Abstract
Introduction
During the cancer treatment path, cancer patients use numerous drugs, including anticancer, supportive, and other prescribed medications, along with herbs and certain products. This puts them at risk of significant drug interactions (DIs). This study describes DIs in cancer patients and their prevalence and predictors.
Methods
A cross-sectional study design was used to achieve the study objectives. The study was carried out in two centers in the northern West Bank, Palestine. The Lexicomp® Drug Interactions tool (Lexi-Comp, Hudson OH, USA) was applied to check the potential DIs. In addition, the Statistical Package for the Social Sciences (SPSS) was used to show the results and find the associations.
Results
The final analysis included 327 patients. Most of the participants were older than 50 years (61.2%), female (68.5%), and had a solid tumor (74.6%). The total number of potential DIs was 1753, including 1510 drug-drug interactions (DDIs), 24 drug-herb interactions, and 219 drug-food interactions. Importantly, the prevalence of DDIs was 88.1%. In multivariate analysis, the number of potential DDIs significantly decreased with the duration of treatment (p = 0.007), while it increased with the number of comorbidities (p < 0.001) and the number of drugs used (p < 0.001).
Conclusions
We found a high prevalence of DIs among cancer patients. This required health care providers to develop a comprehensive protocol to monitor and evaluate DIs by improving doctor-pharmacist communication and supporting the role of clinical pharmacists.
Similar content being viewed by others
Introduction
Cancer is an expression used to describe a set of diseases characterized by uncontrolled cellular growth in any part of the body [1]. It poses a global health burden as its prevalence and death rate swiftly rise [1]. Recently, cancer has become the leading cause of death worldwide [1]. In 2020, 3191 new cancer cases were documented in Palestine, 32.8% being elderly (above 64 years) [2]. According to the last report by the Palestinian Ministry of Health in 2020, cancer was the third cause of death (14.1%) in Palestine [2].
Drug interaction (DI) occurs when the targeted drug is affected by another agent and results in alterations in its clinical effect [3]. This interaction may influence the pharmacokinetics, pharmacodynamics, or the targeted drug's pharmaceutical properties [4]. Consequently, it negatively impacts the patient’s quality of life by either potentiating the drug-related adverse effects or reducing its efficacy [5]. It is noteworthy that oncology patients are prone to such interactions for several reasons [5]. First, they are treated with more than one anticancer agent. Second, multiple drugs are prescribed to treat their chronic conditions [5]. Third, supportive medications are sometimes used to control therapy-related adverse effects or disease-related symptoms [5]. Fourth, they sometimes use alternative medicine (such as herbs) or over-the-counter (OTC) products [5]. In particular, 4% of cancer-related deaths are due to a severe drug-related event, including DIs [6].
Multiple articles were published from the developed and developing countries to describe the prevalence, predictors, and features of drug-drug interactions (DDIs) among cancer patients, which showed a variation in the prevalence of DDIs [7,8,9,10,11,12,13,14,15,16,17]. This could be due to differences in the prescribing pattern and the interaction tool. For example, in Palestine, two studies reported a remarkably high prevalence of DDIs among hemodialysis (89.1%) [18] and cardiovascular patients (94%) [19], while another study documented a prevalence of 56% in surgical patients [20].
Of note, DDIs among Palestinian oncology patients were not described previously. In addition, data regarding the interactions of drugs with herbs and other products were lacking. This makes research in this area paramount to identify and address potential DIs in the cancer population. Our study was designed to identify the prevalence of DIs among Palestinian oncology patients. Therefore, it will help formulate a clinical intervention method to minimize clinically significant DIs in this category. Furthermore, the study aimed to describe the main factors related to DDIs and determine their characteristics. And this work will be a fundamental reference for decision-makers to properly evaluate the profiles of the medications of patients and increase their awareness and knowledge of DIs.
