Abstract
Background
Impaired intestinal microcirculation seems to play an important role in the pathogenesis of necrotizing enterocolitis (NEC). A previous study showed that a SrSO2 < 30% is associated with an increased risk of developing of NEC. We aimed to determine the clinical usefulness of the cut off < 30% for SrSO2 in predicting NEC in extremely preterm neonates.
Methods
This is a combined cohort observational study. We added a second cohort from another university hospital to the previous cohort of extremely preterm infants. SrSO2 was measured for 1–2 h at days 2–6 after birth. To determine clinical usefulness we assessed sensitivity, specificity, positive and negative predictive values for mean SrSO2 < 30. Odds ratio to develop NEC was assessed with generalized linear model analysis, adjusting for center.
Results
We included 86 extremely preterm infants, median gestational age 26.3 weeks (range 23.0-27.9). Seventeen infants developed NEC. A mean SrSO2 < 30% was found in 70.5% of infants who developed NEC compared to 33.3% of those who did not (p = 0.01). Positive and negative predictive values were 0.33 CI (0.24–0.44) and 0.90 CI (0.83–0.96), respectively. The odds of developing NEC were 4.5 (95% CI 1.4–14.3) times higher in infants with SrSO2 < 30% compared to those with SrSO2 ≥ 30%.
Conclusions
A mean SrSO2 cut off ≥ 30% in extremely preterm infants between days 2–6 after birth may be useful in identifying infants who will not develop NEC.
Similar content being viewed by others
Introduction
Impaired microcirculation of the intestines seems to play an important role in the pathogenesis of necrotizing enterocolitis (NEC) in extremely preterm neonates [1]. Fetuses and newborn animals have an immature splanchnic perfusion, with a less pronounced vasodilatory response and an increased oxygen extraction to systemic stress, when compared with older animals and humans [2, 3]. Similarly, many studies on intestinal perfusion measured by near-infrared spectroscopy (NIRS) have reported that splanchnic oxygenation is impaired before the onset of NEC in preterm infants [4, 5].
Since bowel ischemia, or at least impaired intestinal perfusion, seems to be associated with the development of NEC [1, 6], measuring splanchnic oxygenation (SrSO2) and oxygen extraction might detect changes compatible with the pre-stages of NEC. Piglet models have shown that low SrSO2 within the first days of life is a risk factor for NEC [7] and, indeed, impaired SrSO2 before the onset of clinical NEC has been reported in preterm infants (3, 4).
In a previous study in extremely preterm infants, it was shown that a 1-hour mean splanchnic oxygenation < 30%, between days 2 and 6 of life, was associated with an increased risk of developing NEC, but this risk seems to change through gestational age [8]. In order to understand the validity and utility of our previous findings given the relatively low samples size, we chose to combine our cohort with another comparable European cohort to study the clinical usefulness of the splanchnic oxygenation cut off. The aim of this study was to strengthen our previous findings in a larger pooled cohort and to determine whether the cut off value of < 30% for mean SrSO2 in the first week after birth has some clinical usefulness and can predict NEC in extremely preterm neonates.
Methods
This was a combined cohort study pooling extremely preterm neonates (< 28 weeks gestational age) from two level III NICUs at the Karolinska University Hospital, Stockholm, Sweden and the University Medical Center, Groningen, Netherlands.
Participants
The population in this study was formed by merging two European cohorts (one Swedish and one Dutch) of extremely preterm newborns where cerebral and splanchnic monitoring was performed in the first week of life. Inclusion criteria were: infants born before 28 weeks of gestation. Exclusion criteria were infants born before 23 weeks of gestation, major abdominal wall defects, major known intra-abdominal malformations, infants who already had NEC/ spontaneous intestinal perforation or developed NEC/ spontaneous intestinal perforation within 24 h from the measurements and critically ill neonates not tolerating abdominal ultrasound or NIRS monitoring.
