Abstract
Background
Cisplatin-based concurrent chemoradiotherapy has been identified as the primary and standard treatment for locally advanced nasopharyngeal carcinoma (NPC). However, the side effects of cisplatin affect the compliance to therapy. Thus, the search for a platinum-based substitute for NPC has always been a research focus. However, there is a variability in the efficacy of different platinum-based chemotherapies in the treatment of NPC. We performed a meta-analysis to compare the efficacy and safety of cisplatin-based regimens and other platinum-based derivatives (carboplatin, nedaplatin, and lobaplatin) for locally advanced NPC.
Methods
PubMed, EMBASE, Cochrane Library, Web of Science, and ClinicalTrials.gov were systematically searched for all potentially eligible clinical trials as of February 15, 2022. The pooled hazard ratios, risk ratio, and 95% confidence interval were calculated using Review Manager Software version 5.4.
Results
A total of 1,907 patients with locally advanced NPC were eligible from the 1,265 retrieved records. This systematic review included eight articles, six of which were randomized controlled clinical trials. There was no significant difference in the 3- and 5-year overall survival, progression-free survival, distant metastasis-free survival, and locoregional relapse-free survival between cisplatin-based chemotherapy and other platinum-based chemotherapy. Severe acute hematological side effects (≥ grade 3) during treatment, such as neutropenia, leukopenia, and thrombocytopenia, were equivalent in both groups. However, the incidence of anemia was higher in patients receiving other platinum-based chemotherapies. The risk of nausea, vomiting and weight loss was higher in the cisplatin group; however, there was no significant difference in the other non-hematological and late side effects between the two groups.
Conclusions
Other types of platinum-based chemotherapies are as effective as cisplatin-based chemotherapy in the treatment of locally advanced NPC, thus acting as potential alternatives to cisplatin. Further studies providing high-level evidence are needed.
Similar content being viewed by others
Background
The global geographical distribution of nasopharyngeal carcinoma (NPC) is unbalanced, with > 70% of the new NPC cases being reported in China and Southeastern Asia. An age-standardized incidence rate between 3.0 and 10.2 per 100,000 people has been reported in China [1, 2]. More than 70% of newly diagnosed NPC cases are classified as locally advanced disease in stages II–IVB [3]. Cisplatin-based concurrent chemoradiotherapy (CCRT) has been identified as the primary and standard treatment for locally advanced NPC. Although cisplatin offers substantial survival benefits to patients [3,4,5], its limitations lie in the poor adherence to treatment and side effects such as nausea, vomiting, nephrotoxicity, ototoxicity, and neurotoxicity [6, 7]. Therefore, there is an emerging need for other chemotherapeutic agents with similar efficacy against NPC and fewer side effects. Other platinum-based derivatives such as nedaplatin, lobaplatin and carboplatin have similar efficacy and fewer side effects, thus they have been used to replace cisplatin in the treatment of NPC [8,9,10]. However, no statistically significant results have been obtained from these studies. Thus, the aim of this meta-analysis of published clinical trials, retrospective studies, and paired analyses, was to compare the efficacy and safety of cisplatin-based and other platinum-based regimens in the treatment of locally advanced NPC.
Methods
Search strategy
We conducted a thorough search of the databases of medical publications: PubMed trial, EMBASE, Cochrane Library, Web of Science, and ClinicalTrials.gov, searching for all available records until February 15, 2022. The search was conducted by "subject word" or "title or key word." The search terms included: “Nasopharyngeal carcinoma,” “Carcinoma, Nasopharyngeal,” “Carcinomas, Nasopharyngeal,” “Nasopharyngeal Carcinomas,” “Cisplatin,” “lobaplatin,” “Nedaplatin,” “carboplatin,” and “randomized controlled trial or Randomized or placebo or RCT.” We manually searched the references of relevant articles to retrieve more clinical studies. In addition, a search was conducted before the final analysis. Two researchers (ZL and CL) independently screened the literature from the above databases and selected articles that met the inclusion criteria by reading the title or abstracts. If published data overlapped, only the most current information was included. In addition, a third researcher (DY) intervened to resolve any dispute(s).
