Abstract
Background
Patient satisfaction is an important indicator of the quality of healthcare. Pain is one of the most common symptoms among cancer patients that needs optimal treatment; rather, it compromises the quality of life of patients.
Objective
To assess the levels and associated factors of satisfaction with cancer pain treatment among adult patients at cancer centers found in Northern Ethiopia in 2023.
Methods
After obtaining ethical approval, a multi-center cross-sectional study was conducted at four cancer care centers in northern Ethiopia. The data were collected using an interviewer-administered structured questionnaire that included the Lubeck Medication Satisfaction Questionnaire (LMSQ). The severity of pain was assessed by a numerical rating scale from 0 to 10 with a pain score of 0 = no pain, 1–3 = mild pain, 4–6 = moderate pain, and 7–10 = severe pain Binary logistic regression analysis was employed, and the strength of association was described in an adjusted odds ratio with a 95% confidence interval.
Result
A total of 397 cancer patients participated in this study, with a response rate of 98.3%. We found that 70.3% of patients were satisfied with their cancer pain treatment. Being married (AOR = 5.6, CI = 2.6–12, P < 0.001) and being single (never married) (AOR = 3.5, CI = 1.3–9.7, P = 0.017) as compared to divorced, receiving adequate pain management (AOR = 2.4, CI = 1.1–5.3, P = 0.03) as compared to those who didn’t receive it, and having lower pain severity (AOR = 2.6, CI = 1.5–4.8, P < 0.001) as compared to those who had higher level of pain severity were found to be associated with satisfaction with cancer pain treatment.
Conclusion
The majority of cancer patients were satisfied with cancer pain treatment. Being married, being single (never married), lower pain severity, and receiving adequate pain management were found to be associated with satisfaction with cancer pain treatment. It would be better to enhance the use of multimodal analgesia in combination with strong opioids to ensure adequate pain management and lower pain severity scores.
Similar content being viewed by others
Introduction
Pain is defined as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage [1]. The prevalence of pain in cancer patients is 44.5-66%. with the prevalence of moderate to severe pain ranging from 30 to 38%, and it can persist in 5-10% of cancer survivors [2]. Using the World Health Organization’s (WHO) cancer pain management guidelines can effectively reduce cancer-related pain in 70-90% of patients [3, 4]. Compared to traditional pain states, the mechanism of cancer-related pain is less understood; however, cancer-specific mechanisms, inflammatory, and neuropathic processes have been identified [5]. Uncontrolled pain can negatively affect patients’ daily lives, emotional health, social relationships, and adherence to cancer treatment [6]. Patients with moderate to severe pain have a higher fatigue score, a loss of appetite, and financial difficulties [7]. Patients fear the pain caused by cancer more than dying from the disease since pain affects their physical and mental aspects of life [8]. A meta-analysis of 30 studies stated that pain was found to be a significant prognostic factor for short-term survival in cancer patients [9]. Many cancer patients have a very poor prognosis. However, adequate pain treatment prevents suffering and improves their quality of life. Although the WHO suggested non-opioids for mild pain, weak opioids for moderate pain, and strong opioids for severe pain, pain treatment is not yet adequate in one-third of cancer patients [10].
Patient satisfaction with pain management is a valuable measure of treatment effectiveness and outcome. It could be used to evaluate the quality of care [11,12,13]. Patient satisfaction affects treatment compliance and adherence [12]. Studies have reported that 60-76% of patients were satisfied with pain treatment, and a variety of factors were found associated with levels of satisfaction [3, 14,15,16]. Studies conducted in Ethiopia reported the prevalence of pain ranging from 59.9 to 93.4% [17, 18]. These studies indicate that cancer pain is inadequately treated. Assessment of pain treatment satisfaction can help identify appropriate treatment modalities and further its effectiveness. We conducted this study since there was limited research-based evidence on cancer pain management in low-income countries like Ethiopia. Our research questions were: how satisfied are adult cancer patients with pain treatment, and what are the factors associated with the satisfaction of adult cancer patients with pain treatment?
Methodology
Study design, area, period, and population
A multi-center cross-sectional study was conducted at four cancer care centers in Amhara National Regional State, Northern Ethiopia from March to May 2023. Those cancer care centers were found in the University of Gondar Comprehensive Specialized Hospital (UoGCSH), Felege-Hiwot Comprehensive Specialized Hospital (FHCSH), Tibebe-Ghion Comprehensive Specialised Hospital (TGCSH) and Dessie Comprehensive Specialized Hospital (DCSH). We selected these centers as they were the only institutions providing oncologic care in the region during the study period.