Methods
Study design
A cross-sectional study design was used by including two main sources of information; cancer patients and medical records (electronic and patient files). Indeed, this work was done by interviewing all cancer patients who were attending the hospitals to receive their treatment between April 2021 and December 2021. The interviews were achieved by three clinical pharmacists who recorded all patients’ medications (including prescribed, OTC, and supportive care drugs) and miscellaneous products (including alcohol, caffeine, tobacco, and grapefruit) they take, and asked about the symptoms they complained at the time of interview. Moreover, detailed information about patients’ characteristics and anticancer treatment was extracted from medical records.
Study setting
Our study took place in the oncology center at An-Najah National University Hospital and Al-Watani Hospital in Nablus, Palestine. These centers are considered the largest centers in Palestine and the main reference for pediatric and adult patients with hematologic and nonhematologic malignancies in Palestine; the West Bank and Gaza Strip.
Study population and sampling procedure
According to medical records, the number of cancer patients visiting the two hospitals during the study period was around 2150. Using the Daniel formula [21]; n = Z2*P (1-P) / d2, where n = sample to be calculated when the population size is more than 10,000, z = 1.96 (CI of 95%), d = 0.05 (absolute precision as a margin of error), P = 0.5 expected prevalence or response distribution. The resulting sample size was 385 patients. As our population is less than 10,000 (N = 2,150), we adjusted this number using the adjusted sample equation; adjusted sample = n/ (1 + (n/N)). Therefore, the sample size was found to be 327 patients, with a 5% margin of error, a response of 50%, and a 95% confidence interval.
Inclusion and exclusion criteria
Our study included all cancer patients aged 18 years or above with all cancer types and stages who came to the hospitals during the study period to take their anticancer medications in the outpatient setting. Patients who refused or were unable to participate, did not mention all their medications, had psychological problems, or were hospitalized were excluded.
Data collection instrument
The data collection form contained variables regarding sociodemographic and clinical information of the patients, including age, sex, body mass index (BMI), education level, family history of cancer, type of cancer, the current state of disease, the intent of treatment, duration of treatment, current medications, use of miscellaneous agents, herbal use, and symptoms. Based on a previous study [7], all drugs used were classified into two subgroups, which are ≤ 7 drugs or > 7.
All medications, herbs, and other products of each patient were entered into a software program Lexicomp® Drug Interactions (Lexi-Comp, Hudson OH, USA), to assess the potential DIs and classify their clinical significance and implications. This program was chosen because it has high sensitivity and specificity and is sometimes used as a gold standard to compare DI tools [22, 23]. Previously, it was also used to evaluate the drug-dietary supplement interactions [24] and drug-herb interactions [25]. This instrument classifies DIs according to their risk rating (A = no known interaction, B = no action needed, C = monitor therapy, D = consider therapy modification, or X = avoid combination), severity (N/A, minor, moderate, or major), and reliability (poor, fair, good, or excellent). In addition, all potential DDIs were independently checked by three practicing clinical pharmacists to ensure data accuracy.
Ethical approval
All aspects of the study protocol, including access to and use of the patient's clinical information, were approved by the Institutional Review Boards (IRB) and the local health authority. In addition, we fully explained all parts of the study to the patients and obtained their informed verbal consent before starting data collection.
Statistical analysis
We used the Statistical Package for Social Sciences program (IBM-SPSS) version 21 to analyze the data. Frequencies and percentages were used to explain the results. In addition, the median and interquartile ranges were used to express the continuous variables. As appropriate, the Kruskal–Wallis test or Mann–Whitney U test was applied to check the differences between variables. The Spearman test was used to examine the correlation between continuous variables. Furthermore, multiple linear regression analysis was performed to predict the variables that had a significant correlation with the number of DDIs. A p-value of < 0.05 was highlighted as significant for all applied tests.
