Abstract
Objective
Every year, an estimated 20 million babies are born with low birthweight and this number is increasing globally. Survivors are at risk of lifelong morbidities like undernutrition. We assessed the growth and nutritional status for children born with low birthweight at Mulago Hospital, Uganda.
Methods
We conducted a cross sectional study to describe the nutritional status of children aged between 22 and 38 months and born weighing ≤ 2000 g. Anthropometric measurements; weight for height, height for age and weight for age z-scores were generated based on the World Health Organization standards to define wasting, stunting and underweight respectively. Data was collected using a structured questionnaire and analysis was done using STATA version 14.
Results
Of the 251 children, 129 (51.4%) were male, mean age was 29.7 months SD 4.5) and maternal mean age was 29.9 (SD 5.3). A total of 101(40.2%) had normal nutritional status. The prevalence of wasting, underweight and stunting were: 8 (3.2%), 36 (14.4%) and 106 (42.2%) respectively.
Conclusion
Six of ten children born with low birthweight were at risk of undernutrition in early childhood: underweight and stunting were higher than the national prevalence. Targeted interventions are needed for children with very low birth weight.
Similar content being viewed by others
Background
Low birthweight is defined by the World Health organization (WHO) as weight at birth less than 2500 g. It is estimated 15–20% of all births globally are low birthweight (LBW), accounting for 20 million births annually [1]. Estimates of LBW vary across regions and within countries although majority occur in low- and middle-income countries (LMIC). More than 60% babies with LBW are born in Asia and sub Saharan Africa, with rates of 28% and 13% respectively [2]. Data on LBW remain limited in many LMICs as many births occur in homes or in facilities where birthweights are not taken or records are unreliable [3].
LBW is complex and may occur due to restricted fetal growth or preterm birth (born before 37 weeks of gestation), and/ or an overlap between the two [4]. In the current study, we focus on the birthweight categorized as low birthweight less than 2500 g, very low birthweight (VLBW) less than 1500 g and extreme low birthweight (ELBW) less than 1000 g. LBW is a significant public health issue associated with short- and long-term health consequences [3, 5, 6]. Health complications increase with reducing birthweight. Majority of the heavier babies (> 1500 g) will survive with minimal healthcare or no need for neonatal intensive care [3, 7]. LBW is a predictor of prenatal mortality and morbidity and has been found to increase risk for noncommunicable diseases such as diabetes, cardiovascular diseases and malnutrition among survivors extending to early childhood and adulthood [5, 8, 9].
Children born with LBW are at risk of growth and nutritional deficits. Regular assessment through follow-up and appropriate interventions to improve their outcome throughout their life course is crucial [10,11,12]. At 2–3 years of age, children born with LBW are expected to have caught-up on the growth curve with their normal birthweight counterparts [13, 14]. However, some studies have reported that at this age some children have nutritional deficits which may persists later in life [15].
Undernutrition is a known global burden affecting 165 million children below 5 years of age [16, 17] and those born with LBW are at higher risk. Stunting, wasting and underweight are established indicators for the nutritional status of infants and children, indicating their overall health and growth status. Cut-off references in public health are shown in Table 1. Stunting expressed as height-for-age is a chronic marker of nutritional deficit. Underweight expressed as weight-for-age and wasting as weight-for-height are acute markers of nutritional deficit [18]. Normal growth is defined by anthropometric measurements for age and sex with weight and length/height z-scores > -2 SDs of the reference population [19, 20].
There is scarcity of data on early childhood nutritional status of children born with LBW in our setting. Despite the high prevalence of LBW in Uganda [21], minimal efforts exist at national level towards nutritional and growth monitoring beyond the neonatal period for this high risk population. We sought to evaluate the growth and nutritional status for children aged 22 to 38 months born with LBW in a low resource setting. The study provided important information on early childhood nutritional status for children born with LBW at Mulago hospital national referral in Kampala, Uganda.