The UoGCSH had 28 beds in its adult oncology ward and serves 450 cancer patients every month. Three specialist oncologists and 12 nurses provide services in the ward. The FHCSH had 22 beds and provides services for 325 cancer patients every month. Two specialist oncologists, two oncologic nurses, and 7 comprehensive nurses provide services. The TGCSH had eight beds and serves 300 cancer patients every month. There were three specialist oncologists and four oncologic nurses at the care center. The cancer care center at DCSH had 10 beds. It serves 350 cancer patients every month. There was one specialist oncologist, three oncologic nurses, and three comprehensive nurses.
All cancer patients who attended those cancer care centers were the source population, and adult (18+) cancer patients who were prescribed pain treatment for a minimum of one month were the study population. Unconscious patients, patients with psychiatric problems, patients with advanced cancer who were unable to cooperate, and patients with oncologic emergencies were excluded from this study.
Variables and operational definitions
The outcome variable was patient satisfaction with cancer pain treatment, which was measured by the Lubeck Medication Satisfaction Questionnaire. The independent variables were sociodemographic (age, sex, marital status, monthly income, and level of education), clinical (site of tumor, stage of cancer, metastasis), cancer treatment (surgery, chemotherapy, radiotherapy), level of pain, and analgesia (type of analgesia, severity of pain, adequacy of pain treatment, adjuvant analgesic).
Patient satisfaction
perceptions of the patients regarding the outcome of pain management and the extent to which it meets their needs and expectations. It was measured by a 4-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree) using the LMSQ which has 18 items within 6 subscales that have 3 items in each (effectivity, practicality, side-effects, daily life, healthcare providers, and overall satisfaction) [19]. Final categorization was done by dichotomizing into satisfied and dissatisfied by using the demarcation threshold formula.
\((\frac{\text{T}\text{o}\text{t}\text{a}\text{l}\,\,\text{h}\text{i}\text{g}\text{h}\text{e}\text{s}\text{t}\,\,\text{s}\text{c}\text{o}\text{r}\text{e} - \text{T}\text{o}\text{t}\text{a}\text{l}\,\, \text{l}\text{o}\text{w}\text{e}\text{s}\text{t}\,\, \text{s}\text{c}\text{o}\text{r}\text{e} }{2}\)) + Total lowest score [20]. The highest patient satisfaction score was 70 and the lowest satisfaction score was 26. A score < 48 was classified as dissatisfied, and a score ≥ 48 was classified as satisfied.
The Numeric rating scale (NRS) is a validated pain intensity assessment tool that helps to give patients a subjective feeling of pain with a numerical value between 0 and 10, in which 0 = no pain, 1–3 = mild pain, 4–6 = moderate pain, 7–10 = severe pain [21].
The Adequacy of cancer pain treatment was measured by calculating the Pain Management Index (PMI) according to the recommendations of the WHO pain management guideline [22]. The PMI was calculated by considering the prescribed most potent analgesic agent and the worst pain reported in the last 24 h [23]. The prescribed analgesics were scored as follows: 0 = no analgesia, 1 = non-opioid analgesia, 2 = weak opioids, and 3 = strong opioids. The PMI was calculated by subtracting the reported NRS value from the type of most potent analgesics administered. The calculated values of PMI ranged from − 3 (no analgesia therapy for a patient with severe pain) to + 3 (strong opioid for a patient with no pain). Patients with a positive PMI value were considered to be receiving adequate analgesia, whereas those with a negative PMI value were considered to be receiving inadequate analgesia.
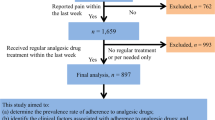
Sample size determination and sampling technique
A single population proportion formula was used to determine the sample size by considering 50% satisfaction with cancer pain treatment and a 5% margin of error at a 95% confidence interval (CI). A non-probability (consecutive) sampling technique was employed to attain a sample size within two months of data collection period. After adjusting the proportional allocation for each center and adding 5% none response, a total of 404 study participants were included in the study: 128 from the University of Gondar Comprehensive Specialized Hospital, 99 from Dessie Comprehensive Specialized Hospital, 92 from Felege Hiwot Comprehensive Specialized Hospital, and 85 from Tibebe Ghion Comprehensive Specialized Hospital.
Data collection, processing, and analysis
Ethical approval
was obtained from the Ethical Review Committee of the School of Medicine at the University of Gondar (Reference number: CMHS/SM/06/01/4097/2015). Data were collected using an interviewer-administered structured questionnaire and chart review during outpatient and inpatient hospital visits by four trained data collectors (one for every center). Written informed consent was obtained from each participant after detailed explanations about the study. Informed consent with a fingerprint signature was obtained from patients who could not read or write after detailed explanations by the data collectors as approved by the Ethical Review Committee of the School of Medicine, at the University of Gondar.