Results
Sociodemographic and clinical characteristics
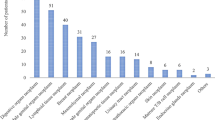
Of the 375 patients, 23 refused or were unable to participate, 4 had a psychological problem, and 21 did not mention all their medications. Therefore, 327 cancer patients were included in the final study. 61.2% of our sample was above 50 years, 68.5% were female, and 36.1% were obese. Regarding cancer types, 25.4% had hematologic malignancies, whereas 74.6% had solid cancer (Table 1). The most frequent types were breast cancer (37.9%), colon cancer (12.2%), non-Hodgkin lymphoma (7.6%), and multiple myeloma (7.6%) (Table 2). Approximately 59% of the patients have been treated for less than a year. Approximately half of the respondents (49.5%) had chronic diseases other than their primary disease (cancer). 51.7% used more than seven medications and 38.8% were prescribed more than two anticancer drugs. The prevalence of herbal use was 56.0%. Furthermore, 81.0% and 29.7% of the patients regularly consumed caffeine and grapefruit, respectively (Table 1).
Reported symptoms
The number of symptoms reported among the study sample ranged from 0 and 16, with a mean ± SD of 6.8 ± 3.5. However, the most common symptoms reported by the respondents were as follows: generalized weakness (75.5%), body aches (66.4%), pallor (57.2%), anorexia (50.0%), and nausea and vomiting (47.4%) (Table 3).
Description of DDIs
The total number of potential DIs was 1753, distributed as 1510 DDIs, 24 drug-herb interactions, and 219 drug-miscellaneous product interactions. Patients have used 1–19 drugs and the mean ± SD was 8.0 ± 3.2. The prevalence of DDIs among cancer patients was 88.1% (N = 288), 27.2% had 1–2 DDIs, 21.1% had 3–4 DDIs, and 12.8% had 5–6 DDIs, while 26.9% of the respondents had more than six DDIs. The characteristics of DDIs are presented in Table 4. Of all potential DDIs, 857 (56.8%) were classified as moderate interactions, while 13.2% were major interactions. In the risk rating classification, most of the DDIs (56.0%) had a ‘C’ category, 11.1% were ‘D’, and only 40 DDIs (2.6%) were considered ‘X’. Furthermore, the majority of DDIs had either fair (69.1%) or good (26.2%) reliability. The most frequent pairs of DDIs were Paracetamol/Ondansetron, Cyclophosphamide/Ondansetron, Doxorubicin/Cyclophosphamide, Metformin/Dexamethasone, and Dexamethasone/Aspirin (Table 5). However, combinations that should be avoided ‘X’ were Doxorubicin/Aprepitant (n = 20) and Promethazine/Metoclopramide (n = 6).
Description of drug-herb and drug-food interactions
The patients have used 0–24 herbs and the mean ± SD was 1.3 ± 1.9. Anise (Pimpinella anisum L.) 28.4%, mixed herb 17.1%, Chamomile (Matricaria chamomilla L.) 11%, and Sage (Salvia officinalis L.) 9.1% were the most used herbs. Only 24 drug-herb interactions were found and 219 drug-miscellaneous product interactions. The most common interactions were Dexamethasone/Grapefruit, Prednisolone/Grapefruit, Paclitaxel/Grapefruit, Atorvastatin/Grapefruit, and Amlodipine/Grapefruit (Table 6). However, the combination that should be avoided ‘X’ was Aprepitant/Grapefruit (n = 8).
Univariate and multivariate analysis of potential DDIs
Univariate analysis showed a significant association between the number of DDIs and the following variables: age (p < 0.001), duration of treatment (p = 0.001), number of comorbid diseases (p < 0.001), number of all drugs used (p < 0.001), number of anticancer drugs (p = 0.001). However, the type and status of cancer were not significantly associated with the number of potential DDIs (Table 7). Furthermore, the Spearman's correlation coefficient showed a significant and positive correlation between the number of observed DDIs and the number of reported symptoms (p = 0.032); (Table 8).
Multiple linear regression analyses revealed that the number of potential DDIs decreased significantly with the treatment duration (p = 0.007). At the same time, it increased with the number of comorbidities (p < 0.001) and the number of drugs used (p < 0.001). No multicollinearity was found between the independent variables (Tables 9 and 10).
