Abstract
Background
For patients with locally advanced nasopharyngeal cancer (LA-NPC), concurrent chemoradiotherapy (CCRT) is the standardized treatment. However, whether a weekly or triweekly cisplatin regimen should be used during CCRT is controversial. Therefore, we conducted this meta-analysis to explore differences in the effects and toxicities of the two regimens.
Methods
We searched PubMed, Embase, and the Cochrane Library (until June 10, 2022). We evaluated overall survival (OS), distant metastasis-free survival (DMFS), locoregional recurrence–free survival (LRFS), disease-free survival (DFS) and grade ≥ 3 adverse events. The effect indices were hazard ratios (HRs) and odds ratios (ORs), and Review Manager software 5.4 (RevMan 5.4) was used for computations.
Results
We identified 7 studies in our analysis. There was no significant difference in OS (HR = 1.00, 95% CI 0.73–1.38, P = 0.99), DMFS (HR = 0.84, 95% CI 0.58–1.22, P = 0.36), LRFS (HR = 0.91, 95% CI 0.63–1.32, P = 0.62) or DFS (HR = 0.93, 95% CI 0.56–1.56; P = 0.78) between the weekly and triweekly cisplatin regimens. We found that the weekly cisplatin regimen was more likely to cause grade ≥ 3 hematological toxicity events than the triweekly cisplatin regimen. In addition, subgroup analyses revealed that patients undergoing CCRT and CCRT plus adjuvant chemotherapy (AC) had similar OS or DFS.
Conclusion
Weekly and triweekly cisplatin regimens had similar efficacy for LA-NPC. The triweekly regimen may replace the weekly regimen for LA-NPC because of lower toxicity. Larger data accumulation and more multicenter clinical trials may be needed to verify these results.
Similar content being viewed by others
Introduction
Nasopharyngeal cancer (NPC) is the most common primary neoplasm of the nasopharynx and is mainly found in Asia, especially in southern China. There are approximately 13,000 new cases of the disease diagnosed worldwide each year [1]. In addition, many patients are already in a locally advanced state at the time the disease is initially diagnosed. Locally advanced nasopharyngeal cancer (LA-NPC), to some extent, has a greater risk of locoregional relapse and distant metastases [2, 3]. Because it is sensitive to radiotherapy and chemotherapy, CCRT is the cornerstone of systemic treatment for patients with NPC. Good local control can be achieved in patients with LA-NPC who receive this therapy [4, 5]. Cisplatin-based therapies administered either once per week or once every three weeks are standard strategies for CCRT [6].
However, the two cisplatin regimens are more superior than other regimens. To date, the optimal schedule for cisplatin during CCRT is still controversial. Hence, the purpose of the meta-analysis was to compare survival outcomes and toxicities of the two different cisplatinum regimens for locally advanced NPC patients.
Methods
Literature search
We thoroughly searched PubMed, Embase, and the Cochrane library (each from inception to June 10, 2022) for literature studies. There was no language restrictions to identify studies. The search terms were constructed as described below: ‘nasopharyngeal neoplasm/carcinoma/cancer/tumor’, ‘nasopharynx neoplasms/carcinoma/cancer/tumor’, ‘concurrent chemoradiotherapy’, ‘chemoradiotherapy’, ‘cisplatinum’, and ‘cisplatin’. The above search terms were combined by using “AND” and “OR”. Qualified articles from the three medical databanks were searched independently by two team members. If there was any dispute, it was settled in a group discussion.
Inclusion criteria
The included studies were required to satisfy the principles of PICOS (Population, Intervention, Comparison, Outcomes and Study design). The details are as follows: (1) P: patients with a pathological diagnosis of nasopharyngeal cancer; (2) I: patients received only cisplatin chemotherapy during CCRT. The experimental group received a triweekly cisplatin treatment, and the control group received a weekly cisplatin treatment; (3) C: Survival outcomes and toxicities were compared between the weekly and triweekly cisplatin regimens; (4) O: Studies with at least one reported outcome as follows: OS, DMFS, LRFS, DFS, and grade ≥ 3 toxicity (including hematological toxicity and nonhematological toxicity); (5) S: The study design consisted of randomized control trials (RCTs) and non-RCTs.