Methods
We conducted a cross sectional study for children born with LBW at the follow-up clinic at Mulago hospital, Kampala. Mulago hospital is also the training institution for Makerere University, College of Health Sciences. It serves mainly the urban and peri-urban population of Kampala the capital city and those referred from other facilities around the country. The clinic is run twice a week for children discharged from the neonatal unit whose birthweight was < 2500 g and /or born < 37 weeks of gestation. The follow-up schedule for the infants is as follows: they are seen in the clinic every fortnight until they gain a weight of ≥ 2500 g, then the interval for follow-up is every two to three months until 18 months of corrected age or two years of life. Services at the follow-up clinic are free of charge and include nutritional education, growth and development assessment of the infants. These are provided by a pediatrician, resident doctor and a nurse. On average, 30 infants are seen every week although nearly 300 neonates are admitted to the neonatal unit every month. Less than 50% of children attended the follow-up clinic for longer than a year (2016 hospital records).
From November 2019 to February 2020, 251 children whose chronological age was 22–38 months at the time of the study, and had birthweight ≤ 2000 g (they are most likely to be preterm with more health problems) were included. Exclusion criteria were those with congenital anomalies and those hospitalized at the time of the study. Participants were identified from the pediatric outpatient/clinic records for those who ever attended between January 2017 to February 2018. A list of 506 eligible children was made, summarized in the flow chart, Fig. 1. We consecutively called up every caretaker when the initial method of calling every second mother did not yield our desired sample size. There was no response to some of the telephone calls made to the caretakers after three attempts. There were also some incomplete or wrong telephone numbers, and other numbers were out of service at the time of the study. A few caretakers/mothers were not able to come back to the clinic despite responding to our call.
Data collection and study measurements
At enrolment, research assistants (nurses) obtained both infant and maternal demographics (age, sex, birth weight and socioeconomic characteristics). Other data collected included: mode and type of delivery, estimated distance from hospital, duration in hospital, duration of exclusive breastfeeding and duration in the follow up clinic. Data was collected using a structured questionnaire from the patients’ clinic records, immunization cards and discharge forms.
Anthropometric measurements: weight and height/length were taken following World Health Organizations (WHO) standard procedures [22]. The weight was taken using a digital portable SECA® weighing scale (Seca 813, Hamburg, Germany) corrected to the nearest 100 g, with the child wearing light clothing and bare feet.
Height/Length was measured using an infant length board (Infant/Child Shorr-Board®, Maryland, USA). Length was measured for children less than two years of age (i.e. up to and including 23 months) while in supine position. Mid-arm upper circumference was taken using color coded tapes (Child 11.5 red/pac-50, UNICEF), both to the nearest 1 mm. Triple measurement for weight, length/height and MUAC were taken and an average obtained.
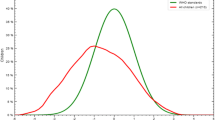
Anthropometric z-scores for weight-for-height/length (WHZ), weight-for-age (WAZ) and height/length-for-age (HAZ) were computed using WHO Anthro version 3.2.2 [20]. Mother’s weight and height were also obtained and the body mass index (BMI) was calculated by dividing the weight in kilograms by the height in meters squared.
Analysis and data management
Data was analyzed using STATA version 14 statistical software (StataCorp. 2017 College Station, TX: StataCorp LLC). The WHO Anthropometrics software was used to convert height, weight and age measurements to height-for-age z-scores (HAZ), weight-for-height z-scores (WHZ) and weight-for-age z-scores (WAZ) which were used to classify stunting, wasting and underweight respectively when z-scores were less than minus 2 SD. The presence of stunting, underweight and wasting among the children were performed using the WHO classification, Table 1, for assessing severity of malnutrition by prevalence ranges among children under-5 years of age [20]. We generated frequencies and percentages of children stunted, wasted and underweight.
Results
Baseline characteristics of the children and their mothers/caretakers
We enrolled 251 children mean age was 29.7 months (SD 4.5) and 51.4% were male. Most of the participants were born by spontaneous vaginal delivery 177 (70.5%) and majority were singletons 179 (71.3%). There were two sets of triplets while the other multiple births were twins. Children with birth weight ≤ 1500gm were 104 (41.6%) and those > 1500 were 146 (58.4%). The median duration of hospital stay post- delivery was 12 days (IQR 7–18). The anthropometric measurements for 236 mothers were included for analysis because 15 children were accompanied by other caretakers (10 fathers, 2 grandparents and one aunt). The summary of the baseline characteristics for the children and their mothers/caretakers are summarized in Table 2. Most mothers were in the informal type of employment, few had attained college or skilled training to translate into formal employment due to the high school dropout.
