Abstract
Background
Malaria in pregnancy can result in placental infection with fetal implications. This study aimed at assessing placental malaria (PM) prevalence and its associated factors in a cohort of pregnant women with peripheral malaria and their offspring.
Method
The data were collected in the framework of a clinical trial on treatments for malaria in pregnant women . Placental malaria (PM) was diagnosed by histopathological detection of parasites and/or malaria pigment on placenta biopsies taken at delivery. Factors associated with PM were assessed using logistic regression.
Results
Out of 745 biopsies examined, PM was diagnosed in 86.8 % of women. Acute, chronic and past PM were retrieved in 11 (1.5 %), 170 (22.8 %), and 466 (62.6 %) women, respectively. A modifying effect was observed in the association of gravidity or anemia at the study start with pooled PM (presence of parasites and/or malaria pigment). In women under 30, gravidity ≤ 2 was associated with an increased prevalence of pooled PM but in women aged 30 years or more, gravidity was no more associated with pooled PM (OR 6.81, 95 % CI 3.18 – 14.60; and OR 0.52, 95 % CI 0.10 – 2.76, respectively). Anemia was associated with pooled PM in women under 30 (OR 1.96, 95 % CI 1.03 – 3.72) but not in women aged 30 years or more (OR 0.68, 95 % CI 0.31 – 1.49). Similarly, the association of gravidity with past-chronic PM depended also on age. A higher prevalence of active PM was observed in women under 30 presenting with symptomatic malaria (OR 3.79, 95 % CI 1.55 – 9.27), while there was no significant increase in the prevalence of active PM (presence of parasites only) in women with symptomatic malaria when aged 30 years or more (OR 0.42, 95 % CI 0.10 – 1.75). In women with chronic PM, the prevalence of low birth weight or prematurity was the highest (31.2 %) as compared with past PM or no PM.
Conclusion
Despite the rapid diagnosis and efficacious treatment of peripheral infection, the prevalence of placental malaria remained high in women with P. falciparum peripheral infection in Nanoro, especially in younger women This underlines the importance of preventive measures in this specific group.
Similar content being viewed by others
Background
In 2019, 12 million pregnant women were infected by malaria worldwide. According to World Health Organization, more than one-third (35 %) of these infections occurred in the West-African region [1]. Plasmodium falciparum (P.falciparum) is the parasite responsible for a large majority of cases of malaria in the general population in Africa [2]. Despite the endemicity of malaria in sub-Saharan African countries, the prevalence of P.falciparum infection following microscopic examination of the peripheral blood of women with prolonged duration of pregnancy in the rainy season at first antenatal care visit raises to 60 % [3]. Placental malaria (PM) has been reported up to 40 % at delivery [4]. Infected red blood cells present at their surface the P.falciparum erythrocyte membrane protein1 (PfEMP1) expressed by the parasite and coded by the var gene family. There are different types of this protein binding to various receptors on the endothelium of the blood vessels [2]. Literature on placental malaria indicates mostly that chondroitin sulfate A (CSA) is the receptor in the placenta on which bind the parasitized red blood cells presenting the variant VAR2CSA a subgroup of the PfEMP1 [2, 5]. This allows the parasites to sequestrate and accumulate in the intervillous spaces [6]. Hyaluronic acid was cited as another receptor of P. falciparum[5]. However, the results are unclear as its activity seemed to be mediated through chondroitin sulfate [5]. Placental malaria can result in maternal anemia [7], low birth weight (LBW), or preterm delivery (PTD) [7,8,9] which can induce neurocognitive and other health disorders later in life [10, 11].
Pregnant women acquire protective immunity against PM as their ages increase. That is why younger pregnant women are more prone to PM than their older counterparts [12, 13]. Also, women pregnant for the first time (primigravidae) are more subject to placental malaria in endemic settings compared to those with second pregnancy or more (multigravidae) [14, 15]. The immune reaction initiated as a response against the infection occurring in the first pregnancy become more and more protective with the subsequent pregnancies as antibodies are developed against the parasite and prevent it binding and sequestrating into the placenta [12, 16].
We hypothesized that the immunity related to age may influence the relationship between gravidity and other maternal characteristics and PM. While factors associated with placental malaria have been studied widely, there is little information on these potential interactions [9, 15, 17,18,19,20,21,22]. Few studies assessed factors associated with PM in Burkina Faso where malaria is endemic with seasonal transmission [15, 23]. In a study conducted in Nanoro in 2013, approximately 43 % of pregnant women attending antenatal care visits presented with peripheral parasitemia and therefore were at increased risk of PM [24].
The current study aims to assess the prevalence of PM in Burkina Faso and to assess if factors associated with PM are depending on age.
Methods
Study settings and population
The present study used data collected in the framework of a multicenter, randomized, open-label trial of treatments for malaria in pregnant women entitled: “safe and efficacious artemisinin-based combination treatments for African pregnant women with malaria (PREGACT)” which is registered under the number NCT00852423. The latter evaluated the efficacy and safety of four artemisinin-based combination treatments (ACT) in pregnant women with P. falciparum parasitemia whatever the presence of symptoms. However, women with symptoms and/or signs (clinical or biological) of severe malaria were not included. Detailed methodology and study results were published elsewhere [25, 26].
Recruitment and follow-up
Briefly, second or thirdtrimester pregnant women with microscopically confirmed P. falciparum peripheral infection, who were willing to give informed consent, were enrolled and treated with one of the four ACTs at random and followed up until delivery. All participants were provided a long-lasting insecticidal bed net upon inclusion.
