Abstract
Background
Children with congenital heart disease are at increased risk of malnutrition. The aim of this study was to describe the prevalence of wasting, underweight and stunting among children with congenital heart disease attending Mulago National Referral Hospital, Uganda.
Methods
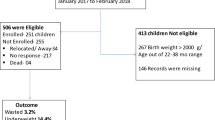
A cross-sectional study among 194 children aged 0–15 years was conducted between August 2013 and March 2014. Anthropometric measurements and clinical assessments were carried out on all children. Anthropometric z-scores based on WHO 2007 reference ranges were generated for each child. Weight-for-height z-scores were generated for children 0–5 years, weight-for-age z-scores for children 0–10 years, and height-for-age and BMI-for-age z-scores for all children. Risk factors associated with malnutrition were determined by Poisson regression.
Results
One hundred and forty five (74.7%) children were aged 0–5 years; and 111 of 194 (57.2%) were female. Forty five of 145 (31.5%) children aged 0–5 years were wasted; 77 of 181 (42.5%) children aged 0–10 years were underweight; 88 of 194 (45.4%) children were stunted; and 53 of 194 (27.3%) children were thin (BMI for age z score < −2). Moderate to severe anaemia (RR 1.11, 95% CI: 1.01–1.22) and moderate to severe heart failure (RR 1.24, 95% CI: 1.13–1.36) were associated with wasting and underweight respectively. Stunting was associated with moderate to severe heart failure (RR 1.11, 95% CI: 1.01–1.21) while thinness was associated with moderate to severe heart failure (RR 1.12, 95% CI: 1.04–1.21) and moderate to severe anaemia (RR 1.15, 95% CI: 1.06–1.25).
Conclusion
Malnutrition is common in children with congenital heart disease, and is associated with anaemia and heart failure. There is need to integrate strategies to identify and manage malnutrition during the care of children with congenital heart disease.
Similar content being viewed by others
Background
Children with congenital heart disease (CHD) are at an increased risk for wasting, underweight and stunting [1–3]. Malnutrition among these children increases their risk to infections and the risk of death even after corrective surgery [4]. In addition, malnutrition leads to poor growth in children which is associated with delayed mental development, poor school performance and reduced intellectual capacity [4, 5]. These outcomes significantly impair economic productivity in adult life.
Risk factors for malnutrition among children with CHD include heart failure, cyanosis, multiple heart defects, delayed corrective surgery, anaemia and pulmonary hypertension [1, 3, 6]. Furthermore, in children with CHD, poor nutrition is also attributed to inadequate nutritional intake due to feeding difficulties and the increased energy expenditure among these children [7]. In developing countries, corrective surgery for congenital heart defects is delayed and this increases the likelihood of the children developing malnutrition [8].
In Uganda, childhood malnutrition is a public health problem with 33% of children aged under 5 years being stunted, 14% underweight and 5% wasted [9]. Thus malnutrition in children with CHD in Uganda is likely to be common and of multi-factorial origin. A clear understanding of the complex nature of malnutrition in children with CHD is essential to design strategies that will improve outcomes in these children. This study was therefore conducted to determine the prevalence of malnutrition in children with congenital heart disease and the factors associated with wasting, underweight and stunting.
Methods
Study setting and population
The study was carried out at Mulago National Referral Hospital and Uganda Heart Institute, Kampala, from August 2013 to March 2014. Participants were 194 children aged 0–15years with congenital heart disease diagnosed by echocardiography. They were part of a previous study which assessed arrhythmias among children; and the details of the methods and the different heart diseases for each child are described elsewhere [10].
Variables
Data were collected on socio-demographic characteristics and clinical assessments of the children. Weight was measured using a SECA® weighing scale and readings were recorded to the nearest 0.1 kg. Height was measured using a stadiometer (measuring board) and readings recorded to the nearest 0.5 cm. Heights for children below 2 years was taken when the children were lying down while older children had their heights taken when standing. We used the World Health Organisation (WHO) z-scores to classify the nutritional status of the children [11]. A child was classified as underweight if the weight-for-age WHO z-score was < −2 SD, wasted if weight-for-height WHO z-score was < −2 SD (for children aged 0–5 years), thin if BMI-for-age WHO z-score was < −2 SD and stunted if height-for-age z-score was < −2 SD.
