Abstract
Background
Bronchopleural fistula (BPF) is a severe complication following pneumonia or pulmonary surgery, resulting in persistent air leakage (PAL) and pneumothorax. Surgical options include resection, coverage of the fistula by video-assisted thoracoscopic surgery (VATS), or pleurodesis. Interventional bronchoscopy is preferred in complex cases and involves the use of sclerosants, sealants and occlusive valve devices.
Case presentation
A 2.5-year-old girl was admitted to our hospital with persistent fever, cough and dyspnoea. Clinical and radiological examination revealed right-sided pneumonia and pleural effusion. The child was started on antibiotics, and the effusion was drained by pleural drainage. Following removal of the chest tube, the child developed tension pneumothorax. Despite insertion of a new drain, the air leak persisted. Thoracoscopic debridement with placement of another new drain was performed after 4 weeks, without abolishment of the air leak. Bronchoscopy with bronchography revealed a BPF in right lung segment 3 (right upper-lobe anterior bronchus). We opted for an interventional approach that was performed under general anaesthesia during repeat bronchoscopy. Following bronchographic visualisation of the fistula, a 2.7 French microcatheter was placed in right lung segment 3 (upper lobe), allowing occlusion of the fistula by successive implantation of 4 detachable high-density packing volume coils, which were placed into the fistula. Subsequent bronchography revealed no evidence of residual leakage, and the chest tube was removed 2 days later. The chest X-ray findings normalized, and follow-up over 4 years was uneventful.
Conclusions
Bronchoscopic superselective occlusion of BPF using detachable high-density packing large-volume coils was a successful minimally invasive therapeutic intervention performed with minimal trauma in this child and has not been reported thus far. In our small patient, the short interventional time, localized intervention and minimal damage in the lung seemed superior to the corresponding outcomes of surgical lobectomy or pleurodesis in a young growing lung, enabling normal development of the surrounding tissue. Follow-up over 4 years did not show any side effects and was uneventful, with normal lung-function test results to date.
Similar content being viewed by others
Background
Bronchopleural fistulae (BPFs) are rare but severe complications of pneumonia, lung abscess or pleural empyema. They may also occur following thoracic surgical procedures resulting in persistent air leakage (PAL). Surgical options include resection, video-assisted thoracoscopic surgery (VATS), coverage of the fistula, or pleurodesis. Interventional bronchoscopy is preferred in complex cases. Endoscopic interventional treatment options in adults comprise a variety of procedures, including implantation of devices such as volume-reduction valves [1] or ASD occluders [2], following fistula visualization and balloon sizing under fluoroscopy. The devices must achieve immediate, airtight occlusion and must subsequently be removed. Risks comprise valve malpositioning and device expectoration during cough [3]. Furthermore, sclerosants are used to achieve pleurodesis by using talc [4], ethanol [5], silver nitrate [6], polyethylene glycol [7], tetracycline, doxycycline [8], minocycline [4] or bleomycin [9]. They have to be administered strictly locally, as they provoke severe inflammatory reactions, which might cause severe damage to other pulmonary segments. Complications include chest pain, fever, acute lung injury, and/or subsequent interstitial lung disease [9]. In cases of persistent pneumothorax, the altered lung may be unable to be re-expanded [10]. Autologous blood instillation into the pleural cavity for coverage of the fistula is of limited success, resulting in a pleural callosity and may be complicated by chest tube clots, pleuritis and empyema [10, 11]. While this treatment is easy to perform, success is uncertain, requiring prolonged periods of chest tube drainage. Sealants such as cyanoacrylate [12, 13], fibrin glue [14,15,16,17], albumin-glutaraldehyde glue [18], hydrogel [19] or oxidized cellulose [20] have also been used for fistula occlusion. Since interventional occlusion with detachable metallic coils usually does not achieve immediate airtight occlusion, it has been recommended to combine the use of these coils with additional topical sealants [21]. While this technique is associated with the risk of displacement of the sealant, long-term animal studies have shown complete resorption of the glue within 3 months [17]. To date, interventional procedures for occlusion of BPFs have been performed exclusively in the adult population.
Case presentation
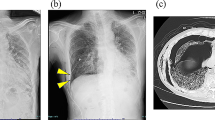
We report on a 2 ½-year-old female child who presented in a reduced general condition with a fever of 40 °C, tachypnoea, marked respiratory distress and cough. Clinically and radiologically, right-sided pneumonia and pleural effusion were diagnosed (Fig. 1a). The child was transferred to the PICU, started on antibiotics, ventilated noninvasively and treated by chest tube insertion. Two days later, immediately after removal of the drainage, the patient developed tension pneumothorax (Fig. 1b). A new drain was placed, but the air leak persisted for the next 3 weeks, and weaning from drainage was impossible. A CT scan (Fig. 1c) displayed a partially collapsed right lung with dystelectasis and septate pneumothorax. As surgical thoracoscopic debridement with insertion of a new drain remained unsuccessful, we performed a diagnostic bronchoscopy 3 days later with bronchographic confirmation of a BPF in right-sided segment 3 (Fig. 1d, Additional video file 1). The girl was monitored for spontaneous breathing in the ICU.