Data collection
At inclusion in the parent study, obstetrical, medical, demographic, and anthropometric data were recorded. The use of malaria prevention methods before the inclusion in the study was documented. Peripheral malaria infection was confirmed and parasites density and species were determined by microscopic examination of thick and thin blood smear stained with Giemsa [25]. Hemoglobin level was determined using a portable HemoCue (Hb301 Hemocue®, Angelholm, Sweden). Gestational age and fetal viability were confirmed ultrasonographically using a portable Fukuda Denshi® machine (FFsonic, UF – 4100).
The cure of the initial episode was ascertained on the basis of a negative blood smear obtained at the end of the three days treatment course. Peripheral malaria parasitemia occurring after the this episodeuntil delivery was recorded.
Delivery date and mode, gestational age, and newborn characteristics were collected. Also, a biopsy of the placenta was collected.
Placental malaria diagnosis
Biopsies pieces were collected from the maternal side of the placenta, as soon as possible after delivery and kept in a neutral buffered 10 % formalin. Subsequent procedures comprised embedment in paraffin wax, slicing in 4 mm thick sections, and staining with hematoxylin– eosin. Reading and classification of PM patterns were done according to the method described by Ismail. Acute PM infection was considered in presence of parasites and absence of malaria pigment. Chronic PM infection was considered in presence of both malaria parasites and malaria pigment. A past PM was considered in absence of malaria parasites but the presence of malaria pigment. No PM infection was considered when there were no malaria parasites nor malaria pigment [27]. An external quality control (EQC) was performed during the study. Before the start of the study, a training set of placental slides prepared by the EQC center was sent to the site for evaluation. At the start of the study, the first 25 samples included in the study site were sent to the EQC center for revision. Finally, 5 % of the samples were revised by the EQC center. Active PM comprised acute or chronic placental infections and represented all placentas with parasites, while past-chronic PM referred to past or chronic infections, corresponding to all placentas with malaria pigment. Gravidity did not include the present pregnancy. Symptomatic malaria referred to , fever at enrolment with parasitemia regardless of the density, or parasitemia witha minimum of three of the following symptoms: fever in the past 24 hours, muscular- and articular pain, head pain, tiredness or weakness [26]. Recurrent malaria was defined as the occurrence of a malaria infection after initial treatment and before delivery regardless of the number of episodes. Anemia was defined as a hemoglobin level lower than 11g/dl. Underweight was defined as pregnancy body mass index < 18.50 kg/m2. Preterm birth was defined as a birth occurring before 37 weeks of gestation and low birth weight was defined as birth weight below 2500 g. The season at delivery was either rainy (July to December) or dry (January to June) [15].
Statistical analysis
The gestational age at delivery was calculated from the estimation done by ultrasonography at inclusion. The association of placental malaria with maternal characteristics was assessed using logistic regression. Only factors associated with PM with p-value < 0.05 in the univariate analysis were kept for the multivariate models. The modifying effect of age was assessed by introducing interactions in logistic regression. Interactions of age with the following maternal characteristics were considered: gravidity, anemia, symptomatic malaria at study start, recurrent malaria during follow-up, and season at delivery. When an interaction was statistically significant, the odds ratios of the association of these variables with placental malaria and their 95 % confidence intervals were estimated by age category. Outcome variables were either pooled PM, active PM, or past-chronic PM. Distribution of low birth weight (LBW) and prematurity by placental malaria status was also outlined.
The statistical significance level was set at 0.05. All analyses were performed using
STATA® statistical software version 16 (Statacorp LLC, Texas, USA).
Only one woman was pregnant for the first time and this did not allow us to create a separate group of primigravidae.
Ethics
The PREGACT study was approved by the ethics committee of the University of Antwerp in Belgium and the National Ethics Committee of Burkina Faso. Written or witnessed thumb-printed informed consent was obtained from all participants before inclusion and any study procedure was undertaken. All the procedures of the study were carried out according to the guidelines of the ethics committees of Burkina Faso and Belgium that provided approvals.
Results
Characteristics of study participants
From June 2010 to April 2013, 870 pregnant women in their second or third trimester were recruited into the PREGACT trial at Nanoro and Nazoanga sites. Among the 847 women who delivered, 779 had a placental histology assessment. After excluding 13 twins and 21 stillbirths or malformations, the remaining cohort included 745 participants (Fig. 1).
At inclusion, 588 (78.9 %) women were under 30 years, 355 (47.7 %) had less than 3 previous pregnancies, 308 (41.4 %) had symptomatic malaria, and 447 (74.2 %) had anemia (Table 1).
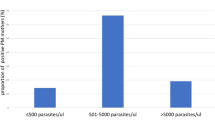
Patterns and distribution of placental malaria
Overall, PM was diagnosed in 647 (86.8 %) women. Parasites were seen in 181 (24.3 %) of the placentas and malaria pigment in 636 (85.4 %). Acute, chronic, and past placental malaria was diagnosed in 11 (1.5 %), 170 (22.8 %) and 466 (62.6 %) women, respectively. (Fig. 2). Past infection prevalence was 69.4 % in women delivering in the dry season. Women under 30 years of age experienced more past PM than women of 30 years or over (64.8 % and 54.1 %, respectively). The past PM was more frequent when gravidity ≤ 2 than when gravidity > 2 (65.1% and 60.3%, respectively). Chronic PM distribution followed a trend similar to past PM for maternal age groups (25.9 % in women < 30 years and 11.5 % in women ≥ 30 years) and gravidity groups (31.0 % in women with gravidity ≤ 2 and 15.4 % in women with gravidity > 2). Acute infections were scarce and observed mostly in women of 30 years or more (3.8 %) (Table 2).