Discussion
Drug-drug interactions (DDIs) are a series of events or circumstances during pharmacotherapy that may cause the patient's expected therapeutic outcomes to be compromised. This study highlights the prevalence and risk rating classification of drug-drug, drug-herb, and drug-food interactions and determines the predictors of DDIs in oncology patients.
In the current study, 68.5% of our sample was female. Female patients accounted for 4,668 cases in Palestine, accounting for more than half (54%) of all cases [2]. Furthermore, solid cancer represented 74.6% of the sample. Similarly, solid tumors (84.8%) account for most cancer cases in Palestine, whereas hematologic malignancies account for 15.2% [2]. Furthermore, breast cancer followed by colon cancer represents the most frequent types in both the study sample and the Palestinian cancer population [2].
According to the findings of this study, the prevalence of DDIs among cancer patients was potentially high (88.1%), which means that the majority of cancer patients had at least one DDI. The percentage is higher compared to other studies, 78% [7] and 24.2% [26]. However, India reported that 88.9% had at least one DDI [27], and in Pakistan, it was 92% [28], and the findings in both studies are similar to our analysis. In a study conducted in Korea specifically on oral antineoplastic agents, the prevalence was highest among the targeted agents (63.2%) followed by traditional agents (21.2%) and endocrine agents (19.3%) [29]. Furthermore, previous studies in Palestine also reported potentially high percentages of DDIs among different populations, such as hemodialysis patients (89.1%) [18] and cardiovascular patients (94%); [19]. However, another study reported a lower percentage (56%) among Palestinian surgical patients [20]. It can be clearly seen that the prevalence of DDIs among the cancer population is extremely high, as described in numerous studies around the world. This is in part due to the use of multiple medications, which requires the development of a clinical oncology pharmacy service to provide pharmacotherapy consultations to prevent any serious DDI, medication errors, and adverse effects related to anticancer medications [30].
Of all 1510 potential DDIs, 857 (56.8%) were classified as moderate interactions, which require medication monitoring. While the majority of the DDIs (56%) had a C category in the risk rating classification and only 11.1% of DDIs that necessitate modifying the medication are in category D. A suitable monitoring strategy should be created to identify the detrimental impacts of Category C interactions. In a small percentage of individuals, dosage changes for one or both medicines may be required. However, in category D, a patient-specific evaluation is required and specific steps must be taken accordingly. Aggressive monitoring, empiric dose modifications, or the use of alternative drugs are examples of these actions.
In our study, patients had 40 interactions (2.6%) with category X. Compared to other studies, this percentage is considered high [7]. However, it was lower than a study conducted in India [27]. The adverse effect of these interactions exceeds the benefits. For instance, Promethazine/Metoclopramide is one of the interactions to be avoided; the probable mechanism for this interaction has been reported as QTc interval prolongation. On the other hand, aprepitant acts as a liver enzyme (cytochrome P450 3A4) inhibitor that affects the metabolism of some cancer drugs and leads to an increase in blood concentration, causing adverse effects related to the drug used, i.e. Doxorubicin/Aprepitant.
Paracetamol/Ondansetron, Cyclophosphamide/Ondansetron, Doxorubicin/Cyclophosphamide, Metformin/Dexamethasone, and Dexamethasone/Aspirin were the most common DDI pairs. Interactions between Cyclophosphamide/Ondansetron and Cyclophosphamide/Doxorubicin were also found in a previous study [7]. Cyclophosphamide may enhance the cardiotoxicity of anthracyclines. However, the interactions, Cyclophosphamide/Ondansetron and Metformin/Dexamethasone, were among the most common in India [27]. The proposed mechanisms of these interactions are that ondansetron may decrease the serum concentration of cyclophosphamide, and dexamethasone may decrease the therapeutic effect of metformin.
