Abstract
Background
In this study we aimed to evaluate the efficacy and safety of the PD-L1 inhibitor durvalumab across various mismatch repair deficient (dMMR) or microsatellite instability-high (MSI-H) tumours in the Drug Rediscovery Protocol (DRUP). This is a clinical study in which patients are treated with drugs outside their labeled indication, based on their tumour molecular profile.
Patients and methods
Patients with dMMR/MSI-H solid tumours who had exhausted all standard of care options were eligible. Patients were treated with durvalumab. The primary endpoints were clinical benefit ((CB): objective response (OR) or stable disease ≥16 weeks) and safety. Patients were enrolled using a Simon like 2-stage model, with 8 patients in stage 1, up to 24 patients in stage 2 if at least 1/8 patients had CB in stage 1. At baseline, fresh frozen biopsies were obtained for biomarker analyses.
Results
Twenty-six patients with 10 different cancer types were included. Two patients (2/26, 8%) were considered as non-evaluable for the primary endpoint. CB was observed in 13 patients (13/26, 50%) with an OR in 7 patients (7/26, 27%). The remaining 11 patients (11/26, 42%) had progressive disease. Median progression-free survival and median overall survival were 5 months (95% CI, 2-not reached) and 14 months (95% CI, 5-not reached), respectively. No unexpected toxicity was observed. We found a significantly higher structural variant (SV) burden in patients without CB. Additionally, we observed a significant enrichment of JAK1 frameshift mutations and a significantly lower IFN-γ expression in patients without CB.
Conclusion
Durvalumab was generally well-tolerated and provided durable responses in pre-treated patients with dMMR/MSI-H solid tumours. High SV burden, JAK1 frameshift mutations and low IFN-γ expression were associated with a lack of CB; this provides a rationale for larger studies to validate these findings.
Trial registration
Clinical trial registration: NCT02925234. First registration date: 05/10/2016.
Similar content being viewed by others
Background
Mismatch repair deficient (dMMR) or microsatellite instability-high (MSI-H) tumours comprise 2 to 4% of all diagnosed cancers and are most commonly observed in colorectal, endometrial and gastric adenocarcinomas [1,2,3]. dMMR/MSI-H tumours have a unique genetic signature caused by germline or acquired deficiency of one of the four major mismatch repair genes, MLH1, MSH2, MSH6 and PMS2 [4, 5]. The protein functions are achieved by heterodimers, MLH1 being the PMS2 partner and MSH2 being the MSH6 partner [6]. Deficiencies in the major mismatch repair genes lead to insertions and deletions (indels) in highly repetitive DNA sequences, termed microsatellites, resulting in a higher degree of microsatellite instability (MSI) [2, 5, 7, 8]. As a consequence, these tumours have an exceptionally high number of somatic mutations, especially frameshift indels, generating a high burden of neoantigens [2, 9,10,11]. Therefore, dMMR/MSI-H tumours are considered to be highly immunogenic, rendering them more sensitive to programmed cell death 1 (PD-1) and programmed cell death ligand 1 (PD-L1) inhibitors [2, 9].
The inhibitory ligand PD-L1 is frequently upregulated in tumours cells, which results in the exhaustion of cytotoxic T cells by binding to PD-1 and contributes to tumour immune escape. This can be reversed by PD-1 or PD-L1 immune checkpoint inhibitors (ICI), thereby restoring anti-tumour immunity [12, 13]. Sensitivity to PD-1 inhibitors, such as nivolumab and pembrolizumab, has been frequently observed across various dMMR/MSI-H tumours. The CheckMate 142 study showed that nivolumab provided durable responses in pre-treated patients with dMMR/MSI-H metastatic colorectal cancer (CRC) and observed an objective response rate (ORR) of 31.1% (95% confidence interval (CI), 20.8–42.9%) [14]. Moreover, the KEYNOTE-158 study observed similar results with pembrolizumab in pre-treated patients with non-CRC dMMR/MSI-H tumours and showed an ORR of 34.3% (95% CI, 28.3–40.8%) [2]. Efficacy of anti-PD1 has also been investigated in first-line metastatic setting. The KEYNOTE-177 study showed that pembrolizumab improved progression free survival (PFS) as first-line therapy in metastatic dMMR/MSI CRC compared to standard of care chemotherapy [15, 16]. Results from these studies have led to several approvals by the Food and Drug Administration, including the first tumour-agnostic authorization for pembrolizumab in unresectable or metastatic dMMR/MSI-H tumours that have progressed after prior standard treatment and lack satisfactory alternative treatment options [17].