Inclusion criteria
All the studies included in this meta-analysis followed the PICOS principles (Participants, Intervention, Comparison and Outcomes, Study design). The details are as follows: (1) P: patients with stage II–IVB locally advanced NPC diagnosed by pathology; (2) I: Patients in the experimental group received chemotherapy with other platinum derivatives (carboplatin, nedaplatin, and lobaplatin), while the control groups received cisplatin chemotherapy. The specific combination of chemotherapy and radiotherapy techniques were ignored in both groups; (3) C: analysis of therapeutic efficacy and toxicity during and after radiotherapy and chemotherapy; (4) O: major positive outcomes include overall survival (OS), progression-free survival (PFS), distant metastasis-free survival (DMFS), locoregional relapse-free survival (LRFS), while negative outcomes include hematologic and non-hematologic toxicities; (5) S: we not only included randomized controlled trials, but also observational studies (including cohort and case–control studies).
Exclusion criteria
Studies with any of the following characteristics were excluded: (1) studies on recurrent and metastatic nasopharyngeal carcinoma, (2) studies including patients with prior treatment with immunosuppressants or antiangiogenic drugs, (3) studies lacking detailed information or conference summaries, (4) unpublished studies, (5) single-arm clinical trials.
Data extraction and quality assessment
The following details were extracted from each eligible clinical trial: first author, publication year, inclusion period, registration number, study design, number of patients, tumor stage, mean age, median follow-up period, therapeutic regimens, OS, PFS, DMFS, LRFS, and adverse events.
Two assessment scales were used to assess the methodological quality of each eligible trial. The Cochrane risk bias assessment tool [11] was used to evaluate the quality of included randomized controlled clinical trials (RCTs). The quality evaluation included six aspects: random sequence generation, assignment hiding, blind method implementation, data integrity, reporting bias and other bias. There were three options for each: “low risk,” “high risk,” or “unclear.” The quality of the two retrospective studies was evaluated using the Newcastle–ottawa Scale (NOS) [12], including study population selection, intergroup comparability, and outcome measurements. It was graded by the semi-quantitative principle of the star system, the full score is 9, and ≥ 6 is classified as high-quality literature. The final NOS scale defined two retrospective studies as high-quality studies. The two researchers (ZL and CL) independently conducted and cross-checked the above-mentioned literature quality during the evaluation process. In case of any disagreement, the third researcher (DY) was consulted.
Statistical analysis
Summary statistics were compiled using the Review Manager Software, version 5.4 (Cochrane Collaboration RevMan, version 5.4, Oxford, UK). Survival outcomes (OS, PFS, DMFS, and LRFS) were assessed by hazard ratios (HRs) and 95% confidence intervals (CIs). If the HR was not directly described in the paper, Engauge Digitalizer version 4.1 software was used to extract data from the Kaplan–Meier survival curves according to the method of Tierney et al. [13], then the natural logarithm of HR (InHR) and standard error could be calculated. The relative risk (RR) was used to quantify and analyze efficacy. The inverse variance (IV) method was used to evaluate HR, and the Mantel Haenszel method was used to evaluate RR. The Χ2 test and I2 statistical and quantitative heterogeneity tests were used in each study, where p < 0.10 or I 2> 50% indicated that there was heterogeneity in each study and the random effect model was used for analysis. However, p > 0.10 or I2 < 50% indicated no statistical heterogeneity (H) and the fixed effect model was used for analysis. Sensitivity analysis excluded any element from the study and observed its impact on the combined statistics and the heterogeneity of test results.
Results
Study selection
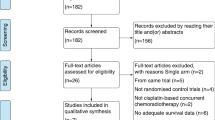
A total of 1,265 articles were retrieved from the PubMed, EMBASE, Cochrane Library and Web of Science databases. Two hundred and fifty-two duplicate records were deleted. After screening the title and abstract, there were 19 qualified articles left. After reading the full texts, eight studies [14,15,16,17,18,19,20,21,22] were finally included in the meta-analysis. The specific process of research screening is shown in Fig. 1.