Growth and nutrition status of the children
Of the children studied, 101 (40.2%) had normal anthropometric measurements for their age and sex based on the reference population [20]. The prevalence for wasting (weight for height z-score <-2SD) was 8 (3.2%), underweight (weight for age z-score <-2 SD) 36 (14.4%) and the prevalence of stunting (height for age z-score <-2) was 106 (42.2%). There were more boys stunted, 64 out of 106 participants compared to girls (p = 0.001). The relationship of child and maternal characteristics with underweight and stunting are summarized in Tables 3, 4, 5 and 6. None of the children reported a recent acute illness (history within two weeks).
Discussion
We sought to establish the growth and nutritional status for children born with LBW at Mulago Hospital, Uganda. From our study, 101 (40.1%) of the participants had normal growth for their age while the rest of the children had undernutrition. The prevalence of stunting was 42.2% and underweight 14.4% and relatively low levels of wasting 3.2%.
Less than half of our participants had normal growth status although children born with LBW are expected to catch-up on growth as those born with appropriate birthweight at 2–3 years of life. This finding was not surprising because we studied a high-risk population. Both prematurity and low birthweight are negatively correlated to postnatal growth [23]. Secondly, undernutrition is a significant public health burden in children under-five in resource limited settings [16]. Our findings were comparable to results of the general population both globally and locally where stunting was highest among the under-fives [16, 17, 24], although these were not limited to children born with LBW. The prevalence of childhood undernutrition in the present study was higher than the country prevalence of 29% and 14.4% for stunting and underweight respectively in the recent Uganda demographic and Health Survey. Wasting was slightly lower, at 3.2% of the study participants versus 4% in the general population of under-fives [24]. We focused on early childhood because it is an important preschool period and growth impacts on learning [9, 16]. Also, the anthropometric parameters at two years can fairly predict the growth outcomes later in life [15].
In our study, 61% of the boys were stunted compared to 39% of the girls. This was documented by Zhihui et al. in several LMICs [25], although further studies are needed to evaluate the mechanism in which sex may contribute to stunting. Furthermore, there were more young mothers with stunted children compared to older mothers also shown in other studies [26, 27]. It is assumed that older mothers are knowledgeable in aspects of child care compared to young and teenage mothers [26] leading to better outcome of their children. The mothers with short stature had stunted children and this could be attributed to genetic and environmental factors [28]. Studies have demonstrated mothers with short stature or those born with low birthweight were more likely to give birth to children with the same features [15, 25]. Even though factors such as maternal education wealth quintile and maternal BMI have been described to be associated with stunting [24, 25], our study did not show the same relationship. Other factors like maternal illness e.g. diabetes, hypertension or malnutrition have been shown to affect the child’s growth. In the current study only one mother was found to have underweight while thirty-four mothers had pregnancy induced hypertension, no other chronic illness was reported.
There were more VLBW infants with underweight than those with LBW or who weighed > 1500 g. This may be explained by the difficulties encountered in feeding VLBW infants majority of whom are preterm babies, thus contributing to underweight in early childhood [29, 30]. Fortification of breastmilk and use of total parental nutrition when the LBW babies need nutritional support the most are not routinely practiced in our setting. The infants who stayed longer in hospital were likely to have underweight later in life. This could be an indicator of difficult in feeding or generally ill-health which may hinder adequate feeding and growth. Only 3.2% of our study participants were wasted as compared to the 4% in the general population [24]. Wasting is an indicator of acute illness and we did not identify children in whom recent acute illness was reported and this probably would explain the low prevalence.