Efficacy of PD-L1 inhibitors however, has mainly been described in a subset of dMMR/MSI-H tumours. The PHAEDRA study showed promising activity of durvalumab in 35 patients with advanced dMMR/MSI-H endometrial cancer and found an ORR of 47% (95% CI, 32–63%), consistent with previous trials evaluating the efficacy of anti-PD1 in dMMR/MSI-H tumours [2, 18,19,20]. In 30 patients with metastatic dMMR/MSI-H CRC, durvalumab also showed encouraging activity equivalent to that of PD-1 inhibitors with an ORR varying between 27% (95% CI, 0.6–61%) and 42.4% (95% CI, 25.5–60.8%) [21, 22]. Furthermore, the SAMCO-PRODIGE 54 trial showed that the PD-L1 inhibitor avelumab was superior to chemotherapy with respect to PFS with a 12-month PFS of 19% and 31% in the control and avelumab group, respectively [23]. However, evidence regarding efficacy of PD-L1 inhibitors in other dMMR/MSI-H solid tumours remains limited. Therefore, we evaluated the efficacy and safety of durvalumab, a human immunoglobulin G1 kappa monoclonal antibody with high affinity and selectivity against PD-L1 [24], across various dMMR/MSI-H solid tumours in the Drug Rediscovery Protocol (DRUP). DRUP is an ongoing prospective, multicentre, non-randomized clinical trial in which cancer patients, who have exhausted all standard of care options, are treated with approved targeted- or immunotherapies outside their registered indication, based on their tumour molecular profile [25]. DRUP aims to facilitate patient access to commercially available anti-cancer drugs and to describe efficacy and safety data of these drugs when used outside their registered indication. Furthermore, DRUP also creates a unique opportunity to explore determinants of (non-) response by performing extensive biomarker analyses on mandatory fresh frozen tumour biopsies.
Methods
Study design
DRUP is an ongoing prospective, multicentre, non-randomized clinical umbrella and basket trial in which patients with metastatic or advanced solid tumours, non-Hodgkin lymphoma or multiple myeloma, without standard of care options, are treated based on their tumour molecular profile with targeted- or immunotherapy outside their registered indication. Patients are enrolled in parallel cohorts, each defined by one tumour type, one molecular variant and one study treatment. For selected biomarkers, such as dMMR/MSI-H, the protocol allows for tumour-agnostic cohorts [25].
DRUP is registered with ClinicalTrials.gov, number NCT02925234. DRUP was approved by the independent ethics committee and by the institutional review boards in every participating hospital. The study is conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki’s ethical principles for medical research. Written informed consent was obtained from all study subjects [25].
Study population
Eligible patients were adults aged ≥ 18 years with advanced solid tumours who had exhausted all standard of care options. Patients were eligible if routine molecular testing demonstrated dMMR by loss of staining of one of the mismatch repair proteins MLH1, MSH2, MSH6 and PMS2 by immunohistochemistry (IHC) or MSI-H by either polymerase chain reaction (PCR), panel-based next generation sequencing (NGS) or whole genome sequencing (WGS). Patients had measurable disease according to the Response Evaluation Criteria in Solid Tumours version 1.1 (RECIST v1.1) [26], or according to Response Assessment in Neuro-Oncology (RANO) [27] criteria, an acceptable organ function and an Eastern Cooperative Oncology Group performance status of 0–1. Patients were considered evaluable if response was radiologically or clinically evaluable, if they received at least one treatment administration and if they were on study for at least one treatment cycle. Non-evaluable patients were replaced and excluded from biomarker analyses.
Treatment assessment and evaluation
Patients were treated with monotherapy durvalumab (1500 mg intravenously every 4 weeks) until disease progression or unmanageable toxicity. Treatment beyond progression was not permitted in the protocol. Radiological imaging for tumour response assessment was performed at baseline and every 8 weeks (2 cycles) after treatment initiation.
Safety was measured by the frequency of grade ≥ 3 treatment related adverse events (AEs) occurring up to 30 days after the last administration of study drug. All AEs were graded according to the Common Terminology Criteria for Adverse Events (CTCAE) v4.03.
The primary endpoints of this study, as previously described [25, 28, 29], were clinical benefit (CB) and safety. CB was defined by confirmed complete or partial response (CR; PR) or stable disease (SD) for at least 16 weeks, according to RECIST 1.1. or RANO criteria and measured at least two times, at least 28 days apart in a particular cohort. Safety was defined as grade ≥ 3 treatment-related AEs. Secondary endpoints included PFS and overall survival (OS). Biomarker analyses on pre-treatment biopsies formed an exploratory endpoint.
Pre-treatment biopsies and biomarker analysis
According to protocol, it was mandatory to obtain a fresh frozen tumour biopsy before start of treatment. Exceptions were made for patients with primary brain tumours. DNA was isolated from biopsies and all biopsies were analysed for WGS (the Hartwig Medical Foundation, Amsterdam, The Netherlands) on the Illumina Novaseq (2 × 151) platform, together with a matched 10-ml blood sample to determine germline DNA of a patient. If the tumour-cell percentage was ≥20% and the DNA yield was ≥300 ng, WGS and RNA sequencing were performed. Hartwig Medical Foundation provides high quality sequencing data as Priestley et al. [30] described with a median average depth of 106x (tumour) and 38x (blood). WGS analysis was performed as previously described [30, 31] whereby somatic single nucleotide variants and indels were called using SAGE, and purity and ploidy estimations, structural variant (SV) and copy number analysis were performed using HMF’s in-house tools GRIDSS, PURPLE and LINX. Tumour mutation burden (TMB) per megabase (Mb), tumour mutational load (ML) and microsatellite-instable indels (msIndels) per Mb were calculated by computing the number of total somatic mutations, the number of missense mutations and number of frameshifts in microsatellite regions, respectively. SV burden was defined as the sum of total number of non-inferred and non-single passing SVs per sample.
Total RNA was extracted using the QIAGEN QIAsymphony RNA kit. Samples with approximately 100 ng total RNA were prepared with KAPA RNA Hyper + RiboErase HMR and RNA libraries were paired end sequenced on the Illumina NextSeq550 platform (2x75bp) or Illumina NovaSeq6000 platform (2x150bp). Gene expression was quantified using Salmon (v1.60) and IFN-gamma (IFN-γ) expression was computed using gene sets as previously described [32].
