Abstract
Background & objective
“Anti-angiogenetic drugs plus chemotherapy” (anti-angio-chemo) and “immune checkpoint inhibitors plus chemotherapy” (ICI-chemo) are superior to traditional chemotherapy in the first-line treatment of patients with advanced non-small-cell lung cancer (NSCLC). However, in the absence of a direct comparison of ICI-chemo with anti-angio-chemo, the superior one between them has not been decided, and the benefit of adding anti-angiogenetic agents to ICI-chemo remains controversial. This study aimed to investigate the role of antiangiogenic agents for advanced NSCLC in the era of immunotherapy.
Methods
Eligible randomized controlled trials (RCTs) comparing chemotherapy versus therapeutic regimens involving ICIs or anti-angiogenetic drugs were included. Outcomes included progression-free survival (PFS), overall survival (OS), objective response rate (ORR), and rate of grade 3–4 toxicity assessment. R-4.3.1 was utilized to perform the analysis.
Results
A total of 54 studies with a sample size of 25,046 were finally enrolled. “Atezolizumab + Bevacizumab + Chemotherapy” significantly improved the ORR compared with “Atezolizumab + Chemotherapy” (Odds ratio (OR) = 2.73, 95% confidence interval (CI): 1.27–5.87). The trend also favored “Atezolizumab + Bevacizumab + Chemotherapy” in PFS and OS (hazard ratio (HR) = 0.71, 95% CI: 0.39–1.31; HR = 0.94, 95% CI: 0.77–1.16, respectively). In addition, “Pembrolizumab + Chemotherapy” and “Camrelizumab + Chemotherapy” significantly prolonged the PFS compared to “Bevacizumab + Chemotherapy” (HR = 0.65, 95% CI: 0.46–0.92; HR = 0.63, 95% CI: 0.41–0.97; respectively). Meanwhile, “Pembrolizumab + Chemotherapy” and “Sintilimab + Chemotherapy” yielded more OS benefits than “Bevacizumab + Chemotherapy” (HR = 0.69, 95% CI: 0.56–0.83; HR = 0.64, 95%CI: 0.46–0.91; respectively). Scheme between “Atezolizumab + Bevacizumab + Chemotherapy” and “Atezolizumab + Chemotherapy” made no significant difference (OR = 1.18, 95%CI: 0.56–2.42) concerning the rate of grade 3–4 toxicity. It seemed that ICI-chemo yielded more improvement in quality-adjusted life-year (QALY) than “Bevacizumab + Chemotherapy” in cost-effectiveness analysis.
Conclusion
Our results suggest that ICI-chemo is associated with potentially longer survival, better cost-effectiveness outcomes, and comparable safety profiles than anti-angio-chemo. Also, adding bevacizumab to ICI-chemo seemed to provide additional therapeutic benefits without adding treatment burden. Our findings would supplement the current standard of care and help the design of future clinical trials for the first-line treatment of patients with advanced NSCLC.
Similar content being viewed by others
Background
Lung cancer is the leading cause of cancer-related mortality worldwide [1]. Novel therapeutic approaches are urgently needed after the arrival of a “chemotherapy efficacy plateau” for advanced non-small cell lung cancer (NSCLC) [2]. Angiogenesis plays a critical role in tumor growth and metastasis. Key angiogenesis pathway is mainly inhibited via vascular endothelial growth factor (VEGF)/VEGF receptor signaling, either at the ligand level (e.g. bevacizumab) or at the receptor level (e.g. ramucirumab) or by the small-molecule small tyrosine kinase inhibitors [TKIs] (e.g. sorafenib) [3, 4]. Notably, bevacizumab plus platinum-based doublet chemotherapy has been approved for the treatment of advanced non-squamous NSCLC in the first-line setting [5].
The application of Ipilimumab in the first-line treatment of advanced NSCLC opened a new era of immunotherapy [6]. Chemotherapy elicits anti-tumor effects through the release of potentially immunogenic tumor antigens, which might result in additional immunotherapy activity and synergistic effect [7, 8]. The combination of Pembrolizumab and platinum-based doublet chemotherapy has been approved as a first-line treatment strategy for advanced non-squamous NSCLC patients without actionable genetic mutation in April 2019 [9]. Noteworthy, anti-programmed death 1 (PD-1) antibody and anti-cytotoxic T-lymphocyte antigen 4 (CTLA-4) antibody take distinct but complementary action. It was particularly critical in recruiting effective antitumor immunity and avoiding alternative exhausting pathway [10,11,12]. Consequently, anti-PD-1 plus CTLA-4 antibody is deemed to play a vital role in the era of immunotherapy. The efficacy of ICIs may be enhanced with the addition of anti-angiogenetic drugs via reversing VEGF-mediated immune-suppression [13, 14]. The landmark study— IMPOWER 150 trial, had firstly elucidated the superior efficacy of adding bevacizumab to ICI-chemo [15].
Anti-angiogenetic drugs plus chemotherapy (anti-angio-chemo) and ICI plus chemotherapy (ICI-chemo) are superior to chemotherapy alone in the first-line treatment for advanced NSCLC [3, 16]. However, the absence of head-to-head trials comparing ICI-chemo with anti-angio-chemo make no conclusion in which regimen is superior. Furthermore, the benefit of adding anti-angiogenetic agents to ICI-chemo remains controversial. In this study, we enrolled randomized-controlled trials (RCTs) and conducted a Bayesian Network Meta-analysis (NMA) to explore the above-mentioned matters. Besides, we reviewed the published articles concerning the cost-effectiveness analysis.
Methods
This systematic review and NMA was performed in accordance with the PRISMA Extension Statement for Reporting Systematic Reviews Incorporating Network Meta-analyses guidelines of Health Care Interventions (Supplementary material 1). The protocol for this study was registered in the Prospective Register of Systematic Reviews (CRD42022309295) to ensure transparency.
Data sources
Two authors (L.L.P and J.D.G) independently searched the records in the electronic database of PubMed, EMBASE, The Cochrane Library, and Web of science. The searching terminal date was June 2nd, 2021. Searching terms focused on “NSCLC”, “antiangiogenic agents”, and “ICIs” with the restriction of clinical trial. If necessary, an additional manual search of related literature in the reference list would be carried out to enroll any relevant publications. The datasets utilized in this analysis could be obtained from the corresponding author upon request. Records were imported into EndnoteX9 software to eliminate duplications. The detailed strategy was presented in Supplementary material 2.
Trial selection criteria and trial identification
Two authors (L.L.P and Y.H.H) independently reviewed the titles, abstracts, and keywords of the identified citations to select appropriate articles for full review. Any disagreement was resolved by consensus. Trials would be eligible only if meeting all the following criteria: 1) treatment-naïve patients with stage IIIB/IV NSCLC; 2) eligible RCTs comparing ICI-chemo or anti-angio-ICI versus the platinum chemotherapy alone; or involving the addition of antiangiogenic drugs into ICI-chemo; 3) full-text publications or conference abstract. Publications would be disregarded if meeting any of the following criteria: 1) any single perioperative chemotherapy, neoadjuvant or adjuvant chemotherapy, or radio-chemotherapy; 2) no first-line treatment; 3) non-accessible outcome.
Outcomes and data extraction
Two authors (L.L.P and J.L) independently performed data extraction and any discrepancies were eliminated by consensus. Data for the eligible trials related to basic characteristics were extracted.