Histopathological diagnosis and distribution of placental malaria. Legend: +: present; -: absent. The region of the grey circle with black dots in the background corresponds to the presence of parasites only in the placenta and represents active placental malaria. The region of the orange circle with orange background corresponds to the presence of malaria pigment only in the placenta and represents past placental malaria. The region where the two circles overlap corresponds to the presence of both parasites and malaria pigment and represents chronic placental malaria. The region of the black circle with white background corresponds to the absence of both parasites or malaria pigment and represents placenta free of malaria infection
Factors associated with placental malaria
In univariate analysis, age < 30 years, gravidity ≤ 2, anemia, symptomatic malaria at inclusion, recurrent malaria during follow-up, and rainy season at delivery were associated with pooled PM (Table 3), with past-chronic PM (Fig. 3), and with active PM (Fig. 4). Women who did not sleep under a bed net the night before their enrollment into the main trial had a higher prevalence of active PM than women who slept under a bed net.
Maternal factors associated with past-chronic placental malaria in univariate analysis. Legend: OR: odds ratio; CI: confidence interval; IPTp: intermittent preventive treatment during pregnancy with sulfadoxine-pyrimethamine; AL; artemether-lumefantrine; ASAQ: artesunate-amodiaquine; MQAS: mefloquine-artesunate. Anemia: hemoglobin < 11g/dl; Underweight: body mass index < 18.5 kg/m2; Rainy season: July-December; Dry season: January-June
Maternal factors associated with active placental malaria in univariate analysis. Legend: OR: odds ratio; CI: confidence interval; IPTp: intermittent preventive treatment during pregnancy with sulfadoxine-pyrimethamine; AL; artemether-lumefantrine; ASAQ: artesunate-amodiaquine; MQAS: mefloquine-artesunate. Anemia: hemoglobin < 11g/dl; Underweight: body mass index < 18.5 kg/m2; Rainy season: July-December; Dry season: January-June
In multivariable analysis, there was a modifying effect in the association of maternal characteristics with PM. In women under 30 years of age, gravidity ≤ 2 was associated with a higher prevalence of pooled PM but in women of 30 years or more, gravidity was no more associated with pooled PM (OR 6.81, 95 % CI 3.18 – 14.60; and OR 0.52, 95 % CI 0.10 – 2.76, respectively). Anemia at enrollment was also associated with pooled PM in women under 30 years of age (OR 1.96, 95 % CI 1.03 – 3.72) but not in women of 30 years or more (OR 0.68, 95 % CI 0.31 – 1.49) (Table 4). A modifying effect was also observed in the association of gravidity with past-chronic PM (Table 5). Symptomatic malaria was associated with active PM in women under 30 years of age (OR 3.79, 95 % CI 1.55 – 9.27). The association was not significant in women of 30 years or more (OR 0.42, 95 % CI 0.10 – 1.75) (Table 6).
Distribution of low birth weight or prematurity by placental malaria patterns
LBW or prematurity was observed in 31.2 % and 23.4 % of newborns from mothers with chronic PM and past PM, respectively. Among newborns from women without PM, 13.3 % were LBW or preterm. Surprisingly, none of the newborns from mothers with acute PM was LBW or preterm. (Fig. 5).
Discussion
Our study showed that PM prevalence was high in this cohort of pregnant women with P. falciparum peripheral infection at inclusion. Past infections were the predominant PM pattern, followed by chronic infections, acute infections being scarce. A modifying effect according to age was noticed in the association of gravidity, anemia, and symptomatic malaria with PM. Our data also evidenced a higher prevalence of LBW or prematurity in newborns from mothers with chronic PM compared to newborns from mothers with past PM or without PM infection.
We reported 86.8 % of women with PM. Placental malaria is expected to be more prevalent in mothers with peripheral infection than in mothers without detectable peripheral infection, as reported in Malawi, in India, and a metanalysis [20, 28, 29]. The lower PM prevalence in Malawi (78.3%) compared to our study could be explained by the peri-urban characteristic of the Malawi study location. Also, malaria in pregnancy burden is usually higher in rural areas like in our study setting than in urban areas [30]. Peripheral infections in our study were all due to P. falciparum, the malaria parasite with the greatest potential to accumulate in the placenta [31]. We hypothesized that this contributed to the higher prevalence of PM in our study compared to an Indian study (64.1 %) where mixed P.falciparum and Plasmodium vivax peripheral infections occurred as well [20].
A lower proportion (56 % to 58 %) of infected placentas compared to our study were reported in the same area in another multicentric study. This difference could be explained by the inclusion of both women with and without peripheral infection in the latter [15].
Malaria parasites were found in 24.3 % (active infection) of the placentas in our study, while malaria pigment was present in 85.4 %. Malaria pigment could be a marker of peripheral parasitemia at the initial stage of the pregnancy, active infection reflecting more near-term intense peripheral infection [29, 32]. It was also suggested that without treatment, malaria pigment could be a marker of prior infection of the placenta [33].