Setting
Swedish cohort
Extremely preterm infants, born before 28 weeks of gestational age, were included in the study from September 2014 to December 2016. Cerebral and splanchnic oxygenation monitoring was performed at postnatal age between days 2 and 6, within 96 h after the first enteral feeding. This population has been described in detail in a previous publication [8]. A near infrared spectroscopy (NIRS) INVOS 5100c monitor (Medtronic™, (Minneapolis,) USA) with neonatal INVOS sensors was used to measure cerebral (CrSO2) and splanchnic regional oxygenation (SrSO2). To measure cerebral oxygenation, a sensor was placed in the frontoparietal side of the head. For the measurement of splanchnic oxygenation, a sensor was placed just below the umbilicus. For each NIRS recording we allowed a baseline of 5 to 15 min for stabilization, which was not included in the analysis. The measurements were performed for at least one hour. According to the local feeding protocol, infants with birth weights < 1250 g were fed by continuous enteral feeds and > 1250 g by bolus feeds during the measurements.
Dutch cohort
Extremely preterm infants, born before 28 weeks of gestational age, were included in the study from January 2016 to March 2018. With the same monitor as the Swedish cohort, INVOS 5100c monitor (Medtronic™, (Minneapolis,) USA), we measured cerebral and splanchnic oxygenation between days 1 and 7 after birth as part of standard clinical care. The neonatal INVOS™ SomaSensor was placed below the umbilicus and on the left or right frontoparietal side of the head for the measurement of SrSO2 and CrSO2, respectively. Sensors were placed on top of Mepitel® sheets (Mölnlycke, Sweden) for skin protection [9]. Data were saved in an offline pseudonymized database.
For research purposes the sensor placement was checked and verified every morning by the attending nurse and researcher. A daily two-hour mean of rsSO2 was calculated before or, when unavailable, closest to the sensor verification. A 2-hour period with at least 80% of available data was selected. According to local protocol, every infant received intermittent bolus feeding every two hours. We selected the measurements at day 4 or, when unavailable, at day 3 or 5 for the comparison with the Swedish cohort.
Clinical variables
Clinical variables collected from the infants’ charts included: demographic data, small for gestational age status (according to the national reference values)[10, 11], amount and type of feeding, hemoglobin levels, presence of intraventricular hemorrhage, Apgar score at 5 min, respiratory support, hemodynamically significant patent ductus arteriosus (defined as infants needing treatment), postnatal age at time of NIRS measurement and mortality.
The outcome was the NEC diagnosis, which was based on clinical signs plus the presence of intramural gas on abdominal radiographs and/or histological evidence of NEC. In both cohorts, NEC diagnosis was verified by the authors of the site (EP,MB,EK,JH) according to the Bell’s criteria. Unclear cases were discussed together, and consensus was reached in all cases. Infants with only a clinical suspicion of NEC (Bell´s stage < 2 A) were not considered as having NEC. Surgical NEC was defined as a patient who had an indication for surgical treatment according to the treating physicians.
Data and statistical analysis
NIRS data were collected automatically once every 6 s and stored offline for analysis. The data were analyzed for artifacts which afterwards were removed. In both cohorts, artifacts were defined as: changes in SrSO2 and CrSO2 that could not be physiologically explained, misplacement of the sensor or missing rSO2 values due to measurement failure. We chose not to exclude the 15% and 95% values (the minimum and maximum values for the device used) from our analyses.
Regarding NIRS variables, we calculated the mean SrSO2 and CrSO2. Moreover, we calculated the splanchnic-cerebral oxygenation ratio (SCOR) as splanchnic oxygenation divided by mean cerebral oxygenation (SrSO2/CrSO2).
First, demographic and clinical variables were compared between the two cohorts. Second, we divided all infants based on the SrSO2 30% cut off [8]. Third, specificity, sensitivity, and positive and negative predictive values with confidence intervals were calculated with a bootstrap cross-validation in R 4.1.2. Fourth, generalized linear models were applied, with logit link and NEC as dependent variable, to analyze the primary outcome (NEC) which was presented as an odds ratio. Finally, variables for the final model were chosen through univariate analysis with a P-value < 0.05.