The primary outcome included progression disease survival (PFS), overall survival (OS), objective response rate (ORR), and rate of grade3-4 toxicity. PFS was defined as the time interval from randomization to disease progression or death, whichever occurred first, while OS referred to the time from random assignment to death from any cause. Secondary outcomes included disease-controlled rate (DCR), any grade toxicity assessment, rate of side effects leading to drug discontinuation or death, and rate of seven commonly reported adverse events, including hematological (anemia, neutropenia, and thrombocytopenia) and non-hematological (nausea/vomiting, fatigue, diarrhea, and asthenia) adverse events. In addition, we reviewed the published articles about the cost-effectiveness analysis. When updated data for survival was available, the latest data was preferred. If necessary, Parmar’s method was utilized to obtain survival outcomes.
Quality and risk of bias assessment
Two researchers (L.L.P and J.D.G) independently assessed the risk of bias of the enrolled trials according to the recommendations of the Cochrane Handbook of Systematic Reviews of Interventions (http://handbook.cochrane.org). Disagreements were resolved by discussion.
Data synthesis and analysis
For PFS and OS, the logarithm of hazard ratio (HR) and their standard error (SE) were pooled into analysis through a Bayesian multiple treatment network meta-analysis with random effects. As for the dichotomous variables, odds ratio (OR) with 95% confidence interval (CI) was applied to calculate. When a network diagram indicated two or more independent loops, only the loop containing “Chemotherapy” was selected for further analysis. The predefined subgroup included PD-L1 expression levels, histology, sex, age, smoking status, ECOG status, and brain metastasis status.
Random effects and consistency model was computed utilizing Markov chain Monte Carlo methods with Gibbs sampling. The algorithm was based on simulations of 50,000 iterations and 20,000 adaptions in each of 4 chains. For a forest plot, “Chemotherapy” was chosen as the common reference comparator. A league table for the survival analysis was presented with the logarithm of HR and their 95% CI. Probability values were summarized and presented with the surface under the cumulative ranking (SUCRA) curve. We also adopted a rank of possibility to provide a hierarchy of treatments concerning both the location and the variance of all relative treatment effects. The SUCRA value would be 0 if treatment is certain to be the worst and 1 if it is certain to be the best. Inconsistency was globally assessed by comparing the fit of consistency and inconsistency models.
All analyses in this article were performed in R-4.3.1 software with the gemtc package version 0.8, while the JAGS version 4.3.0 was utilized for computing a Markov chain. The detailed codes utilized in this analysis also could be obtained from the correspondence author upon request.
Results
The search process, study characteristics, and quality assessment
A total of 3839 records were identified and 2524 records were left to be assessed after removing 1315 duplications. Then, 2273 irrelevant publications were eliminated by skimming their titles, abstracts, and keywords, leaving 251 articles to be considered potentially eligible. 183 articles were further excluded due to duplications (n = 143); not first-line treatment (n = 15); no accessible data (n = 13); non-RCTs (n = 8) and irrelevant to topic (n = 4). Consequently, 68 articles enrolled into analysis after skimming full-text, and another 6 articles were included by browsing the references. Finally, 74 articles (including 54 studies), published from 2004 to 2021, and with total patients of 25,046 were enrolled into meta-analysis (Fig. 1) [6, 9, 15, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87].
Table 1 showed the basic characteristics of the enrolled studies and participants. 27 treatment regimens involved:
-
1)
“chemotherapy”;
-
2)
Anti-angiogenetic drugs plus chemotherapy, including “Bevacizumab + Chemotherapy” (Beva-Chemo), “Axitinib + Chemotherapy” (Axintinib-Chemo), “Endostar + Chemotherapy” (Endostar-Chemo), “Cediranib + Chemotherapy” (Cediranib-Chemo), “Motesanib + Chemotherapy” (Mote-Chemo), “Sorafenib + Chemotherapy” (Sora-Chemo), “Ramucirumab + Chemotherapy” (Ramu-Chemo) and “Thalidomide + Chemotherapy” (Thali-Chemo);
-
3)
ICIs monotherapy, including “Atezolizumab” (Atezo), “Pembrolizumab” (Pembro), “Cemiplimab” (Cemip), “Durvalumab” (Durva) and “Nivolumab” (Nivo);
-
4)
ICIs plus chemotherapy, including “Atezolizumab + Chemotherapy” (Atezo-Chemo), “Ipilimumab + Chemotherapy” (Ipili-Chemo), “Camrelizumab + Chemotherapy” (Camre-Chemo), “Pembrolizumab + Chemotherapy” (Pembro-Chemo), “Sugemalimab + Chemotherapy” (Sugema-Chemo), “Sintilimab + Chemotherapy” (Sinti-Chemo) and “Tislelizumab + Chemotherapy” (Tisle-Chemo);
-
5)
ICIs (dual-agent), including “Durvalumab + Tremelimumab” (Dura-Treme); “Nivolumab + Ipilimumab” (Nivo-Ipili) and “Pembrolizumab + Ipilimumab” (Pembro-Ipli) and “Nivolumab + Ipilimumab + Chemotherapy” (Nivo-Ipili-Chemo);
-
6)
Anti-angiogenetic drugs plus ICI-chemo, including “Atezolizumab + Bevacizumab + Chemotherapy” (Atezo-Beva-Chemo) and “Nivolumab + Bevacizumab + Chemotherapy” (Nivo-Beva-Chemo) (Fig. 2).
Based on the Cochrane Risk of Bias Tool, 28 studies had an overall high risk of bias, 9 studies had an overall low risk of bias while the other 17 studies had an unclear risk of bias (Supplementary Fig. 1A-B). The domain of “blinding of participants and personnel” contributed to the biggest sources of high risk due to the open-label design of 26 enrolled studies.
Primary outcome—PFS
NMA involved 27 treatment regimens except Endostar-Chemo for PFS analysis (Fig. 3A). Atezo-Beva-Chemo and Nivo-Beva-Chemo had a better survival benefit compared with Beva-Chemo (HR = 0.61, 95% CI: 0.37–1; HR = 0.56, 95% CI: 0.33–0.95, respectively). The trend favored Atezo-Beva-Chemo to Atezo-Chemo in PFS with no statistical significance (HR = 0.71, 95%CI: 0.39–1.31). Camre-Chemo significantly prolonged the PFS compared with Ipili-Chemo (HR = 0.5, 95%CI: 0.29–0.84) and Beva-Chemo (HR = 0.65, 95%CI: 0.46–0.9). In addition, Pembro-Chemo had a significant survival benefit compared to anti-angio-chemo including Beva-Chemo (HR = 0.65, 95%CI: 0.46–0.92), Ramu-Chemo (HR = 0.59, 95%CI: 0.36–0.98) and other regimens. However, Durva-Treme was significantly inferior to the Camre-Chemo (HR = 2.34, 95%CI: 1.21–4.51), Pembro-Chemo (HR = 2.28, 95%CI: 1.24–4.2) and Sinti-Chemo (HR = 2.14, 95%CI: 1.11–4.16) in PFS. Ipili-Chemo was also inferior to the Pembro-Chemo (HR = 1.95, 95%CI: 1.24–3.12) and Sinti-Chemo (HR = 1.84, 95%CI: 1.08–3.13).
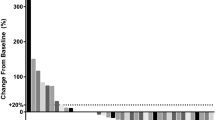
Pooled estimates of the network meta-analysis. A Pooled hazard ratios (95% credible intervals) for progression-free survival(lower triangle) and overall survival(upper triangle). B Pooled odds ratios (95% credible intervals) for objective response rate(lower triangle) and rate of grade3-4 toxicity assessment(upper triangle)
Primary outcome—OS
NMA involved all 27 treatment regimens for OS analysis (Fig. 3A). Atezo-Beva-Chemo performed a divorced trend to Atezo-Chemo regarding OS (HR = 0.94, 95%CI: 0.77–1.16). Camre-Chemo and Sinti-Chemo presented a statistically significant OS benefit compared with the Ipili-Chemo (HR = 0.67, 95%CI: 0.49–0.9; HR = 0.62, 95%CI:0.42–0.90, respectively). Atezo-Chemo and Ipili-Chemo was inferior to Pembro-Chemo in providing OS benefit (HR = 1.31, 95%CI: 1.07–1.62; HR = 1.51, 95%CI: 1.2–1.94). In addition, Nivo-Ipili-Chemo, Pembro-Chemo and Sinti-Chemo obtained a better survival benefit than Beva-Chemo with HR of 0.72 (95%CI: 0.55–0.94), 0.69 (95%CI: 0.56–0.83), and 0.64 (95%CI: 0.46–0.91), respectively. Noteworthy, almost all regimens were superior to Endostar-Chemo in improving OS.