In our study, 13.2 % of the placentas were uninfected. Such discordance between peripheral and placental malaria was already reported in Nigeria. Authors attributed this to peripheral parasitemia of low density occurring at the beginning of the pregnancy [19], probably cleared by chemoprevention [15] before reaching the placenta. It is reported that with time, malaria pigment can be cleaned from the placenta following a rapid and efficacious treatment. Artemether-lumefantrine (AL) has even been found associated with less accumulation of malaria pigment in the placenta than quinine [34,35,36]. In our study, all malaria peripheral infections (initial and subsequent) in the study participants were treated with highly efficacious artemisinin-based combination therapies including AL, regardless of the density of the parasites or the presence of symptoms [26]. This probably contributed to prevent or clear placental malaria in a small proportion of them.
Maternal age [7, 37, 38], gravidity [15, 18, 39, 40], anemia [9, 28], and symptoms [9, 41] are some of the factors associated with placental malaria in studies conducted in pregnant women regardless of patent peripheral parasitemia. The above-mentioned factors were also associated with the presence of malaria pigment in a metanalysis conducted in 2020 using data from a quite selected population of pregnant women with peripheral parasitemia at enrolment.
The association of gravidity, anemia at study start, and symptomatic malaria at study start with PM was modified by maternal age in our study.
Placental malaria affects primigravidae or secundigravidae more than multigravidae [9, 15, 18, 40]. In our study, pooled PM and past-chronic PM were more frequent in younger women with lower gravidity. These findings suggest that for a certain pattern of PM, the protective effect of parity-specific immunity depends on maternal age [12]. Indeed, a study modeling the immunity against placental malaria-specific to the parity in 2013 showed that the highest level of this immunity was overloaded when the entomological inoculation rate (EIR) exceeds 100 [33]. As EIR is usually above that threshold in most of the countries where malaria transmission is high and stable [42], this suggests that the risk of placental malaria might be similar in pregnant women whatever their gravidities in such settings. This is true for older women in our study while younger women with lower gravidities remained more at risk of placental malaria. Thus, this supposes that in settings where malaria transmission is high and stable, age-related immunity contributes significantly to the control of the infection as far as immunity related to parity [12].
In our study, a higher prevalence of pooled PM was observed in anemic women aged less than 30 years. Infected red blood cells bind to the vascular walls in the bone marrow. This results in a lower production of red blood cells contributing to anemia [43, 44]. In malaria-endemic regions, older pregnant women acquire antibodies that prevent infected red blood cells from binding to the vascular walls [2, 45]. We infer that younger pregnant women are producing less protective antibodies and this is why they are more prone to both anemia and PM [2, 30].
Undernutrition is one of the main causes of anemia through iron insufficiency in low and middle-income countries [46, 47] like Burkina Faso. Studies conducted in several countries across sub-Saharan Africa reported a higher prevalence of anemia in younger pregnant women than in older [48,49,50] irrespective of malaria infection. However, there is a probable interaction between malaria and undernutrition [51]. As the nutritional status influences immunity, the ability of an individual to regulate and eradicate infection like malaria could be modified by undernutrition [52]. Conversely, the proteins are increasingly destroyed and the energy consumed during the inflammatory response induced by an infection like malaria. This could lead to the depletion of the nutritional reserve [51, 53]. We hypothesized that the increased prevalence of placental malaria in young anemic women in our study might illustrate the interplay between malaria and nutrition.
Pregnant women could benefit from iron and folic acid supplements without being exposed to an increased risk of malaria compared to those receiving folic acid only [54]. However, the benefit of this supplementation for their offspring was questionable as a study conducted at the Nanoro site reported an increased risk of prematurity in women supplemented with iron and folic acid compared to women supplemented with folic acid alone [55].
Symptomatic malaria was associated with active PM in women aged less than 30 years of age in our study. Acquired immunity against malaria is weak in younger women and may be compared to that of women residing in regions. As a result, they may experience more clinical episodes [13, 56].
Fever is the most common symptom in individuals infected by malaria. The presence of fever implies intense parasitemia above the pyrogenic threshold overpassing the tolerance capacity [57,58,59]. This suggests that in young symptomatic women the number of parasites reaching the placenta is increased because of the high density of parasitemia in the bloodstream. Some authors proposed to use symptomatic malaria as a proxy for PM diagnosis antenatally [60]. In sub-Saharan malaria-endemic regions, this would underestimate the burden of PM as peripheral infections are often asymptomatic [24].
The risk factors of placental malaria are not limited to the above-mentioned. They include environmental and socio-economic factors as far as the use of preventive measures against malaria. Indeed, placental malaria prevalence was higher in women delivering in the dry season compared to those delivering in the rainy season in a study conducted in Benin, Burkina Faso, and The Gambia [15]. In Cameroon, pregnant women who earned less than 28 000 fcfa per month were more at risk of placental malaria [61]. A low educational level may be associated with an increased risk of placental malaria as found in Nigeria [37]. Pregnant women who did not sleep under bed net were more at risk of placental malaria [62, 63]. In our study, the season of delivery was significantly associated with placental malaria with infections occurring more in the rainy season than the dry season. This association did not depend on age. Bed net use and IPTp-SP were not associated with placental malaria in our multivariate analysis.