All children were assessed for heart failure and the severity of heart failure was graded using the modified Ross score; children were grouped into two categories based on a Ross score 0–6 (mild or no heart failure) and a Ross score >6 (moderate to severe heart failure) [12, 13].
Hemoglobin levels of the children were recorded from complete blood counts that were performed using Celltac E MEK-7222 automatic hematology analyzer. Grading of the severity of anaemia (mild, moderate and severe) was done according to WHO age specific reference ranges [14]. An HIV test was performed on each child using Alere™ HIV-1/2 Determine® as a screen, followed by STAT-PAK® HIV-1/2; the Uni-Gold™ Recombigen® for confirmation. HIV infection in children aged under 18 months who were HIV positive by serology test was confirmed using the HIV DNA PCR test.
Data analysis
Age was categorized into three groups: 0–5, 6–10 and 11–15 years. The demographic and clinical characteristics were stratified by age. Continuous anthropometric measures were stratified using a z-score of < −2 as a cut-off for malnutrition. Overall frequencies were determined for all categorical measures followed by stratification by age. Medians and interquartile ranges of the anthropometric measures were determined overall and by age.
Poisson regression with robust error variances was used to determine factors associated with malnutrition both at the univariate and multivariate level. All the variables with at least one factor having a p-value < 0.2 at the univariate level were considered for entry into the multivariate model controlling for age. Statistical analysis was performed using SAS/STAT software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Demographic characteristics of participants
One hundred and forty five of 194 children (74.7%) were aged 0–5 years and 111 of 194 (57.2%) were female. One hundred and thirty eight of 194 children (71.1%) had acyanotic heart disease but only 4 (2.1%) had surgically corrected heart defects (Table 1). Two children (1%) were HIV positive.
Proportion of children wasted, underweight and stunted
Overall, 45 of 145 (31.5%) children aged 0–5 years had weight-for-height z-score < −2 (wasted). The median weight-for-height z-score among these children was −0.89 (IQR: −2.46,-0.10). Of the children aged 0–10 years, 77 of 181 (42.5%) had weight-for-age z-scores < −2 (underweight) and the median weight-for-age z-score among these children was −1.69 (IQR-3.07,-0.69). Fifty three of 194 children (27.3%) had a BMI-for-age z-score < −2 (thin) with a median BMI-for-age z-score of −0.72 (IQR −2.21, 0.17). The number of stunted children was 88 out of 194 (45.4%) with a median height-for-age z-score of −1.67 (IQR −3.21,-0.51). These findings are summarised in Table 2.
Factors associated with malnutrition
Among children under 5 years, children with moderate/severe anaemia (RR: 1.11, 95% CI: 1.01–1.22) had a higher risk of being wasted after controlling for age and heart failure (Table 3). Among children aged 0–10 years, moderate/severe heart failure was associated with being underweight after adjusting for age and anaemia (RR: 1.24, 95% CI: 1.13–1.36) (Table 4). After controlling for age and anaemia, children with moderate/severe heart failure had a higher risk of stunting (RR 1.11, 95% CI 1.01–1.21) (Table 5). After controlling for age, children with moderate/severe heart failure (RR: 1.12, 95% CI: 1.04–1.21) and moderate/severe anaemia (RR: 1.15, 95% CI: 1.06–1.25) had a higher risk of thinness (Table 6).
Discussion
Our study showed that malnutrition in children with congenital heart disease is high. The prevalence of wasting, underweight, thinness and stunting was 31.5%, 42.5%, 27.3% and 45.4% respectively. Malnutrition was more frequent among children with moderate to severe heart failure and moderate to severe anaemia.
