Abstract
Purpose
Poor adherence to analgesic drugs is one of the most common barriers to adequate pain management. This prospective, cross-sectional, patient-oriented observational study aimed to explore the adherence rate, clinical factors, and impact of adherence to analgesic drugs on the quality of life (QoL) among cancer outpatients in Taiwan.
Methods
Eight hundred ninety-seven consecutive adult outpatients with cancer who had reported tumor pain and received regular analgesic drug treatment were enrolled from 16 medical centers across Taiwan. The Brief Pain Inventory was used to assess pain intensity and QoL. Morisky’s four-item medication adherence scale was used to assess adherence to analgesic drugs. Clinical factors possibly associated with good adherence to analgesic drugs were analyzed using multivariate logistic regression analyses.
Results
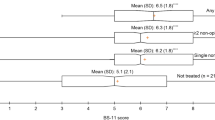
Of the 897 patients, 26.9% met criteria for the good, 35.5% for the moderate, and 37.6% for the poor adherence groups. The good adherence group had significantly better QoL outcomes than the moderate and poor adherence groups (all p < 0.05). Age ≥ 50 years, head and neck or hematological malignancies, cancer-related pain, patients who agreed or strongly agreed that the side effects of analgesic drugs were tolerable, and patients who disagreed or strongly disagreed that the dosing schedule could be flexibly self-adjusted to deal with the actual pain were predictors of good adherence to analgesic drugs.
Conclusions
Awareness of the clinical factors associated with adherence to analgesic drugs may help clinicians to identify cancer patients at a greater risk of non-adherence, reinforce optimal pain management, and improve the QoL by enhancing adherence to pain medications.




Similar content being viewed by others
References
van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J (2007) High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain 132(3):312–320
van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J (2007) Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 18(9):1437–1449
Teunissen SC, Wesker W, Kruitwagen C, de Haes HC, Voest EE, de Graeff A (2007) Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manag 34(1):94–104
Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, Dale O, de Conno F, Fallon M, Hanna M, Haugen DF, Juhl G, King S, Klepstad P, Laugsand EA, Maltoni M, Mercadante S, Nabal M, Pigni A, Radbruch L, Reid C, Sjogren P, Stone PC, Tassinari D, Zeppetella G (2012) Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol 13(2):e58–e68
Ripamonti CI, Bandieri E, Roila F, ESMO Guidelines Working Group (2011) Management of cancer pain: ESMO clinical practice guidelines. In: Ann Oncol 22 Suppl 6:vi69–77
Greco MT, Roberto A, Corli O, Deandrea S, Bandieri E, Cavuto S, Apolone G (2014) Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol 32(36):4149–4154
Deandrea S, Montanari M, Moja L, Apolone G (2008) Prevalence of under-treatment in cancer pain. A review of published literature. Ann Oncol 19(12):1985–1991
National Health Research Institutes and Taiwan Cooperative Oncology Group. Clinical guideline for management of cancer pain, 1st ed (2007). Miaoli County, Taiwan. Available at: http://www.nhri.org.tw/NHRI_ADM/userfiles/file/tcog/pain(2).pdf. Accessed 01 February 2018
Hsieh RK (2005) Pain control in Taiwanese patients with cancer: a multicenter, patient-oriented survey. J Formos Med Assoc 104(12):913–919
Rau KM, Chen JS, Wu HB, Lin SF, Lai MK, Chow JM, Huang ML, Wang CJ, Tai CJ, Hwang WL, Lu YC, Chan CH, Hsieh RK (2015) The impact of pain control on physical and psychiatric functions of cancer patients: a nation-wide survey in Taiwan. Jpn J Clin Oncol 45(11):1042–1049
Shen WC, Chen JS, Shao YY, Lee KD, Chiou TJ, Sung YC, Rau KM, Yen CJ, Liao YM, Liu TC, Wu MF, Lee MY, Yu MS, Hwang WL, Lai PY, Chang CS, Chou WC, Hsieh RK (2017) Impact of undertreatment of cancer pain with analgesic drugs on patient outcomes: a nationwide survey of outpatient cancer patient care in Taiwan. J Pain Symptom Manag 54(1):55–65
Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S (2001) Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain 93(3):247–257
