Abstract
Background
Postoperative adjuvant chemotherapy (AC) is now well-accepted as standard for high-risk stage II and stage III colorectal cancer (CRC) patients, however the optimal time to initiate AC remains elusive.
Methods
A comprehensive literature search was performed using the PubMed and Embase databases. The Hazard ratio (HR) with the corresponding 95% confidence interval (CI) was used as an effect measure to evaluate primary endpoints. All analyses were conducted using Stata software version 12.0 with the Random-effects model.
Results
A total of 30 studies were included in our study. Upon comparison on overall survival (OS), we identified that delaying the initiation of AC for > 8 weeks after operation was significantly associated with poor OS (HR: 1.37; 95% CI: 1.27—1.48; P < 0.01). The poor prognostic value of AC delay for > 8 weeks was not undermined by subgroup analysis based on region, tumor site, sample size and study quality. No obvious differences were observed in survival between AC within 5–8 weeks and ≤ 4 weeks (HR: 1.03; 95% CI: 0.96 -1.10; P = 0.46). Moreover, two studies both highlighted that the survival benefit of AC was still statistically significant when AC was applied 5–6 months after surgery compared with the non-chemotherapy group.
Conclusions
Delaying the initiation of AC for > 8 weeks after surgery was significantly associated with poor OS. AC started within 8 weeks after surgery brought more benefits to CRC patients. There were no obvious differences in survival benefits between AC within 5–8 weeks and ≤ 4 weeks. Compared to patients not receiving AC after surgery, a delay of approximately 5–6 months was still useful to improve prognosis.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is one of the most aggressive gastrointestinal tract cancers and the incidence and mortality rank third and second, respectively [1]. For patients with high-risk stage II and stage III CRC, 5-flurouracil-based adjuvant chemotherapy (AC), which has been verified to decrease the risk of recurrence and cancer associated death via eliminating tumor micro-metastasis [2, 3], was recommended to applied following radical surgery by the National Comprehensive Cancer Network (NCCN).
Recently, the result of the International Duration Evaluation of Adjuvant Therapy (IDEA) study fueled interests in specifying the timing and duration of AC after surgery [4, 5]. With no recommendations provided in NCCN guidelines, AC was generally initiated 6–8 weeks after surgery in most clinical trials. However, delays frequently occurred in daily practice for various reasons [6]. Previously, two meta-analyses demonstrated that postponing the postoperative AC was associated with poor survival in CRC patients. Result from Biagi et al. showed that each 4 weeks delay result in a 14% decrease of overall survival (OS) [7]. Similarly, Guetz’s study indicated that delaying the initiation of AC for > 8 weeks after operation significantly decreased OS [8]. However, owing to limited research data and small sample size, no consensus has been reached on the actual time to start AC after surgery. Recently, studies with larger sample size has been conducted to investigate the impact of the timing of AC on prognosis in CRC, however the results were inconsistent [9,10,11,12]. Therefore, further analysis was needed to instruct clinical practice.
Here in this study, we performed updated meta-analysis, comparing the survival benefits of different time intervals between surgery and postoperative AC (including < 8 weeks vs. > 8 weeks and ≤ 4 weeks vs. 5–8 weeks), to explore the optimal time to initiate AC after surgery. In addition, based on the existing data, the time point at which postoperative AC was no longer beneficial to CRC patients was discussed.
Materials and methods
Literature search
A comprehensive literature search for relevant published studies was performed using the PubMed, Embase databases until February 1st, 2023. The main search terms were “delay”, “interval”, “timing”, “adjuvant chemotherapy”, “colon cancer” and “colorectal cancer”. The references lists of the above articles were also screened.