Primary outcome—ORR
NMA involved 27 treatment regimens for ORR analysis (Fig. 3B). Atezo-Beva-Chemo improved ORR significantly compared to the Atezo-Chemo (OR = 2.73, 95%CI: 1.27–5.87) and Bevi-Chemo (OR = 1.88, 95%CI: 1.01- 3.51). Likewise, Nivo-Beva-Chemo also yield a significantly higher ORR than Durva-Chemo (OR = 4.24, 95%CI: 1.59–11.31), and Atezo-Chemo (OR = 2.28, 95%CI: 1.05–4.95) (OR = 3.48,95%CI: 1.46–8.03). However, ORR was significantly lower in the Durva-Treme group comparing to ICI-chemo regimens, including with ORR of 0.31 to Camre-Chemo (95%CI: 0.13–0.73) and 0.26 to Pembro-Chemo (95%CI: 0.11–0.57). ORR was lower in the Pembor-Ipi group comparing to the Pembro-Chemo group (OR = 0.38, 95%CI: 0.16–0.92). Similarly, ORR was significantly lower in the Ipili-Chemo group comparing to Pembro-Chemo (OR = 0.31, 95%CI: 0.17–0.59) and Tisle-Chemo (OR = 0.41, 95%CI: 0.20–0.85). In addition, ORR was significantly improved in the Camre-Chemo group comparing to the Ipili-Chemo group (OR = 2.64, 95%CI: 1.29–5.21). ORR was significantly lower in Atezo-Chemo group comparing to the Pembro-Chemo group (OR = 0.48, 95%CI: 0.28–0.81).
Primary outcome— rate of grade3-4 toxicity assessment
NMA involved 27 treatment regimens for rate of grade3-4 toxicity assessment (Fig. 3B). No significant difference was observed between Atezo-Beva-Chemo and Atezo-Chemo (OR = 1.18, 95%CI: 0.56–2.42) in the rate of grade3-4 toxicity. Meanwhile, Durva-Treme served lower rate of grade3-4 toxicity comparing to Pembro-Chemo (OR = 0.46, 95%CI: 0.24–0.87), Sinti-Chemo (OR = 0.49, 95%CI: 0.24–0.99) and Tisle-Chemo (OR = 0.37, 95%CI: 0.18–0.76). Likewise, Pembro-Ipili served lower than Ipili-Chemo (OR = 0.33, 95%CI: 0.15–0.76) and Pembro-Chemo (OR = 0.44, 95%CI: 0.21–0.95).
Subgroup analysis of PFS and OS stratified by PD-L1 expression level
-
1)
For PD-L1-negative patients, NMA involved 11 treatment regimens for PFS and 7 treatment regimens for OS (Fig. 4A). Atezo-Beva-Chemo and Atezolizumab alone appeared to obtain more survival benefit than Chemotherapy alone in prolonging PFS with HR of 0.46 (95%CI: 0.22–0.91) and 0.67 (95%CI: 0.45–0.95), respectively. In addition, the PFS of both Pembro-Chemo and Sinti-Chemo was obtain significantly higher PFS benefits than Chemotherapy alone with HR of 0.60 (95%CI: 0.38–0.86) and 0.60 (95%CI: 0.36–0.99), respectively. Meanwhile, Pembro-Chemo significantly pronged OS compared with Chemotherapy (HR = 0.63, 95%CI: 0.43–0.90) (Fig. 4A).
-
2)
For PD-L1-intermediate patients, NMA involved 10 treatment regimens for PFS and 7 treatment regimens for OS (Fig. 4B). Atezo-Beva-Chemo yielded a better PFS benefit comparing to Beva-Chemo (HR = 0.55, 95%CI: 0.33–0.91) and “Chemotherapy” alone (HR = 0.56, 95%CI: 0.31–1). In addition, Pembro-Chemo and Sinti-Chemo yielded a better PFS benefit comparing to Chemotherapy alone (HR = 0.53, 95%CI: 0.36–0.79; HR = 0.57, 95%CI: 0.36–0.90). No significant differences in OS were observed among all regimens for PD-L1-intermediate patients.
-
3)
For PD-L1-high patients, NMA involved 13 treatment regimens for PFS and 9 treatment regimens for OS (Fig. 4C). Atezo-Beva-Chemo had a better PFS benefit than Beva-Chemo (HR = 0.33, 95%CI: 0.16–0.67) and “Chemotherapy” (HR = 0.24, 95%CI: 0.11–0.55). Also, Atezo-Chemo could significantly prolong PFS comparing to Chemotherapy alone (HR = 0.46, 95% CI: 0.30–0.72). Cemiplimab appeared to extend PFS versus “Chemotherapy” (HR 0.54, 95%CI 0.29–1). Pembro-Chemo (HR = 0.36, 95% CI: 0.23–0.59), Sinti-Chemo (HR = 0.38, 95%CI: 0.2–0.63) and Tisleli-Chemo (HR = 0.40, 95%CI: 0.22–0.70) had a better PFS benefit comparing to Chemotherapy alone. Pembro-Chemo and “Pembrolizumab” monotherapy yielded better OS benefits than “Chemotherapy” alone (HR = 0.67, 95%CI: 0.45–0.98; HR = 0.61, 95%CI: 0.38–0.98; respectively).
Subgroup analysis of PFS and OS stratified by other risk factors
Survival analysis was stratified by histology, sex, age, smoking status, ECOG status, and brain metastasis status (Supplementary Fig. 2). For non-squamous NSCLC patients, ICI-chemos including Atezo-Chemo, Pembro-Chemo, Sinti-Chemo, and Beva-Chemo obtained significantly better PFS benefits than Chemotherapy alone with HR of 0.60 (95%CI: 0.36–1.00), 0.50 (95%CI: 0.29–0.87), 0.48 (95%CI:0.22–1.0) and 0.66 (95%CI:0.45–1.0), respectively. Meanwhile, Pembrolizumab, Pembro-Chemo, Sinti-Chemo, Nivol-Ipili-Chemo could significantly extend OS comparing to Chemotherapy alone with HR of 0.58 (95%CI: 0.37–0.92), 0.59 (95%CI: 0.45–0.82), 0.61(95%CI: 0.37–1.0) and 0.69 (95%CI: 0.47–1.0), respectively. However, for squamous advanced NSCLC patients, no regimens could significantly extend PFS except Sugema-Chemo (HR = 0.33, 95%CI: 0.11–1.0). As for subgroup analysis according to other risk factors including sex, age, smoking status, and ECOG status, results were generally consistent with those above-mentioned unselected patients.
Rank probabilities for primary outcomes
As it was presented in Supplementary Table 1, the results of the Bayesian ranking profile were consistent with the pooled analysis using HR and OR. Nivo-Beva-Chemo was most likely to be ranked first for PFS (cumulative probability 37%), Sinti + Chemo for OS (30%), Atezo-Beva-Chemo for ORR (50%), and “Nivolumab” for decreasing rate of grade3-4 toxicity assessment. In contrast, “Nivolumab” was to be ranked worst for PFS (31%). Endostar + Chemotherapy for OS (99%), Nivolumab for ORR (39%), and Sora-Chemo for decreasing rate of grade3-4 toxicity (67%).