Questions to assess the severity of pain and pain relief were taken from the American Pain Society patient outcome questionnaire [24]. Patients were asked to report the worst and least pain in the past 24 h and the current pain by using a numeric rating scale from 0 to 10, with a pain score of 0 = no pain, 1–3 = mild pain, 4–6 = moderate pain, 7–10 = severe pain.
The Pain Management Index (PMI) based on WHO guidelines, was used to quantify pain management by measuring the adequacy of cancer pain treatment [25]. The following scores were given (0 = no analgesia, 1 = non-opioid analgesia, 2 = weak opioid 3 = strong opioid). Pain Management Index was calculated by subtracting self-reported pain level from the type of analgesia administered and ranges from − 3 (no analgesic therapy for a patient with severe pain) to + 3 (strong opioid for a patient with no pain). The level of pain was defined as 0 with no pain, 1 for mild pain, 2 for moderate pain, and 3 for severe pain. Patients with negative PMI scores received inadequate analgesia.
The pain treatment satisfaction was measured by the Lübeck Medication Satisfaction Questionnaire (LMSQ) consisting of 18 items [19]. Lübeck Medication Satisfaction Questionnaire (LMSQ) has six subclasses each consisting of equally waited and similar context of three items. The subclass includes satisfaction with the effectiveness of pain medication, satisfaction with the practicality or form of pain medication, satisfaction with the side effect profile of pain medication, satisfaction with daily life after receiving pain treatment, satisfaction with healthcare providers, and overall satisfaction. Satisfaction was expressed by a four-point Likert scale (4 = Strongly Agree, 3 = Agree, 2 = Disagree, 1 = Strongly Disagree). The side effect subclass was phrased negatively, marked with Asterix, and reverse-scored in STATA before data analysis.
Data were collected with an interviewer-administered questionnaire. The reliability of the questionnaire was assessed by using 40 pretested participants and the reliability coefficient (Cronbach’s alpha value) of the questionnaire was 91.2%. The collected data was checked for completeness, accuracy, and clarity by the investigators. The cleaned and coded data were entered in Epi-data software version 4.6 and exported to STATA version 17. The Shapiro-Wilk test, variance inflation factor, and Hosmer-Lemeshow test were used to assess distribution, multicollinearity, and model fitness, respectively. Descriptive, Chi-square and binary logistic regression analyses were performed to investigate the associations between the independent and dependent variables. The independent variables with a p-value < 0.2 in the bivariable binary logistic regression were fitted to the final multivariable binary logistic regression analysis. Variables with p-value < 0.05 in the final analysis were considered to have a statistically significant association. The strength of associations was described in adjusted odds ratio (AOR) at a 95% confidence interval.
Results
Sociodemographic and clinical characteristics
A total of 397 patients were involved in this study (response rate of 98.3%). Of the participants, 224 (56.4%) were female, and over half were from rural areas (n = 210, 52.9%). The median (IQR) age was 48 (38–59) years [Table 1]. The most common type of cancer was gastrointestinal cancer 114 (28.7%). Most of the study participants, 213 (63.7%), were diagnosed with stage II to III cancer. The majority of the participants were taking chemotherapy alone (292 (73.6%)) [Table 2]. Over 90% of patients reported pain; 42.3% reported mild pain, 39.8% reported moderate pain, and 10.1% reported severe pain. Pain treatment adequacy was assessed by self-reports from study participants following pain management guidelines, and 17.1% of patients responded to having inadequate pain treatment. The majority of patients, 132 (33.3%), were prescribed combinations of non-opioid and weak opioid analgesics for cancer pain treatment. Only 34 (8.6%) cancer patients used either strong opioids alone or in combination with non-opioid analgesics.
Patients’ satisfaction with cancer pain treatment and correlation among the subscales
Most participants strongly agree (243, (61.2%)) with item LMSQ18 in the “overall satisfaction” subscale and strongly disagree (206, (51.9%)) for item LMSQ2 in the “side-effect” subscale respectively [Table 3]. The highest satisfaction score was observed in the side-effect subscale, with a median (IQR) of 10 (9–11) [Table 4].
