Abstract
Background and Aims
Endoscopic retrograde cholangiopancreatography (ERCP) is the standard of care for the management of choledocholithiasis but carries risk of complications which may result in significant morbidity and mortality. While currently available guidelines endorse the use of ERCP for the management of symptomatic common bile duct stones, the need for ERCP in incidentally found asymptomatic choledocholithiasis is more controversial, and practice varies on a geographic and institutional level. This systematic review and meta-analysis is conducted to compare post-ERCP adverse events between asymptomatic and symptomatic choledocholithiasis patients.
Methods
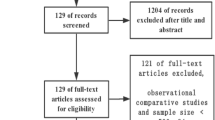
We searched PubMed/Embase/Web of Science databases to include all studies comparing post-ERCP outcomes between asymptomatic and symptomatic choledocholithiasis patients. The primary outcome was post-ERCP pancreatitis (PEP), while secondary outcomes included post-ERCP cholangitis, bleeding, and perforation. We calculated pooled risk ratios (RR) and 95% confidence intervals (CIs) using the Mantel–Haenszel method within a random-effect model.
Results
Our analysis included six observational studies, totaling 2,178 choledocholithiasis patients (392 asymptomatic and 1786 symptomatic); 53% were female. Asymptomatic patients exhibited a higher risk of PEP compared with symptomatic patients (11.7% versus 4.8%; RR 2.59, 95% CI 1.56–4.31, p ≤ 0.001). No significant difference was observed in post-ERCP cholangitis, bleeding, or perforation rates between the two groups.
Conclusions
Asymptomatic patients with choledocholithiasis appear to have a higher risk of PEP than symptomatic patients, while the risk of other post-ERCP adverse events is similar between the two groups. Interventional endoscopists should thoroughly discuss potential adverse events (particularly PEP) with asymptomatic patients before performing ERCP and utilize PEP-prevention measures more liberally in this subgroup of patients.



Similar content being viewed by others
Abbreviations
- PEP:
-
Post-ERCP pancreatitis
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
References
Figueiredo JC et al. Sex and ethnic/racial-specific risk factors for gallbladder disease. BMC gastroenterology 2017;17:1–12.
Hall MJ, Schwartzman A, Zhang J, Liu X. Ambulatory surgery data from hospitals and ambulatory surgery centers: United States. National health statistics reports 2010;2017:1–15.
Buxbaum, J.L., et al., ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointestinal endoscopy, 2019. 89: p. 1075–1105. e15.
Kochar, B., et al., Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointestinal endoscopy, 2015. 81: p. 143–149. e9.
Narula VK et al. Clinical spotlight review for the management of choledocholithiasis. Surgical Endoscopy 2020;34:1482–1491.
Manes G et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2019;51:472–491.
Liver, E.A.f.t.S.O.t., EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. Journal of hepatology, 2016. 65: p. 146–181.
Williams E et al. Updated guideline on the management of common bile duct stones (CBDS). Gut 2017;66:765–782.
Warttig, S., S. Ward, and G. Rogers, Diagnosis and management of gallstone disease: summary of NICE guidance. Bmj, 2014. 349.
Ricci C et al. Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA surgery 2018;153:e181167–e181167.
Chandrasekhara V et al. Adverse events associated with ERCP. Gastrointestinal endoscopy 2017;85:32–47.
Kim SB, Kim KH, Kim TN. Comparison of outcomes and complications of endoscopic common bile duct stone removal between asymptomatic and symptomatic patients. Digestive diseases and sciences 2016;61:1172–1177.
Saito H et al. Endoscopic retrograde cholangiopancreatography-related complications for bile duct stones in asymptomatic and symptomatic patients. JGH Open 2021;5:1382–1390.
Xu XD, Qian JQ, Dai JJ, Sun ZX. Endoscopic treatment for choledocholithiasis in asymptomatic patients. Journal of Gastroenterology and Hepatology 2020;35:165–169.
Page MJ et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International journal of surgery 2021;88:105906.
Stroup DF et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Jama 2000;283:2008–2012.
Wells, G.A., et al., The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
Yamaji, Y., et al., Efficacy and Safety of Endoscopic Removal for Asymptomatic Common Bile Duct Stones in Comparison with Symptomatic Stones. Tokai Journal of Experimental & Clinical Medicine, 2022. 47.
Xiao L et al. Comparable safety of ERCP in symptomatic and asymptomatic patients with common bile duct stones: a propensity-matched analysis. Scandinavian Journal of Gastroenterology 2021;56:111–117.
Kadokura M et al. Asymptomatic common bile duct stones are associated with increased risk of post-endoscopic retrograde cholangiopancreatography pancreatitis. JMA journal 2021;4:141–147.
Hakuta R et al. Natural history of asymptomatic bile duct stones and association of endoscopic treatment with clinical outcomes. Journal of gastroenterology 2020;55:78–85.
Freeman ML et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointestinal endoscopy 2001;54:425–434.
Bailey AA et al. Needle-knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis (with video). Gastrointestinal endoscopy 2010;71:266–271.
Bailey A et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy 2008;40:296–301.
Kaw, M. and P. Kaw, 3357 Complications of diagnostic and therapeutic ercp. Gastrointestinal Endoscopy, 2000. 51: p. AB70.
Collins C et al. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Annals of surgery 2004;239:28.
Möller M et al. Natural course vs interventions to clear common bile duct stones: data from the Swedish Registry for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks). JAMA surgery 2014;149:1008–1013.
Cox MR, Budge JP, Eslick GD. Timing and nature of presentation of unsuspected retained common bile duct stones after laparoscopic cholecystectomy: a retrospective study. Surgical endoscopy 2015;29:2033–2038.
Schneider J et al. Mortality Risk for Acute Cholangitis (MAC): a risk prediction model for in-hospital mortality in patients with acute cholangitis. BMC gastroenterology 2016;16:1–8.
Schepers NJ et al. Urgent endoscopic retrograde cholangiopancreatography with sphincterotomy versus conservative treatment in predicted severe acute gallstone pancreatitis (APEC): a multicentre randomised controlled trial. The Lancet 2020;396:167–176.
Conflict of interest
The authors declare no conflicts of interest related to this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obaitan, I., Mohamed, M.F.H., Beran, A. et al. Comparative Risks of Post-ERCP Adverse Events in Patients with Asymptomatic and Symptomatic Choledocholithiasis: A Systematic Review and Meta-Analysis. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08374-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08374-0