Bayesian ranking profile based on SUCRA results was also in line with the HR and OR estimates (Fig. 5). Nivo-Beva-Chemo appeared to have the highest probability of pronging PFS (SUCRA = 0.898), followed by Camre-Chemo (0.862), Atezo-Beva-Chemo (0.86), and Pembro-Chemo (0.854). Concerning the extension of OS, Sinti-Chemo had the highest probability to be the best regimen (0.885), followed by Pembro-Chemo (0.866) and Camre-Chemo (0.843). In terms of ORR, Atezo-Beva-Chemo was most likely to improve ORR (0.944), followed by Nivo-Beva-Chemo (0.89), Pembro-Chemo (0.887) and Camre-Chemo (0.788). However, “Nivolumab” appeared to have the best grade 3–4 safety profile (0.987), followed by “Pembrolizumab” (0.914) and “Durvalumab” (0.910).
Secondary outcomes—DCR, any grade toxicity assessment, rate of side effects leading to discontinuation and death
NMA involved 20 treatment regimens for DCR, 18 regimens for any grade toxicity assessment, 22 regimens for rate of side effects leading to drug discontinuation, and 19 regimens for rate of side effects leading to death. Bayesian ranking profile of secondary outcomes based on SUCRA was presented in Supplementary Fig. 3. Pembro-Chemo had the highest probability for improving DCR (SUCRA = 0.768), followed by Atezo-Chemo (0.746) and Camre-Chemo (0.745). However, as for any grade toxicity assessment, Endostar-Chemotherapy had the best probability for reducing all grade toxicity assessment (0.954), followed by Sinti-Chemo (0.872). In terms of decreasing rate of side effects leading to drug discontinuation, “Durvalumab” had the lowest risk (0.961), followed by Sinti-Chemo (0.887). In addition, Sinti-Chemo had the lowest risk of suffering from death caused by side effects (0.851), followed by “Atezolizumab” (0.709).
Secondary outcome—specific adverse events
NMA involved 25 regimens for anemia, 24 regimens for neutropenia, 21 regimens for thrombocytopenia, 22 regimens for fatigue, 19 regimens for diarrhea, 25 treatment regimens for nausea/vomiting, and 15 regimens for asthenia. Bayesian ranking profile of specific adverse events based on SUCRA was showed on Supplementary Fig 4. Durva-Treme had the lowest risk of anemia (SUCRA = 0.983) and asthenia (0.739). Meanwhile, “Durvalumab” had the lowest risk of thrombocytopenia (0.959). In addition, “Nivolumab” had the lowest risk of fatigue (0.939), while “Cemiplimab” had the lowest risk of diarrhea (0.958), and “Pembrolizumab” had the lowest risk of nausea/vomiting (0.964).
Secondary outcome—Cost-effectiveness analysis
Table 2 summarized the 21 reviewed studies about the cost-effectiveness analysis based on our above-mentioned enrolled studies, including Beyond [65], CheckMate 227 [66], E4599 [67], LOGIK0201 [55], Impower-110 [68, 69], Impower-130 [70, 71], Keynote-021G [72], Keynote-024 [73,74,75,76], Keynote-042 [24, 26, 39], Keynote-189 [25, 38], Keynote-407 [38, 77, 78] and Pronounce [40] trials. The quality-adjusted life-year (QALY), incremental cost-effectiveness ratio (ICER), life-years (LY), and total cost were commonly used for effectiveness measures. All reviewed studies except three studies applied sensitivity analysis to deal with the effect of uncertainty in results and their generalization ability. The annual discount rate ranged from 3 to 5%.
For Beva-Chemo, ICER was reported to be $130,937.09/QALY (Beyond trial in China) and $559,609.48/QALY (E4599 trial in USA) compared with Chemotherapy alone. Concerning the comparison between Atezolizumab and Chemotherapy alone, ICER was reported to be $168,902.66/QALY in China and $170,730/QALY in the USA (Impower-110 trial). In addition, Atezo-Chemo versus Chemotherapy alone could achieve ICER at $325,328.71/QALY in China and $ 333,199/QALY in the USA (Impower-130 trial). As for Pembrolizumab versus Chemotherapy in Keynote-024 trial, ICER was reported to be $865,189 /QALY (HongKong China), CHF 77,060/QALY(Switzerland), $97,621/QALY (USA) and $64,205/QALY (Portugal). Meanwhile, based on Keynote-042 trial, Pembrolizumab versus “Chemotherapy” could achieve ICER at $39,404/QALY (China) and $130,155/QALY (USA). As for Pembro-Chemo versus Chemotherapy alone, ICER was reported to be $104,823/QALY (Keynote-189 trial in the USA), $116,606/QALY (Keynote-407 trial in France), and $86,293/QALY (Keynote-407 trial in the USA).
Inconsistency assessment
The fit of the consistency model was similar or even better than that of the inconsistency model (Supplementary Table 2).
Discussion
Currently, there is no “head-to-head” trial comparing ICI-chemo versus anti-angio-chemo to validate their comparative efficacy and safety. Meanwhile, ICI plus Beva-Chemo holds the potential to obtain better survival benefits but may be at the expense of toxicities. Nevertheless, the true impact of adding anti-angiogenetic agents to ICI-chemo remains inconclusive. The development of ICIs has resulted in a shift in the first-line treatment landscape for NSCLC patients. Constantly increasing new drugs or therapeutic combinations are formally approved. In this study, we enrolled well-designed RCTs and conducted a Bayesian NMA to compare the efficacy, safety, and cost-effectiveness of different first-line treatment regimens for advanced NSCLC patients. The diversity of responses to different regimens and corresponding toxicity concerns were observed in this study.
Optimal therapeutic strategies could delay the occurrence of drug resistance thus potentially redefining the survival outcome. Atezo-Beva-Chemo was the best regimen to improve significantly ORR comparing to Atezo-Chemo and Beva-Chemo. Atezo-Beva-Chemo and Nivo-Beva-Chemo obtained better survival benefits compared with Beva-Chemo. There was a trend for Atezo-Beva-Chemo to perform better than Atezo-Chemo in assessment of PFS (HR = 0.71, 95%CI: 0.39–1.31). A better trend for Atezo-Beva-Chemo compared to Atezo-Chemo in OS was also revealed (HR 0.94, 95%CI 0.77–1.16). Of note, Nivo-Beva-Chemo was most likely to be ranked first for extending PFS (cumulative probability 37%), while Atezo-Beva-Chemo had the highest probability to be ranked first for improving ORR (50%). Our results suggested that the efficacy could be enhanced after adding Bevacizumab to the ICI-chemo. Therapeutically, the immune-suppressive microenvironment could be converted to be immune-permissive through the immunomodulatory effects of antiangiogenic agents, thus improving the capacity of ICIs [13, 14]. Meanwhile, in terms of side effects, no significant difference was observed between ICI-chemo and Atezo-Beva-Chemo or Nivo-Beva-Chemo. Adding bevacizumab into ICI-chemo seemed to provide additional benefits without adding a significant treatment burden. Remarkably, serval ongoing registered trials [88, 89] have been conducted to investigate the clinical benefit of adding anti-angiogenic agents into ICI-chemo in patients with advanced NSCLC.