The Mann-Whitney U test, Student’s t-test and chi2 or Fisher‘s exact test were used for non-parametric, parametric, or categorical data, respectively. We used the statistical program STATA version 14.2 (StataCorp, TX) to perform the rest of the analyses.
Results
Participants
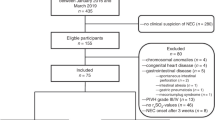
Eighty-six extremely preterm infants were included in the analysis: 44 from the Swedish and 42 from the Dutch cohort (Fig. 1). Eight infants developed NEC in the Swedish and nine in the Dutch cohort, the median postnatal age at NEC diagnosis was 15 (IQR 10–23) days. The incidence of NEC was 19.8%, with 70% of the NEC cases requiring surgical intervention.
Patient characteristics of the two cohorts are shown in Table 1. Median gestational age of the final total cohort was 26.3 weeks IQR (25.3–27.1). Infants from the Swedish cohort had significantly lower gestational age, lower birth weight, and were more often delivered by caesarean section. All infants underwent NIRS monitoring at a mean postnatal age of 4.0 ± 0.9 days. Median SrSO2 was 34.8 (21.5–52.4)%. There was no difference in median SrSO2, CrSO2 or SCOR between the two centers.
Outcomes: Splanchnic oxygenation cut off and NE
In the final cohort, 36 (41.8%) infants had a mean SrSO2 < 30% between days 2–6 of life. These infants had a higher incidence of NEC (33.3% vs. 10.0%, p = 0.012) and surgical NEC (27.8% vs. 4%, p = 0.003) than infants with a SrSO2 ≥ 30% (Table 2). The median age at NEC was 15 day (IQR 10–23). We did not find any other differences between the two groups (Table 2). Of all infants who later on developed NEC, 70.6% had a SrSO2 < 30% while only 33.3% of infants who did not develop NEC had a SrSO2 < 30% (p = 0.012).
Sensitivity, specificity, negative and positive predictive values, and their 95% CIs were calculated (Table 3). The positive predictive value was 0.33 (95% CI 0.24–0.44) and the negative predictive value was 0.90 (95% CI 0.83–0.96).
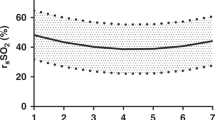
The odds of developing NEC were 4.5 (95% CI 1.4–14.3) times higher in infants with SrSO2 < 30% compared to those with SrSO2 ≥ 30%. The odds ratio was still statistically significant after adjusting for gestational age and cohort: aOR 9.4 (95% CI 2.2–40.2) (Table 4). Because gestational age significantly changed the odds ratio, we plotted a graph to see how the predicted probability of developing NEC if SrSO2 < 30% changed with gestational age (Fig. 2). The association between SrSO2 < 30% and NEC seems to vary with changing gestational age. We therefore performed subgroup analyses and calculated the OR to develop NEC for infants born < 26 weeks and for those born ≥ 26 weeks of age (Table 4). In supplemental material 1, explanatory variables for infants who developed NEC and those who did not are shown. Univariate analyses are shown in supplemental material 2.
Discussion
We found in this multi-center study including extremely preterm infants that the cut off value of 30% for SrSO2, between day 2 and 6 after birth, has a high negative predictive value for NEC, but a rather poor positive predictive value. This indicates that this cut off for SrSO2 could help in identifying extremely preterm newborn infants with a low risk of NEC, but has limited value in positively predicting NEC development. The cut off value of 30% for SrSO2 is more discriminative for surgical NEC and in the smallest infants, born at a gestational age less than 26 weeks.
Despite an increasing amount of research, the role of NIRS as non-invasive monitoring of intestinal oxygenation in preterm infants is still uncertain and NIRS is generally not used as a clinical tool [12, 13]. Previous studies have also found lower SrSO2 in preterm infants before NEC onset [4, 14]. Patel et al. found a lower SrSO2 in the first week in preterm infants who later developed NEC compared to infants who did not develop NEC. Cortez et al. found a lower SrSO2 before NEC/SIP onset in a small study. However, they also found that in the first five days after birth, SrSO2 was similar between the infants who later developed NEC/SIP and the control infants. Moreover, Schat et al. found no lower SrSO2 in preterm infants between days 3 and 5 after birth, but only a trend of a lower SrSO2 in the 48 h before NEC development [5].