[64, 65, 43, 44, 2, 45, 54, 55, 13, 56, 60] Reduced birth weight and preterm birth were more prevalent with chronic infections [9, 66]. In our study, the composite outcome of LBW and prematurity was also more frequent in newborns from mothers with chronic PM. The fetal growth restriction caused by the inflammatory response to chronic infection was cited as a possible contributing factor of LBW [8]. These adverse pregnancy outcomes associated with placental malaria underline the need of protecting pregnant women from malaria. Placental malaria incidence could be significantly reduced in endemic areas through the deployment of preventive measures in the first stage of the pregnancy [33]. It was estimated that up to 65 % of placental malaria occurred during the first trimester of pregnancy [67]. As IPTp-SP cannot be given at that time, the WHO recommends starting the first dose as soon as possible in the second trimester [68]. The emergence of parasites strains resisting SP did not yet compromise its efficacy in West African countries like Burkina Faso. The resistance ranged from low to moderate [69], thus SP is still used for IPTp and remains efficacious against asymptomatic parasitemia [70, 71]. Evaluation of alternative drugs for IPTp like dihydroartemisinin-piperaquine or mefloquine is ongoing, as well as exploration of new strategies such as community-based malaria screening and treatment in pregnancy, alone or in combination with IPTp-SP [15, 72, 73]. Placental malaria prevention could be better achieved by adding the benefit from sleeping under an insecticide-treated bed net starting in the first trimester of pregnancy to that of SP intake [69]. Also, it is known that a substantial part of malaria infection detected at the beginning of the pregnancy likely originate in the preconception period [3, 33, 74]. Therefore, some authors suggest extending prevention actions to this period too [3, 33].
The present analysis had some limitations. The study was not designed primarily to assess factors associated with PM. Thus, we did not assess some factors like educational and socio-economic levels. This information was not captured in the database of the parent study.
In the present study, we aimed at exploring the extent to which age could be associated with placental malaria. Thus, we chose 30 years as the cut-off, going beyond the usual cut-off of fewer than 25 years in most of the studies investigating the relationship between placental malaria and age [7]. This could seem arbitrary. However, our cut-off is close to the mean age of childbearing of 29 years estimated for 2015-2020 for Africa [75]. The cut-off of 30 years was already used in a study assessing risk factors of placental malaria in Nigeria in 2012 [19]. Another study reported a lower utilization of long-lasting insecticidal bed net in women of childbearing age under 30 years than in older women [76]. We explore whether this might represent an extra risk of placental malaria in our cohort. We did not find a significant interaction between age and bed net use before the inclusion in the relationship to placental malaria in multivariable analysis. Only one participant was pregnant for the first time and this may be influenced our results as primigravidae have a different immunity status compared to the others [33]. The study was conducted in a rural area where malaria is highly prevalent compared to urban areas [30]. Therefore, the inference should be limited to such settings. Also, our cohort consisted entirely of women with peripheral infection at enrollment. Therefore, comparison to unselected women could be biased.
However, our study has several strengths. The participants were recruited at peripheral health centers, the first level of contact with the health system and this reduces the chances of a selection bias. The prospective design was also an advantage. Analysis exploring interactions of age with other maternal factors are more relevant to understanding how factors are associated with PM.
Conclusion
Despite the rapid diagnosis and efficacious treatment of peripheral infections, the prevalence of placental malaria remained high in women with peripheral P. falciparum infection in Nanoro, especially in younger women . This underlines the importance of preventive measures in this specific group.
Availability of data and materials
The datasets supporting these analyses were not publicly available due to ethical and privacy considerations. However, access could be granted upon motivated and reasonable request addressed to Tinto Halidou, e-mail: tintohalidou@gmail.com.
Abbreviations
- °C:
-
Celsius degree
- ACT:
-
Artemisinin based combination therapy
- AL:
-
Artemether-Lumefantrine
- ASAQ:
-
Artesunate-Amodiaquine
- CI:
-
Confidence interval
- EIR:
-
Entomological inoculation rate
- EQC:
-
External quality control
- G:
-
Gram
- IPTp-SP:
-
Intermittent preventive treatment during pregnancy with sulfadoxine-pyrimethamine
- Kg:
-
Kilogramm
- LBW:
-
Low birth weight
- m2 :
-
meter square
- mm3 :
-
cubic millimetre
- MQAS:
-
Mefloquine-Artesunate
- OR:
-
Odds ratio
- PM:
-
Placental malaria
- PREGACT:
-
Safe and efficacious artemisinin-based combination treatments for African pregnant women with malaria
- PTD:
-
Preterm delivery
- SP:
-
Sulfadoxine-Pyrimethamine
References
WHO. World malaria report 2019. Available at: https://www.who.int/publications-detail/world-malaria-report-2019#. Accessed 1 Jan 2020.
Clark RL. Genesis of placental sequestration in malaria and possible targets for drugs for placental malaria. Birth Defects Res. 2019;111(10):569–83.
Berry I, Walker P, Tagbor H, Bojang K, Coulibaly SO, Kayentao K, et al. Seasonal Dynamics of Malaria in Pregnancy in West Africa: Evidence for Carriage of Infections Acquired Before Pregnancy Until First Contact with Antenatal Care. Am J Trop Med Hyg. 2018;98(2):534–42.
Chico RM, Mayaud P, Ariti C, Mabey D, Ronsmans C, Chandramohan D. Prevalence of malaria and sexually transmitted and reproductive tract infections in pregnancy in sub-Saharan Africa: a systematic review. JAMA. 2012;307(19):2079–86.