In general, the prevalence of complementary and alternative medicine use especially herbal medicine among cancer patients is significantly high in Palestine, accounting for 69.5% [31], and 68% [32] in the two study cohorts, and other studies reported that in different populations in Palestine [33, 34]. Along with traditional therapy, cancer patients, particularly in Middle Eastern nations, also utilize herbal medications more frequently than the general population. The rationale for this use includes lowering the likelihood of recurrence, increasing health status, and reducing the adverse effects of cancer treatment. Furthermore, a lack of awareness and education on drug-herb interactions among physicians, patients, and the general public and research limitations in this area has resulted in several potential negative effects, including direct toxic effects and potential interactions with anticancer drugs [35]. In this study, the most commonly used herbs in cancer patients were anise, mixed herbs, chamomile, and sage. These findings differ from a couple of studies that found ephedra is the most widely used herb in Palestinian cancer patients [31, 32]. Ephedra use was 0.0% in 2011 [31], 55.2% in 2014 [31], 31.1% in 2016 [32], while it was only 3.4% in our study. During 2014 and 2016, the media played a role in promoting the benefit of ephedra in cancer patients [31, 32], which explained the high prevalence of ephedra use at that time, while currently, its decreased use may be due to improved awareness in this population. Furthermore, in terms of the drug-food relationship, a case report described the significant interaction between docetaxel and grapefruit juice by limiting its clearance by more than 15% [36]. One of the most common interactions in our study was Paclitaxel/Grapefruit, while Aprepitant/Grapefruit should be avoided.
The main outcomes of the current study are the large number of observed DIs and the correlation between the number of reported symptoms and the number of DDIs. In fact, this relationship is quite controversial, as the number of reported symptoms could be a potential cause of DIs only if the drugs involved were prescribed as part of a prescribing cascade to alleviate new symptoms of potential adverse events. However, as expected, the number of potential DDIs, the duration of treatment, and the number of comorbidities were all significant in multiple linear regression. In a study conducted in Pakistan in which hospitalized patients, combination chemotherapy, and patients with solid malignancy were all significant in univariate analysis, but they were insignificant in multiple linear regression. The only predictors were the number of all prescribed drugs and anticancer medications [7]. Furthermore, the number of drugs used was significant, which is consistent with the findings of a study conducted in Iran [37]. Other studies have found that as the number of drugs and health problems increases, the risk of DDIs increases in patients receiving antineoplastic therapy [27, 30, 38]. It was reported that one of the consequences of polypharmacy is DDIs, since the patient, especially the elderly, will have several medications to take, multiple health problems, inpatient admissions, and other medications to treat adverse reactions [27]. However, a study conducted by Riechelmann et al. showed that type of cancer and medication indications (to treat comorbid conditions versus supportive care) were associated with DDIs in patients with cancer [12]. In terms of duration of treatment, it was inversely proportioned with the number of DDIs in multiple regression analysis, this result may be attributed to the good knowledge that the patient acquires during the treatment path. We also found a significant and positive correlation between the number of DDIs and the number of reported symptoms. In fact, a more extensive evaluation is necessary regarding this point, as the consequences of DDIs may cause new symptoms or cancer patients may tend to use medications to alleviate their symptoms, thus increasing the risk of DDIs.
Strengths and limitations
This is the first study in Palestine that describes the prevalence and features of the potential DIs among oncology patients. The main strength of this study is the inclusion of patients with all types of cancer, those who are taking oral or intravenous anticancer medications, and the assessment of the DIs with other substances (such as herbs and foods) that practitioners sometimes neglect. Nonetheless, our study had limitations. First, it has a relatively small sample size, and only two centers are included. Therefore, the results could not be generalized. Second, we did not check the clinical implications of potential DDIs. Third, one screening tool was applied, and some herbs were not found during the searching process. Importantly, there are other available sources of information on drug interactions that may be used at the same time to increase sensitivity to detect potential interactions. Finally, all types of DDIs were included in the analysis even those of low clinical importance, such as classes A and B.