Eligible studies and characteristics
The eight studies included in this review included a total of 1,907 patients. Six of the eight studies were RCTs, while the other two were retrospective studies. Through the Cochrane bias risk analysis tool, four RCTs [14,15,16,17,18] were noted as having used a random number method and the other two RCTs [21, 22] did not indicate specific random methods. All RCTs included in this study did not explain hidden groups and there was no indication that blinding was applied to patients and doctors. However, most of the outcome indicators for those RCTs were based on clinical data, and the blinding method has a relatively little impact on the clinical data. All the literature data were complete, where no missing information or incomplete data affected the analysis of the results, and no selective reports or other sources of bias were found in the studies. The details about the risk bias are shown in Fig. 2. The NOS scale defined two retrospective studies as high-quality studies. Table 1 shows the basic characteristics of the eligible clinical trials, while Table 2 shows the details and outcome measures of the treatment regimens.
OS
The 3-year OS data were obtained from three studies with a total of 655 patients (cisplatin group, 328 patients; and other platinum-based chemotherapies group, 327 patients). Forest plots showed that there was no significant difference in the 3-year OS between the two groups (HR, 0.88; 95% CI, [0.70–1.09]; p = 0.24; H: I2 = 0%, p = 0.41). The 5-year OS data were obtained from three studies with a total of 1,090 patients (cisplatin group, 534 patients; and other platinum-based chemotherapies group, 556 patients). There was no significant difference in the 5-year OS between the two groups (HR, 0.97; 95% CI, [0.70–1.35]; p = 0.87; H: I2 = 0%; p = 0.76; Fig. 3).
PFS
The 3-year PFS data were obtained from 449 patients in two studies (cisplatin group, 223 patients; and other platinum-based chemotherapies group: 226 patients). There was no significant difference in the 3-year PFS between the two groups (HR, 1.12; 95% CI, [0.77–1.65]; p = 0.55; H: I2 = 0%; p = 0.91). The 5-year PFS data were obtained from three studies with a total of 1,090 patients (cisplatin group, 534 patients; and other platinum-based chemotherapies group, 556 patients). There was no significant difference in the 5-year PFS between the two groups (HR, 0.99; 95% CI, [0.78–1.27]; p = 0.94; H: I2 = 0%; p = 0.64) (Fig. 4).
DMFS
The 3-year DMFS data were obtained from a total of 655 patients in three studies (cisplatin group, 328 patients; and other platinum-based chemotherapies group, 327 patients). There was no significant difference in the 3-year DMFS between the two groups (HR, 0.95; 95% CI, [0.65–1.38]; p = 0.79; H: I2 = 56%; p = 0.11). The 5-year DMFS data were obtained from 1,090 patients in three studies (cisplatin group, 534 patients; and other platinum-based chemotherapies group, 556 patients). There was no significant difference in the 5-year DMFS between the two groups (HR, 0.78; 95% CI, [0.57–1.07]; p = 0.12; H: I2 = 0%; p = 0.96) (Fig. 5).
LRFS
The 3-year LRFS data were obtained from a total of 449 patients in two studies (cisplatin group, 223 patients; and other platinum-based chemotherapies group, 226 patients). There was no significant difference in the 3-year LRFS between the two groups (HR, 1.02; 95% CI, [0.97–1.07]; p = 0.47; H: I2 = 0%; p = 0.51). The 5-year LRFS data were obtained from three studies with a total of 1,090 patients (cisplatin group, 534 patients; and other platinum-based chemotherapies group, 556 patients). There was no significant difference in the 5-year LRFS between the two groups (HR, 1.13; 95% CI, [0.78–1.63]; p = 0.51; H: I2 = 26%; p = 0.26) (Fig. 6).
Grade ≥ 3 acute toxicities
Based on acute grade 3 or higher acute toxicities during treatment in the other platinum-based chemotherapies and cisplatin groups, the following risks were calculated. With regard to hematological toxicities, there was no significant difference in the risk of neutropenia (RR, 1.21; 95% CI, [0.94–1.57]; p = 0.14), leukopenia (RR, 0.97; 95% CI, [0.81–1.17]; p = 0.78), or thrombocytopenia (RR, 1.62; 95% CI, [0.98–2.69]; p = 0.06) between the other platinum-based chemotherapies group and the cisplatin group. However, the risk of anemia in the other platinum-based chemotherapies group was significantly higher than that of the cisplatin group (RR, 0.30; 95% CI, [0.12–0.77]; p = 0.01).