Statistical analysis
In DRUP, as previously described [25, 28, 29], cohorts are monitored using a Simon-like two-stage “admissible” monitoring plan to identify cohorts with evidence of activity [33]. If no CB is observed in any of the first enrolled 8 patients in the cohort, the cohort will be closed. Otherwise, an additional 16 patients will be included in the cohort. Four or fewer patients with CB would suggest a lack of activity, whereas five or more patients with CB will suggest that further investigation of the drug in the tumour/variant is warranted. The null hypothesis and alternative hypothesis to be tested are defined as clinical benefit rate (CBR) of 10% versus ≥ 30%. This design has 85% power to reject the null hypothesis of a CBR of 10% when the true CBR is 30%, with a one-sided alpha error rate of 7.8% [29]. Cohorts with a response rate of ≥ 30% are considered potentially successful and may proceed to stage III in DRUP to validate and confirm results earlier found [34].
All statistical analyses were performed using R version 4.0.3. Patient characteristics, AEs and tumour responses were summarized using descriptive statistics. Kaplan-Meier methods were used to estimate PFS (from start treatment to progression or death from any cause and censoring patients alive without progression) and OS (calculated from the first day of treatment administration to the date of death from any cause, censoring patients who were alive at last follow-up). Duration of response (DoR) was calculated from the first date response was measured until disease progression. Differences in CB between different groups of patients were analysed using the Fisher’s exact test. Differences of genomic features in patients with CB and without CB were compared using the Mann-Whitney U test.
Results
Accrual and patient characteristics
From January 2019 through April 2020, a total of 47 patients with histologically confirmed dMMR/MSI-H solid tumours who had exhausted all standard of care options, were submitted to the central study team for evaluation for potential study participation in the cohort “Durvalumab for dMMR/MSI-H tumours”. Forty-three patients were approved by the central study team to be screened for treatment with durvalumab, but 17 patients dropped out after allocation. Of those, four patients underwent alternative treatment options and four patients preferred not to undergo study treatment. The remaining nine patients did not meet the inclusion criteria, mainly due to rapid clinical deterioration (n = 6, 67%) (Supplemental Fig. S1). Twenty-six patients with ten different tumour types were considered eligible and started study treatment, of which the majority (n = 8, 31%) had CRC. Twenty-four patients were evaluable for the primary endpoint. Two patients were not evaluable for the primary endpoint according to our protocol definition on treatment evaluability (one patient had rapid clinical deterioration and one patient had disease progression confirmed by radiological imaging, both within the first treatment cycle). Baseline characteristics are presented in Table 1.
Clinical benefit and safety
Thirteen out of 26 patients (50%, 95% CI, 30–70%) had CB upon treatment with durvalumab. An objective response (OR) was observed in 7 out of 26 patients (27%, 95% CI, 12–48%); three patients achieved a CR (3/26, 12%) and four patients achieved a PR (4/26, 15%; Supplemental Table S1). The remaining 11 evaluable patients (11/26, 42%) had progressive disease. CB was more frequently observed in patients with CRC vs non-CRC tumours (85% vs. 41%); however, this difference was not statistically significant (p = 0.08).
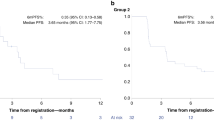
At data cut-off (16th of December, 2021), after a median follow-up of 29 months (95% CI, 23–32 months), the median duration of response was not yet reached (95% CI, 15–NA months) and seven patients were still on study. The median time on treatment was 4.2 months (95% CI, 1.1–15.9 months; Fig. 1). Median PFS and OS were 5 months (95% CI, 2–NA months; Fig. 2A) and 14 months (95% CI, 5–NA months; Fig. 2B), respectively.
Treatment efficacy of durvalumab. Swimmer plot of the time on treatment (in months) for each evaluable patient (n = 24). Patients marked with an arrow were still on study (as per December 16th, 2021). The red dot marks treatment discontinuation. The diamond-shape marks partial responses (PR) and the asterisk marks complete responses (CR)
A Progression Free Survival curve. B Overall Survival curve. Legend: Progression free survival (PFS) and overall survival (OS) of each enrolled patient (n = 26) in the cohort “Durvalumab for dMMR/MSI-H tumours”. Kaplan-Meier curves for estimated PFS (A) and OS (B), with 95% Confidence Intervals (dashed lines)
Overall, durvalumab was well-tolerated. Grade ≥ 3 AEs occurred in 15 patients (15/26, 58%) and treatment-related grade ≥ 3 AEs occurred in 5 patients (5/26, 19%) (Table 2). In one patient treatment was discontinued due to development of a grade 3 contained gastric perforation at the tumour site, which was considered to be possibly treatment-related. This patient went off study and was lost to follow-up. No grade ≥ 3 immune related AEs, grade 5 AEs and serious unexpected AEs occurred.
Baseline biopsies sequencing and MSI classification
Pre-treatment biopsies were obtained in 25 out of 26 enrolled patients. One patient with a primary brain tumour did not undergo a biopsy according to protocol. Biopsies from six patients (6/26, 23%) could not be sequenced due to insufficient tumour purity (< 20%). Therefore, 19 biopsies had sufficient material for WGS sequencing (19/26, 73%) and 14 biopsies (14/19, 74%) were also available for RNA sequencing.