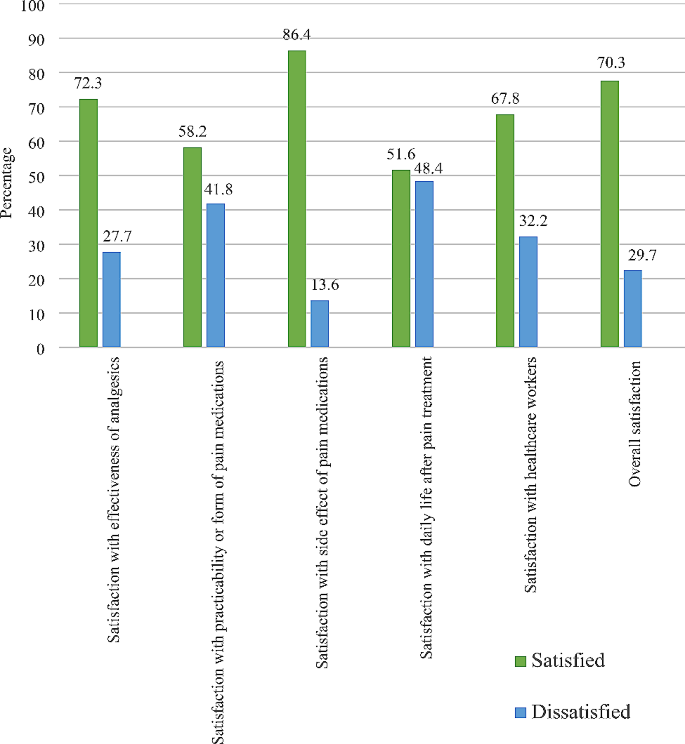
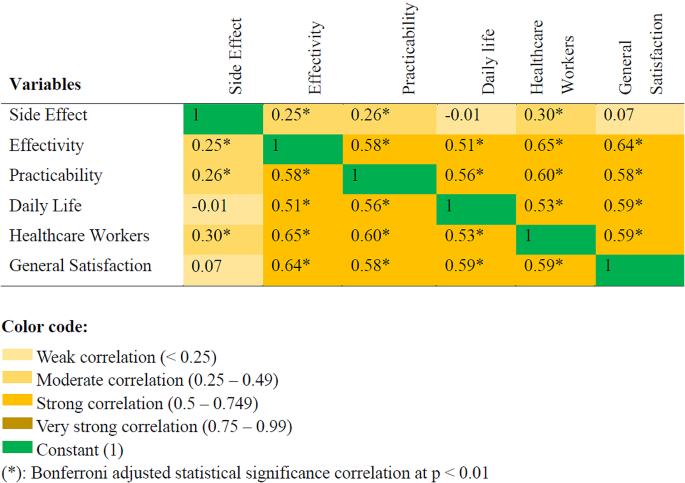
Two hundred and seventy-nine (70.3%) cancer patients were found to be satisfied with cancer pain treatment (CI = 65.6−74.6%). The highest satisfaction rate was observed in the “side-effects” subscale, to which 343 (86.4%) responded satisfied [Fig. 1]. A Spearman’s correlation test revealed that there were correlations among the subscales of LMSQ; and the strongest positive correlation was observed between effectivity and healthcare workers subscale (rs = 0.7, p < 0.0001). The correlation among the subscales is illustrated in a heatmap [Fig. 2].
Factors associated with patient satisfaction with cancer pain treatment
In the bivariable binary logistic regression analysis, marital status, stage of cancer, types of cancer treatment, severity of pain in the last 24 h, current pain severity, types of analgesics, and pain management index met the threshold of P-value < 0.2 to be included into the final multivariable binary logistic regression analysis. In the final analysis, marital status, current pain severity, and pain management index were significantly associated with patient satisfaction (P-value < 0.05). Married and single cancer patients had higher odds of being satisfied with cancer pain treatment compared to divorced patients (AOR = 5.6, CI, 2.6–12.0, P < 0.001), (AOR = 3.5, CI = 1.3–9.7, P = 0.017), respectively. The odds of being satisfied with cancer pain treatment among patients who received adequate pain management were more than two times greater than those who received inadequate pain management (AOR = 2.4, CI = 1.1–5.3, P = 0.03). Patients who reported a lesser severity of current pain were nearly three times more likely to be satisfied with cancer pain treatment (AOR = 2.6, CI = 1.5–4.8, P < 0.001) [Table 5].