Inclusion and exclusion criteria
The eligible studies were enrolled in this study according to PICOS criteria (population, intervention, comparison, outcomes and study design): (1) Population: patients were definitely diagnosed with colon cancer, rectal cancer or colorectal cancer; (2) Intervention: delayed adjuvant chemotherapy; (3) Comparison: colon cancer or colorectal cancer patients with delayed adjuvant chemotherapy in the experimental group versus those without delay in the control group; (4) Outcomes: OS, relapse-free survival (RFS), disease-free survival (DFS), cancer specific-survival (CSS); (5) Study design: comparative studies based on patients with delayed adjuvant chemotherapy and adjuvant chemotherapy without delay. Studies were excluded following exclusion criteria: (1) duplicated articles based on the same patient population or database (studies with different outcomes would be included); (2) studies whose outcome was not reported or impossible to estimate outcomes from the original data; (3) studies with insufficient information (including abstracts or reports from meeting); (4) meta-analyses and reviews.
Data extraction and assessment of study quality
Two authors reviewed each eligible study and extracted the data independently, and any disagreements were resolved via discussion. Following information was extracted from eligible studies: population year and country, the first author, study design, sample size and source, age and sex of patients, adjuvant chemotherapy regimens, delayed time of adjuvant chemotherapy and survival benefits. The Newcastle–Ottawa scale (NOS) was used to evaluate the quality of eligible studies [13]. Studies with NOS scores ≥ 6 (median score) were assigned as high-quality study (Table S1).
Statistical analysis
Hazard ratios (HRs) and their 95% confidence intervals (CIs) were used as effect measures to evaluate the primary endpoints (time-to-event outcomes). The method of Tierney was adopted to estimate the HR and 95% CI for those studies in which the HR cannot be extracted directly [14]. All analyses were conducted using the Random-effects model with the method of DerSimonian and Laird. Cochran’s Q test and I2 statistics were applied to evaluate statistical heterogeneity. Begg’s and Egger’s tests were used to calculate the effect of publication bias. Sensitivity analysis was performed to assess robustness and reliability of the combined outcomes. All analyses were conducted using the Review Manager 5.2 software (Copenhagen—The Nordic Cochrane Centre; The Cochrane Collaboration, 2012) and STATA software (version 12.0; Stata Corporation, College Station, TX, USA). All statistical tests were two-sided and a P-value of less than 0.05 was considered statistically significant.
Result
Search results and study characteristics
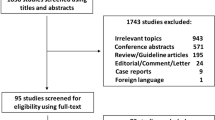
A total of 317 potentially relevant articles were initially identified from database searches. Ruling out 130 duplicated studies, 187 studies underwent detailed review. After reviewing the titles and abstracts, 126 studies were further removed. Then 31 studies were excluded based on the inclusion and exclusion criteria after full text review. Finally, a total of 30 studies were included in our study [9,10,11,12, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] (Fig. 1).
These studies were published between 2005 and 2023. Aside from seven studies based on Asian populations, 23 studies were performed on Western population (including US, UK, France, Canada, Denmark and Brazil). 29 studies were retrospective cohort studies, and one study was a secondary analysis on a randomized trial. The median sample size was 1053 (Range 102–51,250). Study quality was judged based on the Newcastle–Ottawa Scale (Table S1). The characteristics of these selected studies were summarized in Table 1.
Quantitative synthesis
< 8 weeks vs. > 8 weeks
For survival comparison, a total of 18 studies can be stratified according to a common cut-off of 8 weeks’ interval between operation and adjuvant chemotherapy. Upon summarizing above studies, we found that the 5-year OS rate was higher in patients receiving AC in < 8 weeks after surgery than those starting the AC in > 8 weeks after surgery (Table S2). Moreover, the result of meta-analysis suggested that postponing the initiation of AC for > 8 weeks after operation was associated with significantly shorter OS (HR: 1.37; 95% CI: 1.27—1.48; P < 0.01, Fig. 2A, Table 2). Then the Begg’s and Egger’s tests confirmed the absence of publication bias (Figure S1A, Figure S1B). Sensitivity analysis was performed to evaluate the robustness of our findings. The pooled HR for OS was stable, indicating that the results were reliable (Figure S1C).