Duffy PE. Plasmodium in the placenta: parasites, parity, protection, prevention and possibly preeclampsia. Parasitology. 2007;134(13):1877–81.
Matteelli A, Caligaris S, Castelli F, Carosi G. The placenta and malaria. Ann Trop Med Parasitol. 1997;91(7):803–10.
Omer SA, Idress HE, Adam I, Abdelrahim M, Noureldein AN, Abdelrazig AM, et al. Placental malaria and its effect on pregnancy outcomes in Sudanese women from Blue Nile State. Malar J. 2017;16(1):374.
Umbers AJ, Aitken EH, Rogerson SJ. Malaria in pregnancy: small babies, big problem. Trends Parasitol. 2011;27(4):168–75.
Lufele E, Umbers A, Ordi J, Ome-Kaius M, Wangnapi R, Unger H, et al. Risk factors and pregnancy outcomes associated with placental malaria in a prospective cohort of Papua New Guinean women. Malar J. 2017;16(1):427.
Lawford HLS, Lee AC, Kumar S, Liley HG, Bora S. Establishing a conceptual framework of the impact of placental malaria on infant neurodevelopment. Int J Infect Dis. 2019;84:54–65.
Chibwesha CJ, Zanolini A, Smid M, Vwalika B, Phiri Kasaro M, Mwanahamuntu M, et al. Predictors and outcomes of low birth weight in Lusaka, Zambia. Intl J Gynaecol Obstetr Official Organ Intl Feder Gynaecol Obstetr. 2016;134(3):309–14.
Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7(2):93–104.
Fried M, Duffy PE. Malaria during Pregnancy. Cold Spring Harb Prespect Med. 2017;7:a025551.
Okiring, J., Olwoch, P., Kakuru, A. et al. Household and maternal risk factors for malaria in pregnancy in a highly endemic area of Uganda: a prospective cohort study. Malar J. 2019; 18(1):144 PMID 31014336.
Cosmic Consortium. Community-based Malaria Screening and Treatment for Pregnant Women Receiving Standard Intermittent Preventive Treatment With Sulfadoxine-Pyrimethamine: A Multicenter (The Gambia, Burkina Faso, and Benin) Cluster-randomized Controlled Trial. Clin Infect Dis. 2019;68(4):586–96.
Rogerson SJ, Boeuf P. New approaches to pathogenesis of malaria in pregnancy. Parasitology. 2007;134(Pt 13):1883–93.
Boudova S, Divala T, Mungwira R, Mawindo P, Tomoka T, Laufer MK. Placental but Not Peripheral Plasmodium falciparum Infection During Pregnancy Is Associated With Increased Risk of Malaria in Infancy. J Infect Dis. 2017;216(6):732–5.
Briggs J, Ategeka J, Kajubi R, Ochieng T, Kakuru A, Ssemanda C, et al. Impact of Microscopic and Submicroscopic Parasitemia During Pregnancy on Placental Malaria in a High-Transmission Setting in Uganda. J Infect Dis. 2019;220(3):457–66.
Ezebialu IU, Eke AC, Ezeagwuna DA, Nwachukwu CE, Ifediata F, Ezebialu CU. Prevalence, pattern, and determinants of placental malaria in a population of southeastern Nigerian parturients. Int J Infect Dis. 2012;16(12):e860–5.
Ahmed R, Singh N, ter Kuile FO, Bharti PK, Singh PP, Desai M, et al. Placental infections with histologically confirmed Plasmodium falciparum are associated with adverse birth outcomes in India: a cross-sectional study. Malar J. 2014;13:232.
Adam I, Salih MM, Mohmmed AA, Rayis DA, Elbashir MI. Pregnant women carrying female fetuses are at higher risk of placental malaria infection. PLoS One. 2017;12(7):e0182394.
Carmona-Fonseca J, Arango E, Maestre A. Placental malaria in Colombia: histopathologic findings in Plasmodium vivax and P. falciparum infections. Am J Trop Med Hyg. 2013;88(6):1093–101.
Tagbor H, Cairns M, Bojang K, Coulibaly SO, Kayentao K, Williams J, et al. A Non-Inferiority, Individually Randomized Trial of Intermittent Screening and Treatment versus Intermittent Preventive Treatment in the Control of Malaria in Pregnancy. PLoS One. 2015;10(8):e0132247.
Tahita MC, Tinto H, Menten J, Ouedraogo J-B, Guiguemde RT, van Geertruyden JP, et al. Clinical signs and symptoms cannot reliably predict Plasmodium falciparum malaria infection in pregnant women living in an area of high seasonal transmission. Malar J. 2013;12:464.
Nambozi M, Mulenga M, Halidou T, Tagbor H, Mwapasa V, Phiri LK, et al. Safe and efficacious artemisinin-based combination treatments for African pregnant women with malaria: a multicentre randomized control trial. Reprod Health. 2015;12(1):5.
The PREGACT study Group. Four Artemisinin-Based Treatments in African Pregnant Women with Malaria. N Engl J Med. 2016;374(10):913–27.
Ismail MR, Ordi J, Menendez C, Ventura PJ, Aponte JJ, Kahigwa E, et al. Placental pathology in malaria: A histological, immunohistochemical, and quantitative study. Human Pathology. 2000;31(1):85–93.