Discussion
The objective of the present study was to assess patients’ satisfaction with cancer pain treatment at adult oncologic centers. Our study revealed that most cancer patients (70.3%) have been satisfied with cancer pain treatment. This is consistent with studies done by Kaggwa et al. and Mazzotta et al. [16, 26]. Whereas, it is a higher rate of satisfaction compared to other studies that reported 33.0% [27] and 47.7% [28] of satisfaction. The differences might be possibly explained by the use of different pain and satisfaction assessment tools, the greater inclusion (about 70%) of patients with advanced stages of cancer, the duration of cancer pain treatment, and the adequacy of pain management. In the current study, only 19.6% of patients have been diagnosed with stage IV cancer: patients should take treatment at least for a month, and over 80% of patients have received adequate pain management according to PMI. However, some studies have reported higher rates of satisfaction with cancer pain treatment [15, 29]. The possible reason for the discrepancy might be the greater (over 40%) use of strong opioid analgesics in the previous studies. Strong opioids were prescribed only for 8.6% of patients in our study. Due to the complex pathophysiology, cancer pain involves multiple pain pathways. Hence, multimodal analgesia in combination with strong opioids is vital in cancer pain management [30]. Furthermore, the use of epidural analgesia could be another reason for higher rates of satisfaction [29].
Regarding satisfaction with subscales of LMSQ, about 80% of patients were satisfied with the information provided by the healthcare providers [27]. In our study; 67.8% of patients were satisfied with the education provided by healthcare providers about their disease and treatment. In contrast, a higher proportion of participants were satisfied with information provision in a study conducted by Kharel et al. [29]. Furthermore, we observed the lowest satisfaction rate in the daily life subscale. About 48% of cancer patients were not satisfied with their daily lives after receiving analgesic treatment for cancer pain.
Married and single (never married) cancer patients were found to have higher odds of being satisfied with cancer pain treatment as compared to divorced cancer patients. These findings could be explained by the presence of better social support from family or loved ones. Better social support can enhance positive coping mechanisms, increase a sense of well-being, and decrease anxiety and depression. It also improves a sense of societal vitality and results in higher patient’ satisfaction [31, 32].
Patients who had a lower pain score were satisfied compared to those who reported a higher pain score, and this is supported by multiple previous studies [16, 26, 27, 29, 33, 34]. This could be explained by the negative impacts of pain on physical function, sleep, mood, and wellbeing [35]. Moreover, higher pain severity scores could increase financial expenses because of unnecessary or avoidable emergency department visits; and has a consequence of dissatisfaction [23]. On the contrary, there are studies that state pain severity does not affect patients’ satisfaction [36, 37].
Positive PMI scores were significantly associated with cancer pain treatment satisfaction. Patients who received adequate pain management were highly likely to be satisfied with cancer pain treatment. This finding is similar to that of a study done in Taiwan [38]. However, a study conducted by Kaggwa et al. has denied any association between PMI scores and cancer pain satisfaction [16].
Satisfaction with healthcare workers and effectivity of analgesics
This study showed that there was a moderately positive correlation between satisfaction with healthcare workers and satisfaction with patients’ perceived effectiveness of analgesics. This might be explained by a positive relationship between healthcare professionals and patients receiving cancer pain treatment. Healthcare providers who provide health education regarding the effectiveness of analgesics may improve patients’ adherence to the prescribed analgesic agent and improve patients’ perceived satisfaction with the effectiveness of analgesics. A systematic review showed that the hope and positivity of healthcare professionals were important for patients to cope with cancer and increase satisfaction with care [39]. Increased patient satisfaction with care provided by healthcare workers may change attitude of patients who accepted cancer pain as God’s wisdom or punishment and create a positive attitude toward the effectiveness of analgesics [40]. Another study supported this finding and stated that healthcare providers who deliver health education regarding the prevention of drug addiction, side effects of analgesics, timing, and dosage of analgesics improve patient attitude and cancer pain treatment [41].
Correlation of each subclass of cancer pain treatment satisfaction
A Spearman correlation was run to assess the correlation of each subclass of LMSQ using the total sample. There was strong positive correlation (rs = 0.5–0.64) between most of LMSQ subclass at p < 0.01.
A cross-sectional study stated that the effectiveness of analgesic, efficacy of medication and patient healthcare provider communication were associated with patient satisfaction [42]. In this study, 58.2% of patients were satisfied with the practicability of analgesic medications. Comparable to this study, a cross-sectional study stated that patients who were prescribed convenient, fast-acting medications were more satisfied [43]. Another study stated that 100% of patients who received sufficient information on analgesic treatment and 97.9% of patients who received sufficient information about the side effects of analgesic treatment were satisfied with cancer pain management [44]. Patients who were satisfied with their pain levels reported statistically lower mean pain scores (2.26 ± 1.70) compared to those not satisfied (4.68 ± 2.07) or not sure (4.21 ± 2.21) [27]. This may be explained by the impact of pain on daily activity. Patients who report a lower average pain score may have a lower impact of pain on physical activity compared to those who report a higher mean pain score. Another study also supports this evidence and states that patients who reported a severe pain score and lower quality of life had lower satisfaction with the treatment received [45].