a Forest plot assessing overall survival and sharing a common cutoff delay of 8 weeks between surgery and adjuvant chemotherapy. Hazard Ratio (HR) > 1 indicates a worse survival for delayed adjuvant chemotherapy. b Forest plot assessing relapse-free survival and sharing a common cut-off delay of 8 weeks between surgery and adjuvant chemotherapy. Hazard Ratio (HR) > 1 indicates a worse survival for delayed adjuvant chemotherapy
Subgroup analyses were stratified by region (Asian vs. non-Asian), tumor site (colon vs. rectum), sample size (≥ 1000 vs. < 1000), and study quality (≥ 6 vs. < 6). Patients who started the AC in < 8 weeks after surgery showed longer OS compared to those receiving the AC in > 8 weeks after surgery in all prespecified clinical subgroups. The pooled results confirmed the poor prognostic role of receiving AC in > 8 weeks after surgery on OS in CRC (Table 2, Fig. 3).
Forest plot of hazard ratios in subgroup analyses by region, tumor site, sample size and study quality comparing overall survival in patients receiving adjuvant chemotherapy in > 8 weeks versus those receiving adjuvant chemotherapy in < 8 weeks after surgery. Hazard Ratio (HR) > 1 indicates a worse survival for delayed adjuvant chemotherapy
For recurrence investigation, 3 studies can be stratified according to a cut-off of 8 weeks’ interval. The pooled result demonstrated that patients receiving AC in < 8 weeks after surgery had a lower risk of recurrence with longer RFS than those receiving AC in > 8 weeks after surgery, although the difference was not statistically significant (HR: 1.41; 95% CI: 0.90—2.21; P = 0.13, Fig. 2B). The results about 5-year RFS of these 3 studies are listed in Table S3.
5–8 weeks vs. ≤ 4 weeks
5 studies were enrolled in the comparison of prognosis following two groups: patients receiving AC in ≤ 4 weeks after surgery and patients starting AC in 5–8 weeks after surgery. We found that compared with receiving AC in ≤ 4 weeks after surgery, starting AC in 5–8 weeks was not significantly associated with OS benefits (HR: 1.03; 95% CI: 0.96 -1.10; P = 0.46, Fig. 4). Indeed, the summary table showed that 5-year OS was similar in two groups (Table S4).
Discussion
According to this updated meta-analysis, delaying initiation of AC after surgery for > 8 weeks was significantly associated with poorer OS. The negative prognostic indication value of delaying initiation of AC for > 8 weeks was not undermined by subgroup analysis based on region, tumor site, sample size and study quality. In addition, publication bias absence verified by Begg’s and Egger’s tests together with sensitivity analysis confirmed the stability and reliability of results from this study.
AC is nowadays well acknowledged as inhibiting tumor growth and prolonging survival after surgery in CRC patients. Some studies reported that trauma by surgery could promote residual tumor growth and tumor metastasis by releasing growth-stimulating factors and triggering immunosuppression [41, 42]. Studies also have shown that surgical trauma can cause an increase in transforming growth factor α (TGFα), which plays an important role in colorectal tumor invasion and metastasis [43, 44]. In vivo experiments on mouse model confirmed that growth factors in healing wounds may promote tumor growth, affecting therapeutic effect of immunotherapy with interleukin-2 (IL-2) and lympokine activated killer (LAK) cells [45, 46]. Therefore, a prolonged interval between operation and AC may lead to the tumor growth and micro-metastases [9]. Moreover, in the blood of some CRC patients after surgery, circulating tumor cells (CTC) or circulating tumor DNA (ctDNA) were detected, and RFS of these patients was significantly reduced [47,48,49,50]. About 25% of minimal residual disease (MRD) positive patients can achieve ctDNA clearance through adjuvant infusional fluorouracil, leucovorin, and oxaliplatin chemotherapy, making contributions to improve survival [51, 52].