With regard to non-hematological toxicities, there was no significant difference in the risk of xerostomia (RR, 0.83; 95% CI, [0.51–1.35]; p = 0.46), dermatitis (RR, 1.02; 95% CI, [0.58–1.81]; p = 0.95), mucositis (RR, 1.02; 95% CI, [0.58–1.81]; p = 0.95), or elevated levels of aminotransferase (RR, 0.71; 95% CI, [0.25–2.05], p = 0.53) between the other platinum-based chemotherapies group and the cisplatin group. However, the risk of nausea (RR, 0.12; 95% CI, [0.06–0.25]; p < 0.0001), vomiting (RR, 0.15; 95% CI, [0.06–0.40]; p = 0.0001), and weight loss (RR, 0.34; 95% CI, [0.12–0.98], p = 0.04) were significantly lower in the other platinum-based chemotherapies group than those in the cisplatin group (Table 3).
Treatment-related late toxicities
Based on the late adverse events during the treatment with other platinum derivatives and cisplatin, there was no significant difference between the two groups regarding the risk of xerostomia (RR, 0.96; 95% CI, [0.88–1.05]; p = 0.40), subcutaneous fibrosis (RR, 0.95; 95% CI, [0.83–1.08]; p = 0.42), hearing impairment (RR, 0.91; 95% CI, [0.64–1.31]; p = 0.62), trismus (RR, 0.70; 95% CI, [0.45–1.07]; p = 0.10), cranial nerve palsy (RR, 0.83; 95% CI, [0.57–1.20], p = 0.32), or temporal lobe necrosis (RR, 0.80; 95% CI, [0.51–1.25]; p = 0.32) (Fig. 7).
Subgroup and sensitivity analyses
Two studies reported the efficacy and side effects of induction chemotherapy alone [18, 21], so these two outcomes were analyzed separately. After induction chemotherapy, there was no significant difference in complete response (RR, 1.24; 95% CI, [0.88–1.75.08]; p = 0.21) or partial response (RR, 1.25; 95% CI, [0.97–1.62]; p = 0.09) between the other platinum-based chemotherapies group and the cisplatin group. There was also no significant difference in the risk of leukocytopenia (RR, 1.06; 95% CI, [0.53–2.12]; p = 0.86) or thrombocytopenia (RR, 0.67; 95% CI, [0.22–2.09]; p = 0.49) between the two groups. However, the risk of anemia (RR, 0.47; 95% CI, [0.28–0.80]; p = 0.005) was significantly higher in the other platinum-based chemotherapies group than that of the cisplatin group. Moreover, the incidence of vomiting (RR, 0.24; 95% CI, [0.12–0.49]; p < 0.0001) in the cisplatin group was significantly higher than that of the other platinum-based chemotherapies group. The sensitivity analysis showed that the aggregated results at all endpoints remained unchanged when any study was deleted, indicating that the results of this meta-analysis are reliable (Fig. 8).
Discussion
The study showed that the other platinum-based chemotherapy alternatives did not reduce survival and did not significantly increase the incidence of hematological and non-hematological side effects compared with cisplatin-based chemotherapy. To the best of our knowledge, this is the first meta-analysis to examine the efficacy and side effects of cisplatin versus other platinum-based chemotherapies in locally advanced NPC.
In the past 20 years, three major advances have significantly improved the prognosis of patients with NPC. First, intensity-modulated radiation therapy can cover the target area and the local expansion area with good precision. Intensity-modulated radiation therapy can better protect the adjacent normal tissue, especially for patients whose tumors extend backward to the cranial nerve [23, 24]. Second, the combination of cisplatin-based CCRT, induction chemotherapy, or adjuvant chemotherapy effectively improves the survival rate and disease control of NPC [3, 5, 25,26,27]. Third, the use of advanced imaging techniques, especially the application of MRI and PET-CT, can better evaluate the local and distant invasion of the tumor, which is very critical for the accurate application of intensity-modulated radiation therapy. However, cisplatin-based chemotherapy regimens are known to increase the acute and late toxicities of radiotherapy [16]. Long-term side effects such as nausea, vomiting, auditory function, renal function, or effects on peripheral nerves caused by cisplatin may affect the quality of life of survivors. Moreover, cisplatin-based CCRT requires pretreatment and post-treatment hydration during cisplatin administration to protect the kidneys, which can prolong the hospital stay [14, 16, 17].
