36(5):733–5.
Rashid R, Arfin MS, Karim AB, Alam MB, Mahmud S. Endoscopic Retrograde Cholangiopancreatography in Bangladeshi Children: Experiences and Challenges in a Developing Country. Pediatr Gastroenterol Hepatol Nutr. 2022;25(4):332.
Rescorla FJ, Plumley DA, Sherman S, Scherer L III, West KW, Grosfeld JL. The efficacy of early ERCP in pediatric pancreatic trauma. Journal of pediatric surgery. 1995;30(2):336–40.
Rocca R, Castellino F, Daperno M, Masoero G, Sostegni R, Ercole E, et al. Therapeutic ERCP in paediatric patients. Digest Liver Dis. 2005;37(5):357–62.
Rosen JD, Lane RS, Martinez JM, Perez EA, Tashiro J, Wagenaar AE, et al. Success and safety of endoscopic retrograde cholangiopancreatography in children. J Pediatr Surg. 2017;52(7):1148–51.
Saito T, Terui K, Mitsunaga T, Nakata M, Kuriyama Y, Higashimoto Y, et al. Role of pediatric endoscopic retrograde cholangiopancreatography in an era stressing less-invasive imaging modalities. J Pediatr Gastroenterol Nutr. 2014;59(2):204–9.
Shah R, Cohen RZ, Mekaroonkamol P, Taylor A, Freeman AJ, Fritzen C, et al. Retrospective Multicenter Matched Controlled Comparison of Endoscopic Retrograde Cholangiopancreatography in Pediatric Patients: A 10-year Experience. J Pediatr Gastroenterol Nutr. 2020;70(5):568–73.
Tagge EP, Tarnasky PR, Chandler J, Tagge DU, Smith C, Hebra A, et al. Multidisciplinary approach to the treatment of pediatric pancreaticobiliary disorders. J Pediatr Surg. 1997;32(2):158–65.
Taj MA, Leghari A, Qureshi S, Ghazanfar S, Niaz SK, Quraishy MS. Endoscopic retrograde cholangiopancreatography: a therapeutic modality in children and adolescents. JPMA. 2012;62(2):98–101.
Teng R, Yokohata K, Utsunomiya N, Takahata S, Nabae T, Tanaka M. Endoscopic retrograde cholangiopancreatography in infants and children. J Gastroenterol. 2000;35:39–42.
Troendle DM, Barth BA. ERCP can be safely and effectively performed by a pediatric gastroenterologist for choledocholithiasis in a pediatric facility. J Pediatr Gastroenterol Nutr. 2013;57(5):655–8.
Troendle DM, Barth BA. Pediatric considerations in endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin. 2016;26(1):119–36.
Troendle DM, Ruan W, Fishman DS, Barth BA, Liu QY, Giefer M, et al. Technical Outcomes in Pediatric Endoscopic Retrograde Cholangiopancreatography: Data from an International Collaborative. J Pediatr Gastroenterol Nutr. 2022;75(6):755–60.
Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB. Technical outcomes and complications of ERCP in children. Gastrointest Endosc. 2004;60(3):367–71.
Vegting I, Tabbers M, Taminiau J, Aronson D, Benninga M, Rauws E. Is endoscopic retrograde cholangiopancreatography valuable and safe in children of all ages? J Pediatr Gastroenterol Nutr. 2009;48(1):66–71.
Vrochides DV, Sorrells DL Jr, Kurkchubasche AG, Wesselhoeft CW Jr, Tracy TF Jr, Luks FI. Is there a role for routine preoperative endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in children? Arch Surg. 2005;140(4):359–61.
Wen J, Li T, Liu L, Bie L-K, Gong B. Long-term outcomes of therapeutic ERCP in pediatric patients with pancreas divisum presenting with acute recurrent or chronic pancreatitis. Pancreatology. 2019;19(6):834–41.
Yıldırım AE, Altun R, Ocal S, Kormaz M, Ozcay F, Selcuk H. The safety and efficacy of ERCP in the pediatric population with standard scopes: Does size really matter? Springerplus. 2016;5(1):1–5.
Yu Z, Zhu L, Yang X, Cao R, Chen Y. Efficacy and safety of endoscopic retrograde cholangiopancreatography in children. Zhonghua er ke za zhi= Chin J Pediatr. 2022;60(12):1295–301.
Zargar SA, Javid G, Khan BA, Yattoo GN, Shah AH, Gulzar GM, et al. Endoscopic sphincterotomy in the management of bile duct stones in children. Am J Gastroenterol. 2003;98(3):586–9.
Zeng JQ, Deng ZH, Yang KH, Zhang TA, Wang WY, Ji JM, et al. Endoscopic retrograde cholangiopancreatography in children with symptomatic pancreaticobiliary maljunction: A retrospective multicenter study. World J Gastroenterol. 2019;25(40):6107–15.
Zhang J, Guo S, Mei TL, Zhou J, Wang GL, Yu FH, et al. Endoscopic retrograde cholangiopancreatography in the treatment of pancreaticopleural fistula in children. World J Gastroenterol. 2020;26(37):5718–30.
Weng M, Wang L, Weng H, Gu J, Wang X. Utility of endoscopic retrograde cholangiopancreatography in infant patients with conservational endoscopy. Transl Pediatr. 2021;10(10):2506.
Kolodziejczyk E, Jurkiewicz E, Pertkiewicz J, Wejnarska K, Dadalski M, Kierkus J, et al. MRCP versus ERCP in the evaluation of chronic pancreatitis in children: which is the better choice? Pancreas. 2016;45(8):1115–9.
Tanisaka Y, Ryozawa S, Mizuide M, Araki R, Fujita A, Ogawa T, et al. Status of single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: Systematic review and meta-analysis on biliary interventions. Digest Endosc. 2021;33(7):1034–44.
Sun R, Xu X, Zheng Q, Zhan J. Therapeutic endoscopic retrograde cholangiopancreatography for pediatric hepato-pancreato-biliary diseases: a systematic review and meta-analysis. Front Pediatr. 2022;10:915085.
Usatin D, Fernandes M, Allen IE, Perito ER, Ostroff J, Heyman MB. Complications of endoscopic retrograde cholangiopancreatography in pediatric patients; a systematic literature review and meta-analysis. J Pediatr. 2016;179:160-5 e3.
Thaker AM, Mosko JD, Berzin TM. Post-endoscopic retrograde cholangiopancreatography pancreatitis. Gastroenterol Rep. 2015;3(1):32–40.
Ribeiro IB, do Monte Junior ES, Neto AAM, Proença IM, de Moura DTH, Minata MK, et al. Pancreatitis after endoscopic retrograde cholangiopancreatography: A narrative review. World J Gastroenterol. 2021;27(20):2495.
Adler DG. Endoscopic retrograde cholangiopancreatography (ERCP) in children: technique, success, and adverse events.
Acknowledgements
This research project has been funded by Clinical Reseach Development Center, Mofid Children's Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran. and the National Agency for Strategic Research in Medical Education. Tehran. Iran. Grant No 992942.
We express our gratitude to the participants of this study.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
S.F. and A.H. contributed to the conception, design, and statistical analysis. MH.S., E.SH., A.S., S.T., N.I., and S.F. contributed to data collection and manuscript draft. S.F and A.H contributed to the manuscript draft and critical revision. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research council and ethics committee Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hosseini, A., Sohouli, M.H., Sharifi, E. et al. Indications, success, and adverse event rates of pediatric endoscopic retrograde cholangiopancreatography (ERCP): a systematic review and meta-analysis. BMC Pediatr 23, 596 (2023). https://doi.org/10.1186/s12887-023-04392-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04392-5