As a secondary outcome, only 16% of patients were diagnosed to have stage I cancer. This finding could indirectly indicate that there were delays in cancer diagnosis at earlier stage. Further studies may be required to underpin this finding.
In this study, baseline pain before analgesic treatment was not assessed and documented. As a cross-sectional study, we could not draw a cause-and-effect conclusion. Since questions that were used to measure oncologic pain treatment satisfaction were self-reported, answers to each question might not be trustful. The expectation and opinion of the interviewer also might affect the result of the study. These could be potential limitations of the study.
Conclusions
Despite the fact that most cancer patients reported moderate to severe pain, there was a high rate of satisfaction with cancer pain treatment. It would be better if hospitals, healthcare professionals, and administrators took measures to enhance the use of multimodal analgesia in combination with strong opioids to ensure adequate pain management, lower pain severity scores, and better daily life. We also urge the arrangement of better social support mechanisms for cancer patients, the improvement of information provision, and the deployment of professionals who have trained in pain management discipline at cancer care centres.
Data availability
Data and materials used in this study are available and can be presented by the corresponding author upon reasonable request.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- COR:
-
Crude Odds Ratio
- CI:
-
Confidence Interval
- DCSH:
-
Dessie Compressive and Specialized Hospital
- FHCSH:
-
Felege-Hiwot Compressive and Specialized Hospital
- IQR:
-
Inter-quartile Range
- LMSQ:
-
Lubeck Medication Satisfaction Questionnaire
- NRS:
-
Numerical Rating Scale
- PMI:
-
Pain Management Index
- SD:
-
Standard Deviation
- TGCSH:
-
Tibebe-Ghion Compressive and Specialized Hospital
- UoGCSH:
-
University of Gondar Compressive and Specialized Hospital
- WHO:
-
World health organization
References
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–82.
Brown MR, Ramirez JD, Farquhar-Smith P. Pain in cancer survivors. Br J pain. 2014;8(4):139–53.
Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ. Update on Prevalence of Pain in Patients With Cancer: Systematic Review and Meta-Analysis. Journal of pain and symptom management. 2016;51(6):1070-90.e9.
Snijders RAH, Brom L, Theunissen M, van den Beuken-van Everdingen MHJ. Update on Prevalence of Pain in patients with Cancer 2022: a systematic literature review and Meta-analysis. Cancers. 2023;15(3).
Falk S, Dickenson AH. Pain and nociception: mechanisms of cancer-induced bone pain. J Clin Oncol. 2014;32(16):1647–54.
Gibson S, McConigley R. Unplanned oncology admissions within 14 days of non-surgical discharge: a retrospective study. Support Care Cancer. 2016;24:311–7.
Oliveira KG, von Zeidler SV, Podestá JRV, Sena A, Souza ED, Lenzi J, et al. Influence of pain severity on the quality of life in patients with head and neck cancer before antineoplastic therapy. BMC Cancer. 2014;14(1):39.
Smith MD, Meredith PJ, Chua SY. The experience of persistent pain and quality of life among women following treatment for breast cancer: an attachment perspective. Psycho-oncology. 2018;27(10):2442–9.
Zylla D, Steele G, Gupta P. A systematic review of the impact of pain on overall survival in patients with cancer. Support Care Cancer. 2017;25(5):1687–98.
Greco MT, Roberto A, Corli O, Deandrea S, Bandieri E, Cavuto S, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32(36):4149–54.
Baker TA, Krok-Schoen JL, O’Connor ML, Brooks AK. The influence of pain severity and interference on satisfaction with pain management among middle-aged and older adults. Pain Research and Management. 2016;2016.
Baker TA, O’Connor ML, Roker R, Krok JL. Satisfaction with pain treatment in older cancer patients: identifying variants of discrimination, trust, communication, and self-efficacy. J Hospice Palliat Nursing: JHPN: Official J Hospice Palliat Nurses Association. 2013;15(8).
Naidu A. Factors affecting patient satisfaction and healthcare quality. Int J Health care Qual Assur. 2009.
Davies A, Zeppetella G, Andersen S, Damkier A, Vejlgaard T, Nauck F, et al. Multi-centre European study of breakthrough cancer pain: pain characteristics and patient perceptions of current and potential management strategies. Eur J Pain. 2011;15(7):756–63.