Carboplatin, nedaplatin, and lobaplatin were successively included in the study as cisplatin substitutes to improve the compliance of patients, reduce the side effects of chemotherapy and meet the clinical needs. A randomized non-inferiority trial showed that there was no difference between carboplatin-based CCRT and a cisplatin-based regimen in patients with locally advanced NPC. Moreover, carboplatin showed better tolerance in patients with locally advanced NPC [22]. Two other trials indicated that carboplatin induction chemotherapy combined with CCRT did not improve survival in patients with locally advanced NPC compared with carboplatin induction chemotherapy combined with radiotherapy alone [9]. In addition, carboplatin was less effective than cisplatin when given during CCRT in patients with borderline renal function [28].
Nedaplatin, a cisplatin analog, has antitumor mechanism and therapeutic effects similar to that of cisplatin and does not require hydration to protect the kidneys. Two Phase 2 studies have shown that nedaplatin in combination with fluorouracil or docetaxel has an inductive effect on chemotherapy. In addition, nedaplatin-based CCRT is an effective and safe treatment for patients with stage II–IVB NPC, indicating that nedaplatin may be a promising alternative to cisplatin [15, 29]. In a randomized phase III trial, Mai et al. [16] showed that for patients with stages II–IVB NPC, nedaplatin-based CCRT was not inferior to cisplatin-based CCRT with respect to the 2-year PFS. Subsequent comments [30] indicate that it is too early to conclude that nedaplatin will replace cisplatin. However, the newly published results of the 5-year follow-up still support the results of the initial report [17].
Lobaplatin is a third-generation platinum drug. In previous studies, lobaplatin was found to overcome some forms of multiple drug resistance caused by other platinum-based drugs, such as cisplatin or carboplatin [8]. A random non-inferiority trial showed that lobaplatin-based induction chemotherapy plus CCRT has similar survival outcomes and side effect profiles as cisplatin-based therapy and thus may act as a promising alternative [14]. Clinical studies, such as ChiCTR1900021536 and ChiCTR-IIR-17013112, are ongoing and aim to further assess the benefits and risks of lobaplatin for NPC and verify the value of these treatment strategies.
Cisplatin has a lower drug price than platinum derivatives; however, it also has more symptomatic adverse events that require additional treatment processes, such as hydration and antiemetic preconditioning, and this increases the cost of treatment accordingly [31]. Liao et al. [10] found that nedaplatin is an advantageous and low-cost alternative to concurrent chemoradiotherapy for stage II–IVB NPC, based on a cost–benefit curve analysis. Lv et al. [14] mentioned that in south China, an area with high incidence of NPC, although the price of a new generation of platinum derivatives is higher than that of cisplatin, various chemotherapy drugs (such as lobaplatin) are included in the list of essential drugs under China's medical insurance system, and the supply of generic drugs reduces the cost [32]. However, the limited number of inpatient beds and the length of stay pose challenges. Patients waiting for hospital treatment may experience disease progression and have increased psychological stress. Shorter hospital stays with cisplatin derivatives may help alleviate these problems.
