Abstract
Background
To compare the clinical outcomes of bilateral implantation of enhanced intermediate function intraocular lenses (IOLs) and standard monofocal IOLs.
Methods
In this prospective, randomized, comparative controlled study, we compared the visual outcomes of patients who underwent bilateral cataract surgery at the Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, with either enhanced monofocal IOLs (Tecnis Eyhance, ICB00, Johnson and Johnson Vision Care, Inc) (Group 1) or standard monofocal IOLs (Tecnis, ZCB00, Johnson and Johnson Vision Care, Inc) (Group 2). The assessment included monocular and binocular uncorrected distance visual acuity (UDVA), uncorrected intermediate (UIVA at 60 cm) and near (UNVA at 40 cm) visual acuity, uncorrected defocus curves, contrast sensitivity testing (CST), and reading speed test using Quality of vision was evaluated using the Visual Function Questionnaire (VFQ-25).
Results
At 3-months postoperatively, monocular and binocular outcomes of UIVA and UNVA were statistically significantly better in Group 1 (P < 0.05). The binocular uncorrected defocus curve of Group 1 showed statistically significantly better outcomes at vergence ranges of -1.5 to -4.0 D (P < 0.05). Significantly higher reading speed test was also observed in Group 1 in all ranges tested (1.0 to 0.1 LogMAR) (P < 0.05). There were no statistically significant differences in CST between groups.
Conclusions
Bilateral implantation of enhanced monofocal IOLs provided better vision at intermediate and near distances compared to standard monofocal IOLs, while maintaining good distance vision and contrast sensitivity.
Similar content being viewed by others
Background
Today, multifocal intraocular lenses (IOLs) are widely used to provide good spectacle independent vision at far, intermediate, and near distances [1]. However, patients with such multifocal optics may experience photic phenomena such as glare and halo or perceive reduced contrast sensitivity [2]. Thus, various studies have sought to investigate whether combining trifocal, bifocal, extended depth of focus (EDoF), and monofocal IOLs may minimize such optical side effects while maintaining good visual quality [3, 4].
Previously, we performed a combined implantation of trifocal and EDoF IOLs in cataract patients and observed good visual outcomes in far to near distances as well as a high spectacle independence [5]. In another study, we compared the visual function in patients who underwent either blended implantation of bifocal and EDoF IOLs or bilateral implantation of trifocal IOLs, and we reported satisfactory spectacle-independent vision at far, intermediate, and near distances in both groups [6]. In all three strategies we investigated, however, there still remained the issue of photic phenomena that caused some degree of patient dissatisfaction.
The Tecnis® Eyhance (Model ICB00, Johnson and Johnson Vision Care, Inc) is a recently developed monofocal IOL with a higher-order aspheric anterior surface designed to improve intermediate vision. As it has been shown to provide good uncorrected visual quality at far to intermediate distances, the Tecnis Eyhance is increasingly gaining popularity [7,8,9,10,11]. Kang et al. reported that Tecnis Eyhance can not only achieve superior intermediate vision and comparable visual performance at distance, but also generate low incidence of photic phenomena comparable to that of a Tecnis standard monofocal IOL [10]. Similar results were observed in other studies that compared the Tecnis Eyhance with Alcon and Rayner’s standard monofocal IOLs [12, 13].
In this study, we sought to compare the visual outcomes, contrast sensitivity, reading speed, photic phenomena, and patient satisfaction in patients who underwent binocular implantation of Tecnis Eyhance IOL (Model ICB00) and binocular implantation of a standard Tecnis monofocal IOL (Model ZCB00) that shares the same optical platform.
Methods
This prospective, randomized, and comparative controlled study included patients with age-related cataracts who underwent bilateral cataract extraction with phacoemulsification and IOL implantation with either an enhanced monofocal IOL (Tecnis Eyhance, ICB00, Johnson and Johnson Vision Care, Inc) (Group 1) or a standard monofocal IOL (Tecnis, ZCB00, Johnson and Johnson Vision Care, Inc) (Group 2). Both groups comprised of 25 patients and the diagnosis was made using the lens opacities classification system (LOCS) III.
This study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Kangbuk Samsung Hospital (IRB File No. 2019–12-030). All study participants signed the informed consent before enrollment.