Important gap remains in our knowledge on mechanical association between the timing of AC and prognosis. There are several possible reasons. Firstly, as mentioned above, residual tumor-promoting cytokines and MRD after surgery are possible drivers for tumor recurrence and metastasis. Given that growth rate is higher in early stage, early intervention with AC may suppress the tumor growth and dissemination [53]. Secondly, with classic mathematical model, Goldie et al. demonstrated that aside from mutation rate of tumor cells and sizes, time is also one major contributor to mutation associated drug resistance [54]. Third, Farzaneh et al. found that patients in delayed AC group had a higher proportion of positive surgical margin, one important factor for poor prognosis in locally advanced CRC [38]. Harless and colleagues reported the effectiveness of AC was inversely proportional to the interval between surgery and AC initiation [55]. Finally, therapy delay is usually induced due to poor nutritional and performance statuses of patients, which may also contribute to poor clinical outcomes. Whether AC delay is a cause or a consequence of poor prognosis for these patients remains unknown.
Combined with previous studies, our study verified the inverse association of prolonged interval between surgery and AC and survival of patients. While in clinical practice, situation is more complex as therapeutic toxicity may be maximized owning to patient’s poor immune and performance status after operation. Early postoperative intervention may lead to severe chemotherapy-related adverse events and even death [56]. Therefore, the survival benefit of AC may be time-dependent [10]. In parallel with results from another meta-analysis by Guetz et al. [8], our study also suggested that AC should be started within 8 weeks after surgery. However, little evidence is available on optimal timepoint to start AC after surgery. Our pooled result showed that 5–8 weeks’ interval between AC and surgery did not increase the risk of mortality compared with that less than 4 weeks, and the 5-year OS was similar between two groups. On the other hand, Bos et al. [29] compared the survival of two cohorts, one with 2,950 patients receiving AC 5–6 weeks after surgery and the other with 1,562 patients receiving AC 7–8 weeks after operation, and found that the 5-year OS was slightly higher in the former one (76% vs. 73%). Generally, patients with colorectal surgery need a recovery period of at least 2–4 weeks for wound healing, physical recovery and treatment of postoperative complication. In sum, we hypothesized that 5–6 weeks’ interval may be more reasonable as it may be the optimal choice taking these factors into consideration. Deeper investigations are warranted for further validation.
Until now, the postoperative time point at which AC is no longer beneficial to CRC patients is unclear. In the study performed by Biagi and colleagues, they found that patients starting AC > 12 weeks exhibited better survival compared with patients not receiving AC, and posited a prognostic benefit at 4 or 5 months, which was longer than that commonly recommended in clinical practice [7]. Based on a total of 18,491 patients, Gao’s group showed that the survival benefit of AC was still statistically significant when initiated more than 20 weeks after operation compared with the non-chemotherapy group, thus, AC might be still beneficial with a delay of 5 months [10]. While Turner reported that 489 patients who initiated AC > 24 weeks had a significantly better OS than 20,807 patients who omitted chemotherapy [11]. Therefore, the above mentioned results indicated that AC might still be useful even with a delay of 5–6 months. These results should be confirmed by more studies in the future.
Limitations exist in our study. First, as randomized trial design of postponing AC is neither ethical nor feasible, most of the included studies in this study were retrospective cohort studies, and one was a secondary analysis from a randomized trial. Second, owning to the detailed information availability and limitations of the size and number of studies, we could not perform other subgroup analyses (such as stage III vs. stage II with high-risk features). Third, the cut-offs of time interval among selected studies were different. Besides, with great breakthroughs on CRC postoperative chemotherapy in the last decades, the adjuvant therapy regimen has changed. As 5-fluorouracil-based chemotherapy regimen was mostly used in previous studies while two-drug combination chemotherapy regimen, such as oxaliplatin plus capecitabine, is more commonly used currently. Whether different AC regimens make differences on the choice of initiation time point remains to be determined.