Our study findings show that undernutrition is higher in this at-risk population and growth monitoring should extend to childhood and beyond. Child growth and nutritional status may be strongly linked to fetal life suggesting a need for interventional focus on nutrition during pregnancy and early childhood [15]. To end all forms of malnutrition by 2030: Sustainable Development Goal 2 [31], a life-course approach of nutritional interventions are needed to break the vicious cycle of health problems related to undernutrition such as LBW. These will in turn lead to child survival, educational achievements and overall well- being later in life. Secondly, collection and analysis of long-term data in former LBW children linked to nutritional strategies and growth parameters are strongly recommended in our setting. Although pre-pregnancy and natal nutritional status was not assessed in our study, they have been linked to growth failures in early childhood in other studies [23, 28]. It is therefore important to mind the mother’s nutritional status from pre-conception throughout pregnancy [15, 16].
The strength of this study was the predominant mode of feeding was exclusive breastfeeding with no modification for all the participants. The results are therefore generalizable to settings where fortification of preterm feeds is not readily available. There is limited literature on the topic in our setting, our study provides additional evidence to guide interventions aimed at improving outcome children born with LBW. The limitations of a cross-sectional design were data not reflecting changes in growth of individual children overtime and inferring cause of LBW and undernutrition among the participants. This was a single center study, a national referral hospital with variations in the clients served. The fairly small sample size affected the power to analyze for association of LBW and undernutrition. Nevertheless, the results clearly indicate a need for rigorous growth monitoring for children born LBW beyond the neonatal period.
Conclusion
Six of every ten children born with LBW are at risk of undernutrition in early childhood: underweight and stunting were highly prevalent compared to the national prevalence. Targeted interventions are specifically needed for children born with very low birthweight, males and those requiring long postnatal hospitalization.
Data Availability
All data and materials supporting the conclusions of this article are included within the manuscript. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HAZ:
-
Height for-age z-scores
- LBW:
-
Low birth weight
- LMICs:
-
Low- and Middle-income Countries
- WAZ:
-
Weight-for-age z-scores
- WHZ:
-
Weight-for-height z-scores
- WHO:
-
World Health Organization
References
UNICEF. WHO Low birthweight. estimates 2019. https://www.data.unicef.org/topic/nutrition/low-birthweight
Wardlaw TM. Low birthweight: Country, regional and global estimates. Unicef; 2004.
Kerber KJ, de Graft-Johnson, Lawn JE, et al. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. The Lancet. 2007;370(9595):1358–69.
Blencowe H, Cousens S, Oestergaard M, et al. National, regional and worldwide estimates of preterm birth rates in the year 2010 with time trends for selected countries since 1990: a systemic analysis and implications. Lancet. 2012;379:2162–72.
Liu L, Johnson H, Cousens S, et al. Global, regional and national causes of child mortality in 2000–2013, with projections to inform post-2015 priorities: an updated systematic analysis. The Lancet. 2015;385(9966):430–40.
Pinto F, Fernades E, Virella D, et al. Born Preterm: a public health issue. Portuguese J Public Health. 2019;37(1):38–49.
WHO U, UNFPA, UNICEF, Women UN, The World Bank Group. Survive, Thrive, Transform. Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030). 2018 monitoring report: Current status and strategic priorities. 2018.
Lawn JE, Gravett MG, Nunes TM, et al. Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Preg Childbirth. 2010;10(Suppl 1):1–S.
Ntenda PAM. Association of low birth weight with undernutrition in preschool-aged children in Malawi. J Nutr. 2019;18(1):1–15.
Abdallah Y, Namiiro F, Nankunda J, et al. Growth of preterm very low birth weight infants discharged with weight of less than 1500grams. BMC Pediatr. 2021;21(1):145.
Zoleko-Manego R, Mischlinger J, Dejon-Agobé JC, et al. Birth weight, growth, nutritional status and mortality of infants from Lambaréné and Fougamou in Gabon in their first year of life. PLoS ONE. 2021;16(2):e0246694.
Ho LY. Follow-up care and outcome evaluation of high-risk preterm infants: a life-course commitment. Ann Acad Med Singapore. 2018;47(2):51–5.
Durá-Travé T, San Martín-García I, Gallinas-Victoriano F, et al. Catch-up growth and associated factors in very low birth weight infants. Anal Pediatr. 2020;93(5):282–8.
Hack M, Merkatz IR, McGrath SK, Jones PK, Fanaroff AA. Catch-up growth in very-low-birth-weight infants: clinical correlates. J Amer Disease Children. 1984;138(4):370–5.