Conclusions
As mentioned earlier, the prevalence of potential DDIs among the cancer population was extremely high, which required local institutions to develop a comprehensive protocol to monitor and evaluate the DIs by improving doctor-pharmacist communication and supporting the role of clinical pharmacists. For example, the clinical pharmacist should continuously review the medications profile of cancer patients to accurately detect any interactions. On the other hand, many sources detect the interactions, which may differ significantly with respect to the information posted. Therefore, a group consensus should be reached to use a specific interaction screening tool. Furthermore, healthcare professionals must improve patients’ knowledge of self-medication and improve their awareness regarding DIs. We recommend conducting more studies to examine the relationship between observed DDIs and poor health and economic outcomes.
Availability of data and materials
Due to privacy, the datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DIs:
-
Drug interactions
- SPSS:
-
Statistical Package for the Social Sciences
- DDIs:
-
Drug-drug interactions
- OTC:
-
Over-the-counter
- BMI:
-
Body mass index
- IRB:
-
Institutional Review Boards
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase (AST)
- MM:
-
Multiple myeloma
- NHL:
-
Non-Hodgkin lymphoma
- HL:
-
Hodgkin lymphoma
- AML:
-
Acute myeloid leukemia
- ALL:
-
Acute lymphoblastic leukemia
- CLL:
-
Chronic lymphocytic leukemia
References
World Health Organisation. Cancer. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed 7 Sept 2021.
Palestinian Ministry of Health. Statistical reports: Health Annual Report. Palestine; 2020. Available from: http://site.moh.ps/Content/Books/chup6JkjmKecG8zGx6hnXjILuGecGmPq7Bt4Q4HsFj6vv7tW2W4aGE_ZiCEqSMuZx7v6kHVcDAjC59QDCVuSXx3NmUfwX6Ciqm4OxQrB4xAE6.pdf. Accessed 7 Sept 2021.
Riechelmann RP, Del Giglio A. Drug interactions in oncology: how common are they? Ann Oncol. 2009;20(12):1907–12.
Beijnen JH, Schellens JH. Drug interactions in oncology. Lancet Oncol. 2004;5(8):489–96.
Riechelmann R, Girardi D. Drug interactions in cancer patients: a hidden risk? J Res Pharm Pract. 2016;5(2):77–8.
Buajordet I, Ebbesen J, Erikssen J, Brørs O, Hilberg T. Fatal adverse drug events: the paradox of drug treatment. J Intern Med. 2001;250(4):327–41.
Ismail M, Khan S, Khan F, Noor S, Sajid H, Yar S, Rasheed I. Prevalence and significance of potential drug-drug interactions among cancer patients receiving chemotherapy. BMC Cancer. 2020;20(1):335.
Vecchia S, Orlandi E, Confalonieri C, Damonti E, Riva A, Sartori A, Cavanna L. Prevalence study on potential drug-drug interaction in cancer patients in Piacenza hospital’s Onco-Haematology department. J Oncol Pharm Pract. 2018;24(7):490–3.
Ramos-Esquivel A, Víquez-Jaikel Á, Fernández C. Potential drug-drug and herb-drug interactions in patients with cancer: a prospective study of medication surveillance. J Oncol Pract. 2017;13(7):e613–22.
Singh H, Singh B. Drug-drug interactions in cancer chemotherapy: an observational study in a tertiary health care centre. Drug Metab Pers Ther. 2017;32(4):219–23.
Mouzon A, Kerger J, D’Hondt L, Spinewine A. Potential interactions with anticancer agents: a cross-sectional study. Chemotherapy. 2013;59(2):85–92.
Riechelmann RP, Tannock IF, Wang L, Saad ED, Taback NA, Krzyzanowska MK. Potential drug interactions and duplicate prescriptions among cancer patients. J Natl Cancer Inst. 2007;99(8):592–600.
van Leeuwen RWF, Jansman FGA, van den Bemt P, de Man F, Piran F, Vincenten I, Jager A, Rijneveld AW, Brugma JD, Mathijssen RHJ, et al. Drug-drug interactions in patients treated for cancer: a prospective study on clinical interventions. Ann Oncol. 2015;26(5):992–7.