We conducted this meta-analysis to evaluate the efficacy and safety of other platinum-based chemotherapies versus cisplatin-based chemotherapy for locally advanced NPC. Choi et al. [33] performed a network meta-analysis on the efficacy of different neoadjuvant chemotherapeutic strategies in the treatment of NPC. The results showed that some cisplatin-based neoadjuvant chemotherapy regimens improved the prognosis of patients with NPC and reduced the toxicity of chemotherapy. However, the optimal neoadjuvant chemotherapy protocol is not fully consistent in terms of survival and efficiency. Yuan et al. [34] showed that the induction chemotherapy regimen, gemcitabine plus cisplatin, shows better performance in terms of survival outcomes. To date, there is no meta-analysis to adequately demonstrate differences in the efficacy of various platinum-based regimens in locally advanced NPC. To reduce bias, we selected RCTs that are clinically registered as eligible studies. Our meta-analysis revealed that there was no significant difference between other platinum-based and cisplatin-based chemotherapy in terms of OS, PFS, DMFS, and LRFS. Severe acute hematological side effects (≥ grade 3) such as neutropenia, leukopenia and thrombocytopenia were observed after platinum-based induction chemotherapy or throughout the treatment period; however, such side effects were equivalent to those in the cisplatin treatment group. It is worth noting that the risk of anemia was higher in patients receiving other platinum-based treatments. In contrast, the risk of non-hematological side effects such as nausea, vomiting, and weight loss after induction chemotherapy or during the whole treatment period was higher in the cisplatin treatment group. There was no difference in other non-hematological side effects, such as xerostomia, dermatitis, mucositis, and elevated levels of aminotransferase, between the two groups. Moreover, there was no significant difference in the late side effects such as xerostomia, subcutaneous fibrosis, hearing impairment, trismus, cranial nerve palsy and temporal lobe necrosis between the two groups. The studies included in this meta-analysis did not report any treatment-related disability or death.
The main limitation of this meta-analysis is that some of the studies included were not RCTs, which may affect our research outcomes. Moreover, most studies were conducted in China, which may be a source of potential bias. In addition, there are differences in the specific study populations, combined treatment schemes and treatment durations, which may affect further data analyses. Finally, the DNA level of EB virus is a prognostic factor for NPC, however, the included studies could not be analyzed by subgroups to address this factor.
Conclusion
Based on the systematic review and meta-analysis of the included studies, other platinum-based chemotherapy regimens were not inferior to cisplatin-based regimens and could be effective alternatives to cisplatin for the treatment of locally advanced NPC. Since most eligible studies were conducted in endemic areas, high-level evidence is needed to verify these findings in the future.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- NPC:
-
Nasopharyngeal carcinoma
- RCT:
-
Randomized controlled trials
- IC:
-
Induction chemotherapy
- CCRT:
-
Concurrent chemoradiotherapy
- AC:
-
Adjuvant chemotherapy
- Con:
-
Control group (cisplatin-based group)
- Exp:
-
Experimental group (other platinum-based group)
- NA:
-
Not available
- Re:
-
Retrospetive study
- NR:
-
Not reported
- FE:
-
Fail to extract
- 5FU:
-
5-Fluorouracil
- OS:
-
Overall survival
- PFS:
-
Progressive-free survival
- DMFS:
-
Distant metastasis-free survival
- LRFS:
-
Locoregional relapse-free survival
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Chen YP, Chan A, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64–80.
Sun Y, Li WF, Chen NY, Zhang N, Hu GQ, Xie FY, Sun Y, Chen XZ, Li JG, Zhu XD, et al. Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol. 2016;17(11):1509–20.
Zhang L, Huang Y, Hong S, Yang Y, Yu G, Jia J, Peng P, Wu X, Lin Q, Xi X, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase 3 trial. Lancet. 2016;388(10054):1883–92.
Chen L, Hu CS, Chen XZ, Hu GQ, Cheng ZB, Sun Y, Li WX, Chen YY, Xie FY, Liang SB, et al. Concurrent chemoradiotherapy plus adjuvant chemotherapy versus concurrent chemoradiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2012;13(2):163–71.
Rybak LP, Mukherjea D, Jajoo S, Ramkumar V. Cisplatin ototoxicity and protection: clinical and experimental studies. Tohoku J Exp Med. 2009;219(3):177–86.
Fung C, Dinh PJ, Ardeshir-Rouhani-Fard S, Schaffer K, Fossa SD, Travis LB. Toxicities Associated with Cisplatin-Based Chemotherapy and Radiotherapy in Long-Term Testicular Cancer Survivors. Adv Urol. 2018;2018:8671832.
McKeage MJ. Lobaplatin: a new antitumour platinum drug. Expert Opin Investig Drugs. 2001;10(1):119–28.
Huang PY, Cao KJ, Guo X, Mo HY, Guo L, Xiang YQ, Deng MQ, Qiu F, Cao SM, Guo Y, et al. A randomized trial of induction chemotherapy plus concurrent chemoradiotherapy versus induction chemotherapy plus radiotherapy for locoregionally advanced nasopharyngeal carcinoma. Oral Oncol. 2012;48(10):1038–44.