Conclusions
In conclusion, delaying the initiation of AC for > 8 weeks after surgery was significantly associated with poor OS. AC started within 8 weeks after surgery brought more benefits to CRC patients. There were no obvious differences in survival benefits between AC within 5–8 weeks and ≤ 4 weeks. Compared to patients not receiving AC after surgery, a delay of approximately 5–6 months was still useful to improve prognosis.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CRC:
-
Colorectal cancer
- NCCN:
-
National Comprehensive Cancer Network
- AC:
-
Adjuvant chemotherapy
- IDEA:
-
International Duration Evaluation of Adjuvant Therapy
- OS:
-
Overall survival
- RFS:
-
Relapse-free survival
- DFS:
-
Disease-free survival
- CSS:
-
Cancer specific-survival
- NOS:
-
Newcastle-Ottawa scale
- HR:
-
Hazard ratios
- CI:
-
Confidence interval
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Benson AB 3rd, Schrag D, Somerfield MR, Cohen AM, Figueredo AT, Flynn PJ, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408–19.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. Colon cancer, Version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021;19(3):329–59.
Grothey A, Sobrero AF, Shields AF, Yoshino T, Paul J, Taieb J, et al. duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378(13):1177–88.
Spiegel DY, Boyer MJ, Hong JC, Williams CD, Kelley MJ, Salama JK, et al. Survival advantage with adjuvant chemotherapy for locoregionally advanced rectal cancer: a veterans health administration analysis. J Natl Compr Canc Netw. 2020;18(1):52–8.
Malietzis G, Mughal A, Currie AC, Anyamene N, Kennedy RH, Athanasiou T, et al. Factors implicated for delay of adjuvant chemotherapy in colorectal cancer: a meta-analysis of observational studies. Ann Surg Oncol. 2015;22(12):3793–802.
Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011;305(22):2335–42.
Des Guetz G, Nicolas P, Perret GY, Morere JF, Uzzan B. Does delaying adjuvant chemotherapy after curative surgery for colorectal cancer impair survival? A meta-analysis. Eur J Cancer (Oxford, England : 1990). 2010;46(6):1049–55.
Sun Z, Adam MA, Kim J, Nussbaum DP, Benrashid E, Mantyh CR, et al. Determining the optimal timing for initiation of adjuvant chemotherapy after resection for stage II and III colon cancer. Dis Colon Rectum. 2016;59(2):87–93.
Gao P, Huang XZ, Song YX, Sun JX, Chen XW, Sun Y, et al. Impact of timing of adjuvant chemotherapy on survival in stage III colon cancer: a population-based study. BMC Cancer. 2018;18(1):234.
Turner MC, Farrow NE, Rhodin KE, Sun Z, Adam MA, Mantyh CR, et al. Delay in adjuvant chemotherapy and survival advantage in stage III colon cancer. BMC Cancer. 2018;226(4):670–8.
Dos Santos LV, Faria TM, Lima AB, Abdalla KC, de Moraes ED, Cruz MR, et al. Timing of adjuvant chemotherapy in colorectal cancer. Colorectal Dis. 2016;18(9):871–6.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Chau I, Norman AR, Cunningham D, Tait D, Ross PJ, Iveson T, et al. A randomised comparison between 6 months of bolus fluorouracil/leucovorin and 12 weeks of protracted venous infusion fluorouracil as adjuvant treatment in colorectal cancer. Ann Oncol. 2005;16(4):549–57.
Andre T, Quinaux E, Louvet C, Colin P, Gamelin E, Bouche O, et al. Phase III study comparing a semimonthly with a monthly regimen of fluorouracil and leucovorin as adjuvant treatment for stage II and III colon cancer patients: final results of GERCOR C96.1. J Clin Oncol. 2007;25(24):3732–8.
Berglund A, Cedermark B, Glimelius B. Is it deleterious to delay the start of adjuvant chemotherapy in colon cancer stage III? Ann Oncol. 2008;19(2):400–2.