Concordance between MSI classification based on WGS data and IHC analysis was observed in 17 patients (17/19, 89%). Two patients were classified as microsatellite stable (MSS) by WGS. One of these patients with endometrial cancer was enrolled based on IHC indicating loss of MLH1/PMS2 and no methylation of MLH1. However, WGS revealed a clear MSS lesion with a msIndel burden of only 0.28 indels/Mb (MSI cut-off: 4 indels/Mb) and low TMB of 3.6 mut/Mb. The other patient was diagnosed with a Lynch associated pancreatic carcinoma and was enrolled because of isolated loss of MSH6 by IHC. WGS indicated MSS with a msIndel burden of 3.31 indels/Mb and high TMB of 21.7 mut/Mb. Both patients (18% of all that had PD) did not experience CB. (Table 3).
MSS samples and samples of patients considered as non-evaluable were excluded from the further biomarker analyses. Thus, 15 samples and 12 samples were included in the genomic and transcriptomic analysis, respectively (Table 3).
Genomic-derived biomarkers of ICI response
Given previous reports on TMB as an independent biomarker of response in dMMR/MSI-H CRC [35], we next compared TMB of patients with CB and without CB. Generally, we found that patients experiencing CB had a higher TMB than patients without CB (median TMB 193 mut/Mb vs. 114 mut/Mb), but this difference was not statistically significant (p = 0.61; Fig. 3A). Tumours with a high ML and/or high msIndel burden harbour an expanded neoantigen repertoire, making them more immunogenic and responsive to ICI [2, 10, 11, 36]. Therefore, we analysed patients by ML and msIndel burden, but we did not observe any statistically significant differences by CB (p = 0.22, p = 0.61; Fig. 3B/C). Patients with CB and without CB had a median ML of 1424 and median msIndel burden of 137 indels/Mb compared with a median ML of 820 and median msIndel burden of 77 indels/Mb, respectively. SVs may result in more foreign neoantigens than neoantigens derived by single mutations or small insertions and deletions [37] and we therefore lastly evaluated SV burden. Interestingly, we observed that patients without CB had a significantly higher SV burden compared to patients with CB (median SV burden 300 vs. 138, p = 0.026; Fig. 3D).
Comparison of genomic features. A Tumour mutation burden per megabase, B Tumour mutational load (log10), C microsatellite-instable indels per megabase, D structural variant burden, E expression score of IFN-gamma (IFN-γ) in patients experiencing clinical benefit (blue) or no clinical benefit (red), F expression score of IFN-γ in patients with two JAK1 (K860N/P430R) frameshift mutations (orange) or not (green) and G proportion of patients with two JAK1 (K860N/P430R) frameshift mutations or not, by clinical benefit. The box plot shows the median, first and third quartiles, whiskers extend to 1.5 times the interquartile range, and outlying points are plotted individually and two-sided. In A-F a two-sided Mann-Whitney U test was used. In G a Fisher’s Exact test was used *p < 0.05; ns, not significant
Association between IFN-γ signalling pathway and CB
Anti-tumour immune responses require adequate antigen presentation, which is coordinated by several genes, including B2M [38, 39]. However, in our cohort, B2M mutations were more often observed in patients with CB (4/5, 80%; Table 3) compared to patients without CB (1/5, 20%; Table 3), but this difference was not statistically significant (p = 0.58; Table 3).
Antigen presentation is also mediated by the IFN-γ signalling pathway, which is a critical driver of PD-L1 expression in tumour cells and therefore plays an important role in the efficacy of ICI [32, 38, 39]. We therefore examined mRNA expression of IFN-γ in patients with and without CB and observed that IFN-γ expression was significantly lower in patients without CB (p = 0.01; Fig. 3E). The IFN-γ signalling pathway can be modulated by several genes, including JAK1, JAK2 and STAT1 [38,39,40]. Interestingly, we observed the presence of JAK1 mutations in five patients (5/15, 33%; Table 3), which is comparable to the frequency of JAK1 mutations among dMMR/MSI-H tumours in The Cancer Genome Atlas (TCGA) dataset (91/400, 23%) [41]. However, within this group, we observed the presence of two concurrent frameshift JAK1 mutations (K860N/P430R), in four patients (4/5, 80%; Table 3), which is a higher prevalence than found in the TCGA dataset (5/91, 5%) [41]. We found the presence of the two JAK1 frameshift mutations to be significantly enriched in patients that did not experience CB (p = 0.011; Fig. 3G). Furthermore, we found that the presence of the two JAK1 frameshift mutations was significantly associated with a lower IFN-γ expression compared to tumours without those JAK1 frameshift mutations (p = 0.036; Fig. 3F). Additionally, we did not find any statistically significant enrichment of mutations in STAT1 and JAK2 in patients with or without CB (Table 3).
Discussion
The PD-L1 inhibitor durvalumab provided durable responses in previously treated patients with advanced dMMR/MSI-H solid tumours, with 13 patients (50%) experiencing CB, including 7 patients (27%) with an OR. These findings are in line with previously reported response rates to ICI in pre-treated dMMR/MSI-H tumours [2, 21].