Jamison RN, Sheehan KA, Scanlan E, Matthews M, Ross EL (2014) Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag 10(6):375–382
Potter VT, Wiseman CE, Dunn SM, Boyle FM (2003) Patient barriers to optimal cancer pain control. Psychooncology 12(2):153–160
Liang SY, Yates P, Edwards H, Tsay SL (2008) Factors influencing opioid-taking self-efficacy and analgesic adherence in Taiwanese outpatients with cancer. Psychooncology 17(11):1100–1107
Lin CC (2000) Barriers to the analgesic management of cancer pain: a comparison of attitudes of Taiwanese patients and their family caregivers. Pain 88(1):7–14
Gunnarsdottir S, Donovan HS, Serlin RC, Voge C, Ward S (2002) Patient-related barriers to pain management: the Barriers Questionnaire II (BQ-II). Pain 99(3):385–396
Lee BO, Liu Y, Wang YH, Hsu HT, Chen CL, Chou PL, Hsu WC (2015) Mediating effect of family caregivers’ hesitancy to use analgesics on homecare cancer patients' analgesic adherence. J Pain Symptom Manag 50(6):814–821
Corli O, Montanari M, Deandrea S, Greco MT, Villani W, Apolone G (2012) An exploratory analysis on the effectiveness of four strong opioids in patients with cancer pain. Pain Med 13(7):897–907
Miaskowski C, Dodd MJ, West C, Paul SM, Tripathy D, Koo P, Schumacher K (2001) Lack of adherence with the analgesic regimen: a significant barrier to effective cancer pain management. J Clin Oncol 19(23):4275–4279
Valeberg BT, Miaskowski C, Hanestad BR, Bjordal K, Moum T, Rustoen T (2008) Prevalence rates for and predictors of self-reported adherence of oncology outpatients with analgesic medications. Clin J Pain 24(7):627–636
Graziottin A, Gardner-Nix J, Stumpf M, Berliner MN (2011) Opioids: how to improve compliance and adherence. Pain Pract 11(6):574–581
Daut RL, Cleeland CS, Flanery RC (1983) Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain 17(2):197–210
Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330(9):592–596
Morisky DE, Green LW, Levine DM (1986) Concurrent and predictive validity of a self- reported measure of medication adherence. Med Care 24(1):67–74
Tzeng JI, Chang CC, Chang HJ, Lin CC (2008) Assessing analgesic regimen adherence with the Morisky Medication Adherence Measure for Taiwanese patients with cancer pain. J Pain Symptom Manag 36(2):157–166
Schmid H, Hartmann B, Schiffl H (2009) Adherence to prescribed oral medication in adult patients undergoing chronic hemodialysis: a critical review of the literature. Eur J Med Res 14(5):185–190
McHorney CA (2009) The Adherence Estimator: a brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin 25(1):215–238
Zhang H, Singer B (1999) Recursive partitioning in the health sciences. In: Analysis of censored data: survival trees. Springer, New York, pp 93–104
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353(5):487–497
Meghani SH, Thompson AM, Chittams J, Bruner DW, Riegel B (2015) Adherence to analgesics for cancer pain: a comparative study of African Americans and Whites using an electronic monitoring device. J Pain 16(9):825–835
Ogrodniczuk JS, Piper WE, Joyce AS (2006) Treatment compliance in different types of group psychotherapy: exploring the effect of age. J Nerv Ment Dis 194(4):287–293
Ktsanas D, Al-Souffi MH, Waxman BP, King RW, Polkinghorne KR, Woolley IJ (2006) Adherence to guidelines for prevention of postsplenectomy sepsis. Age and sex are risk factors: a five-year retrospective review. ANZ J Surg 76(7):542–547
Ward SE, Golberg N, Miller-McCauley V et al (1993) Patient-related barriers to management of cancer pain. Pain 52(3):319–324
Cohen HW, Shmukler C, Ullman R, Rivera CM, Walker EA (2010) Measurements of medication adherence in diabetic patients with poorly controlled HbA(1c). Diabet Med 27(2):210–216
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
The authors gratefully acknowledge the assistance of the patients who participated in this study, and support grants from the Taiwan Society of Cancer Palliative Medicine and Johnson & Johnson.
Conflicts of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Chou, WC., Chen, JS., Hung, CY. et al. A nationwide survey of adherence to analgesic drugs among cancer patients in Taiwan: prevalence, determinants, and impact on quality of life. Support Care Cancer 27, 2857–2867 (2019). https://doi.org/10.1007/s00520-018-4599-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4599-x