Intervention: After interdisciplinary consultation, we opted for interventional occlusion of the fistula, applying a vascular occlusion technique. In contrast to endovascular occlusion procedures, a vascular plug requiring thrombus formation inside the device could not be used to achieve complete occlusion. We therefore decided to use detachable large-volume coils, which can be applied via microcatheters (Ruby Coil Penumbra®, Alameda California USA) for the occlusion of cardiovascular malformations [22, 23]. Since these coils allow a high packing density, they offer a high probability of primary airtight occlusion and complete abolishment of air leakage. The bronchoscopic intervention was performed under general anaesthesia starting with bronchographic visualisation of the BPF (contrast media (Ultravist® 400)). A 4 French catheter (Glidecath Terumo®, Tokyo Japan) was advanced into segment 3 as a guiding catheter to allow selective placement of a 2.7 French microcatheter (Progreat Terumo®, Tokyo Japan). Superselective embolization of the fistula was achieved by successive placement and dense packing of 4 large-volume detachable coils (2 mmx1 cm, 3 mmx5 cm and 4 mmx6 cm Ruby soft coils and 3 mmx5 cm Ruby Standard Coil®, Ruby Coil Penumbra®, Alameda California USA). Repeat bronchography revealed complete occlusion of the fistula without evidence of residual leakage (Fig. 2a). Two days later, the drain was removed, and the child was extubated. During follow-up over 4 years, the coil position remained unchanged, the X-ray findings normalized, and the child was clinically asymptomatic (Fig. 2b) with normal lung function both in spirometry and bodyplethysmography. She shows normal total lung capacity and vital capacity, normal oxygen saturation and normal exercise tolerance in daily life. Three supplementary movie files show these diagnostics and procedure in more detail (see Additional files 1, 2 and 3).
Discussion and conclusions
Air leaks due to BPF are associated with high morbidity (up to 57% for resectional surgery or pneumonia) and significant mortality (16–72%) [1, 24,25,26,27,28]. Such leaks persisting longer than 5–7 days [1] are defined as ‘persistent air leaks (PALs)’, specified as the entry of air into the pleural space originating either from central airways (BPF) [1] or from the periphery (alveolo-pleural fistula). For diagnostic confirmation, sequential bronchial blocking or methylene blue staining in the pleura are recommended [29]. In our case, we achieved exact defect localization by endoscopically controlled selective bronchography.
Although a variety of therapeutic options have been published, they have to be adjusted to the origin and size of the fistula. Fistulae developing after surgical resection therapy due to cancer or malformation may be easier to occlude surgically than fistulae developing as a complication of severe pneumonia or empyema. In addition, a fistula of > 8 mm should be primarily closed surgically [28], although endoscopic intervention may be less invasive than a thoracotomy. According to a review of the literature and to the recommendations and guidelines of the American Thoracic Society (ATS, 2001) [30], British Thoracic Society (BTS, 2010) [27] and European Association for Cardio-Thoracic Surgery (EACTS, 2015) [31], the treatment of first choice is a conservative approach with drainage by a chest tube (suction or water seal) and observation [1]. A digital measurement of air leak flow by means of newer electronic chest drainage systems is helpful [1]. In cases of failure of this conservative approach, surgical therapy is recommended. Surgical treatment (open or as VATS) comprises either resection of any bullae, blebs or visible anomalies; coverage of the fistula [32, 33]; or mechanical or chemical pleurodesis [1]. However, in patients with BPF following surgical procedures, endoscopic therapy has been recommended as the treatment of first choice since it has proven superior to resurgery [25]. As discussed above, endoscopic interventional treatment options in adults comprise a variety of procedures, including occluding device implantation and topical administration of sclerosants or sealants. Plugs and valves are large in size and derived from adult medicine and COPD therapy; however, Amplatzer® devices and coils used in paediatric cardiology may be used in older children. Valves have to be removed after healing, can be expectorated by accident and are too large for small children. In our patient, we did not favour the use of topical sclerosant administration due to the risk of accidental malplacement of the sealant in the presence of rather small airways.
With respect to the age and small size of the bronchial anatomy in our patient, we decided on a hitherto unpublished interventional approach of bronchoscopic fistula occlusion by implantation of detachable high-density packing, high-volume coils (Penumbra®). They are relatively small, become progressively softer from their distal to proximal end rather than being of uniform stiffness, exhibit a tight conformational structure and have a more robust stretch-resistance platform. Normally indicated for aneurysms and arterial and venous embolization in the peripheral vasculature, they have proven to be safe for endovascular procedures [22, 34].