Baseline WGS was successfully performed on 73% of the obtained biopsies. This is consistent with the overall WGS success rate within DRUP [25] and within the Dutch CPCT-02 study [30]. Interestingly, in two patients there was no concordance between WGS and IHC analysis. Both patients did not experience CB, possibly explained by the MSS status. Potential explanations for the discrepancy between IHC and WGS in the patient with somatic endometrial cancer can be misinterpretation of IHC by the pathologist [6] or tumour heterogeneity. Although dMMR is an early event in carcinogenesis, tumour heterogeneity in dMMR (endometrial) tumours has previously been reported [6, 42, 43]. The discrepancy in the patient with Lynch associated pancreatic cancer may be explained by the isolated loss of MSH6, since it has been shown that isolated loss of MSH6 does not always result in complete loss of mismatch repair function [6], which possibly explains why the tumour did not reach the cut-off of a msIndel burden of 4.0 indels/Mb [31]. These data highlight the importance of optimal molecular diagnostics. Additional studies are essential to determine the accuracy of currently used routine tests for dMMR/MSI-H in a pan-cancer setting.
Next, we observed that ML, TMB and msIndels were generally higher in patients with CB than patients without CB, which is line in with previous literature [35, 44, 45]. However, these differences were not significant in this patient cohort, possibly due to small sample size or the inherent differences between tumours depending on subtype. Interestingly, we found that higher SV burden was statistically significantly associated with no CB, which is consistent with previously reported data in melanoma patients treated with ICI [46]. However, research into the role of SVs is limited due to difficulties in detection [47] and therefore their role in resistance to ICI is not entirely clear. Our finding suggests that dMMR/MSI-H tumours with high SV burden are less sensitive to ICI, which mechanistically may be due to the formation of resistance mechanisms generated by structural changes. Further research is required to confirm this observation in order to better understand the possible role of SVs as a potential biomarker in dMMR/MSI-H tumours.
We also explored IFN-γ expression and genes associated with the IFN-γ signalling pathway, as it has been shown that this pathway plays a crucial role in efficacy of ICI [32, 38, 39]. As expected, based on previous literature, we found that patients without CB had significantly lower IFN-γ expression than patients with CB [32]. Furthermore, we observed a significant enrichment of JAK1 frameshift mutations in patients without CB. These JAK1 frameshift mutations have previously been described as recurrent mutations and non-functional mutations, especially in dMMR/MSI-H tumours and have been associated with resistance to ICI if complete loss of function occurs [9, 40, 48,49,50,51]. The presence of two JAK1 mutations and the significantly lower IFN-γ expression both suggest complete loss of function of JAK1. We therefore considered these JAK1 frameshift mutations as a possible route for primary resistance mechanism to ICI, which may suggest that patients with dMMR/MSI-H tumours harbouring these JAK1 frameshift mutations are possibly not good candidates for ICI treatment and should be excluded from this treatment.
Interestingly, we observed the presence of two JAK1 frameshift in a higher prevalence (4/5, 80%) compared to the TCGA dataset (5/91, 5%). This difference may be influenced by our small sample size or may reflect the fact that the TCGA also includes newly diagnosed dMMR/MSI-H cancers whereas our dataset only consisted of patients with advanced, pre-treated dMMR/MSI-H tumours.
This study has several potential limitations. One limitation is the heterogeneity of this cohort. Ten different tumour types were enrolled, resulting in a heterogeneous study population with large variations in prior treatment regimes. Furthermore, WGS was not in all cases available to confirm MSI status. Additionally, as response evaluations were performed according to RECIST criteria, potential pseudoprogression could not be taken into consideration [52]. Besides, as a result of the DRUP design, it should be noted that these results were obtained in a small sample size and therefore require validation in a larger cohort. Nevertheless, we detected a clinically relevant signal of activity of durvalumab across various advanced dMMR/MSI-H solid tumours and it thus shows that studies like DRUP can contribute significantly to the identification of clinical signs of activity.
Conclusion
In conclusion, the PD-L1 inhibitor durvalumab provided durable responses in previously treated patients with advanced dMMR/MSI-H solid tumours with CB in 50% and an OR in 27%. Biomarker analyses revealed high SV burden, JAK1 frameshift mutations and low IFN-γ expression as possible resistance mechanisms to anti-PDL1 in dMMR/MSI-H tumours, providing a rationale for larger studies to validate these findings.
Availability of data and materials
All data described in this study are freely available for academic use, and can be obtained through the Netherlands Cancer Institute and the HMF through standardized procedures and request forms. These can be found at https://www.hartwigmedicalfoundation.nl/en. For further information, see van der Velden (Nature, 2019).
Abbreviations
- AEs:
-
Adverse events
- CB:
-
Clinical benefit
- CI:
-
Confidence Interval
- CR:
-
Complete response
- CRC:
-
Colorectal cancer
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- dMMR:
-
Mismatch repair deficient
- DoR:
-
Duration of response
- DRUP:
-
Drug Rediscovery Protocol
- ICI:
-
Immune checkpoint inhibitors
- IFN-γ:
-
IFN-gamma
- IHC:
-
Immunohistochemistry
- indels:
-
insertions and deletions
- Mb:
-
Megabase
- ML:
-
Tumour mutational load
- MSI(-H):
-
Microsatellite instability(-high)
- MSS:
-
Microsatellite stable
- msIndels:
-
Microsatellite-instable indels
- NGS:
-
Next generation sequencing
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PCR:
-
Polymerase chain reaction
- PD-1:
-
Programmed cell death 1
- PD-L1:
-
Programmed cell death ligand 1
- PFS:
-
Progression free survival
- PR:
-
Partial response
- RANO:
-
Response Assessment in Neuro-Oncology
- RECIST:
-
Response Evaluation Criteria in Solid Tumours version 1.1
- SD:
-
Stable disease
- SV:
-
Structural variant
- TCGA:
-
The Cancer Genome Atlas
- TMB:
-
Tumour mutational burden
- WGS:
-
Whole genome sequencing
References
Cortes-Ciriano I, Lee S, Park WY, Kim TM, Park PJ. A molecular portrait of microsatellite instability across multiple cancers. Nat Commun. 2017;8:15180.