Popa MA, Wallace KJ, Brunello A, Extermann M, Balducci L. Potential drug interactions and chemotoxicity in older patients with cancer receiving chemotherapy. J Geriatr Oncol. 2014;5(3):307–14.
Riechelmann RP, Moreira F, Smaletz O, Saad ED. Potential for drug interactions in hospitalized cancer patients. Cancer Chemother Pharmacol. 2005;56(3):286–90.
Ko Y, Tan SL, Chan A, Wong YP, Yong WP, Ng RC, Lim SW, Salim A. Prevalence of the coprescription of clinically important interacting drug combinations involving oral anticancer agents in Singapore: a retrospective database study. Clin Ther. 2012;34(8):1696–704.
Chen L, Cheung WY. Potential drug interactions in patients with a history of cancer. Curr Oncol. 2014;21(2):e212-220.
Al-Ramahi R, Raddad AR, Rashed AO, Bsharat A, Abu-Ghazaleh D, Yasin E, Shehab O. Evaluation of potential drug- drug interactions among Palestinian hemodialysis patients. BMC Nephrol. 2016;17:96.
Al-Jabi SW, Aldabe L, Alhaj-Asaad L, Thaher M. Zyoud SeH, Sweileh WM: Assessment of drug interactions and their associated factors among patients with cardiovascular diseases: a cross-sectional study from the occupied Palestinian territory. The Lancet. 2021;398:S8.
Rabba AK, Abu Hussein AM, Abu Sbeih BK, Nasser SI. Assessing drug-drug interaction potential among patients admitted to surgery departments in three palestinian hospitals. Biomed Res Int. 2020;2020:9634934.
Daniel WW. Biostatistics: A Foundation for analysis in the health sciences. 7th ed. New York: John Wiley & Sons; 1999.
Morte-Romea E, Luque-Gómez P, Arenere-Mendoza M, Sierra-Monzón JL, Camón Pueyo A, Pellejero Sagastizabal G, Verdejo Muñoz G, Sánchez Fabra D, Paño-Pardo JR. Performance assessment of software to detect and assist prescribers with antimicrobial drug interactions: are all of them created equal? Antibiotics (Basel). 2020;9(1):19.
Marcath LA, Xi J, Hoylman EK, Kidwell KM, Kraft SL, Hertz DL. Comparison of nine tools for screening drug-drug interactions of oral oncolytics. J Oncol Pract. 2018;14(6):e368–74.
Patel RI, Beckett RD. Evaluation of resources for analyzing drug interactions. J Med Libr Assoc. 2016;104(4):290–5.
Tsai H-H, Lin H-W, Lu Y-H, Chen Y-L, Mahady GB. A review of potential harmful interactions between anticoagulant/antiplatelet agents and Chinese herbal medicines. PLoS ONE. 2013;8(5):e64255–e64255.
Marcath LA, Coe TD, Hoylman EK, Redman BG, Hertz DL. Prevalence of drug-drug interactions in oncology patients enrolled on National Clinical Trials Network oncology clinical trials. BMC Cancer. 2018;18(1):1155.
Ramasubbu SK, Mahato SK, Agnihotri A, Pasricha RK, Nath UK, Das BD. Prevalence, severity, and nature of risk factors associated with drug-drug interactions in geriatric patients receiving cancer chemotherapy: a prospective study in a tertiary care teaching hospital. Cancer Treat Res Commun. 2021;26: 100277.
Bibi R, Azhar S, Iqbal A, Jabeen H, Kalsoom UE, Iqbal MM, Nazeer M. Prevalence of potential drug-drug interactions in breast cancer patients and determination of their risk factors. J Oncol Pharm Pract. 2021;27(7):1616–22.
Kim SH, Suh Y, Ah YM, Jun K, Lee JY. Real-world prevalence of potential drug-drug interactions involving oral antineoplastic agents: a population-based study. Support Care Cancer. 2020;28(8):3617–26.