Meanwhile, Camre-Chemo, Pembro-Chemo, Sinti-Chemo, and Tisle-Chemo also showed advantages over Beva-Chemo in providing PFS benefit. Notably, Sinti-Chemo and Pembro-Chemo showed better OS benefits than Beva-Chemo. Sinti-Chemo ranked best to be the regimen of extending OS benefits. In particular, Endostar-Chemo ranked the worst for OS benefits. The reason of worse efficacy of anti-angio-chemo may be associated with the resistant mechanism and compensatory pathway of angiogenesis in tumor [90]. PD-1 inhibitors in combination with platinum-based chemotherapy hold the potential to prolong patients’ life expectancy. However, our results should be interpreted with caution due to the variety of follow-up periods and post-progression interventions in different treatment groups. Therefore, further mature OS data and head-to-head RCTs were warranted to be performed. In terms of the rate of grade3-4 toxicity, no significant difference was observed between ICI-chemo and anti-angio-chemo. As for cost-effectiveness analysis, it seemed that ICI-chemo yielded more improvement in QALY than Beva-Chemo. In conclusion, ICI-chemo is associated with potentially higher survival and better cost-effectiveness outcomes than anti-angio-chemo with comparable safety profiles.
Noteworthy, Ipili-Chemo (CTLA-4 inhibitors plus chemotherapy) was inferior to Camre-Chemo, Pembro-Chemo and Tisleli-Chemo in improving ORR and extending survival. In comparison with CTLA-4, our results inferred that PD-1/PDL-1 may play a more important role in the immune response for patients with advanced NSCLC. However, there was no significant difference between the PD-1/PDL-1 and CTLA-4 inhibitors monotherapy. Of note, Durva-Treme was significantly inferior to the ICI-Chemo regarding the ORR and PFS benefit, with lower rate of grade3-4 toxicity. It is reasonable to interpret that ICIs (dual agent) monotherapy are not the optimal therapeutic methods in obtaining survival benefit despite their superior safety profiles. Nevertheless, Nivo-Ipili-Chemo obtained a better survival benefit than Beva-Chemo. Anti-PD-1 and anti-CTLA-4 antibody are ICIs with distinct but complementary mechanisms of action. Consequently, ICIs (dual agent), especially PD-1 plus CTLA4 inhibitors, in combination with chemotherapy may represent the focus in designing the future clinical trials.
In addition, Pembro-Chemo could significantly perform better than Atezo-Chemo in ORR at this study. Likewise, our results suggested that Sinti-Chemo and Pembro-Chemo showed more OS benefits than Atezo-Chemo. A potential biological explanation is that Pembrolizumab and Sintilimab (PD-1 inhibitors) rather than Atezolimumab (PD-L1 inhibitors) block the binding between PD-1 and corresponding ligands PD-L2, which is estimated to be 2–6 folds stronger than the affinity of PD-1 binding to PD-L1 [88]. However, no statistically significant difference was observed between Pembrolizumab and Atezolimumab monotherapy. Although this could be partly explained by the imbalance in the basic characteristics of the enrolled studies, the underlying mechanism still warranted further exploration. Given the promising results of PD-1 inhibitors plus chemotherapy, further research is supposed to shed light on the combination of PD-1 inhibitors plus chemotherapy and anti-angiogenetic agents, e.g. Pembrolizumab + Bevacizumab + Chemotehrapy.
The diversity of responses to ICIs has raised the questions about how to better tailor the treatment strategy and choose the best-targeted population. The PD-L1 expression status is a potential biomarker [89]. For PD-L1 negative patients, Atezol-Beva-Chemo, Pembro-Chemo and Sinti-Chemo obtained more survival benefit than Chemotherapy alone in prolonging PFS. Moreover, Pembro-Chemo showed advantages over Chemotherapy alone in the extension of OS. Chemotherapy induces recruitment of CD8 + cells and provides an appropriate binding site for ICIs [7]. For PD-L1 intermediate patients, Atezoli-Beva-Chemo yielded the best survival benefit compared with Beva-Chemo and Chemotherapy alone. In addition, Pembro-Chemo and Sinti-Chemo serves better than Chemotherapy alone in these settings. For PD-L1 high NSCLC patients, Atezo-Beva-Chemo had significantly longer PFS than Beva-Chemo and Chemotherapy. Also, Atezo-Chemo, Pembro-Chemo, Sinti-Chemo and Tisle-Chemo could significantly prolong PFS compared with Chemotherapy alone. Pembro-Chemo yielded a better OS survival than Chemotherapy alone. These results were generally consistent with the above-mentioned results in the unselected patients and previously reported results. Of note, Atezol-Beva-Chemo, Pembro-Chemo and Sinti-Chemo obtained more survival benefit than Chemotherapy alone in prolonging PFS, irrespective off the PD-L1 expression level. Furthermore, Pembro-Chemo is the only regimen to extend OS for PD-L1 negative or PD-L1 high patients. Nevertheless, given the relatively limited data of targeted treatment regimens, the variety of detection methods or predefined thresholds of PD-L1 expression, our results should be interpreted with caution. Some misclassification bias could lead to underestimation or overestimation of treatment results in various PD-L1 cohorts.
The immune microenvironment of squamous NSCLC patients presents different [91,92,93]. For squamous advanced NSCLC patients, we found that except “Suge-Chemo”, no regimens could significantly extend PFS. However, results in the non-squamous NSCLC patients’ group were generally in line with the unselected group. This distinct result in different pathological types highlights the urgent need for further exploration of the mechanism behind the tumor microenvironment.
The toxicity and adverse events are the major concern when prescribing the combined regimens. Consistent with previously studies, our results showed that ICIs monotherapy had the best safety profile compared with chemotherapy and other regimens [16, 33]. Our results provided further evidence supporting the toxicity assessment of different combined regimens. Compared with ICIs monotherapy, our results suggested that better efficacy may occur in the combined regimens (ICIs plus chemotherapy) with increasing side effects. As for the cost-effectiveness analysis, ICIs monotherapy or ICI-chemo yielded more improvement in QALY than Beva-Chemo. In addition, Pembro-Chemo appeared to obtain more QALY benefits than Atezo-Chemo. Due to the differences in the study horizons and the costs of expenditure, our results warrant further confirmation.
To the best of our knowledge, the present study presents the most comprehensive NMA to compare ICI-chemo with anti-angio-chemo. Although a published indirect-comparison has demonstrated that ICI-chemo is superior to Beva-Chemo in first-line treatment for non-squamous NSCLC, they failed to observe the respective characteristics of different therapeutic regimens [94]. Another highlight of our analysis is to answer an important question of whether anti-angiogenetic agents plus ICI-chemo could provide additional benefits or change the safety profile compared with ICI-chemo for the first time. A large-scale number of subjects involved in a meta-analysis is critically important to reduce the statistical errors. Concerning the first-line treatment landscape for advanced NSCLC, the current study enrolled the largest scale of patients so far.
There were some limitations in this study. Firstly, several included studies were conference abstracts, where we could not obtain all data and assess the risk of bias. Secondly, the original data was limited since some trials were ongoing. Thirdly, uniform methods in assessment of PD-L1 expression status exerted a negative effect on the subgroup analysis stratified by PD-L1 expression level. Last but not least, various follow-up periods and trial designs of enrolled studies imposed the heterogeneity of the present study.
In summary, our results suggest that ICI-chemo is associated with better survival benefits and cost-effectiveness outcomes than anti-angio-ICI with comparable safety profiles. Adding bevacizumab to ICI-chemo seemed to provide additional therapeutic benefits without extra treatment burden. Atezol-Beva-Chemo, Pembro-Chemo and Sinti-Chemo could obtain more survival benefits than Chemotherapy alone in prolonging PFS irrespective off the PD-L1 expression level. Our findings could supplement the current standard of care and lead the design of the future clinical trials in the first-line treatment of patients with advanced NSCLC.