Exclusion criteria
This meta-analysis had five exclusion criteria: (1) patients with distant metastases or severe coexisting illness; (2) Prior radiotherapy, chemotherapy, or clear primary neoplasms or lymph node surgical history; (3) lactation or pregnancy; (4) a significant difference in baseline data or no valuable information in the study; and (5) single arm studies, reviews, case reports, letters, comments or other unsuitable study types.
Data extraction
Qualified articles from the abovementioned databanks were searched by two reviewers to determine whether they met the inclusion and exclusion criteria. Two team members read the selected articles to be included in this meta-analysis, and they were responsible for extracting relevant information according to the items in a standardized manner. Items were inventoried as follows: (1) baseline characteristics, including the first author’s name, country, published year, research period, median follow-up time, number of cases, study type, Eastern Cooperative Oncology Group Performance Status Scale (ECOG/PS) or Karnofsky's index of performance status (KPS), neoplasms clinical stage, intervention, comparisons, and patients’ ages and sexes; and (2) outcomes, including OS, DMFS, LRFS, DFS and grade ≥ 3 adverse events. We excluded articles with missing data. Disagreements were resolved in a panel discussion.
Risk of bias and quality evaluation
Two researchers evaluated the risk of bias, and a third team member resolved differentials. The risk of bias in RCTs was evaluated by employing the Cochrane risk of bias tool, and the risk of bias in non-RCTs was evaluated by employing the Newcastle‒Ottawa Scale (NOS). The Cochrane risk of bias assessment tool has seven criteria, which are as follows: selection bias (including random sequence generation and allocation concealment), performance bias, detection bias, reporting bias, attrition bias and other bias. Three different levels (including high, low, or unclear risk bias) were used to evaluate each clause [7]. The NOS scale has the following three criteria: selection of experimental and control groups, comparability of experimental and control groups, and outcomes of research [8]. We gave a ‘star’ when we recognized the clause as ‘high ‘quality’. With the exception of the 'comparability' clause, which was allowed a maximum of two stars, the remaining clauses were allowed a maximum of one star. Study quality was classified as high level (7 ≤ stars ≤ 9), middle level (4 ≤ stars ≤ 6), and low level (1 ≤ stars ≤ 3).
Statistical analysis
We used Review Manager software 5.4 (RevMan 5.4) to conduct this meta-analysis. We chose HR as the effect index, and the inverse-variance (IV) method was used to pool survival statistics [9]. Engauge Digitizer software was employed to extract HR from the survival curve when it could not be extracted immediately from qualified articles. Dichotomous variables were calculated by the odds ratio (OR), and the Mantel‒Haenszel (MH) method was used to evaluate the OR. We used χ2 and the I2 test statistic to examine heterogeneity. If the P value of the χ2 test was > 0.05 and I2 < 50%, the fixed-effect model was adopted for data with nonsignificant heterogeneity. Conversely, the random-effect model was employed due to significant heterogeneity. Moreover, to demonstrate the effect of AC, a subgroup analysis was conducted based on concurrent chemoradiotherapy.
The meta-analysis protocol was prospectively registered at PROSPERO (CRD42022341140).
Results
Study selection
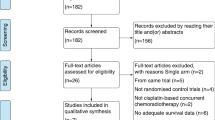
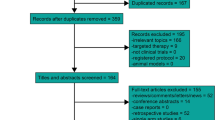
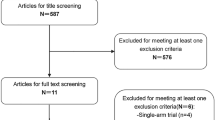
After we completed the relevant search, a total of 1801 articles were retrieved and records were excluded after removing duplicates or screening titles (n = 1784).Finally, 17 eligible articles remained. Ten articles were eliminated, and only 7 articles were included in this meta-analysis. The exclusion reasons were as follows: 2 articles were not available in full text, 6 articles were excluded after reviewing the abstract, 1 article was a single arm study, and 1 article did not satisfy the intervention. The entire process of study selection is displayed in Fig. 1.