The predicted probability of developing NEC seems to vary with gestational age as the association between a SrSO2 < 30% and NEC was stronger in the more extreme preterm infants (< 26 weeks of gestation). It is known that SrSO2 varies with gestational and postnatal age [9], hence, gestational age is an important confounder in this study [15]. The reason for the fact that SrSO2 appears to be more predictive in the most extreme preterm infants remains unknown. Perhaps, in the complex multifactorial pathogenesis of preterm NEC, the contribution of immature splanchnic microcirculation may be larger for the smallest infants than for the older ones. An extremely immature splanchnic microcirculation has less capacity to maintain an adequate splanchnic oxygenation when needed, while slightly older infants may have a better capacity to maintain an adequate splanchnic oxygenation from becoming critically low [2, 16]. Another potential explanation would be that older infants have more stools which may affect the NIRS value increasing the absorption of NIRS photons [17] or due to the increased peristalsis that can affect the NIRS signal. It is also known that probiotics, which have been extensively studied as a prevention for NEC [18], do not work as well in infants with a birth weight of less than 1000 g [19, 20], meaning that preventing dysbiosis appears not to be enough in the smallest infants, where impaired microcirculation and ischemia might play a bigger role in NEC development.
A low splanchnic oxygenation is a proxy for impaired microcirculation or, less likely, increased intestinal oxygen consumption [21]. The use of splanchnic NIRS monitoring in the first week of life can lead to possible preventive measures, such as slower increasing of feeds, waiting for supplementations and a higher level of monitoring. Nevertheless, at the moment there is no evidence that all these strategies can actually decrease the risk of NEC or improve the outcome [22, 23]. Alternatively, being able to select a very high NEC risk population using NIRS would enable newly developed strategies to be tested in only this very high risk population. Not only that, it would also prevent possibly harmful strategies from being applied in this population.
The percentage of NEC-required surgery was very high in this population, probably due to the low gestational age of this combined cohort and the exclusion of uncertain NEC cases.
Although this study has some major strengths such as the combination of two cohorts from two different level three university hospitals, it also has some limitations such as the relatively small number of patients, differences between the two cohorts (i.e. different feeding strategies and umbilical catheters) and the use of only one single measurement. In the Dutch center, at the time of the study, we used to tape the umbilical catheter to the infraumbilical skin, which left only little space for the NIRS sensor, and unfortunately resulted in the exclusion of a number of small infants, potentially inducing selection bias. Another limitation of the study may be a substantial difference in the incidence of caesarean sections between both cohorts which may indicate a more active approach in the Swedish cohort, which was also reflected by the lower mean gestational age in this cohort. Finally, although the inclusion and exclusion criteria were similar between both cohorts, the Swedish cohort used an opt-in inclusion strategy while the Dutch cohort used an opt-out inclusion strategy for the study. Clearly all these differences could affect the outcome of the study. Even so, we did not detect a difference in SrSO2 between the two centers. Moreover, we corrected for the potential bias of center in the regression analysis.
The cut off was previously calculated from the Swedish cohort, but being aware that the results from small cohort carry uncertainty and less external validity, we needed to test it again in a combined cohort to increase the validity of the results and to study the association between SrSO2 and surgical NEC with increased numbers.
There are also limitations related to NIRS measurements and technology. Short measurements that are not repeated as well as artefacts (such as movements, air, and stools) are the two most important ones. We opted for short measurement durations because it was easier to ensure the quality of the SrSO2 in the smallest infants and to better estimate when artefacts were caused by movements.
In conclusion, using a cut off of 30% for splanchnic oxygenation measured in the first week in extremely preterm infants appeared to be clinically useful only in identifying infants who will not develop NEC. Finally extremely preterm infants with splanchnic oxygenation below 30% in the first week of life carry higher odds of developing NEC, especially if born before 26 weeks of gestation, supporting the contribution of gut hypoxia to NEC development in extremely preterm born infants.