Cheung WY, Neville BA, Earle CC. Etiology of delays in the initiation of adjuvant chemotherapy and their impact on outcomes for Stage II and III rectal cancer. Dis Colon Rectum. 2009;52(6):1054–63 discussion 64.
Zeig-Owens R, Gershman ST, Knowlton R, Jacobson JS. Survival and time interval from surgery to start of chemotherapy among colon cancer patients. J Registry Manag. 2009;36(2):30–41 quiz 61-2.
Ahmed S, Ahmad I, Zhu T, Arnold FP, Faiz Anan G, Sami A, et al. Early discontinuation but not the timing of adjuvant therapy affects survival of patients with high-risk colorectal cancer: a population-based study. Dis Colon Rectum. 2010;53(10):1432–8.
Bayraktar UD, Chen E, Bayraktar S, Sands LR, Marchetti F, Montero AJ, et al. Does delay of adjuvant chemotherapy impact survival in patients with resected stage II and III colon adenocarcinoma? Cancer. 2011;117(11):2364–70.
Czaykowski PM, Gill S, Kennecke HF, Gordon VL, Turner D. Adjuvant chemotherapy for stage III colon cancer: does timing matter? Dis Colon Rectum. 2011;54(9):1082–9.
Lima IS, Yasui Y, Scarfe A, Winget M. Association between receipt and timing of adjuvant chemotherapy and survival for patients with stage III colon cancer in Alberta. Canada Cancer. 2011;117(16):3833–40.
Kang KM, Hong KS, Noh GT, Oh BY, Chung SS, Lee RA, et al. Optimal time of initiating adjuvant chemotherapy after curative surgery in colorectal cancer patients. Ann Coloproct. 2013;29(4):150–4.
Tevis SE, Kohlnhofer BM, Stringfield S, Foley EF, Harms BA, Heise CP, et al. Postoperative complications in patients with rectal cancer are associated with delays in chemotherapy that lead to worse disease-free and overall survival. Dis Colon Rectum. 2013;56(12):1339–48.
Yu S, Shabihkhani M, Yang D, Thara E, Senagore A, Lenz HJ, et al. Timeliness of adjuvant chemotherapy for stage III adenocarcinoma of the colon: a measure of quality of care. Clin Colorectal Cancer. 2013;12(4):275–9.
Day AR, Middleton G, Smith RV, Jourdan IC, Rockall TA. Time to adjuvant chemotherapy following colorectal cancer resection is associated with an improved survival. Colorectal Dis. 2014;16(5):368–72.
Xu F, Rimm AA, Fu P, Krishnamurthi SS, Cooper GS. The impact of delayed chemotherapy on its completion and survival outcomes in stage II colon cancer patients. PLoS ONE. 2014;9(9):e107993.
Bos AC, van Erning FN, van Gestel YR, Creemers GJ, Punt CJ, van Oijen MG, et al. Timing of adjuvant chemotherapy and its relation to survival among patients with stage III colon cancer. Eur J Cancer. 2015;51(17):2553–61.
Jeong IS, Yoo JH, Seo SH, An MS, Kim KH, Bae KB, et al. Association between time (initiation and length) and oncological outcomes for the patients with colon cancer treated with adjuvant chemotherapy. Indian J Surg. 2015;77(Suppl 3):1252–7.
Jeong WK, Shin JW, Baek SK. Oncologic outcomes of early adjuvant chemotherapy initiation in patients with stage III colon cancer. Ann Surg Treat Res. 2015;89(3):124–30.
Kim IY, Kim BR, Kim YW. Factors affecting use and delay (>/=8 weeks) of adjuvant chemotherapy after colorectal cancer surgery and the impact of chemotherapy-use and delay on oncologic outcomes. PLoS ONE. 2015;10(9):e0138720.