Features of the included studies
Ultimately, 7 studies with a total of 2151 patients were included in this meta-analysis. Among the 7 eligible articles, two [1, 10] were randomized controlled trials and five [6, 11,12,13,14] were retrospective studies. We used the Cochrane risk of bias tool to evaluate the quality of the two randomized controlled trials. Details are displayed in Figs. 2. We used the NOS scale to estimate the quality of the 5 retrospective studies, which were recognized as high level because all of them had 7 stars. Moreover, the basic information of the qualified studies contained in this meta-analysis is stated in Tables 1 and 2.
Primary endpoint
Overall survival (OS)
In all the studies [1, 6, 10,11,12,13,14] in our meta-analysis, OS data were reported and 817 patients received the weekly cisplatin regimen, whereas 1334 patients received the triweekly cisplatin regimen. Specifically, the OS data obtained by Meng [6] and Wang [12] were extracted from the results of the multivariate analyses, whereas the OS data obtained by Gundog [13] were extracted from the results of the univariate analyses. OS was very similar in patients receiving weekly and triweekly cisplatin regimens (pooled HR = 1.00, 95% CI 0.73–1.38, P = 0.99, Fig. 3A). A fixed-effect model was used since the heterogeneity test showed no significant difference (I2 = 31%, P = 0.19).
Secondary endpoints
Distance metastasis-free survival (DMFS)
We could immediately extract the HRs of DMFS from 5 studies [1, 6, 11,12,13]. DMFS data obtained by Gundog [13] and Wang [12] were extracted from the results of the univariate analysis, and DMFS data obtained by Meng [6] were extracted from the results of the multivariate analysis. A fixed-effect model was used to compute pooled data due to no significant heterogeneity (I2 = 43%, P = 0.13). The results showed that the weekly and triweekly cisplatin groups had similar DMFS (pooled HR = 0.84, 95% CI 0.58–1.22, P = 0.36, Fig. 3B).
Local recurrence-free survival (LRFS)
LRFS data were reported in five articles [1, 6, 11,12,13], which contained a total of 1969 patients. It should be noted that LRFS data obtained by Gundog [13], Wang [12] and Meng [6] were from the results of the univariate and multivariate analyses, respectively. There was no significant difference between the two cisplatin regimens (pooled HR = 0.91, 95% CI 0.63–1.32, P = 0.62, Fig. 3C), with no heterogeneity (I2 = 35%, P = 0.18). Therefore, we employed a fixed-effect model.
Disease-free survival (DFS)
DFS data were reported in four studies [6, 11, 12, 14] with 1434 patients and used for our meta-analysis. Furthermore, the DFS data obtained by Meng [6] and Wang [12] were extracted from the results of the multivariate analyses. There was significant heterogeneity among these trials (I2 = 53%, P = 0.10); hence, a random-effect model was adopted to merge the data. The merged data revealed no statistically significant advantage for the weekly and triweekly cisplatin groups, with an HR of 0.93 (95% CI 0.56–1.56, P = 0.78, Fig. 3D).
Sensitivity and subgroup analysis
We performed a sensitivity analysis of this meta-analysis and found that all endpoints of the pooled results remained unchanged after removing each of the studies one by one. This suggests that the results of our meta-analysis are stable. In addition, we found two articles [10, 14] in which patients were treated with CCRT plus AC and other articles [1, 6, 11,12,13] in which patients were treated with only CCRT. Therefore, we designed a subgroup analysis. The results showed that OS and DFS were similar between the subgroups (details can be viewed in Table 3).
Treatment-related grade ≥ 3 adverse events
In 7 selected articles, researchers reported grade ≥ 3 adverse events, including hematologic toxic events (leukopenia, neutropenia, thrombocytopenia and anemia) and nonhematologic toxic events (nephrotoxicity/renal dysfunction, nausea/vomiting/constipation/diarrhea, skin reaction/dermatitis/rash, mucositis/stomatitis, xerostomia, and ototoxicity). Acute toxicity was evaluated according to the Common Terminology Criteria for Adverse Events (CTCAE). As shown in Table 4, the weekly cisplatin regimen was significantly associated with thrombocytopenia (pooled OR = 3.49, 95% CI 1.98–6.16, P < 0.0001), leukopenia (pooled OR = 1.50, 95% CI 1.16–1.93, P = 0.002) and neutropenia (pooled OR = 1.48, 95% CI 1.02–2.15, P = 0.04) compared to the triweekly cisplatin regimen. There was no statistically significant difference in the other adverse events between the two cisplatin groups.