Marabelle A, Le DT, Ascierto PA, Di Giacomo AM, De Jesus-Acosta A, Delord JP, et al. Efficacy of Pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient Cancer: results from the phase II KEYNOTE-158 study. J Clin Oncol. 2020;38(1):1–10.
Bonneville R, Krook MA, Kautto EA, Miya J, Wing MR, Chen HZ, et al. Landscape of microsatellite instability across 39 Cancer types. JCO Precis Oncol. 2017;2017:PO17.00073. https://doi.org/10.1200/PO.17.00073. Epub 2017 Oct 3.
Seth S, Ager A, Arends MJ, Frayling IM. Lynch syndrome - cancer pathways, heterogeneity and immune escape. J Pathol. 2018;246(2):129–33.
Dudley JC, Lin MT, Le DT, Eshleman JR. Microsatellite instability as a biomarker for PD-1 blockade. Clin Cancer Res. 2016;22(4):813–20.
Evrard C, Tachon G, Randrian V, Karayan-Tapon L, Tougeron D. Microsatellite instability: diagnosis, heterogeneity, discordance, and clinical impact in colorectal Cancer. Cancers (Basel). 2019;11(10):1567. https://doi.org/10.3390/cancers11101567.
Cancer Genome Atlas N. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487(7407):330–7.
Timmermann B, Kerick M, Roehr C, Fischer A, Isau M, Boerno ST, et al. Somatic mutation profiles of MSI and MSS colorectal cancer identified by whole exome next generation sequencing and bioinformatics analysis. PLoS One. 2010;5(12):e15661.
Takahashi N, Rajapakse VN, Pongor L, Kumar S, Tlemsani C, Erwin-Cohen R, et al. Dynamics of genomic and immune responses during primary immunotherapy resistance in mismatch repair-deficient tumors. Cold Spring Harb Mol Case Stud. 2020;6(5):a005678. https://doi.org/10.1101/mcs.a005678.
Yang G, Zheng RY, Jin ZS. Correlations between microsatellite instability and the biological behaviour of tumours. J Cancer Res Clin Oncol. 2019;145(12):2891–9.
Mandal R, Samstein RM, Lee KW, Havel JJ, Wang H, Krishna C, et al. Genetic diversity of tumors with mismatch repair deficiency influences anti-PD-1 immunotherapy response. Science. 2019;364(6439):485–91.
Yi M, Jiao D, Xu H, Liu Q, Zhao W, Han X, et al. Biomarkers for predicting efficacy of PD-1/PD-L1 inhibitors. Mol Cancer. 2018;17(1):129.
Lee HT, Lee JY, Lim H, Lee SH, Moon YJ, Pyo HJ, et al. Molecular mechanism of PD-1/PD-L1 blockade via anti-PD-L1 antibodies atezolizumab and durvalumab. Sci Rep. 2017;7(1):5532.
Overman MJ, McDermott R, Leach JL, Lonardi S, Lenz HJ, Morse MA, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol. 2017;18(9):1182–91.
Andre T, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab in microsatellite-instability-high advanced colorectal Cancer. N Engl J Med. 2020;383(23):2207–18.
Diaz LA Jr, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022;23(5):659–70.
Marcus L, Lemery SJ, Keegan P, Pazdur R. FDA approval summary: Pembrolizumab for the treatment of microsatellite instability-high solid tumors. Clin Cancer Res. 2019;25(13):3753–8.
Antill Y, Kok PS, Robledo K, Yip S, Cummins M, Smith D, et al. Australia New Zealand Gynaecological Oncology Group (ANZGOG). Clinical activity of durvalumab for patients with advanced mismatch repair-deficient and repair-proficient endometrial cancer. A nonrandomized phase 2 clinical trial. J Immunother Cancer. 2021;9(6):e002255. https://doi.org/10.1136/jitc-2020-002255.
Ott PA, Bang YJ, Berton-Rigaud D, Elez E, Pishvaian MJ, Rugo HS, et al. Safety and antitumor activity of Pembrolizumab in advanced programmed death ligand 1-positive endometrial Cancer: results from the KEYNOTE-028 study. J Clin Oncol. 2017;35(22):2535–41.
Oaknin A, Tinker AV, Gilbert L, Samouelian V, Mathews C, Brown J, et al. Clinical activity and safety of the anti-programmed death 1 monoclonal antibody Dostarlimab for patients with recurrent or advanced mismatch repair-deficient endometrial Cancer: a nonrandomized phase 1 clinical trial. JAMA Oncol. 2020;6(11):1766–72.
Segal NH, Wainberg ZA, Overman MJ, Ascierto PA, Arkenau H-T, Butler MO, et al. Safety and clinical activity of durvalumab monotherapy in patients with microsatellite instability–high (MSI-H) tumors. J Clin Oncol. 2019;37(4_suppl):670.
Oh CR, Kim JE, Hong YS, Kim SY, Ahn JB, Baek JY, et al. Phase II study of durvalumab monotherapy in patients with previously treated microsatellite instability-high/mismatch repair-deficient or POLE-mutated metastatic or unresectable colorectal cancer. Int J Cancer. 2022;150(12):2038–45.