The prevalence of wasting among children aged under 5 years with congenital heart disease in our study was higher than the 7.5% global prevalence of wasting in children under 5 years [15]. In addition, our findings show that children with congenital heart disease are six times more likely to be wasted compared to their counterparts in Uganda [9]. Our study found a high proportion of underweight, stunted and thin children relative to those previously described globally [15, 16] and in Uganda [9, 17]. Other studies have also demonstrated that children with congenital heart disease are at higher risk of malnutrition compared to those without heart disease [1, 18, 19].
Okoromah and colleagues reported prevalence of wasting, stunting and underweight of 41.1%, 28.8% and 20.5% respectively in children with congenital heart disease attending an outpatient tertiary hospital in Nigeria [1]. Although they noted a higher prevalence of wasting, and the proportions of stunted and underweight children were lower than those seen in our study. Furthermore, in comparison to our study, a higher prevalence of malnutrition among children with congenital heart disease was described in India; wasting (55.9%) and underweight (59%) [20]. Lower prevalence of wasting (23.8%) and underweight (14.3%) was reported in Egypt among children under 6 years of age [21]. These studies indicate that the prevalence of malnutrition is high in children with congenital heart disease in various countries. However, heterogeneity exists from country to country implying differences in risk factors for malnutrition among children, in the different settings.
Similar to our findings, various studies have reported an association between malnutrition and heart failure in children with congenital heart disease [1, 20, 21] which is attributed to increased metabolic needs of these children yet they have low energy intake due to their inability to tolerate a high volume of feeds [7, 22].
Anaemia has also been reported to be associated with malnutrition in children with congenital heart disease [1, 21]. This is similar to our findings where children with moderate or severe anaemia were more likely to be wasted and thin. Children with malnutrition commonly have anaemia which is attributed to bone marrow hypoplasia, iron, vitamin B12, vitamin A and folate deficiency [23, 24]. Even though we did not assess for these causes of anaemia in our study, we think that these could explain the association between anaemia and malnutrition among children with congenital heart disease noted from our study.
Delayed time to surgical correction of the heart defects has been associated with malnutrition among the children with congenital heart disease [1, 3, 20]. In our study, only 4 children had received surgical correction of their heart defects, and therefore we could not assess this relationship due to small numbers. There was no significant association between cyanotic heart disease and malnutrition, a finding that is contrary to other studies. It may be that a different outcome would have been achieved by a larger sample size.
Although, Uganda has a number of policies and guidelines on promotion of nutrition among children, there is limited emphasis on congenital heart diseases as an underlying risk factor for malnutrition [25, 26]. Hence there is a need to develop interventions such as early surgical repair for heart defects and institutionalisation of other measures to prevent and manage malnutrition in these children.
Limitations
We did not assess other factors that are known to contribute to malnutrition in these children with congenital heart disease such as genetic disorders [27], pulmonary hypertension [3] and social economic status of the households. However, socio-economic status is better assessed in community studies than hospital based studies.
Children with cyanotic congenital heart disease tend to have polycythemia resulting in higher haemoglobin levels [28]. In our study, we used the WHO age specific reference haemoglobin levels to define anaemia [14]. In children with cyanotic heart disease, these reference ranges may not be the best markers for anaemia. However, there are no standardised haemoglobin reference levels for these children and the variations in their haemoglobin levels are not uniform. The sample size of the children in our study is also relatively small but this may not have significantly affected our results.
Conclusion
Children with congenital heart disease had high prevalence rates of wasting, underweight, stunting and thinness. Wasting was associated with moderate to severe anaemia. Stunting and underweight were associated with moderate to severe heart failure, while thinness was associated with moderate to severe heart failure and moderate to severe anaemia. With these high rates of malnutrition in children with congenital heart disease, there is need to integrate strategies to identify and manage malnutrition during their care.