Discussion
As described above, survival outcomes (including OS, DFS, DMFS, and LRFS) were similar between weekly cisplatin and triweekly cisplatin regimens during the CCRT period. However, it should be noted that the weekly cisplatin regimen had a higher incidence rate of grade ≥ 3 acute hematological toxic events, particularly in terms of thrombocytopenia and leukopenia. Subgroup analysis revealed no significant difference in OS or DFS between CCRT and CCRT plus AC. This suggests that patients with locally advanced nasopharyngeal cancer may not benefit from AC.
According to Chen’s research, CCRT could improve the overall survival (OS) and progression-free survival (PFS) of nasopharyngeal carcinoma patients compared with radiotherapy alone in the era of traditional 2D-RT [15]. The subsequent intergroup 0099 randomized trial confirmed that CCRT was better than radiotherapy alone for patients with locally advanced nasopharyngeal cancer (LA-NPC) [16]. Several meta-analyses have already shown that CCRT combined with or without AC could significantly improve OS [17,18,19,20]. Thus, CCRT has become the core therapy for patients with locally advanced nasopharyngeal cancer (LA-NPC). However, in the field of concurrent cisplatin dose delivery, either once a week or every 3 weeks, we found that the two regimens are popularly used in clinical practice but lack high-quality comparable evidence. Therefore, we performed this meta-analysis and discovered no statistical differences in survival outcomes between the two regimens, which was consistent with results from two other meta-analyses of cisplatin regimens in head and neck carcinoma [21, 22]. The possible reasons for the above results are as follows: First, for NPC, radiotherapy is the cornerstone, and radiotherapy alone may already achieve good local control. Second, during radiotherapy combined with cisplatin chemotherapy, whether the weekly or triweekly regimen both can improve radiotherapy sensitivity, eliminate micrometastases and prolong survival. Third, there is some evidence to suggest that the cumulative dose of cisplatin during CCRT is more meaningful than the administration schedule. Some studies have shown that good efficacy can be achieved if the cumulative dose of cisplatin is no less than 200 mg/m2 [23]. In our meta-analysis, except for the study by Meng [6] and Gundog [13], and the median cumulative dose of cisplatin in other studies [1, 10,11,12, 14] all reached or exceeded 200 mg/m2.
Although there were no significant differences in survival outcomes of the weekly and triweekly cisplatin regimens,through this meta-analysis, we observed differences in hematological adverse events in the two groups. Contrasting with the triweekly cisplatin regimen, the weekly cisplatin regimen obviously led to more thrombocytopenia and leukopenia. The reason for this result may be that there was a short interval between the weekly cisplatin regimen, and patients who had not recovered from previous chemotherapy and received concurrent radiotherapy at the same time were more prone to develop hematotoxicity. However, the report by Lee suggested similar toxicity between the two groups [10]. Furthermore, Rampino believed that more frequent administration of smaller dosages of cisplatin would cause less toxicity when preserving the therapeutic effect [24]. Nonetheless, we believe that our meta-analysis is more convincing because it included RCTs and retrospective studies with large sample sizes. Of course, an increasing level of exploration is warranted in the future.
Our subgroup analysis showed that AC was not associated with efficacy. CCRT was close to CCRT + AC in terms of OS and DFS for patients with locally advanced nasopharyngeal cancer. This finding is consistent with several published studies. Two clinical trials revealed that AC did not significantly improve OS or PFS [25, 26]. In addition, two meta-analyses showed that AC after CCRT did not improve survival [27, 28]. Regarding CCRT plus AC, patients have more serious toxicity, resulting in poor tolerance and compliance. Thus, only some of the patients can undergo AC in most cases, which may be the reason why AC cannot increase survival benefits [29, 30].