Availability of data and material
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- CI:
-
Confidence interval
- CTLA-4:
-
Anti-cytotoxic T-lymphocyte antigen 4
- DCR:
-
Disease-controlled rate
- HR:
-
Hazard ratio
- ICIs:
-
Immune checkpoint inhibitors
- NMA:
-
Bayesian Network Meta-analysis
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- ORR:
-
Objective response rate
- OR:
-
Odds ratio
- PD-1:
-
Programmed death 1
- PFS:
-
Progression free survival
- RCTs:
-
Randomized controlled trials
- SE:
-
Standard error
- SUCRA:
-
Surface under the cumulative ranking
- TKIs:
-
Tyrosine kinase inhibitors
- VEGF:
-
Vascular endothelial growth factor
References
Sung H, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Arbour KC, Riely GJ. Systemic Therapy for Locally Advanced and Metastatic Non-Small Cell Lung Cancer: A Review. JAMA. 2019;322(8):764–74.
Xiao YY, et al. Chemotherapy plus multitargeted antiangiogenic tyrosine kinase inhibitors or chemotherapy alone in advanced NSCLC: a meta-analysis of randomized controlled trials. Eur J Clin Pharmacol. 2013;69(2):151–9.
Ellis PM, Al-Saleh K. Multitargeted anti-angiogenic agents and NSCLC: clinical update and future directions. Crit Rev Oncol Hematol. 2012;84(1):47–58.
Sandler A, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–50.
Lynch TJ, et al. Ipilimumab in combination with paclitaxel and carboplatin as first-line treatment in stage IIIB/IV non-small-cell lung cancer: results from a randomized, double-blind, multicenter phase II study. J Clin Oncol. 2012;30(17):2046–54.
Apetoh L, et al. Combining immunotherapy and anticancer agents: the right path to achieve cancer cure? Ann Oncol. 2015;26(9):1813–23.
Zitvogel L, et al. Mechanism of action of conventional and targeted anticancer therapies: reinstating immunosurveillance. Immunity. 2013;39(1):74–88.
Mok TSK, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819–30.
Das R, et al. Combination therapy with anti-CTLA-4 and anti-PD-1 leads to distinct immunologic changes in vivo. J Immunol. 2015;194(3):950–9.
Sharma P, Allison JP. Dissecting the mechanisms of immune checkpoint therapy. Nat Rev Immunol. 2020;20(2):75–6.
Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10.
Hegde PS, Wallin JJ, Mancao C. Predictive markers of anti-VEGF and emerging role of angiogenesis inhibitors as immunotherapeutics. Semin Cancer Biol. 2018;52(Pt 2):117–24.
Voron T, et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T cells in tumors. J Exp Med. 2015;212(2):139–48.
Socinski MA, et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–301.
Liang H, et al. PD-(L)1 inhibitors vs. chemotherapy vs. their combination in front-line treatment for NSCLC: An indirect comparison. Int J Cancer. 2019;145(11):3011–21.
Deng T, et al. Clinical Observation on the Bevacizumab Combined with Pemetrexed plus Cisplatin in the Treatment of Non-small Cell Lung Cancer. Anti-tumor Pharmacy. 2014;4(03):193–6.
Herbst RS, et al. Atezolizumab for First-Line Treatment of PD-L1-Selected Patients with NSCLC. N Engl J Med. 2020;383(14):1328–39.
Jotte R, et al. Atezolizumab in Combination With Carboplatin and Nab-Paclitaxel in Advanced Squamous NSCLC (IMpower131): Results From a Randomized Phase III Trial. J Thorac Oncol. 2020;15(8):1351–60.
West H, et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):924–37.
Nishio M, et al. Atezolizumab Plus Chemotherapy for First-Line Treatment of Nonsquamous NSCLC: Results From the Randomized Phase 3 IMpower132 Trial. J Thorac Oncol. 2021;16(4):653–64.
Zhou C, et al. BEYOND: A Randomized, Double-Blind, Placebo-Controlled, Multicenter, Phase III Study of First-Line Carboplatin/Paclitaxel Plus Bevacizumab or Placebo in Chinese Patients With Advanced or Recurrent Nonsquamous Non-Small-Cell Lung Cancer. J Clin Oncol. 2015;33(19):2197–204.
Zhou C, et al. Camrelizumab plus carboplatin and pemetrexed versus chemotherapy alone in chemotherapy-naive patients with advanced non-squamous non-small-cell lung cancer (CameL): a randomised, open-label, multicentre, phase 3 trial. Lancet Respir Med. 2021;9(3):305–14.
Zhou K, Jiang C, Li Q. Cost-effectiveness analysis of pembrolizumab monotherapy and chemotherapy in the non-small-cell lung cancer with different PD-L1 tumor proportion scores. Lung Cancer. 2019;136:98–101.
Insinga RP, et al. Cost-effectiveness of pembrolizumab in combination with chemotherapy in the 1st line treatment of non-squamous NSCLC in the US. J Med Econ. 2018;21(12):1191–205.
Huang M, et al. Cost-effectiveness of pembrolizumab versus chemotherapy as first-line treatment in PD-L1-positive advanced non-small-cell lung cancer in the USA. Immunotherapy. 2019;11(17):1463–78.
Rizvi NA, et al. Durvalumab With or Without Tremelimumab vs Standard Chemotherapy in First-line Treatment of Metastatic Non-Small Cell Lung Cancer: The MYSTIC Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020;6(5):661–74.
Yang Y, et al. Efficacy and Safety of Sintilimab Plus Pemetrexed and Platinum as First-Line Treatment for Locally Advanced or Metastatic Nonsquamous NSCLC: a Randomized, Double-Blind, Phase 3 Study (Oncology pRogram by InnovENT anti-PD-1-11). J Thorac Oncol. 2020;15(10):1636–46.
Li N, et al. Efficacy of endostar combined with chemotherapy in multi-cycle treatment of patients with advanced non-small cell lung cancer. Zhonghua Zhong Liu Za Zhi. 2011;33(12):937–42.
Carbone DP, et al. First-Line Nivolumab in Stage IV or Recurrent Non-Small-Cell Lung Cancer. N Engl J Med. 2017;376(25):2415–26.
Paz-Ares L, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(2):198–211.
Cheng, Y., et al., LBA20Keynote-407 China Extension study: Pembrolizumab (pembro) plus chemotherapy in Chinese patients with metastatic squamous NSCLC. Ann Oncol. 2019;30(Suppl 9):mdz446.
Awad MM, et al. Long-Term Overall Survival From KEYNOTE-021 Cohort G: Pemetrexed and Carboplatin With or Without Pembrolizumab as First-Line Therapy for Advanced Nonsquamous NSCLC. J Thorac Oncol. 2021;16(1):162–8.
Berling M, et al. MO01.02 Cost-Effectiveness Analysis of Nivolumab Plus Ipilimumab in the First-Line Treatment of Metastatic Non-Small Cell Lung Cancer in the United States. J Thoracic Oncol. 2021;16:S15–6.
Novello S, et al. Motesanib plus carboplatin/paclitaxel in patients with advanced squamous non-small-cell lung cancer: results from the randomized controlled MONET1 study. J Thorac Oncol. 2014;9(8):1154–61.
Hellmann MD, et al. Nivolumab plus Ipilimumab in Advanced Non-Small-Cell Lung Cancer. N Engl J Med. 2019;381(21):2020–31.
Reck M, et al. Overall survival with cisplatin-gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non-small-cell lung cancer: results from a randomised phase III trial (AVAiL). Ann Oncol. 2010;21(9):1804–9.
Insinga R, et al. PCN41 Cost-Effectiveness of Pembrolizumab in Combination with Chemotherapy in the 1ST LINE Treatment of Metastatic NSCLC in Taiwan. Value Health Reg Issues. 2020;22:S12.