Taieb J, Bouche O, Andre T, Barbier E, Laurentpuig P, Bez J, et al. Avelumab versus standard second-line treatment chemotherapy in metastatic colorectal cancer (mCRC) patients with microsatellite instability (MSI): the SAMCO-PRODIGE 54 randomised phase II trial. Ann Oncol. 2022;33:S808–S96.
Faiena I, Cummings AL, Crosetti AM, Pantuck AJ, Chamie K, Drakaki A. Durvalumab: an investigational anti-PD-L1 monoclonal antibody for the treatment of urothelial carcinoma. Drug Des Devel Ther. 2018;12:209–15.
van der Velden DL, Hoes LR, van der Wijngaart H, van Berge Henegouwen JM, van Werkhoven E, Roepman P, et al. The drug rediscovery protocol facilitates the expanded use of existing anticancer drugs. Nature. 2019;574(7776):127–31.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Wen PY, Chang SM, Van den Bent MJ, Vogelbaum MA, Macdonald DR, Lee EQ. Response assessment in neuro-oncology clinical trials. J Clin Oncol. 2017;35(21):2439–49.
van Berge Henegouwen JM, Jebbink M, Hoes LR, van der Wijngaart H, Zeverijn LJ, van der Velden DL, et al. Trastuzumab and pertuzumab combination therapy for advanced pre-treated HER2 exon 20-mutated non-small cell lung cancer. Eur J Cancer. 2022;171:114–23.
van der Wijngaart H, Hoes LR, van Berge Henegouwen JM, van der Velden DL, Zeverijn LJ, Roepman P, et al. Patients with Biallelic BRCA1/2 inactivation respond to Olaparib treatment across histologic tumor types. Clin Cancer Res. 2021;27(22):6106–14.
Priestley P, Baber J, Lolkema MP, Steeghs N, de Bruijn E, Shale C, et al. Pan-cancer whole-genome analyses of metastatic solid tumours. Nature. 2019;575(7781):210–6.
Roepman P, de Bruijn E, van Lieshout S, Schoenmaker L, Boelens MC, Dubbink HJ, et al. Clinical validation of whole genome sequencing for Cancer diagnostics. J Mol Diagn. 2021;23(7):816–33.
Ayers M, Lunceford J, Nebozhyn M, Murphy E, Loboda A, Kaufman DR, et al. IFN-gamma-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest. 2017;127(8):2930–40.
Jung SH, Lee T, Kim K, George SL. Admissible two-stage designs for phase II cancer clinical trials. Stat Med. 2004;23(4):561–9.
van Waalwijk van Doorn-Khosrovani SB, Pisters-van Roy A, van Saase L, van der Graaff M, Gijzen J, Sleijfer S, et al. Personalised reimbursement: a risk-sharing model for biomarker-driven treatment of rare subgroups of cancer patients. Ann Oncol 2019;30(5):663–665.
Schrock AB, Ouyang C, Sandhu J, Sokol E, Jin D, Ross JS, et al. Tumor mutational burden is predictive of response to immune checkpoint inhibitors in MSI-high metastatic colorectal cancer. Ann Oncol. 2019;30(7):1096–103.
Samstein RM, Lee CH, Shoushtari AN, Hellmann MD, Shen R, Janjigian YY, et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet. 2019;51(2):202–6.
Holtstrater C, Schrors B, Bukur T, Lower M. Bioinformatics for Cancer immunotherapy. Methods Mol Biol. 2020;2120:1–9.
Keenan TE, Burke KP, Van Allen EM. Genomic correlates of response to immune checkpoint blockade. Nat Med. 2019;25(3):389–402.
Kalbasi A, Ribas A. Tumour-intrinsic resistance to immune checkpoint blockade. Nat Rev Immunol. 2020;20(1):25–39.
Shin DS, Zaretsky JM, Escuin-Ordinas H, Garcia-Diaz A, Hu-Lieskovan S, Kalbasi A, et al. Primary resistance to PD-1 blockade mediated by JAK1/2 mutations. Cancer Discov. 2017;7(2):188–201.
Cancer Genome Atlas Research N, Weinstein JN, Collisson EA, Mills GB, Shaw KR, Ozenberger BA, et al. The Cancer genome Atlas Pan-Cancer analysis project. Nat Genet. 2013;45(10):1113–20.
Stelloo E, Jansen AML, Osse EM, Nout RA, Creutzberg CL, Ruano D, et al. Practical guidance for mismatch repair-deficiency testing in endometrial cancer. Ann Oncol. 2017;28(1):96–102.
Joost P, Veurink N, Holck S, Klarskov L, Bojesen A, Harbo M, et al. Heterogenous mismatch-repair status in colorectal cancer. Diagn Pathol. 2014;9:126.
Chida K, Kawazoe A, Kawazu M, Suzuki T, Nakamura Y, Nakatsura T, et al. A low tumor mutational burden and PTEN mutations are predictors of a negative response to PD-1 blockade in MSI-H/dMMR gastrointestinal tumors. Clin Cancer Res. 2021;27(13):3714–24.
Loupakis F, Depetris I, Biason P, Intini R, Prete AA, Leone F, et al. Prediction of benefit from checkpoint inhibitors in mismatch repair deficient metastatic colorectal Cancer: role of tumor infiltrating lymphocytes. Oncologist. 2020;25(6):481–7.