Kalilani-Phiri L, Thesing PC, Nyirenda OM, Mawindo P, Madanitsa M, Membe G, et al. Timing of Malaria Infection during Pregnancy Has Characteristic Maternal, Infant and Placental Outcomes. PLoS One. 2013;8(9):e74643.
Saito M, Mansoor R, Kennon K, Anvikar AR, Ashley EA, Chandramohan D, et al. Pregnancy outcomes and risk of placental malaria after artemisinin-based and quinine-based treatment for uncomplicated falciparum malaria in pregnancy: a WorldWide Antimalarial Resistance Network systematic review and individual patient data meta-analysis. BMC Med. 2020;18(1):138.
Rogerson SJ, Desai M, Mayor A, Sicuri E, Taylor SM, van Eijk AM. Burden, pathology, and costs of malaria in pregnancy: new developments for an old problem. Lancet Infect Dis. 2018;18(4):e107–e18.
Ayres Pereira M, Mandel Clausen T, Pehrson C, Mao Y, Resende M, Daugaard M, et al. Placental Sequestration of Plasmodium falciparum Malaria Parasites Is Mediated by the Interaction Between VAR2CSA and Chondroitin Sulfate A on Syndecan-1. PLoS Pathog. 2016;12(8):e1005831.
Brabin BJ, Romagosa C, Abdelgalil S, Menéndez C, Verhoeff FH, McGready R, et al. The Sick Placenta—The Role of Malaria. Placenta. 2004;25(5):359–78.
Walker PGT, Griffin JT, Cairns M, Rogerson SJ, van Eijk AM, ter Kuile F, et al. A model of parity-dependent immunity to placental malaria. Nat Commun. 2013;4:1609.
McGready R, Davison BB, Stepniewska K, Cho T, Shee H, Brockman A, et al. The effects of Plasmodium falciparum and P. vivax infections on placental histopathology in an area of low malaria transmission. Am J Trop Med Hyg. 2004;70(4):398–407.
McGready R, Brockman A, Cho T, Levesque MA, Tkachuk AN, Meshnick SR, et al. Haemozoin as a marker of placental parasitization. Trans R Soc Trop Med Hyg. 2002;96(6):644–6.
Muehlenbachs A, Nabasumba C, McGready R, Turyakira E, Tumwebaze B, Dhorda M, et al. Artemether-lumefantrine to treat malaria in pregnancy is associated with reduced placental haemozoin deposition compared to quinine in a randomized controlled trial. Malar J. 2012;11:150.
Fehintola OA, Fehintola OF, Bakare B, et al. Prevalence, predictors, and perceived susceptibility to placental malaria parasitemia among pregnant women in a tertiary hospital in South-Western Nigeria. Res J Health Sci. 2019;7(4):280–9.
Oweisi PW, John CT, Omietimi JE, Aigere EOS, Allagoa DO, Kotingo EL. Placental malaria parasitization at delivery: experience at a Nigerian tertiary hospital. Eur Sci J. 2018;14(9):243–59.
Tran EE, Cheeks ML, Kakuru A, Muhindo MK, Natureeba P, Nakalembe M, et al. The impact of gravidity, symptomatology and timing of infection on placental malaria. Malar J. 2020;19(1):227.
Kapisi J, Kakuru A, Jagannathan P, Muhindo MK, Natureeba P, Awori P, et al. Relationships between infection with Plasmodium falciparum during pregnancy, measures of placental malaria, and adverse birth outcomes. Malar J. 2017;16(1):400.
Ndeserua R, Juma A, Mosha D, Chilongola J. Risk factors for placental malaria and associated adverse pregnancy outcomes in Rufiji, Tanzania: a hospital based cross sectional study. Afr Health Sci. 2015;15(3):810–8.
Kelly-Hope LA, McKenzie FE. The multiplicity of malaria transmission: a review of entomological inoculation rate measurements and methods across sub-Saharan Africa. Malar J. 2009;8(1):19.
Haldar K, Mohandas N. Malaria, erythrocytic infection, and anemia. Hematology. 2009;2009(1):87–93.
Obaldia N 3rd, Meibalan E, Sa JM, Ma S, Clark MA, Mejia P, et al. Bone Marrow Is a Major Parasite Reservoir in Plasmodium vivax Infection. mBio. 2018;9(3):e00625–18.
Doolan DL, Dobaño C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22(1):13–36.
Brabin BJ, Hakimi M, Pelletier D. An analysis of anemia and pregnancy-related maternal mortality. J Nutr. 2001; 131(2S-2):604S-14S; discussion 14S-15S.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet (London, England). 2013;382(9890):427–51.
Workicho A, Belachew T, Ghosh S, Kershaw M, Lachat C, Kolsteren P. Burden and determinants of undernutrition among young pregnant women in Ethiopia. Matern Child Nutr. 2019; 15(3):e12751-e.
Ampiah MKM, Kovey JJ, Apprey C, Annan RA. Comparative analysis of trends and determinants of anaemia between adult and teenage pregnant women in two rural districts of Ghana. BMC Public Health. 2019;19(1):1379.
Tandu-Umba B, Mbangama AM. Association of maternal anemia with other risk factors in occurrence of Great obstetrical syndromes at university clinics, Kinshasa, DR Congo. BMC Pregnancy Childbirth. 2015;15:183.
Unger HW, Ashorn P, Cates JE, Dewey KG, Rogerson SJ. Undernutrition and malaria in pregnancy - a dangerous dyad? BMC Med. 2016;14(1):142.