Abbreviations
- BMIZ:
-
Body mass index-for-age z score
- CHD:
-
Congenital heart disease
- HAZ:
-
Height-for-age z score
- WAZ:
-
Weight-for-age z score
- WHO:
-
World Health Organisation
- WHZ:
-
Weight-for-height z score
References
Okoromah CA, Ekure EN, Lesi FE, Okunowo WO, Tijani BO, Okeiyi JC. Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case-control observational study. Arch Dis Child. 2011;96(4):354–60.
Mitchell I, Logan R, Pollock J, Jamieson M. Nutritional status of children with congenital heart disease. Br Heart J. 1995;73(3):277–83.
Varan B, Tokel K, Yilmaz G. Malnutrition and growth failure in cyanotic and acyanotic congenital heart disease with and without pulmonary hypertension. Arch Dis Child. 1999;81(1):49–52.
Medoff-Cooper B, Ravishankar C. Nutrition and growth in congenital heart disease: a challenge in children. Curr Opin Cardiol. 2013;28(2):122–9.
Grantham-McGregor S, Baker-Henningham H. Review of the evidence linking protein and energy to mental development. Public Health Nutr. 2005;8(7a):1191–201.
De Staebel O. Malnutrition in Belgian children with congenital heart disease on admission to hospital. J Clin Nurs. 2000;9(5):784–91.
Menon G, Poskitt E. Why does congenital heart disease cause failure to thrive? Arch Dis Child. 1985;60(12):1134–9.
Vaidyanathan B, Roth SJ, Rao SG, Gauvreau K, Shivaprakasha K, Kumar RK. Outcome of ventricular septal defect repair in a developing country. J Pediatr. 2002;140(6):736–41.
Uganda Bureau of Statistics (UBOS) and ICF International Inc. Uganda Demographic and Health Survey 2011. Kampala: UBOS and Calverton, Maryland: ICF International Inc; 2012.
Batte A, Lwabi P, Lubega S, Kiguli S, Nabatte V, Karamagi C. Prevalence of arrhythmias among children below 15 years of age with congenital heart diseases attending Mulago National Referral Hospital, Uganda. BMC Cardiovasc Disord. 2016;16(1):1.
World Health Organisation. Anthropometric reference data for international use. http://www.who.int/childgrowth/publications/deonis_habicht_1996/en/. Accessed 18 Jul 2016.
Ross RD, Bollinger RO, Pinsky WW. Grading the severity of congestive heart failure in infants. Pediatr Cardiol. 1992;13(2):72–5.
Reithmann C, Reber D, Kozlik-Feldmann R, Netz H, Pilz G, Welz A, Werdan K. A post-receptor defect of adenylyl cyclase in severely failing myocardium from children with congenital heart disease. Eur J Pharmacol. 1997;330(1):79–86.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva: Vitamin and Mineral Nutrition Information System; 2011.
International Food Policy Research Institute. Global Nutrition Report 2016. Washington, DC: From Promise to Impact: Ending Malnutrition by 2030; 2016.
Manyanga T, El-Sayed H, Doku DT, Randall JR. The prevalence of underweight, overweight, obesity and associated risk factors among school-going adolescents in seven African countries. BMC Public Health. 2014;14(1):1.
Lwanga F, Kirunda BE, Orach CG. Intestinal helminth infections and nutritional status of children attending primary schools in Wakiso District, Central Uganda. Int J Environ Res Public Health. 2012;9(8):2910–21.
Chen CW, Li CY, Wang JK. Growth and development of children with congenital heart disease. J Adv Nurs. 2004;47(3):260–9.
Daymont C, Neal A, Prosnitz A, Cohen MS. Growth in children with congenital heart disease. Pediatrics. 2013;131(1):e236–42.
Vaidyanathan B, Nair SB, Sundaram KR, Babu UK, Shivaprakasha K, Rao SG, Kumar RK. Malnutrition in children with congenital heart disease (CHD) determinants and short term impact of corrective intervention. Indian Pediatr. 2008;45(7):541–6.