Leroy JL, Ruel M, Habicht J-P, Frongillo EA. Linear Growth Deficit continues to Accumulate beyond the first 1000 days in low- and middle-income countries: global evidence from 51 national surveys. J Nutrit. 2014;144(9):1460–6.
Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60.
Prendergast JA, Humphrey HJ. The stunting syndrome in developing countries. Paediatr Intern Child Health. 2014;34(4):250–65.
WHO. Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide. 2019.
Nutrition Landscape Information. System (NLIS) country profile indicators: interpretation guide. World Health Organisation; 2010.
WHO. World Health Organization Multicentre Growth Reference Study Group. WHO Child Growth standards based on length/height, weight and age.l 2006. Acta Paediatr Suppl. 2006;450(14):76–85.
Mbonye AK, Sentongo M, Mukasa GK, et al. Newborn survival in Uganda: a decade of change and future implications. Health Policy Plann. 2012;27(suppl3):iii104–iii17.
WHO child growth. Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006. p. 312.
Parul C, Sun EL, Moira DA, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. J Int Epid. 2013;42:1340–55.
USAID. “Country Profile: Uganda: Nutrition Profile.“ 2018.
Zhihui L, Rockli K, Sebastian V, Subramanian VS. Factors associated with child stunting, wasting, and underweight in 35 low- and middle-income countries. JAMA 2020;3.
Wemakor A, Garti H, Azongo T, et al. Young maternal age is a risk factor for child undernutrition in Tamale Metropolis, Ghana. BMC Res Notes. 2018;11(1):877.
Yu SH, Mason J, Crum J, et al. Differential effects of young maternal age on child growth. Glob Health Action. 2016;9(1):31171.
Martorell R, Zongrone A. Intergenerational influences on child growth and undernutrition. Paediatr Perinat Epid. 2012;26(Suppl 1):302–14.
Dusick AM, Poindexter BB, Ehrenkranz RA, et al. Growth failure in the preterm infant: can we catch up? Sem Perinat: Elsevier; 2003.
Ziegler EE, Carlson SJ. Early nutrition of very low birth weight infants. J Maternal-Fetal & Neonat Med. 2009;22(3):191–7.
Sachs J, Schmidt-Traub G, Kroll C et al. SDG Index and Dashboards report 2017. New York: Bertelsmann Stiftung and Sustainable Development Solutions Network (SDSN). 2017.
Acknowledgements
We thank the Management of Mulago Hospital, Staff at the Preterm Clinic, mentorship from Drs Ezekiel Mupere and Yaser Abdallah, Research Assistants: Rachael Namono, Jennifer Wabulya, Flora Fawling, Carol Akello & Florence Nakirijja and all the participants.
Funding
Support was from the Forgaty International Center of National Institutes of Health, U.S Department of State’s Office of Global AIDS Coordinator and Health Diplomacy (S/GAC), and President’s Emergency Plan for AIDS Relief (PEPFAR) under Award Number 1R25TW011213. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
FN, AB, JR, VOK: contributed to the conception and design of the study. FN and JR supervised the research, RS was involved in the analysis and interpretation of data, and FN, NNB, IGM, and SK were involved in drafting and revision of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by Makerere University Research and Ethics Committee (Ref 2019 − 117) and the Uganda National Council of Science & Technology (Ref HS 2690). Administrative clearance was obtained from Mulago National Referral Hospital. The caretakers who were the children’s legal guardians gave informed consent to participate in the study. Participation was voluntary and caregivers/ legal guardians signed a printed statement of an informed consent before inclusion in the study. A thumbprint of the statement was made by guardians who were not able to read/or write in presence of a witness who was not a member of the research team. This process was approved by the REC. All methods were performed in accordance with the relevant guidelines and regulations in Ethics Approval and Consent to participate in Declarations.
Consent for publication
Not Applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Namiiro, F.B., Batte, A., Rujumba, J. et al. Nutritional status of young children born with low birthweight in a low resource setting: an observational study. BMC Pediatr 23, 520 (2023). https://doi.org/10.1186/s12887-023-04356-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04356-9