Inclusion criteria were patients aged 50 years or older at time of study enrollment, who underwent surgery of fellow eye 1 week after surgery of the first eye, showed postoperative visual potential of 20/25 or better, and had pre-existing corneal astigmatism of less than 1.25 D. Exclusion criteria were: any general condition that may affect the surgical outcomes and a history of ocular trauma, surgery, or pathology that may limit the visual function.
All patients received preoperative ophthalmic examination including mesopic (3 cd/\({m}^{2}\)) pupillometry, manifest refraction, uncorrected (UDVA) and corrected distance visual acuity (CDVA), uncorrected intermediated (UIVA) and near visual acuity (UNVA), topography (Galilei G6: Ziemer Ophthalmic Systems AG), corneal aberration (KR-1W Wavefront Analyzer; Topcon Europe Medical BV), optical biometry and keratometry (IOLMaster 700, Carl Zeiss Meditec), slit-lamp examination and fundoscopy. The mesopic pupil diameter was measured using the length of slit light with minimum width during slit-lamp examination.
All surgeries were performed by one surgeon (CYC): under topical anesthesia, a 2.2 mm corneal incision was made, followed by manual capsulorrhexis and phacoemulsification. All IOLs were implanted in the bag. Postoperative target refraction was determined as the lowest myopic value after emmetropia using the Haigis formula in IOL calculation.
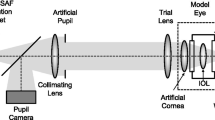
Follow-up examinations were performed at 1-week, 1-month, and 3-months after implantation of the second IOL. Main outcome measures included visual acuities, monocular and binocular defocus curves, contrast sensitivity testing (CST), reading speed test, and patient questionnaires. UDVA, UIVA at 66 cm, and UNVA at 40 cm were measured using the Early Treatment Diabetic Retinopathy Study charts (ETDRS; Vector Vision, Ltd., Greenville, OH, USA). Uncorrected monocular and binocular defocus curves were obtained for distance vision with the ETDRS charts at intervals of 0.50 spherical D from − 4.00 to + 1.00 D. CS was measured at 3.0, 6.0, 12.0, and 18.0 cycles per degree (cpd) under photopic (85 cd/m2) and mesopic (3 cd/m2) conditions with and without glare with the CSV-1000 (Vector vision, Inc., Greenville, OH, USA).
Patients' subjective satisfaction was analyzed using the quality of vision (QoV) and vision-related quality of life (QoL) questionnaires both preoperatively and 3-month postoperatively, while spectacle independence was assessed using the 25-item National Eye Institute Functional Questionnaire (NEI VFQ-25).
The binocular reading speed at 40 cm was measured at 3-months postoperatively as described by the Korean Reading Speed Application tester [5, 6]. Letter sizes from 0.0 logMAR to 1.0 logMAR were displayed in steps of 0.1 logMAR. Patients were asked to read sentences of different sizes one after the other. Reading speed (words per minute) was automatically calculated by its own system “Hangul”.
Statistical analysis was performed using the SPSS software (Version 24.0: SPSS, Inc). Intergroup comparisons of monocular and binocular visual outcomes were performed with the independent two sample t-test and Pearson’s chi-square test. The Mann–Whitney U test was used to compare quantitative variables (such as refraction) and reading speed. The t test for independent samples was used to compare overall satisfaction and spectacle independence. For the adjustment of P values, the Bonferroni correction was used. Data were expressed as mean and standard deviation. For all analyses, the level of significance was a P value of less than 0.05. Normal distribution of our data was confirmed via histogram.
Results
Demographic and preoperative clinical characteristics of all patients are shown in Table 1. There were no statistically significant differences in any of the variables between the two groups.
Table 2 lists the mean binocular and monocular UDVA, CDVA, UIVA, UNVA, and spherical equivalent (SE) values of both groups measured 3-month postoperatively. Group 1 achieved better monocular UDVA as well as monocular and binocular UIVA and UNVA compared to Group 2 (p < 0.05 for all cases). Binocular UDVA (p = 0.146) and CDVA (p = 0.193) were better Group 1 compared to Group 2, but there were no statistically significant differences.