Xu H, Ma AX. PCN175 Cost-effectiveness analysis of pembrolizumab versus chemotherapy as first-line treatment for metastatic non-small cell lung cancer with different PD-L1 expression levels in China using both partition survival and markov models. Value in Health. 2020;23:S53–4.
Tfayli A, et al. PCN197-Cost utility analysis of first-line paclitaxel with carboplatin and bevacizumab followed by maintenance bevacizumab versus pemetrexed in patients with advanced non-squamous non-small cell lung cancer in Lebanon. Value in Health. 2018;21:S47.
Gandhi L, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med. 2018;378(22):2078–92.
Boyer M, et al. Pembrolizumab Plus Ipilimumab or Placebo for Metastatic Non-Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score ≥ 50%: Randomized, Double-Blind Phase III KEYNOTE-598 Study. J Clin Oncol. 2021;39(21):2327–38.
Reck M, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2016;375(19):1823–33.
Thomas, S., et al. A phase 2 randomized open-label study of ramucirumab (RAM) plus first-line platinum-based chemotherapy in patients (pts) with recurrent or advanced non-small cell lung cancer (NSCLC): Final results from squamous pts. Ann Oncol. 2017;28:ii42–ii43.
Doebele RC, et al. Phase 2, randomized, open-label study of ramucirumab in combination with first-line pemetrexed and platinum chemotherapy in patients with nonsquamous, advanced/metastatic non-small cell lung cancer. Cancer. 2015;121(6):883–92.
Kubota K, et al. Phase III study (MONET1) of motesanib plus carboplatin/paclitaxel in patients with advanced nonsquamous nonsmall-cell lung cancer (NSCLC): Asian subgroup analysis. Ann Oncol. 2014;25(2):529–36.
Scagliotti G, et al. Phase III study of carboplatin and paclitaxel alone or with sorafenib in advanced non-small-cell lung cancer. J Clin Oncol. 2010;28(11):1835–42.
Govindan R, et al. Phase III Trial of Ipilimumab Combined With Paclitaxel and Carboplatin in Advanced Squamous Non-Small-Cell Lung Cancer. J Clin Oncol. 2017;35(30):3449–57.
Paz-Ares LG, et al. Phase III, randomized, double-blind, placebo-controlled trial of gemcitabine/cisplatin alone or with sorafenib for the first-line treatment of advanced, nonsquamous non-small-cell lung cancer. J Clin Oncol. 2012;30(25):3084–92.
Kubota K, et al. Phase III, Randomized, Placebo-Controlled, Double-Blind Trial of Motesanib (AMG-706) in Combination With Paclitaxel and Carboplatin in East Asian Patients With Advanced Nonsquamous Non-Small-Cell Lung Cancer. J Clin Oncol. 2017;35(32):3662–70.
Zinner RG, et al. PRONOUNCE: randomized, open-label, phase III study of first-line pemetrexed + carboplatin followed by maintenance pemetrexed versus paclitaxel + carboplatin + bevacizumab followed by maintenance bevacizumab in patients ith advanced nonsquamous non-small-cell lung cancer. J Thorac Oncol. 2015;10(1):134–42.
Laurie SA, et al. Randomised, double-blind trial of carboplatin and paclitaxel with daily oral cediranib or placebo in patients with advanced non-small cell lung cancer: NCIC Clinical Trials Group study BR29. Eur J Cancer. 2014;50(4):706–12.
Lee SM, et al. Randomized double-blind placebo-controlled trial of thalidomide in combination with gemcitabine and Carboplatin in advanced non-small-cell lung cancer. J Clin Oncol. 2009;27(31):5248–54.
Niho S, et al. Randomized phase II study of first-line carboplatin-paclitaxel with or without bevacizumab in Japanese patients with advanced non-squamous non-small-cell lung cancer. Lung Cancer. 2012;76(3):362–7.
Fukuda M, et al. Randomized phase II study of pemetrexed or pemetrexed plus bevacizumab for elderly patients with previously untreated non-squamous non-small cell lung cancer: Results of the Lung Oncology Group in Kyushu (LOGIK1201). Lung Cancer. 2019;132:1–8.
Belani CP, et al. Randomized phase II study of pemetrexed/cisplatin with or without axitinib for non-squamous non-small-cell lung cancer. BMC Cancer. 2014;14:290.
Zhao X, et al. A randomized phase II study of recombinant human endostatin plus gemcitabine/cisplatin compared with gemcitabine/cisplatin alone as first-line therapy in advanced non-small-cell lung cancer. Invest New Drugs. 2012;30(3):1144–9.
Johnson DH, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 2004;22(11):2184–91.
Goss GD, et al. Randomized, double-blind trial of carboplatin and paclitaxel with either daily oral cediranib or placebo in advanced non-small-cell lung cancer: NCIC clinical trials group BR24 study. J Clin Oncol. 2010;28(1):49–55.
Paz-Ares L, et al. A Randomized, Placebo-Controlled Trial of Pembrolizumab Plus Chemotherapy in Patients With Metastatic Squamous NSCLC: Protocol-Specified Final Analysis of KEYNOTE-407. J Thorac Oncol. 2020;15(10):1657–69.
Zhou C., et al. Sintilimab Plus Platinum and Gemcitabine as First-Line Treatment for Advanced or Metastatic Squamous NSCLC: Results From a Randomized, Double-Blind, Phase 3 Trial (ORIENT-12). J Thorac Oncol. 2021;16(9):1501–11.
Chen Q, et al. A Study of Endostar Combined with Gemcitabine in the First-Line Treatment of the Elderly Patients with Advanced Non-Small Cell Lung Cancer. J Thorac Oncol. 2017;12(1):S889–90.
Lu S., et al. Tislelizumab Plus Chemotherapy as First-Line Treatment for Locally Advanced or Metastatic Nonsquamous NSCLC (RATIONALE 304): A Randomized Phase 3 Trial. J Thorac Oncol. 2021;16(9):1512–22.
Wang J, et al. Tislelizumab plus chemotherapy vs chemotherapy alone as first-line treatment for advanced squamous non-small-cell lung cancer: a Phase 3 randomized clinical trial. JAMA Oncol. 2021;7(5):709–17.
Li X, Li W, Hou L. A Trial-Based Cost-Effectiveness Analysis of Bevacizumab and Chemotherapy Versus Chemotherapy Alone for Advanced Nonsquamous Non-Small-Cell Lung Cancer in China. Value Health Reg Issues. 2019;18:1–7.
Courtney PT, et al. Cost-effectiveness of Nivolumab-Ipilimumab Combination Therapy for the Treatment of Advanced Non-Small Cell Lung Cancer. JAMA Netw Open. 2021;4(5):e218787.
Goulart B, Ramsey S. A trial-based assessment of the cost-utility of bevacizumab and chemotherapy versus chemotherapy alone for advanced non-small cell lung cancer. Value Health. 2011;14(6):836–45.
Liu G, et al. Cost-effectiveness analysis of Atezolizumab versus chemotherapy as first-line treatment for metastatic non-small-cell lung cancer with different PD-L1 Expression Status. Front Oncol. 2021;11:669195.
Peng Y, et al. First-Line Atezolizumab for Metastatic NSCLC with High PD-L1 Expression: A United States-Based Cost-Effectiveness Analysis. Adv Ther. 2021;38(5):2447–57.
Lin S, et al. Cost-effectiveness of atezolizumab plus chemotherapy for advanced non-small-cell lung cancer. Int J Clin Pharm. 2020;42(4):1175–83.
Yang Z., et al. First-line atezolizumab plus chemotherapy in advanced non-squamous non-small cell lung cancer: a cost-effectiveness analysis from China. Expert Rev Pharmacoecon Outcomes Res. 2021;21(5):1061–67.