Klein M, Azaquoun N, Jensen BV, Gogenur I. Improved survival with early adjuvant chemotherapy after colonic resection for stage III colonic cancer: a nationwide study. J Surg Oncol. 2015;112(5):538–43.
Nachiappan S, Askari A, Mamidanna R, Munasinghe A, Currie A, Stebbing J, et al. The impact of adjuvant chemotherapy timing on overall survival following colorectal cancer resection. Eur J Surg Oncol. 2015;41(12):1636–44.
Peixoto RD, Kumar A, Speers C, Renouf D, Kennecke HF, Lim HJ, et al. Effect of delay in adjuvant oxaliplatin-based chemotherapy for stage III colon cancer. Clin Colorectal Cancer. 2015;14(1):25–30.
Kim YW, Choi EH, Kim BR, Ko WA, Do YM, Kim IY. The impact of delayed commencement of adjuvant chemotherapy (eight or more weeks) on survival in stage II and III colon cancer: a national population-based cohort study. Oncotarget. 2017;8(45):80061–72.
Choi JH, Lee JS, Baek SK, Kim JG, Kim TW, Sohn SK, et al. Association between Timing and Duration of Adjuvant Chemotherapy and Colorectal Cancer Survival in Korea, 2011–2014: A Nationwide Study based on the Health Insurance Review and Assessment Service Database. J Cancer. 2022;13(8):2440–6.
Farzaneh CA, Pigazzi A, Duong WQ, Carmichael JC, Stamos MJ, Dekhordi-Vakil F, et al. Analysis of delay in adjuvant chemotherapy in locally advanced rectal cancer. Tech Coloproctol. 2023;27(1):35–42.
Becerra AZ, Aquina CT, Mohile SG, Tejani MA, Schymura MJ, Boscoe FP, et al. Variation in Delayed Time to Adjuvant Chemotherapy and Disease-Specific Survival in Stage III Colon Cancer Patients. Ann Surg Oncol. 2017;24(6):1610–7.
Tsai WS, Hsieh PS, Yeh CY, Chiang JM, Tang R, Chen JS, et al. Impact of chemotherapy-related prognostic factors on long-term survival in patients with stage III colorectal cancer after curative resection. Int J Clin Oncol. 2013;18(2):242–53.
Hensler T, Hecker H, Heeg K, Heidecke CD, Bartels H, Barthlen W, et al. Distinct mechanisms of immunosuppression as a consequence of major surgery. Infect Immun. 1997;65(6):2283–91.
Fisher B, Gunduz N, Coyle J, Rudock C, Saffer E. Presence of a growth-stimulating factor in serum following primary tumor removal in mice. Can Res. 1989;49(8):1996–2001.
Ono I, Gunji H, Suda K, Iwatsuki K, Kaneko F. Evaluation of cytokines in donor site wound fluids. Scand J Plast Reconstr Surg Hand Surg. 1994;28(4):269–73.
Hobor S, Van Emburgh BO, Crowley E, Misale S, Di Nicolantonio F, Bardelli A. TGFalpha and amphiregulin paracrine network promotes resistance to EGFR blockade in colorectal cancer cells. Clin Cancer Res. 2014;20(24):6429–38.
Eggermont AM, Steller EP, Sugarbaker PH. Laparotomy enhances intraperitoneal tumor growth and abrogates the antitumor effects of interleukin-2 and lymphokine-activated killer cells. Surgery. 1987;102(1):71–8.
Eggermont AM, Steller EP, Marquet RL, Jeekel J, Sugarbaker PH. Local regional promotion of tumor growth after abdominal surgery is dominant over immunotherapy with interleukin-2 and lymphokine activated killer cells. Cancer Detect Prev. 1988;12(1–6):421–9.
Tie J, Wang Y, Tomasetti C, Li L, Springer S, Kinde I, et al. Circulating tumor DNA analysis detects minimal residual disease and predicts recurrence in patients with stage II colon cancer. Sci Transl Med. 2016;8(346):92.