Group 1 showed better visual acuity than Group 2 in monocular defocus curve from + 1.0 to -4.0 (p < 0.05) except at 0 D (p = 0.948). In binocular defocus curve testing, Group 1 demonstrated statistically significantly superior visual acuities from -1.5 to -4.0 D (p < 0.05) (Fig. 1).
As shown in Fig. 2, Group 1 showed statistically significantly better binocular reading speed than Group 2 for all letter sizes (p < 0.05) except for 0.5 logMAR (p = 0.223).
Figure 3 demonstrates postoperative monocular and binocular contrast sensitivity results under photopic and mesopic conditions with and without glare. For all light conditions, no statistically significant differences were observed at any spatial frequency between the two groups.
The results of the VFQ-25 questionnaire are shown in Fig. 4. All patients reported better outcomes in every category except for ocular pain compared to preoperative values, although there were no statistically significant difference except in general health between Group 1 and Group 2 postoperatively.
Questionnaire results regarding the perception of photic phenomena and spectacle independent vision satisfaction are shown in Fig. 5. In both groups, more than 90% of patients reported to not experience any glare, halo or starburst phenomena, still there were no statistically significant differences between two groups. Group 1 showed higher spectacle independent vision satisfaction at near distance than Group 1, while there were no statistically significant difference in vision satisfaction at any distances.
Both groups showed very high rate of spectacle independence for far distance with over 90% of patients in each group requiring no glasses, while the rate of spectacle independence at intermediate distance was higher in Group 1 (91%) compared to Group 2 (72% (Fig. 6).
Discussion
In this study, we compared the clinical outcomes after bilateral implantation of an enhanced monofocal IOL and a standard monofocal IOL to investigate the efficacy of the novel optical design for intermediate distance. At 3-months postoperatively, patients with bilateral Tecnis Eyhance IOL demonstrated statistically significantly better monocular and binocular UIVA and UNVA in addition to superior monocular UDVA and CDVA compared to patients with bilateral standard monofocal IOLs. Most importantly, the incidence of dysphotopsia perceived by patients with bilateral Eyhance IOLs was comparable to that of patients with bilateral standard monofocal lenses, demonstrating the efficacy of the Eyhance IOL in providing good vision at all distances while minimizing the optical side effects.
Our findings are in alignment with those of previous reports which demonstrated superiority of the Eyhance IOL in UDVA and UIVA [7,8,9,10,11,12,13]. The slight disparities in the reported visual outcomes between studies may be ascribable to the differences in distances at which the visual acuity was measured (e.g. 66 or 80 cm) and the range in postoperative SE (-0.27 to -0.36 in mean value) [11, 14,15,16,17]. Our findings also confirm the results of a previous study which showed that the Tecnis Eyhance IOL leads to higher tolerance for residual refractive error compared to a standard monofocal IOL [14].
Both the monocular and binocular defocus curves measured in Group 1 demonstrated a wider and smoother slope than those of Group 2. While the defocus curves from previous studies [15] demonstrated a higher and sharper peak at 0 SE, it is important to note that we obtained an uncorrected defocus curve. Indeed, corrected defocus curves would represent the inherent characteristics of the IOLs themselves better; however, it would not be fully representative of the real-life visual function perceived by patients who now mostly live independent with spectacle. Furthermore, assessing the defocus curve with additional trial lenses to correct the residual refractive error may induce wavefront errors, which may lead to fictitious results.
Reading speed is a better indicator of the patients’ actual visual function in daily life and thus has been widely used in numerous clinical studies to characterize the functional outcomes [18, 19]. In our analysis, patients with bilateral Eyhance IOL implantation showed superior reading speed for all letter sizes and visual ranges tested (1.0 to 0.1 LogMAR) compared to those with a standard monofocal IOL. It is important to note that in this study the reading performance was tested using the Korean alphabet known as ‘Hangul’, which is commonly considered to be more complicated in design compared to the English alphabet, composed of vowel and consonants in particular position lather than just enumerating it in a row. Reading performance in other languages may therefore differ from that of our study. To the best of our knowledge, this is the first report comparing the reading performance of these IOLs in a Korean population.