Newell F, Pires da Silva I, Johansson PA, Menzies AM, Wilmott JS, Addala V, et al. Multiomic profiling of checkpoint inhibitor-treated melanoma: identifying predictors of response and resistance, and markers of biological discordance. Cancer Cell. 2022;40(1):88–102 e7.
van Belzen I, Schonhuth A, Kemmeren P, Hehir-Kwa JY. Structural variant detection in cancer genomes: computational challenges and perspectives for precision oncology. NPJ Precis Oncol. 2021;5(1):15.
Ren Y, Zhang Y, Liu RZ, Fenstermacher DA, Wright KL, Teer JK, et al. JAK1 truncating mutations in gynecologic cancer define new role of cancer-associated protein tyrosine kinase aberrations. Sci Rep. 2013;3:3042.
Albacker LA, Wu J, Smith P, Warmuth M, Stephens PJ, Zhu P, et al. Loss of function JAK1 mutations occur at high frequency in cancers with microsatellite instability and are suggestive of immune evasion. PLoS One. 2017;12(11):e0176181.
Sveen A, Johannessen B, Tengs T, Danielsen SA, Eilertsen IA, Lind GE, et al. Multilevel genomics of colorectal cancers with microsatellite instability-clinical impact of JAK1 mutations and consensus molecular subtype 1. Genome Med. 2017;9(1):46.
Gulhan DC, Garcia E, Lee EK, Lindemann NI, Liu JF, Matulonis UA, et al. Genomic determinants of De novo resistance to immune checkpoint blockade in mismatch repair-deficient endometrial Cancer. JCO Precis Oncol. 2020;4:492–7.
Seymour L, Bogaerts J, Perrone A, Ford R, Schwartz LH, Mandrekar S, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18(3):e143–e52.
Acknowledgements
The Drug Rediscovery Protocol team thanks the Stelvio for Life Foundation and the Dutch Cancer Society for their financial support; AstraZeneca for their in-kind and financial support; the Centre for Personalized Cancer Treatment; Multidisciplinary Expert Board for supporting the central case-review process; the Independent Data Monitoring Committee for their advice on cohort decisions and the monitoring of preliminary safety data; the Netherlands Cancer Institute’s Biobank Facility, Scientific Department and Pharmacy for their facilitating services; the Hartwig Medical Foundation for their in-kind support by providing sequencing on baseline biopsies; and all participating hospitals for supporting and facilitating the conduct of the DRUP trial.
Funding
The DRUP trial is supported by the Stelvio for Life Foundation, [grant number not applicable]; the Dutch Cancer Society [grant number 10014]; and received equal funding from a number of pharmaceutical companies, among which AstraZeneca.
Author information
Authors and Affiliations
Contributions
Conception and design: Birgit S. Geurts, Thomas W. Battaglia, Henk M.W. Verheul, Hans Gelderblom, Emile E. Voest. Provision of study materials or patients: Birgit S. Geurts, J. Maxime van Berge Henegouwen, Laurien J. Zeverijn, Louisa R. Hoes, Hanneke van der Wijngaart, Gijs F. de Wit, Paul Roepman, Anne M.L. Jansen, Wendy W.J. de Leng. Collection and assembly of data: Birgit S. Geurts, Thomas W. Battaglia, J. Maxime Van Berge Henegouwen, Laurien J. Zeverijn, Gijs F. De Wit, Louisa R. Hoes, Hanneke van der Wijngaart, Vincent van der Noort, Paul Roepman, Wendy W.J. de Leng, Anne M.L. Jansen, Frans L. Opdam, Maja J.A. de Jonge, Geert A. Cirkel, Mariette Labots, Ann Hoeben, Emile D. Kerver, Adriaan D. Bins, Frans G.L. Erdkamp, Johan M. van Rooijen, Danny Houtsma, Mathijs P Hendriks, Jan-Willem B. de Groot, Henk M.W. Verheul, Hans Gelderblom, Emile E. Voest. Data analysis and interpretation: Birgit S. Geurts, Thomas W. Battaglia, Vincent van der Noort. The work reported in the paper has been performed by the authors, unless clearly specified in the text. Manuscript writing: All authors. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
DRUP was approved by the independent ethics committee and by the institutional review boards in every participating hospital. The study is conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki’s ethical principles for medical research. Written informed consent was obtained from all study subjects.
Consent for publication
Not applicable.
Competing interests
Emile E.Voest, Henk M.W. Verheul and Hans Gelderblom have, through the DRUP and other studies, received support from pharmaceutical companies participating in the DRUP. Frans L. Opdam reports research funding by Boehringer Ingelheim, AstraZeneca, GSK, Cytovation, InteRNA technologies, Merus, Taiho, Pierre Fabre and Kinnate. Mathijs P. Hendriks reports research funding by Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Clovis Oncology, Eisai, Ipsen, Merck Sharp & Dohme, Novartis, Pfizer and Roche. Jan-Willem B. de Groot is involved in advisory boards for Pierre Fabre, BMD and MSD. The other authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Geurts, B.S., Battaglia, T.W., van Berge Henegouwen, J.M. et al. Efficacy, safety and biomarker analysis of durvalumab in patients with mismatch-repair deficient or microsatellite instability-high solid tumours. BMC Cancer 23, 205 (2023). https://doi.org/10.1186/s12885-023-10663-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-10663-2