It is worth noting that in our included studies, whether using a weekly cisplatin regimen or triweekly cisplatin regimen, most patients received radiotherapy with intensity-modulated radio therapy (IMRT) technology, while only a few patients received radiotherapy with 2D-RT or 3D-RT technology. With the improvement of radiotherapy technology, IMRT technology has become mainstream for nasopharyngeal cancer patients by degrees. In two studies, it was suggested that IMRT improves local control for nasopharyngeal carcinoma compared to 2D-RT [31, 32]. Another study compared the 10-year survival outcomes of 2D-RT with IMRT, showing that IMRT improved OS and DFS in nasopharyngeal carcinoma patients [33]. However, we did not focus on radiotherapy techniques in our statistical analysis. The reason was that we thought that 2D-RT or 3D-RT may be able to achieve the optimal radiotherapy effect for patients with LA-NPC. Furthermore, the multivariate Cox analyses of two studies discovered that different radiotherapy techniques were not significantly related to survival outcomes [34, 35]. Therefore, more research is required to identify the best radiotherapy techniques in the future.
Moreover, the 2022 American Society of Clinical Oncology (ASCO) annual meeting has already reported that IMRT alone can achieve similar survival rates compared to CCRT for low-risk stage II nasopharyngeal carcinoma, and it can decrease toxicity and increase quality of life [36]. However, in our meta-analysis, some studies included stage II patients, but risk stratification was not performed, and all patients with stage II received CCRT treatment. It may be necessary for the future to further classify patients with stage II NPC and to use different treatments for different types to maximize the patient's benefit.
Nonetheless, there were some limitations in our meta-analysis. First, this meta-analysis had only two RCTs, and the others were retrospective studies. Second, most of the studies came from China, which has a high incidence of nasopharyngeal cancer, and it is not clear whether our results are applicable to other regions. Third, not all articles showed data on LRFS, DFS and DMFS. Fourth, the level of radiotherapy varies among centers. Finally, different studies had different median follow-up times.
Conclusion
The weekly cisplatin regimen showed no difference in survival outcomes but more hematological toxicity in the treatment process than the triweekly cisplatin regimen. We speculate that the triweekly regimen has the potential to replace the weekly regimen for locally advanced nasopharyngeal cancer in the future, although larger data accumulation and more multicenter clinical trials may be needed to verify these results.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LA-NPC:
-
Locally advanced nasopharyngeal cancer
- CCRT:
-
Concurrent chemoradiotherapy
- OS:
-
Overall survival
- DMFS:
-
Distant metastasis-free survival
- LRFS:
-
Locoregional recurrence–free survival
- DFS:
-
Disease-free survival
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- RevMan 5.4:
-
Review Manager software 5.4
- AC:
-
Adjuvant chemotherapy
- NPC:
-
Nasopharyngeal cancer
- PICOS:
-
Population, Intervention, Comparison, Outcomes and Study design
- RCT:
-
Randomized control trial
- ECOG/PS:
-
Eastern Cooperative Oncology Group Performance Status Scale
- KPS:
-
Karnofsky's index of performance status
- NOS:
-
Newcastle‒Ottawa Scale
- MH:
-
Mantel‒Haenszel
- ASCO:
-
American Society of Clinical Oncology
- Re.:
-
Retrospetive study
- AJCC:
-
American Joint Committee on Cancer
- UICC:
-
The Union for International Cancer
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- NA:
-
Not available
- IMRT:
-
Intensity modulated radiotherapy
- 3D-CRT:
-
3-Dimensional conformalradiation therapy
- 2D-CRT:
-
2-Dimensional conformalradiation therapy
- LRRFS:
-
Loco-regional relapse-free survival
- FFS:
-
Failure-free survival
- ORR:
-
Overall response rate
- PFS:
-
Progression-free survival
- QOL:
-
The European Organization for Research and Treatment of Cancer QOL questionnaire modules QLQ-C30 and QLQ-H&N35
- CI:
-
Confifidence interval
References
Xia WX, Lv X, Liang H, Liu GY, Sun R, Zeng Q, et al. A Randomized controlled trial comparing two different schedules for cisplatin treatment in patients with locoregionally advanced nasopharyngeal cancer. Clin Cancer Res. 2021;27(15):4186–94. https://doi.org/10.1158/1078-0432.CCR-20-4532.
Afqir S, Ismaili N, Errihani H. Concurrent chemoradiotherapy in the management of advanced nasopharyngeal carcinoma: current status. J Can Res Ther. 2009;5(1):3–7. https://doi.org/10.4103/0973-1482.48763.