Thinh DHQ, Sriraj W, Mansor M, Tan KH, Irawan C, Kurnianda J et al. Patient and physician satisfaction with analgesic treatment: findings from the analgesic treatment for cancer pain in Southeast Asia (ACE) study. Pain Research and Management. 2018;2018.
Kaggwa AT, Kituyi PW, Muteti EN, Ayumba RB. Cancer-related Bone Pain: patients’ satisfaction with analgesic Pain Control. Annals Afr Surg. 2022;19(3):144–52.
Adugna DG, Ayelign AA, Woldie HF, Aragie H, Tafesse E, Melese EB et al. Prevalence and associated factors of cancer pain among adult cancer patients evaluated at the Oncology unit in the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Front Pain Res.3:231.
Tuem KB, Gebremeskel L, Hiluf K, Arko K, Hailu HG. Adequacy of cancer-related pain treatments and factors affecting proper management in Ayder Comprehensive Specialized Hospital, Mekelle, Ethiopia. Journal of Oncology. 2020;2020.
Matrisch L, Rau Y, Karsten H, Graßhoff H, Riemekasten G. The Lübeck medication satisfaction Questionnaire—A Novel Measurement Tool for Therapy satisfaction. J Personalized Med. 2023;13(3):505.
Bayable SD, Ahmed SA, Lema GF, Yaregal Melesse D. Assessment of Maternal Satisfaction and Associated Factors among Parturients Who Underwent Cesarean Delivery under Spinal Anesthesia at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia, 2019. Anesthesiology research and practice. 2020;2020:8697651.
Breivik H, Borchgrevink P-C, Allen S-M, Rosseland L-A, Romundstad L, Breivik Hals E, et al. Assessment of pain. BJA: Br J Anaesth. 2008;101(1):17–24.
Tegegn HG, Gebreyohannes EA. Cancer Pain Management and Pain Interference with Daily Functioning among Cancer patients in Gondar University Hospital. Pain Res Manage. 2017;2017:5698640.
Shen W-C, Chen J-S, Shao Y-Y, Lee K-D, Chiou T-J, Sung Y-C, et al. Impact of undertreatment of cancer pain with analgesic drugs on patient outcomes: a nationwide survey of outpatient cancer patient care in Taiwan. J Pain Symptom Manag. 2017;54(1):55–65. e1.
Gordon DB, Polomano RC, Pellino TA, Turk DC, McCracken LM, Sherwood G, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010;11(11):1172–86.
Thronæs M, Balstad TR, Brunelli C, Løhre ET, Klepstad P, Vagnildhaug OM, et al. Pain management index (PMI)—does it reflect cancer patients’ wish for focus on pain? Support Care Cancer. 2020;28:1675–84.
Mazzotta M, Filetti M, Piras M, Mercadante S, Marchetti P, Giusti R. Patients’ satisfaction with breakthrough cancer pain therapy: A secondary analysis of IOPS-MS study. Cancer Manage Res. 2022:1237–45.
Golas M, Park CG, Wilkie DJ. Patient satisfaction with Pain Level in patients with Cancer. Pain Manage Nursing: Official J Am Soc Pain Manage Nurses. 2016;17(3):218–25.
Tang ST, Tang W-R, Liu T-W, Lin C-P, Chen J-S. What really matters in pain management for terminally ill cancer patients in Taiwan. J Palliat Care. 2010;26(3):151–8.
Kharel S, Adhikari I, Shrestha K. Satisfaction on Pain Management among Cancer patient in selected Cancer Care Center Bhaktapur Nepal. Int J Med Sci Clin Res Stud. 2023;3(4):597–603.
Breivik H, Eisenberg E, O’Brien T. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013;13:1–14.
Gonzalez-Saenz de Tejada M, Bilbao A, Baré M, Briones E, Sarasqueta C, Quintana J, et al. Association between social support, functional status, and change in health‐related quality of life and changes in anxiety and depression in colorectal cancer patients. Psycho‐oncology. 2017;26(9):1263–9.
Yoo H, Shin DW, Jeong A, Kim SY, Yang H-k, Kim JS, et al. Perceived social support and its impact on depression and health-related quality of life: a comparison between cancer patients and general population. Jpn J Clin Oncol. 2017;47(8):728–34.
Hanna MN, González-Fernández M, Barrett AD, Williams KA, Pronovost P. Does patient perception of pain control affect patient satisfaction across surgical units in a tertiary teaching hospital? Am J Med Qual. 2012;27(5):411–6.
Naveh P. Pain severity, satisfaction with pain management, and patient-related barriers to pain management in patients with cancer in Israel. Number 4/July 2011. 2011;38(4):E305–13.