As reported by previous studies [11, 14,15,16], the contrast sensitivity was within age-adjusted normal range for both groups and did not show any statistically significant differences under all light conditions tested, which is expected given that monofocal IOLs generally do not deteriorate the contrast sensitivity [20] and the Tecnis Eyhance employs the same optical platform as the Tecnis monofocal IOL examined in this study.
We also evaluated the patients’ subjective satisfaction in their daily life using QoV, QoL, and NEI VFQ-25 questionnaires. Both groups showed improvement postoperatively in all questionnaires and showed excellent outcomes in terms of photic phenomena, with more than 90% of patients indicating to experience ‘none’ of photic phenomena in any situation. As the Tecnis Eyhance features an additional optic design in its central optic to generate intermediate vision, one may expect a higher rate of positive dysphotospia. Our results, however, could not substantiate this hypothesis as we observed a comparable rate of photic phenomena in both groups. Given that more than 90% of patients in Group 1 indicated to be spectacle independent for performing tasks in far and intermediate distances, our results suggest that the Tecnis Eyhance IOL is able to provide satisfactory far and intermediate vision, while causing minimal optical side effects.
Although this study may be limited by its relatively short follow-up period and a small sample size, this is the first prospective, randomized controlled study aimed at characterizing the patients’ daily visual performance after bilateral implantation of the Tecnis Eyhance IOL by assessing various visual parameters including reading performance.
Conclusions
In conclusion, bilateral implantation of an enhanced monofocal IOL demonstrated very good uncorrected far and intermediate visual acuities compared to a standard monofocal IOL that shares the same optical platform. Spectacle independence was high at far and intermediate distances. As evidenced by the defocus curve, patients with bilateral enhanced monofocal IOLs had strong advantages at intermediate distance. Enhanced monofocal IOLs may therefore present a good option in patients with higher demand for distant and intermediate vision without any concern of positive dysphotopsia.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IOL:
-
Intraocular lens
- UDVA:
-
Uncorrected distant visual acuity
- UIVA:
-
Uncorrected intermediate visual acuity
- UNVA:
-
Uncorrected near visual acuity
- CDVA:
-
Corrected distant visual acuity
- CST:
-
Contrast sensitivity
- EDoF:
-
Extended depth of focus
- NEI VFQ:
-
National Eye Institute Visual Functional Questionnaire
- CPD:
-
Cycles per degree
- D:
-
Diopters
- SE:
-
Spherical equivalent
- logMAR:
-
Logarithm of the minimal angle of resolution
References
Salerno LC, Tiveron MC Jr, Alio JL. Multifocal intraocular lenses: Types, outcomes, complications and how to solve them. Taiwan J Ophthalmol. 2017;7(4):179–84.
Black S. A clinical assessment of visual performance of combining the TECNIS((R)) Symfony Extended Range of Vision IOL (ZXR00) with the +3.25 D TECNIS Multifocal 1-piece IOL (ZLB00) in subjects undergoing bilateral cataract extraction. Clin Ophthalmol. 2018;12:2129–36.
Altemir-Gomez I, Millan MS, Vega F, Bartol-Puyal F, Gimenez-Calvo G, Larrosa JM, et al. Comparison of visual and optical quality of monofocal versus multifocal intraocular lenses. Eur J Ophthalmol. 2020;30(2):299–306.
Yamauchi T, Tabuchi H, Takase K, Ohsugi H, Ohara Z, Kiuchi Y. Comparison of visual performance of multifocal intraocular lenses with same material monofocal intraocular lenses. PLoS ONE. 2013;8(6): e68236.
Song JE, Han SY, Khoramnia R, Tandogan T, Auffarth GU, Choi CY. Clinical outcomes of combined implantation of an extended depth of focus IOL and a Trifocal IOL in a Korean population. J Ophthalmol. 2021;2021:9034258.
Song JE, Khoramnia R, Son HS, Knorz MC, Choi CY. Comparison Between bilateral implantation of a Trifocal IOL and mix-and-match implantation of a Bifocal IOL and an extended depth of focus IOL. J Refract Surg. 2020;36(8):528–35.