Hassan BA, Albanna EA, Morsy SM, Siam AG, Al Shafie MM, Elsaadany HF, Sherbiny HS, Shehab M, Grollmuss O. Nutritional status in children with un-operated congenital heart disease: an Egyptian center experience. Front Pediatr. 2015;2015:3.
Rogers EJ, Gilbertson HR, Heine RG, Henning R. Barriers to adequate nutrition in critically ill children. Nutrition. 2003;19(10):865–8.
Özkale M, Sipahi T. Hematologic and bone marrow changes in children with protein-energy malnutrition. Pediatr Hematol Oncol. 2014;31(4):349–58.
Müller O, Krawinkel M. Malnutrition and health in developing countries. Can Med Assoc J. 2005;173(3):279–86.
National Planning Authority. Uganda Nutrition Action Plan 2011–2016. Kampala: National Planning Authority; 2011.
National Planning Authority. National nutrition planning guidelines for Uganda. Kampala: National Planning Authority; 2015.
Knirsch W, Zingg W, Bernet V, Balmer C, Dimitropoulos A, Prêtre R, Bauersfeld U, Latal B. Determinants of body weight gain and association with neurodevelopmental outcome in infants operated for congenital heart disease. Interact Cardiovasc Thorac Surg. 2010;10(3):377–82.
Territo MC, Rosove MH. Cyanotic congenital heart disease: hematologic management. J Am Coll Cardiol. 1991;18(2):320–2.
Acknowledgements
We acknowledge the support and input from the staff and administration of Mulago Hospital, Uganda Heart Institute and Child Health and Development Center, Makerere University. We are also grateful to the patients and caretakers who participated in this study.
Funding
Research reported in this publication was supported by the Fogarty International Center, the National Heart Lung and Blood Institute, and the Common Fund of the National Institutes of Health under Award Number 5R24 TW008861. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Availability of data and materials
All relevant supporting data on which conclusions of this article have been drawn has been included within the main body of this manuscript.
Authors’ contribution
AB, PL, SL, SK, VN and CK participated in the design of the study. AB supervised patients’ enrolment and coordinated the study. AB, PL, SL, SK, KO, LC, VN and CK participated in data analysis, interpretation of results and writing of the manuscript. All authors read and approved the final manuscript.
Authors’ information
Anthony Batte, MBChB, Mmed (Pediatrics), is a Lecturer and Paediatric Nephrologist at Child Health and Development Centre, Makerere University, Uganda. Peter Lwabi, MBChB, Mmed (Pediatrics), Dip Cardiology, is a Pediatric Cardiologist at Uganda Heart Institute. Sulaiman Lubega - MBChB, MMed (Pediatrics), Dip Cardiology, is a Pediatric Cardiologist at Uganda Heart Institute. Sarah Kiguli - MBChB, Mmed (Pediatrics), MHPE is a Professor of Pediatrics and Child Health Makerere University. Kennedy Otwombe B.Ed (Science), M.Sc. (Stats), is a Biostatistician at the Perinatal HIV Research Unit, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa. Lucy Chimoyi B.Sc (Biochem), M.Sc (Env Sci), M.Sc. (Epid& Biostat), is a Researcher in the Epidemiology Unit at The Aurum Institute, Johannesburg, South Africa. Violette Nabatte - MBChB, M.med (Pediatrics) is a Pediatrician at Nakaseke Hospital, Uganda. Charles Karamagi, MBChB, Mmed (Pediatrics), PhD is an Associate Professor of Pediatrics and Child health also working with the Clinical Epidemiology Makerere University.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by Makerere University School of Medicine Research and Ethics Committee (SOMREC) and the Uganda National Council for Science and Technology. All caretakers of children provided written informed consent before participation in the study. Furthermore, children aged 8 years and above provided assent before participating in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Batte, A., Lwabi, P., Lubega, S. et al. Wasting, underweight and stunting among children with congenital heart disease presenting at Mulago hospital, Uganda. BMC Pediatr 17, 10 (2017). https://doi.org/10.1186/s12887-017-0779-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-017-0779-y