Liao W, Huang J, Wu Q, Zhu G, Wang X, Wen F, Zhang P, Zhang N, Li Q. Concurrent chemoradiotherapy with nedaplatin versus cisplatin in stage II-IVB nasopharyngeal carcinoma: A cost-effectiveness analysis. Oral Oncol. 2019;93:15–20.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Lv X, Cao X, Xia WX, Liu KY, Qiang MY, Guo L, Qian CN, Cao KJ, Mo HY, Li XM, et al. Induction chemotherapy with lobaplatin and fluorouracil versus cisplatin and fluorouracil followed by chemoradiotherapy in patients with stage III-IVB nasopharyngeal carcinoma: an open-label, non-inferiority, randomised, controlled, phase 3 trial. Lancet Oncol. 2021;22(5):716–26.
Tang C, Wu F, Wang R, Lu H, Li G, Liu M, Zhu H, Zhu J, Zhang Y, Hu K. Comparison between nedaplatin and cisplatin plus docetaxel combined with intensity-modulated radiotherapy for locoregionally advanced nasopharyngeal carcinoma: a multicenter randomized phase II clinical trial. Am J Cancer Res. 2016;6(9):2064–75.
Tang LQ, Chen DP, Guo L, Mo HY, Huang Y, Guo SS, Qi B, Tang QN, Wang P, Li XY, et al. Concurrent chemoradiotherapy with nedaplatin versus cisplatin in stage II-IVB nasopharyngeal carcinoma: an open-label, non-inferiority, randomised phase 3 trial. Lancet Oncol. 2018;19(4):461–73.
Tang QN, Liu LT, Qi B, Guo SS, Luo DH, Sun R, Sun XS, Chen DP, Guo L, Mo HY, et al. Effect of Concurrent Chemoradiotherapy With Nedaplatin vs Cisplatin on the Long-term Outcomes of Survival and Toxic Effects Among Patients With Stage II to IVB Nasopharyngeal Carcinoma: A 5-Year Follow-up Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open. 2021;4(12):e2138470.
Hu Y, Fu JT, Shi D, Feng B, Shi Z. Clinical efficacy and safety of gemcitabine plus nedaplatin in the treatment of advanced nasopharyngeal carcinoma. J Cancer Res Ther. 2016;12(Supplement):C252–5.
Liu T, Sun Q, Chen J, Li B, Qin W, Wang F, Ye Z, Hu F. Neoadjuvant Chemotherapy with Fluorouracil plus Nedaplatin or Cisplatin for Locally Advanced Nasopharyngeal Carcinoma: a Retrospective Study. J Cancer. 2018;9(20):3676–82.
Zhan Z, Tao H, Qiu W, Liu Z, Zhang R, Liao K, Li G, Yuan Y, Yuan T, Zheng R. Clinical value of nedaplatin-based chemotherapy combined with radiotherapy for locoregional advanced nasopharyngeal carcinoma: a retrospective, propensity score-matched analysis. J Cancer. 2020;11(23):6782–9.
Cao K, Zhang A, Ma W, Huang P, Luo D, Xia W. Nedaplatin or cisplatin combined with 5-fluorouracil for treatment of stage III-IVa nasopharyngeal carcinoma: a randomized controlled study. Chin J Oncol. 2011;33(1):50–2.
Chitapanarux I, Lorvidhaya V, Kamnerdsupaphon P, Sumitsawan Y, Tharavichitkul E, Sukthomya V, Ford J. Chemoradiation comparing cisplatin versus carboplatin in locally advanced nasopharyngeal cancer: randomised, non-inferiority, open trial. Eur J Cancer. 2007;43(9):1399–406.
Kam MK, Leung SF, Zee B, Chau RM, Suen JJ, Mo F, Lai M, Ho R, Cheung KY, Yu BK, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol. 2007;25(31):4873–9.
Zhang MX, Li J, Shen GP, Zou X, Xu JJ, Jiang R, You R, Hua YJ, Sun Y, Ma J, et al. Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: A 10-year experience with a large cohort and long follow-up. Eur J Cancer. 2015;51(17):2587–95.