Reinert T, Henriksen TV, Christensen E, Sharma S, Salari R, Sethi H, et al. Analysis of plasma cell-free DNA by ultradeep sequencing in patients with stages I to III colorectal cancer. JAMA Oncol. 2019;5(8):1124–31.
Tie J, Cohen JD, Lahouel K, Lo SN, Wang Y, Kosmider S, et al. Circulating tumor DNA analysis guiding adjuvant therapy in stage II colon cancer. N Engl J Med. 2022;386(24):2261–72.
Bork U, Rahbari NN, Scholch S, Reissfelder C, Kahlert C, Buchler MW, et al. Circulating tumour cells and outcome in non-metastatic colorectal cancer: a prospective study. Br J Cancer. 2015;112(8):1306–13.
Tie J, Cohen JD, Wang Y, Christie M, Simons K, Lee M, et al. Circulating tumor DNA analyses as markers of recurrence risk and benefit of adjuvant therapy for stage III colon cancer. JAMA Oncol. 2019;5(12):1710–7.
Parikh AR, Van Seventer EE, Siravegna G, Hartwig AV, Jaimovich A, He Y, et al. Minimal residual disease detection using a plasma-only circulating tumor DNA assay in patients with colorectal cancer. Clin Cancer Res. 2021;27(20):5586–94.
de Lacroix WF, Lennartz KJ. Changes in the proliferation characteristics of a solid transplantable tumour of the mouse with time after transplantation. Cell Tissue Kinet. 1981;14(2):135–42.
Goldie JH, Coldman AJ. A mathematic model for relating the drug sensitivity of tumors to their spontaneous mutation rate. Cancer Treat Rep. 1979;63(11–12):1727–33.
Harless W, Qiu Y. Cancer: A medical emergency. Med Hypotheses. 2006;67(5):1054–9.
Goldman LI, Lowe S, al-Saleem T. Effect of fluorouracil on intestinal anastomoses in the rat. Arch Surg. 1969;98(3):303–4.
Acknowledgements
We thank the Department of Gastrointestinal Oncology of Tianjin Medical University Cancer Institute and Hospital.
Funding
This research was funded by the National Natural Science Foundation of China (82072664 and 82103677), National Key Research and Development Program of China (2020YFC2006404) and Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-009A).
Author information
Authors and Affiliations
Contributions
Conceptualization: Yuchong Yang, Yao Lu, Yi Ba and Ting Deng; Literature searching: Le Zhang and Hui Tan; Literature screening: Ming Bai, Xia Wang and Shaohua Ge; Data extraction: Tao Ning, Yao Lu and Jingjing Duan; Assessment of study quality: Yuchong Yang, Rui Liu, and Yansha Sun; Statistical analysis: Yuchong Yang, Yao Lu and Ting Deng; Writing-Original Draft: Yuchong Yang and Yao Lu; Writing-Review and Editing: Ting Deng, Hongli Li and Yi Ba; Funding acquisition: Jingjing Duan and Yi Ba. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Test result for publication bias A. Begg’s test (P = 0.13); B. Egger’s test (P = 0.36); C. Sensitivity analysis of the hazard ratio of overall survival. Table S1. The Newcastle-Ottawa scale quality of included studies. Table S2. The summary results about 5-year overall survival in patients receiving AC in < 8 weeks and that in patients who started the AC in > 8 weeks. Table S3. The summary results about 5-year relapse-free survival in patients receiving AC in < 8 weeks and that in patients who started the AC in > 8 weeks. Table S4. The summary results about 5-year overall survival in patients receiving AC in ≤ 4 weeks and that in patients who started the AC in 5-8 weeks.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Y., Lu, Y., Tan, H. et al. The optimal time of starting adjuvant chemotherapy after curative surgery in patients with colorectal cancer. BMC Cancer 23, 422 (2023). https://doi.org/10.1186/s12885-023-10863-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-10863-w