Moghaddas A, Adib-Majlesi M, Sabzghabaee AM, Hajigholami A, Riechelmann R. Potential drug-drug Interactions in hospitalized cancer patients: A report from the Middle-East. J Oncol Pharm Pract. 2021;27(1):46–53.
Ali-Shtayeh MS, Jamous RM, Salameh NM, Jamous RM, Hamadeh AM. Complementary and alternative medicine use among cancer patients in Palestine with special reference to safety-related concerns. J Ethnopharmacol. 2016;187:104–22.
Jaradat NA, Shawahna R, Eid AM, Al-Ramahi R, Asma MK, Zaid AN. Herbal remedies use by breast cancer patients in the West Bank of Palestine. J Ethnopharmacol. 2016;178:1–8.
Zyoud SH, Al-Jabi SW, Sweileh WM, Tabeeb GH, Ayaseh NA, Sawafta MN, Khdeir RL, Mezyed DO, Daraghmeh DN, Awang R. Use of complementary and alternative medicines in haemodialysis patients: a cross-sectional study from Palestine. BMC Complement Altern Med. 2016;16:204.
Al-Ramahi R, Jaradat N, Shalalfeh R, Nasir S, Manasra Y, Shalalfeh I, Esam Y. Evaluation of potential drug- herb interactions among a group of Palestinian patients with chronic diseases. BMC Complement Altern Med. 2015;15:221.
Ben-Arye E, Samuels N, Goldstein LH, Mutafoglu K, Omran S, Schiff E, Charalambous H, Dweikat T, Ghrayeb I, Bar-Sela G, et al. Potential risks associated with traditional herbal medicine use in cancer care: A study of Middle Eastern oncology health care professionals. Cancer. 2016;122(4):598–610.
Valenzuela B, Rebollo J, Perez T, Brugarolas A, Perez-Ruixo JJ. Effect of grapefruit juice on the pharmacokinetics of docetaxel in cancer patients: a case report. Br J Clin Pharmacol. 2011;72(6):978–81.
Tavousi F, Sadeghi A, Darakhshandeh A, Moghaddas A. Potential drug-drug interactions at a referral pediatric oncology ward in iran: a cross-sectional study. J Pediatr Hematol Oncol. 2019;41(3):e146–51.
Fogli S, Del Re M, Curigliano G, van Schaik RH, Lancellotti P, Danesi R. Drug-drug interactions in breast cancer patients treated with CDK4/6 inhibitors. Cancer Treat Rev. 2019;74:21–8.
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
AAK conceptualized and designed the study, analyzed the data, wrote the manuscript, checked all potential DIs, and supervised the team. MAN and BAS performed data collection, reviewed the literature, and participated in data analysis and manuscript writing. SSS and NTA checked all potential DIs, reviewed the literature, and participated in data analysis. ANS participated in data collection and analysis and reviewed the literature. RA, HTS, and SHZ took responsibility for the accuracy of the analysis, revised the manuscript critically for enhancement of intellectual contents, and assisted in the final write-up of the manuscript. Then, all authors reviewed and accepted the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All aspects of the study protocol, including access to and use of the patient clinical information, were approved by An-Najah National University’s Institutional Review Board (IRB) (approval number: Pharm July/2020/1) and the Palestinian ministry of health. We fully explained all parts of the study to the patients and obtained their informed verbal consent before starting data collection. The IRB of An-Najah National University approved only verbal consent. Because we did not collect any identifying information during the interview and our study did not pose a major risk to participants, An-Najah National University’s IRB waived the requirement for written informed consent. The authors confirmed that all methods were performed following the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Koni, A.A., Nazzal, M.A., Suwan, B.A. et al. A comprehensive evaluation of potentially significant drug-drug, drug-herb, and drug-food interactions among cancer patients receiving anticancer drugs. BMC Cancer 22, 547 (2022). https://doi.org/10.1186/s12885-022-09649-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09649-3