Baujat B, Audry H, Bourhis J, et al. Chemotherapy in locally advanced nasopharyngeal carcinoma: an individual patient data meta-analysis of eight randomized trials and 1753 patients. Int J Radiat Oncol Biol Phys. 2006;64(1):47–56. https://doi.org/10.1016/j.ijrobp.2005.06.037.
Wei WI, Sham JS. Present status of management of nasopharyngeal carcinoma. Expert Rev Anticancer Ther. 2001;1(1):134–41. https://doi.org/10.1586/14737140.1.1.134.
Wei WI, Sham JS. Nasopharyngeal carcinoma. Lancet. 2005;365(9476):2041–54. https://doi.org/10.1016/S0140-6736(05)66698-6.
Meng DF, Sun R, Peng LX, Huang YS, Yang Q, Luo DH, et al. A comparison of weekly versus 3-weekly cisplatin during concurrent chemoradiotherapy for locoregionally advanced nasopharyngeal carcinoma using intensity modulated radiation therapy: a matched study. J Cancer. 2018;9(1):92–9. https://doi.org/10.7150/jca.21357.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928. https://doi.org/10.1136/bmj.d5928.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. https://doi.org/10.1186/1745-6215-8-16.
Lee JY, Sun JM, Oh DR, Lim SH, Goo J, Lee SH, et al. Comparison of weekly versus triweekly cisplatin delivered concurrently with radiation therapy in patients with locally advanced nasopharyngeal cancer: a multicenter randomized phase II trial (KCSG-HN10–02). Radiother Oncol. 2016;118(2):244–50. https://doi.org/10.1016/j.radonc.2015.11.030.
Zhu Q, Hu H, Tang LQ, You R, Zhao JJ, Weng DS, et al. Weekly versus triweekly cisplatin plus intensity-modulated radiotherapy in locally advanced nasopharyngeal carcinoma: a propensity score analysis with a large cohort. J Cancer. 2018;9(19):3447–55. https://doi.org/10.7150/jca.26110.
Wang K, Dong J, He S, Wang X, Jiang C, Hu P, et al. Comparison of weekly and triweekly cisplatin regimens during concurrent chemoradiotherapy for nasopharyngeal carcinoma. BMC Cancer. 2019;19(1):482. https://doi.org/10.1186/s12885-019-5688-z.
Gundog M, Basaran H, Bozkurt O, Eroglu C. A comparison of cisplatin cumulative dose and cisplatin schedule in patients treated with concurrent chemo-radiotherapy in nasopharyngeal carcinoma. Braz J Otorhinolaryngol. 2020;86(6):676–86. https://doi.org/10.1016/j.bjorl.2019.04.008.
Jagdis A, Laskin J, Hao D, Hay J, Wu J, Ho C. Dose delivery analysis of weekly versus 3-weekly cisplatin concurrent with radiation therapy for locally advanced nasopharyngeal carcinoma (NPC). Am J Clin Oncol. 2014;37(1):63–9. https://doi.org/10.1097/COC.0b013e31826b9b1a.
Chen QY, Wen YF, Guo L, Liu H, Huang PY, Mo HY, Li NW, Xiang YQ, Luo DH, Qiu F, Sun R, Deng MQ, Chen MY, Hua YJ, Guo X, Cao KJ, Hong MH, Qian CN, Mai HQ. Concurrent chemoradiotherapy vs radiotherapy alone in stage II nasopharyngeal carcinoma: phase III randomized trial. J Natl Cancer Inst. 2011;103(23):1761–70. https://doi.org/10.1093/jnci/djr432.
Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized Intergroup study 0099. J Clin Oncol. 1998;16:1310–7. https://doi.org/10.1200/JCO.1998.16.4.1310.
Liang ZG, Zhu XD, Zhou ZR, Qu S, Du YQ, Jiang YM. Comparison of concurrent chemoradiotherapy followed by adjuvant chemotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a meta-analysis of 793 patients from 5 randomized controlled trials. Asian Pac J Cancer Prev. 2012;13(11):5747–52. https://doi.org/10.7314/apjcp.2012.13.11.5747. (PMID: 23317250).