Blanchard P, Lee A, Marguet S, Leclercq J, Ng WT, Ma J, Chan AT, Huang PY, Benhamou E, Zhu G, et al. Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC meta-analysis. Lancet Oncol. 2015;16(6):645–55.
Ribassin-Majed L, Marguet S, Lee A, Ng WT, Ma J, Chan A, Huang PY, Zhu G, Chua D, Chen Y, et al. What Is the Best Treatment of Locally Advanced Nasopharyngeal Carcinoma? An Individual Patient Data Network Meta-Analysis. J Clin Oncol. 2017;35(5):498–505.
Frikha M, Auperin A, Tao Y, Elloumi F, Toumi N, Blanchard P, Lang P, Sun S, Racadot S, Thariat J, et al. A randomized trial of induction docetaxel-cisplatin-5FU followed by concomitant cisplatin-RT versus concomitant cisplatin-RT in nasopharyngeal carcinoma (GORTEC 2006–02). ANN ONCOL. 2018;29(3):731–6.
Yau TK, Lee AW, Wong DH, Pang ES, Ng WT, Yeung RM, Soong IS. Treatment of Stage IV(A-B) nasopharyngeal carcinoma by induction-concurrent chemoradiotherapy and accelerated fractionation: impact of chemotherapy schemes. Int J Radiat Oncol Biol Phys. 2006;66(4):1004–10.
Zheng J, Wang G, Yang GY, Wang D, Luo X, Chen C, Zhang Z, Li Q, Xu W, Li Z, et al. Induction chemotherapy with nedaplatin with 5-FU followed by intensity-modulated radiotherapy concurrent with chemotherapy for locoregionally advanced nasopharyngeal carcinoma. Jpn J Clin Oncol. 2010;40(5):425–31.
Blanchard P, Tao Y. Nedaplatin in nasopharyngeal cancer: the rebirth of platinum salts? Lancet Oncol. 2018;19(4):429–31.
Blower PR. The role of specific 5-HT3 receptor antagonism in the control of cytostatic drug-induced emesis. Eur J Cancer. 1990;26(Suppl 1):S8–11.
National Healthcare Security Administration. http://www.nhsa.gov.cn (Accessed 25 Nov 2020).
Choi HC, Chan SK, Lam KO, Chan SY, Chau SC, Kwong DL, Leung TW, Luk MY, Lee AW, Lee VH. The Most Efficacious Induction Chemotherapy Regimen for Locoregionally Advanced Nasopharyngeal Carcinoma: A Network Meta-Analysis. Front Oncol. 2021;11:626145.
Yuan C, Xu XH, Luo SW, Wang L, Sun M, Ni LH, Xu L, Wang XL, Zeng G. Which neoadjuvant chemotherapy regimen should be recommended for patients with advanced nasopharyngeal carcinoma?: A network meta-analysis. Medicine (Baltimore). 2018;97(34):e11978.
Acknowledgements
We thank the members in the Min Kang’s workgroup for helping to improve the grammar and spelling.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 71964003, 71964003, 81760542, 82160467), the Natural Science Foundation of Guangxi Zhuang Autonomous Region (No.2018JJA141048), the Research Foundation of the Science and Technology Department of Guangxi Province, China (grant No.2016GXNSFAA380252, 2018AB61001 and 2019GXNSFAA185040), the Research Foundation of the Health Department of Guangxi Province, China (No.S2018087), Guangxi Medical University Training Program for Distinguished Young Scholars (2017), Medical Excellence Award Funded by the Creative Research Development Grant from the First Affiliated Hospital of Guangxi Medical University (2016).Guangxi Medical High-level Talents Training Program.
Author information
Authors and Affiliations
Contributions
ZL and CL wrote the manuscript. DY, JS and TL performed the data search and data analysis. ZZ and LZ prepared figures. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Z., Li, C., Yang, D. et al. Comparing the efficacy and safety of cisplatin and other platinum-based chemotherapies in locally advanced nasopharyngeal carcinoma: a systematic review and meta-analysis. BMC Cancer 22, 616 (2022). https://doi.org/10.1186/s12885-022-09712-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09712-z