Data Availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Watkins DJ, Besner GE. The role of the intestinal microcirculation in necrotizing enterocolitis. Semin Pediatr Surg. 2013;22(2):83–7.
Chaaban H, Stonestreet BS. Intestinal hemodynamics and oxygenation in the perinatal period. Semin Perinatol. 2012;36(4):260–8.
Yao AC, Gootman PM, Frankfurt PP, DiRusso SM. Age-related superior mesenteric arterial flow changes in piglets: effects of feeding and hemorrhage. Am J Physiol. 1986;251(5 Pt 1):G718–723.
Patel AK, Lazar DA, Burrin DG, Smith EO, Magliaro TJ, Stark AR, Brandt ML, Zamora IJ, Sheikh F, Akinkuotu AC, et al. Abdominal near-infrared spectroscopy measurements are lower in preterm infants at risk for necrotizing enterocolitis. Pediatr Crit Care Med. 2014;15(8):735–41.
Schat TE, van Zoonen A, van der Laan ME, Mebius MJ, Bos AF, Hulzebos CV, Boezen HM, Hulscher JBF, Kooi EMW. Early cerebral and intestinal oxygenation in the risk assessment of necrotizing enterocolitis in preterm infants. Early Hum Dev. 2019;131:75–80.
Young CM, Kingma SD, Neu J. Ischemia-reperfusion and neonatal intestinal injury. J Pediatr. 2011;158(2 Suppl):e25–28.
Gay AN, Lazar DA, Stoll B, Naik-Mathuria B, Mushin OP, Rodriguez MA, Burrin DG, Olutoye OO. Near-infrared spectroscopy measurement of abdominal tissue oxygenation is a useful indicator of intestinal blood flow and necrotizing enterocolitis in premature piglets. J Pediatr Surg. 2011;46(6):1034–40.
Palleri E, Wackernagel D, Wester T, Bartocci M. Low splanchnic oxygenation and risk for necrotizing Enterocolitis in extremely Preterm Newborns. J Pediatr Gastroenterol Nutr. 2020;71(3):401–6.
McNeill S, Gatenby JC, McElroy S, Engelhardt B. Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J perinatology: official J Calif Perinat Association. 2011;31(1):51–7.
Hoftiezer L, Hof MHP, Dijs-Elsinga J, Hogeveen M, Hukkelhoven C, van Lingen RA. From population reference to national standard: new and improved birthweight charts. Am J Obstet Gynecol. 2019;220(4):383. e381-383 e317.
Niklasson A, Ericson A, Fryer JG, Karlberg J, Lawrence C, Karlberg P. An update of the swedish reference standards for weight, length and head circumference at birth for given gestational age (1977–1981). Acta Paediatr Scand. 1991;80(8–9):756–62.
Seager E, Longley C, Aladangady N, Banerjee J. Measurement of gut oxygenation in the neonatal population using near-infrared spectroscopy: a clinical tool? Archives of disease in childhood Fetal and neonatal edition. 2020;105(1):76–86.
Metcalfe KHM, Stienstra R, McHoney M. NIRS as a biomarker of bowel ischaemia & surgical pathology: a meta-analysis of studies in newborns. Early Hum Dev. 2021;161:105437.
Cortez J, Gupta M, Amaram A, Pizzino J, Sawhney M, Sood BG. Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J maternal-fetal neonatal medicine: official J Eur Association Perinat Med Federation Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2011;24(4):574–82.
Kuik SJ, van Zoonen A, Bos AF, Van Braeckel K, Hulscher JBF, Kooi EMW. The effect of enteral bolus feeding on regional intestinal oxygen saturation in preterm infants is age-dependent: a longitudinal observational study. BMC Pediatr. 2019;19(1):404.
Sieber C, Beglinger C, Jaeger K, Hildebrand P, Stalder GA. Regulation of postprandial mesenteric blood flow in humans: evidence for a cholinergic nervous reflex. Gut. 1991;32(4):361–6.