Page R, et al. Expanding indications of existing drugs and associated costs under risk reimbursement models. J Clin Oncol. 2017;35:e18306–e18306.
Loong HH, et al. Cost Effectiveness of PD-L1-Based Test-and-Treat Strategy with Pembrolizumab as the First-Line Treatment for Metastatic NSCLC in Hong Kong. Pharmacoecon Open. 2020;4(2):235–47.
Pinheiro B, et al. Cost-Effectiveness of Pembrolizumab for The First-Line Treatment of Metastatic Non-Small Cell Lung Carcinoma in Portugal. Value in Health. 2017;20:A432.
Bhadhuri A, et al. Cost effectiveness of pembrolizumab vs chemotherapy as first-line treatment for metastatic NSCLC that expresses high levels of PD-L1 in Switzerland. Swiss Med Wkly. 2019;149:w20170.
Huang M, et al. Cost Effectiveness of Pembrolizumab vs. Standard-of-Care Chemotherapy as First-Line Treatment for Metastatic NSCLC that Expresses High Levels of PD-L1 in the United States. Pharmacoeconomics. 2017;35(8):831–44.
Insinga RP, et al. Cost-effectiveness of pembrolizumab in combination with chemotherapy versus chemotherapy and pembrolizumab monotherapy in the first-line treatment of squamous non-small-cell lung cancer in the US. Curr Med Res Opin. 2019;35(7):1241–56.
Chouaid C, et al. Cost-effectiveness of pembrolizumab (Keytruda (R)) in combination with chemotherapy for first-line treatment of metastatic squamous non-small cell lung cancer (NSCLC) in France. Value in Health. 2020;23:S433–S433.
Sezer A, et al. Cemiplimab monotherapy for first-line treatment of advanced non-small-cell lung cancer with PD-L1 of at least 50%: a multicentre, open-label, global, phase 3, randomised, controlled trial. Lancet. 2021;397(10274):592–604.
Zhou C, et al. GEMSTONE-302: A phase III study of platinum-based chemotherapy (chemo) with placebo or CS1001, an antiPDL1 antibody, for first-line (1L) advanced non-small cell lung cancer (NSCLC). Ann Oncol. 2020;31:S1386–S1386.
Zhou C, et al. 96O Camrelizumab or placebo plus carboplatin and paclitaxel as first-line treatment for advanced squamous NSCLC (CameL-sq): A randomized, double-blind, multicenter, phase III trial. J Thorac Oncol. 2021;16:S748.
Galetta D, et al. Cisplatin/Pemetrexed Followed by Maintenance Pemetrexed Versus Carboplatin/Paclitaxel/Bevacizumab Followed by Maintenance Bevacizumab in Advanced Nonsquamous Lung Cancer: The GOIM (Gruppo Oncologico Italia Meridionale) ERACLE Phase III Randomized Trial. Clin Lung Cancer. 2015;16(4):262–73.
Huang JA, et al. Interim report on CIV recombinant human endostatin in combination with docetaxel/cisplatin (DP)) in comparison to DP in the first-line treatment of phase IIIb/IV squamous-cell NSCLC (JSLCG-001): A multicenter, open-label, randomized phase III controlled study (NCT: 02513342). J Clin Oncol. 2019;37:e20541–e20541.
Han L., Xing D. Clinical observation of Endostar combined with TP chemotherapy in the treatment of advanced stage NSCLC. Chin J Clin Oncol. 2009;36:1205–7.
Murakami H., et al.,Randomized phase II study of bevacizumab combined with CBDCA-PTX in Japanese patients with advanced non-sq NSCLC. Ann Oncol. 2010;21(Suppl 9):ix11–ix12; (Abstr PL-O3).
Wang J, et al. Results of randomized, multicenter, double-blind phase III trial of rh-endostatin (YH-16) in treatment of advanced non-small cell lung cancer patients. Zhongguo Fei Ai Za Zhi. 2005;8(4):283–90.
Han BH, et al. A multicenter, randomized, double-blind, placebo-controlled safety study to evaluate the clinical effects and quality of life of paclitaxel-carboplatin (PC) alone or combined with endostar for advanced non-small cell lung cancer (NSCLC). Zhonghua Zhong Liu Za Zhi. 2011;33(11):854–9.
Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. 2018;359(6382):1350–5.
Zhang B, et al. Predictive effect of PD-L1 expression for immune checkpoint inhibitor (PD-1/PD-L1 inhibitors) treatment for non-small cell lung cancer: A meta-analysis. Int Immunopharmacol. 2020;80: 106214.
Chen JH, et al. Indirect comparison of efficacy and safety between immune checkpoint inhibitors and antiangiogenic therapy in advanced non-small-cell lung cancer. Sci Rep. 2018;8(1):9686.
Socinski MA, et al. Current and Emergent Therapy Options for Advanced Squamous Cell Lung Cancer. J Thorac Oncol. 2018;13(2):165–83.
Hiraoka K, et al. Concurrent infiltration by CD8+ T cells and CD4+ T cells is a favourable prognostic factor in non-small-cell lung carcinoma. Br J Cancer. 2006;94(2):275–80.
Ruffini E, et al. Clinical significance of tumor-infiltrating lymphocytes in lung neoplasms. Ann Thorac Surg. 2009;87(2):365–71 discussion 371–2.
Yu H., Chen P., Xia L., et al. PD-1/PD-L1 inhibitor plus chemotherapy versus bevacizumab plus chemotherapy in first-line treatment for non-squamousnon-small-cell lung cancer. J ImmunoTher Cancer. 2021;9:e003431. https://doi.org/10.1136/jitc-2021-003431.
Acknowledgements
This work was financially supported by the Chinese National Natural Science Foundation Project (81772476).
Funding
This work was financially supported by the Chinese National Natural Science Foundation Project (81772476). The funding body has no role in the design of the study and collection, analysis, and interpretation of data and in the writing of manuscript.
Author information
Authors and Affiliations
Contributions
W.F.F. contributed to the conception. L.L.P. performed the design of the work. L.L.P. and J.D.G. performed the data acquisition and formal analysis. W.F.F. contributed to funding acquisition. L.L.P. and J.D.G. performed the interpretation of data and visualization. W.T.Z. and W-A-S.A helped in the revision process. All authors contributed to the original draft, and review and editing. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 3: Supplementary Figure 1.
Risk of bias assessment. A Risk of bias graph. B Risk of bias summary.
Additional file 4: Supplementary Figure 2.
Progression-free survival and overall survival comparison profile for advanced NSCLC under subgroup analysis stratified by histology, sex, age, smoking status, ECOG status, and brain metastasis or not.
Additional file 5: Supplementary Table 1.
Bayesian ranking results of network meta-analysis for progression-free survival, overall survival, objective response rate, and decrement rate of grade 3-4 assessment. Supplementary Table 2. Comparisons of the fit of consistency and inconsistency models.
Additional file 6: Supplementary Figure 3.
Bayesian ranking profile based on the SUCRA results of disease-controlled rate (DCR), decrement rate of any grade toxicity assessment, and rate of side effects leading to discontinuation and death.
Additional file 7: Supplementary Figure 4.
Bayesian ranking profile based on the SUCRA results of decrement rate of toxicity assessment on seven commonly reported adverse events, including hematological (anemia, neutropenia, and thrombocytopenia) and non-hematological (nausea/vomiting, fatigue, diarrhea, and asthenia) adverse events.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pang, LL., Gan, JD., Huang, YH. et al. Role of antiangiogenic agents in first-line treatment for advanced NSCLC in the era of immunotherapy. BMC Cancer 23, 72 (2023). https://doi.org/10.1186/s12885-022-10446-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10446-1