Zhang B, Li MM, Chen WH, Zhao JF, Chen WQ, Dong YH, Gong X, Chen QY, Zhang L, Mo XK, Luo XN, Tian J, Zhang SX. Association of chemoradiotherapy regimens and survival among patients with nasopharyngeal carcinoma: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(10): e1913619. https://doi.org/10.1001/jamanetworkopen.2019.13619.
Blanchard P, Lee A, Marguet S, Leclercq J, Ng WT, Ma J, et al. Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC metaanalysis. Lancet Oncol. 2015;16:645–55. https://doi.org/10.1016/S1470-2045(15)70126-9.
Zhang ZJ, Shi LL, Hong XH, Xiao BY, Lin GH, Liu Q, Wang BC. A Bayesian network meta-analysis of the primary definitive therapies for locoregionally advanced nasopharyngeal carcinoma: IC+CCRT, CCRT+AC, and CCRT alone. PLoS ONE. 2022;17(3): e0265551. https://doi.org/10.1371/journal.pone.0265551.
Szturz P, Wouters K, Kiyota N, Tahara M, Prabhash K, Noronha V, Castro A, Licitra L, Adelstein D, Vermorken JB. Weekly low-dose versus three-weekly high-dose cisplatin for concurrent chemoradiation in locoregionally advanced non-nasopharyngeal head and neck cancer: a systematic review and meta-analysis of aggregate data. Oncologist. 2017;22(9):1056–66. https://doi.org/10.1634/theoncologist.2017-0015.
Jacinto JK, Co J, Mejia MB, Regala EE. The evidence on effectiveness of weekly vs triweekly cisplatin concurrent with radiotherapy in locally advanced head and neck squamous cell carcinoma (HNSCC): a systematic review and meta-analysis. Br J Radiol. 2017;90(1079):20170442. https://doi.org/10.1259/bjr.20170442.
Peng H, Chen L, Zhang Y, Li WF, Mao YP, Zhang F, Guo R, Liu LZ, Lin AH, Sun Y, Ma J. Prognostic value of the cumulative cisplatin dose during concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma: a secondary analysis of a prospective phase III clinical trial. Oncologist. 2016;21(11):1369–76. https://doi.org/10.1634/theoncologist.2016-0105.
Rampino M, Ricardi U, Munoz F, Reali A, Barone C, Musu AR, Balcet V, Franco P, Grillo R, Bustreo S, et al. Concomitant adjuvant chemoradiotherapy with weekly low-dose cisplatin for high-risk squamous cell carcinoma of the head and neck: a phase II prospective trial. Clin Oncol. 2011;23(2):134–40. https://doi.org/10.1016/j.clon.2010.09.004.
Chan ATC, Hui EP, Ngan RKC, Tung SY, Cheng ACK, Ng WT, Lee VHF, Ma BBY, Cheng HC, Wong FCS, Loong HHF, Tong M, Poon DMC, Ahuja AT, King AD, Wang K, Mo F, Zee BCY, Chan KCA, Lo YMD. Analysis of plasma epstein-barr virus DNA in nasopharyngeal cancer after chemoradiation to identify high-risk patients for adjuvant chemotherapy: a randomized controlled trial. J Clin Oncol. 2018. https://doi.org/10.1200/JCO.2018.77.7847.
Chen L, Hu CS, Chen XZ, Hu GQ, Cheng ZB, Sun Y, Li WX, Chen YY, Xie FY, Liang SB, Chen Y, Xu TT, Li B, Long GX, Wang SY, Zheng BM, Guo Y, Sun Y, Mao YP, Tang LL, Chen YM, Liu MZ, Ma J. Adjuvant chemotherapy in patients with locoregionally advanced nasopharyngeal carcinoma: Long-term results of a phase 3 multicentre randomised controlled trial. Eur J Cancer. 2017;75:150–8. https://doi.org/10.1016/j.ejca.2017.01.002.
Yan M, Kumachev A, Siu LL, Chan KK. Chemoradiotherapy regimens for locoregionally advanced nasopharyngeal carcinoma: a Bayesian network meta-analysis. Eur J Cancer. 2015;51(12):1570–9. https://doi.org/10.1016/j.ejca.2015.04.027.