Thompson A, Benni P, Seyhan S, Ehrenkranz R. Meconium and transitional stools may cause interference with near-infrared spectroscopy measurements of intestinal oxygen saturation in preterm infants. Adv Exp Med Biol. 2013;765:287–92.
van den Akker CHP, van Goudoever JB, Shamir R, Domellöf M, Embleton ND, Hojsak I, Lapillonne A, Mihatsch WA, Berni Canani R, Bronsky J, et al. Probiotics and Preterm Infants: a position paper by the European Society for Paediatric Gastroenterology Hepatology and Nutrition Committee on Nutrition and the european Society for Paediatric Gastroenterology Hepatology and Nutrition Working Group for Probiotics and Prebiotics. J Pediatr Gastroenterol Nutr. 2020;70(5):664–80.
Abrahamsson TR. Using probiotics to prevent necrotising enterocolitis. Acta Paediatr (Oslo Norway: 1992). 2017;106(11):1718–9.
Sharif S, Meader N, Oddie SJ, Rojas-Reyes MX, McGuire W. Probiotics to prevent necrotising enterocolitis in very preterm or very low birth weight infants. Cochrane Database Syst Rev. 2020;10:CD005496.
Dotinga BM, Mintzer JP, Moore JE, Hulscher JBF, Bos AF, Kooi EMW. Maturation of intestinal oxygenation: a review of mechanisms and clinical implications for Preterm Neonates. Front Pediatr. 2020;8:354.
Oddie SJ, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2017;8:CD001241.
Dorling J, Abbott J, Berrington J, Bosiak B, Bowler U, Boyle E, Embleton N, Hewer O, Johnson S, Juszczak E, et al. Controlled trial of two incremental milk-feeding rates in Preterm Infants. N Engl J Med. 2019;381(15):1434–43.
Acknowledgements
We thank the nurses, the medical staff of the neonatology department of both Karolinska University Hospital in Stockholm and Beatrix Children’s Hospital in Groningen, and the medical students who participate in the NIRS-team, for their contribution in collecting data of this study. This study was part of the research program of the Graduate School of Medical Sciences, Research Institutes SHARE and BCN, University of Groningen. We, furthermore, acknowledge our statistician Eva Hagel at Karolinska Institutet for the statistical advice.
Funding
Open access funding provided by Karolinska Institute. The study was financially supported by Stiftelsen Frimurare Barnhuset, Lilla Barnets fond, and Kronprinsessan Lovisas Förening för Barnasjukvård in Stockholm and the Junior Scientific Master Class of the University of Groningen. They had no role in this study.
Author information
Authors and Affiliations
Contributions
EP, MH, and EK were involved in the design and execution of the study. TW wrote the ethical application to IRB. Data were collected by EP and MB (Swedish cohort) and by MH and EK (in the Dutch Cohort). EP performed the analysis. All other authors were involved in the final consensus process of the protocol, interpretation of the data and revised the manuscript critically for important intellectual content. EP and MH drafted the manuscript and all other authors read, edited and approved the final manuscript for publication.EP prepared the tables, MH prepared the flow chart.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
For the Swedish cohort, we obtained informed parental consent in all cases. Ethical approval was obtained from the Etikprövningsmyndigheten, Ethical Review Board in Stockholm (Dnr 2014/500 − 31).
For the Dutch cohort, the data were collected as part of standard clinical care and stored pseudonymized. We used data from patients whose parents did not opt-out of data collection, as was routinely offered. The need for parental consent was therefore waived by the Medical Ethical Committee of the University Medical Center Groningen (2016/00410). Ethical approval is provided from different Ethical boards in different European countries.
In both the Swedish and the Dutch cohort all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
This manuscript does not include any details, image or video relating to an individual person. We obtained the consent for publication of the study data and results as whole.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Palleri, E., van der Heide, M., Hulscher, J.B. et al. Clinical usefulness of splanchnic oxygenation in predicting necrotizing enterocolitis in extremely preterm infants: a cohort study. BMC Pediatr 23, 336 (2023). https://doi.org/10.1186/s12887-023-04145-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04145-4