Black B, Herr K, Fine P, Sanders S, Tang X, Bergen-Jackson K, et al. The relationships among pain, nonpain symptoms, and quality of life measures in older adults with cancer receiving hospice care. Pain Med. 2011;12(6):880–9.
Kelly A-M. Patient satisfaction with pain management does not correlate with initial or discharge VAS pain score, verbal pain rating at discharge, or change in VAS score in the emergency department. J Emerg Med. 2000;19(2):113–6.
Lin J, Hsieh RK, Chen JS, Lee KD, Rau KM, Shao YY, et al. Satisfaction with pain management and impact of pain on quality of life in cancer patients. Asia-Pac J Clin Oncol. 2020;16(2):e91–8.
Su W-C, Chuang C-H, Chen F-M, Tsai H-L, Huang C-W, Chang T-K, et al. Effects of Good Pain Management (GPM) ward program on patterns of care and pain control in patients with cancer pain in Taiwan. Support Care Cancer. 2021;29(4):1903–11.
Prip A, Møller KA, Nielsen DL, Jarden M, Olsen M-H, Danielsen AK. The patient–healthcare professional relationship and communication in the oncology outpatient setting: a systematic review. Cancer Nurs. 2018;41(5):E11.
Orujlu S, Hassankhani H, Rahmani A, Sanaat Z, Dadashzadeh A, Allahbakhshian A. Barriers to cancer pain management from the perspective of patients: a qualitative study. Nurs open. 2022;9(1):541–9.
Uysal N. Clearing barriers in Cancer Pain Management: roles of nurses. Int J Caring Sci. 2018;11(2).
Beck SL, Towsley GL, Berry PH, Lindau K, Field RB, Jensen S. Core aspects of satisfaction with pain management: cancer patients’ perspectives. J Pain Symptom Manag. 2010;39(1):100–15.
Wada N, Handa S, Yamamoto H, Higuchi H, Okamoto K, Sasaki T, et al. Integrating Cancer patients’ satisfaction with Rescue Medication in Pain assessments. Showa Univ J Med Sci. 2020;32(3):181–91.
Antón A, Montalar J, Carulla J, Jara C, Batista N, Camps C, et al. Pain in clinical oncology: patient satisfaction with management of cancer pain. Eur J Pain. 2012;16(3):381–9.
Valero-Cantero I, Casals C, Espinar-Toledo M, Barón-López FJ, Martínez-Valero FJ, Vázquez-Sánchez MÁ. Cancer Patients’ Satisfaction with In-Home Palliative Care and Its Impact on Disease Symptoms. Healthcare. 2023;11(9):1272.
Acknowledgements
We would like to acknowledge the University of Gondar Comprehensive Specialized Hospital, Tibebe-Ghion Comprehensive Specialized Hospital, Felege-Hiwot Comprehensive Specialized Hospital, Dessie Comprehensive Specialized Hospital. We would also want to acknowledge Ludwig Matrisch from the Department of Rheumatology and Clinical Immunology, Universität zu Lübeck, 23562 Lübeck, Germany for supporting us on the utilization of the Lübeck Medication Satisfaction Questionnaire (LMSQ) ludwig@matrisch.de,
Funding
This study was supported by University of Gondar and Debre Birhan University with no conflict of interest. The support did not include publication charges.
Author information
Authors and Affiliations
Contributions
‘’M.A. has conceptualized the study and objectives; and developed the proposal. Y.W.B., H.E.A., and A.B.G. criticized the proposal. All authors had participated in the data management and statistical analyses. Y.W.B, M.A., and H.E.A. have prepared the final manuscript. All authors read and approved the final manuscript.‘’.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Review Committee of the School of Medicine, at the University of Gondar (Reference number: CMHS/SM/06/01/4097/2015, Date: March 24, 2023). Permission support letters were obtained from FHCSH, TGCSH, and DCSH. Written informed consent was obtained from each participant after detailed explanations about the study. Informed consent with a fingerprint signature was obtained from patients who could not read or write after detailed explanations by the data collectors as approved by the Ethical Review Committee of the School of Medicine, at the University of Gondar.
Consent for publication
Not applicable; this article does not include any personal details of any participant.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amsalu, M., Ashagrie, H.E., Getahun, A.B. et al. Patients’ satisfaction with cancer pain treatment at adult oncologic centers in Northern Ethiopia; a multi-center cross-sectional study. BMC Cancer 24, 647 (2024). https://doi.org/10.1186/s12885-024-12359-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12359-7