Huh J, Eom Y, Yang SK, Choi Y, Kim HM, Song JS. A comparison of clinical outcomes and optical performance between monofocal and new monofocal with enhanced intermediate function intraocular lenses: a case-control study. BMC Ophthalmol. 2021;21(1):365.
Wan KH, Au ACK, Kua WN, Ng ALK, Cheng GPM, Lam NM, et al. Enhanced monofocal versus conventional monofocal intraocular lens in cataract surgery: a meta-analysis. J Refract Surg. 2022;38(8):538–46.
de Luis Eguileor B, Martinez-Indart L, Martinez Alday N, Sacristan Eguen C, Cuadros Sanchez C. Differences in intermediate vision: monofocal intraocular lenses vs. monofocal extended depth of focus intraocular lenses. Arch Soc Esp Oftalmol (Engl Ed). 2020;95(11):523–7.
Kang KH, Song MY, Kim KY, Hwang KY, Kwon YA, Koh K. Visual performance and optical quality after implantation of a new generation monofocal intraocular lens. Korean J Ophthalmol. 2021;35(2):112–9.
Auffarth GU, Gerl M, Tsai L, Janakiraman DP, Jackson B, Alarcon A, et al. Clinical evaluation of a new monofocal IOL with enhanced intermediate function in patients with cataract. J Cataract Refract Surg. 2021;47(2):184–91.
Cinar E, Bolu H, Erbakan G, Yuce B, Aslan F, Fece M, et al. Vision outcomes with a new monofocal IOL. Int Ophthalmol. 2021;41(2):491–8.
Nanavaty MA, Ashena Z, Gallagher S, Borkum S, Frattaroli P, Barbon E. Visual acuity, wavefront aberrations, and defocus curves with an enhanced monofocal and a monofocal intraocular lens: a prospective. Randomized Study J Refract Surg. 2022;38(1):10–20.
Unsal U, Sabur H. Comparison of new monofocal innovative and standard monofocal intraocular lens after phacoemulsification. Int Ophthalmol. 2021;41(1):273–82.
Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378–87.
Pedrotti E, Bruni E, Bonacci E, Badalamenti R, Mastropasqua R, Marchini G. Comparative analysis of the clinical outcomes with a monofocal and an extended range of vision intraocular lens. J Refract Surg. 2016;32(7):436–42.
Yangzes S, Kamble N, Grewal S, Grewal SPS. Comparison of an aspheric monofocal intraocular lens with the new generation monofocal lens using defocus curve. Indian J Ophthalmol. 2020;68(12):3025–9.
Attia MSA, Auffarth GU, Kretz FTA, Tandogan T, Rabsilber TM, Holzer MP, Khoramnia R. Clinical evaluation of an extended depth of focus intraocular lens with the Salzburg reading desk. J Refract Surg. 2017;33(10):664–9.
Son HS, Khoramnia R, Yildirim TM, Baur I, Labuz G, Auffarth GU. Functional outcomes and reading performance after combined implantation of a small-aperture lens and a segmental refractive bifocal lens. J Refract Surg. 2019;35(9):551–8.
Mesci C, Erbil HH, Olgun A, Aydin N, Candemir B, Akçakaya AA. Differences in contrast sensitivity between monofocal, multifocal and accommodating intraocular lenses: long-term results. Clin Exp Ophthalmol. 2010;38(8):768–77.
Acknowledgements
Not applicable.
Funding
The project was funded by Medical Research Funds from Kangbuk Samsung Hospital. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Chul Young Choi and Wan Kyu Choi designed the study, performed clinical process, collected data, performed statistic analysis and wrote the manuscript. Hyo Ji Han collected data. Hyeck Soo Son, Ramin Khoramnia and Gerd U. Auffarth wrote the manuscript. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the tenets of the Declaration of Helsinki. Approval to conduct this study was obtained from the Institutional Review Board of Kangbuk Samsung Hospital (Seoul, Republic of Korea; IRB File No. 2019–12-030). Informed written consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Choi, W.K., Han, H.J., Son, HS. et al. Clinical outcomes of bilateral implantation of new generation monofocal IOL enhanced for intermediate distance and conventional monofocal IOL in a Korean population. BMC Ophthalmol 23, 157 (2023). https://doi.org/10.1186/s12886-023-02897-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-02897-2