These coils can be delivered via microcatheters allowing superselective occlusion of small structures and have been used in paediatric cardiology and neuroradiology. Due to the dense 3D packing of 4 consecutive coils, we were able to achieve immediate airtight occlusion with minimal trauma to the pulmonary tissue, avoiding the requirement of the additional application of fibrin glue or other sealants. Rapid removal of the drain and discharge from the hospital was possible, with uneventful follow-up over a 4-year period. As only 2 subsegments of segment 3 of the right upper lobe had been occluded, and with respect to the Euler-Liljestrand reflex, no VQ mismatch was expected; moreover, callous scarring enabled compensatory enlargement of the resting neighbouring lobe segments.
In summary, we report bronchoscopic superselective occlusion of a BPF using detachable high-density packing large-volume coils as a successful minimally invasive therapeutic intervention in a 2.5-year-old girl. According to our experience, detachable high-density packing microcoils, which can be placed selectively via microcatheters, may represent an attractive alternative for interventional occlusion of BPFs in small children. This minimally invasive therapeutic intervention has advantages compared to surgery due to its minimally invasive nature associated with only minor trauma to the lung tissue. Since the method described here can be performed in adults under local anaesthesia, it could be a therapeutic option for this life-threatening complication in selected patients who are at high risk for surgery under general anaesthesia. Further experience will be necessary to recommend this new method for standard care in the future.
Change history
28 August 2022
Missing Open Access funding information has been added in the Funding Note.
Abbreviations
- ATS:
-
American Thoracic Society
- BPF:
-
Bronchopleural fistula
- BTS:
-
British Thoracic Society
- CT:
-
Computed tomography
- CR:
-
Chest X-ray
- EACTS:
-
European Association of Cardio-Thoracic Surgery
- PAL:
-
Persistent air leak
- VATS:
-
Video-assisted thoracoscopic surgery
References
Lazarus DR, Casal RF. Persistent air leaks: a review with an emphasis on bronchoscopic management. J Thorac Dis. 2017;9:4660–70.
Fruchter O, Kramer MR, Dagan T, Raviv Y, Abdel-Rahman N, Saute M, et al. Endobronchial closure of bronchopleural fistulae using amplatzer devices: our experience and literature review. Chest. 2011;139:682–7.
Travaline JM, McKenna RJ Jr, De GT, Venuta F, Hazelrigg SR, Boomer M, et al. Treatment of persistent pulmonary air leaks using endobronchial valves. Chest. 2009;136:355–60.
How CH, Hsu HH, Chen JS. Chemical pleurodesis for spontaneous pneumothorax. J Formos Med Assoc. 2013;112:749–55.
Takaoka K, Inoue S, Ohira S. Central bronchopleural fistulas closed by bronchoscopic injection of absolute ethanol. Chest. 2002;122:374–8.
Stratakos G, Zuccatosta L, Porfyridis I, Sediari M, Zisis C, Mariatou V, et al. Silver nitrate through flexible bronchoscope in the treatment of bronchopleural fistulae. J Thorac Cardiovasc Surg. 2009;138:603–7.
Lim AL, Kim CH, Hwang YI, Lee CY, Choi JH, Shin T, et al. Bronchoscopic ethanolamine injection therapy in patients with persistent air leak from chest tube drainage. Tuberc Respir Dis (Seoul). 2012;72:441–7.
Martin WR, Siefkin AD, Allen R. Closure of a bronchopleural fistula with bronchoscopic instillation of tetracycline. Chest. 1991;99:1040–2.
Liberman M, Muzikansky A, Wright CD, Wain JC, Donahue DM, Allan JS, et al. Incidence and risk factors of persistent air leak after major pulmonary resection and use of chemical pleurodesis. Ann Thorac Surg. 2010;89:891–7.
Dugan KC, Laxmanan B, Murgu S, Hogarth DK. Management of Persistent air Leaks. Chest. 2017;152:417–23.
Cao G, Kang J, Wang F, Wang H. Intrapleural instillation of autologous blood for persistent air leak in spontaneous pneumothorax in patients with advanced chronic obstructive pulmonary disease. Ann Thorac Surg. 2012;93:1652–7.
Roksvaag H, Skalleberg L, Nordberg C, Solheim K, Høivik B. Endoscopic closure of bronchial fistula. Thorax. 1983;38:696–7.
Wood RE, Lacey SR, Azizkhan RG. Endoscopic management of large, postresection bronchopleural fistulae with methacrylate adhesive (super glue). J Pediatr Surg. 1992;27:201–2.
York EL, Lewall DB, Hirji M, Gelfand ET, Modry DL. Endoscopic diagnosis and treatment of postoperative bronchopleural fistula. Chest. 1990;97:1390–2.