Chen YP, Wang ZX, Chen L, Liu X, Tang LL, Mao YP, Li WF, Lin AH, Sun Y, Ma J. A Bayesian network meta-analysis comparing concurrent chemoradiotherapy followed by adjuvant chemotherapy, concurrent chemoradiotherapy alone and radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma. Ann Oncol. 2015;26(1):205–11. https://doi.org/10.1093/annonc/mdu507.
Chen L, Hu CS, Chen XZ, Hu GQ, Cheng ZB, Sun Y, Li WX, Chen YY, Xie FY, Liang SB, Chen Y, Xu TT, Li B, Long GX, Wang SY, Zheng BM, Guo Y, Sun Y, Mao YP, Tang LL, Chen YM, Liu MZ, Ma J. Concurrent chemoradiotherapy plus adjuvant chemotherapy versus concurrent chemoradiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2012;13(2):163–71. https://doi.org/10.1016/S1470-2045(11)70320-5.
Chen Y, Liu MZ, Liang SB, Zong JF, Mao YP, Tang LL, Guo Y, Lin AH, Zeng XF, Ma J. Preliminary results of a prospective randomized trial comparing concurrent chemoradiotherapy plus adjuvant chemotherapy with radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma in endemic regions of china. Int J Radiat Oncol Biol Phys. 2008;71(5):1356–64. https://doi.org/10.1016/j.ijrobp.2007.12.028.
Zhang MX, Li J, Shen GP, Zou X, Xu JJ, Jiang R, et al. Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: a 10-year experience with a large cohort and long follow-up. Eur J Cancer. 2015;51(17):2587–95. https://doi.org/10.1016/j.ejca.2015.08.006.
Xu T, Zhou X, Shen C, Hu C. Suggestions for surveillance and radiation strategy in nasopharyngeal carcinoma treated with IMRT: based on hazard-rate and patterns of recurrence. Oral Oncol. 2018;76:61–7. https://doi.org/10.1016/j.oraloncology.2017.11.022.
Chen L, Zhang Y, Lai SZ, Li WF, Hu WH, Sun R, et al. 10-year results of therapeutic ratio by intensity-modulated radiotherapy versus two-dimensional radiotherapy in patients with nasopharyngeal carcinoma. Oncologist. 2019;24(1):e38-45. https://doi.org/10.1634/theoncologist.2017-0577.
Fountzilas G, Ciuleanu E, Bobos M, et al. Induction chemotherapy followed by concomitant radiotherapy and weekly cisplatin versus the same concomitant chemoradiotherapy in patients with nasopharyngeal carcinoma: a randomized phase II study conducted by the Hellenic Cooperative Oncology Group (HeCOG) with biomarker evaluation. Ann Oncol. 2012;23(2):427–35. https://doi.org/10.1093/annonc/mdr116.
Hong RL, Hsiao CF, Ting LL, et al. Final results of a randomized phase III trial of induction chemotherapy followed by concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in patients with stage IVA and IVB nasopharyngeal carcinoma Taiwan Cooperative Oncology Group (TCOG) 1303 Study. AnnOncol. 2018;29(9):1972–9. https://doi.org/10.1093/annonc/mdy249.
Ma J, Tang L-L, Guo R, Zhang N, Deng B, Zhang Y, et al. Radiotherapy alone versus concurrent chemoradiotherapy in intermediate risk nasopharyngeal carcinoma: A multicentre, open-label, noninferiority, randomised phase III trial. J Clin Oncol. 2022;40(16):6000–6000. https://doi.org/10.1200/JCO.2022.40.16_suppl.6000.
Acknowledgements
Not applicable.
Funding
“Ten Thousand Plan” Youth Talent Project in Yunnan Province(no grant number is idoneous) sponsored this protocol. The project participated in design of the study.
Author information
Authors and Affiliations
Contributions
XW, XY and SCZ performed this study. LX,LL and SRM were responsible for data acquisition. GJY, LZF, XYY, ZLX, XTR, LX, LL analyzed the data and did the Statistical analysis. LX, LL, SRM, GJY were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, X., Li, L., Sun, R. et al. Weekly versus triweekly cisplatin treatment in patients with locally advanced nasopharyngeal cancer during concurrent chemoradiotherapy. Eur J Med Res 28, 399 (2023). https://doi.org/10.1186/s40001-023-01297-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01297-y