Hollaus PH, Lax F, Janakiev D, Lucciarini P, Katz E, Kreuzer A, et al. Endoscopic treatment of postoperative bronchopleural fistula: experience with 45 cases. Ann Thorac Surg. 1998;66:923–7.
Finch CK, Pittman AL. Use of fibrin glue to treat a persistent pneumothorax with bronchopleural fistula. Am J Health Syst Pharm. 2008;65:322–4.
McCarthy PM, Trastek VF, Bell DG, Buttermann GR, Piehler JM, Payne WS, et al. The effectiveness of fibrin glue sealant for reducing experimental pulmonary ari leak. Ann Thorac Surg. 1988;45:203–5.
Ranu H, Gatheral T, Sheth A, Smith EE, Madden BP. Successful endobronchial seal of surgical bronchopleural fistulas using BioGlue. Ann Thorac Surg. 2009;88:1691–2.
Mehta HJ, Malhotra P, Begnaud A, Penley AM, Jantz MA. Treatment of alveolar-pleural fistula with endobronchial application of synthetic hydrogel. Chest. 2015;147:695–9.
Sprung J, Krasna MJ, Yun A, Thomas P, Bourke DL. Treatment of a bronchopleural fistula with a Fogarty catheter and oxidized regenerated cellulose (surgicel). Chest. 1994;105:1879–81.
Watanabe S, Watanabe T, Urayama H. Endobronchial occlusion method of bronchopleural fistula with metallic coils and glue. Thorac Cardiovasc Surg. 2003;51:106–8.
Hofbeck M, Sieverding L, Groezinger G, Kagan KO. Coil occlusion of a congenital left ventricular aneurysm in a newborn. Catheter Cardiovasc Interv. 2020;96:389–92.
Hummel J, Stiller B, Kroll J, Grohmann J. Primary coiling of the left ventricle in Hypoplastic left heart with Ventriculo-coronary connections. Ann Thorac Surg. 2017;103:e559.
Salmon CJ, Ponn RB, Westcott JL. Endobronchial vascular occlusion coils for control of a large parenchymal bronchopleural fistula. Chest. 1990;98:233–4.
Lois M, Noppen M. Bronchopleural fistulas: an overview of the problem with special focus on endoscopic management. Chest. 2005;128:3955–65.
Pierson DJ, Horton CA, Bates PW. Persistent bronchopleural air leak during mechanical ventilation. A review of 39 cases. Chest. 1986;90:321–3.
MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(Suppl 2):ii18–31. https://doi.org/10.1136/thx.2010.136986.:ii18-ii31.
Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med. 2000;342:868–74.
Sakata KK, Reisenauer JS, Kern RM, Mullon JJ. Persistent air leak - review. Respir Med. 2018;137:213–8. https://doi.org/10.1016/j.rmed.2018.03.017 Epub@2018 Mar 14.:213-218.
Boyer D, Thomson CC, Cohen R, Rao D, Dell S, Rayment J, et al. ATS Core curriculum 2016: part III. Pediatric pulmonary medicine. Ann Am Thorac Soc. 2016;13:955–66.
Scarci M, Abah U, Solli P, Page A, Waller D, Van Schil P, et al. EACTS expert consensus statement for surgical management of pleural empyema. Eur J Cardiothorac Surg. 2015;48:642–53.
Jester I, Nijran A, Singh M, Parikh DH. Surgical management of bronchopleural fistula in pediatric empyema and necrotizing pneumonia: efficacy of the serratus anterior muscle digitation flap. J Pediatr Surg. 2012;47:1358–62.
Chittithavorn V, Duangpakdee P, Rergkliang C, Preukprasert N. A novel approach for the treatment of post-pneumonectomy bronchopleural fistula by using an autologous corticocancellous bone graft. J Thorac Dis. 2018;10:4453–63.
Stapleton CJ, Torok CM, Patel AB. Early experience with the penumbra SMART coil in the endovascular treatment of intracranial aneurysms: safety and efficacy. Interv Neuroradiol. 2016;22:654–8.
Acknowledgements
We acknowledge support by Open Access Publishing Fund of University of Tuebingen.
Funding
No funding was obtained in regard to this case report. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
WB and LS planned and performed the intervention and drafted the manuscript. SW, JS and MH revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No further Ethics approvement necessary in this case report.
Consent for publication
Written informed consent to publish this case (including publication of images and videos) was obtained from the parents.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Additional movie file 1. Bronchography showing BPF in right sided segment 3
Additional file 2: Additional movie file 2. Procedure of coiling the BPF
Additional file 3: Additional movie file 3. Control bronchography after interventional coiling
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baden, W., Hofbeck, M., Warmann, S.W. et al. Interventional closure of a bronchopleural fistula in a 2 year old child with detachable coils. BMC Pediatr 22, 250 (2022). https://doi.org/10.1186/s12887-022-03298-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03298-y