Katona P, Katona-Apte J. The interaction between nutrition and infection. Clin Infect Dis. 2008;46(10):1582–8.
Raiten DJ, Sakr Ashour FA, Ross AC, Meydani SN, Dawson HD, Stephensen CB, et al. Inflammation and Nutritional Science for Programs/Policies and Interpretation of Research Evidence (INSPIRE). J Nutr. 2015;145(5):1039s–108s.
Gies S, Diallo S, Roberts SA, Kazienga A, Powney M, Brabin L, et al. Effects of Weekly Iron and Folic Acid Supplements on Malaria Risk in Nulliparous Women in Burkina Faso: A Periconceptional, Double-Blind, Randomized Controlled Noninferiority Trial. J Infect Dis. 2018;218(7):1099–109.
Brabin B, Gies S, Roberts SA, Diallo S, Lompo OM, Kazienga A, et al. Excess risk of preterm birth with periconceptional iron supplementation in a malaria endemic area: analysis of secondary data on birth outcomes in a double blind randomized controlled safety trial in Burkina Faso. Malar J. 2019;18(1):161.
Menendez C. Malaria During Pregnancy. Current Molecular Medicine. 2006;6(2):269–73.
WWARN Artemisinin based Combination Therapy (ACT) Africa Baseline Study Group. Clinical determinants of early parasitological response to ACTs in African patients with uncomplicated falciparum malaria: a literature review and meta-analysis of individual patient data. BMC Med. 2015; 13(1):212.
Medzhitov R, Schneider DS, Soares MP. Disease tolerance as a defense strategy. Science. 2012;335(6071):936–41.
Galatas B, Bassat Q, Mayor A. Malaria Parasites in the Asymptomatic: Looking for the Hay in the Haystack. Trends Parasitol. 2016;32(4):296–308.
Teo A, Hasang W, Randall LM, Unger HW, Siba PM, Mueller I, et al. Malaria preventive therapy in pregnancy and its potential impact on immunity to malaria in an area of declining transmission. Malar J. 2015;14(1):215.
Tonga C, Kimbi HK, Anchang-Kimbi JK, Nyabeyeu HN, Bissemou ZB, Lehman LG. Malaria risk factors in women on intermittent preventive treatment at delivery and their effects on pregnancy outcome in sanaga-maritime, Cameroon. PLoS One. 2013; 8(6):e65876 PMID 23762446.
Gontie GB, Wolde HF, Baraki AG. Prevalence and associated factors of malaria among pregnant women in Sherkole district, Benishangul Gumuz regional state, West Ethiopia. BMC Infect Dis. 2020;20(1):573.
De Beaudrap P, Turyakira E, White LJ, Nabasumba C, Tumwebaze B, Muehlenbachs A, et al. Impact of malaria during pregnancy on pregnancy outcomes in a Ugandan prospective cohort with intensive malaria screening and prompt treatment. Malar J. 2013;12:139.
Henry M, Florey L, Youll S, Gutman JR. An analysis of country adoption and implementation of the 2012 WHO recommendations for intermittent preventive treatment for pregnant women in sub-Saharan Africa. Malar J. 2018;17(1):364.
Stanisic DI, Moore KA, Baiwog F, Ura A, Clapham C, King CL, et al. Risk factors for malaria and adverse birth outcomes in a prospective cohort of pregnant women resident in a high malaria transmission area of Papua New Guinea. Trans R Soc Trop Med Hyg. 2015;109(5):313–24.
Muehlenbachs A, Fried M, McGready R, Harrington WE, Mutabingwa TK, Nosten F, et al. A novel histological grading scheme for placental malaria applied in areas of high and low malaria transmission. J Infect Dis. 2010;202(10):1608–16.
Walker PG, ter Kuile FO, Garske T, Menendez C, Ghani AC. Estimated risk of placental infection and low birthweight attributable to Plasmodium falciparum malaria in Africa in 2010: a modelling study. The Lancet Global health. 2014;2(8):e460–7.
WHO. WHO policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP). available at: [https://www.who.int/docs/default-source/documents/publications/gmp/iptp-sp-updated-policy-brief-24jan2014.pdf?sfvrsn=d542acbe_2&download=true]. Accessed on 20 August 2020.
Walker PG, Floyd J, Ter Kuile F, Cairns M. Estimated impact on birth weight of scaling up intermittent preventive treatment of malaria in pregnancy given sulphadoxine-pyrimethamine resistance in Africa: A mathematical model. PLoS Med. 2017;14(2):e1002243.
Tahita MC, Tinto H, Erhart A, Kazienga A, Fitzhenry R, VanOvermeir C, et al. Prevalence of the dhfr and dhps Mutations among Pregnant Women in Rural Burkina Faso Five Years after the Introduction of Intermittent Preventive Treatment with Sulfadoxine-Pyrimethamine. PLoS One. 2015;10(9):e0137440.
Cisse M, Awandare GA, Soulama A, Tinto H, Hayette MP, Guiguemdé RT. Recent uptake of intermittent preventive treatment during pregnancy with sulfadoxine-pyrimethamine is associated with increased prevalence of Pfdhfr mutations in Bobo-Dioulasso, Burkina Faso. Malar J. 2017;16(1):38.
Kakuru A, Jagannathan P, Muhindo MK, Natureeba P, Awori P, Nakalembe M, et al. Dihydroartemisinin-piperaquine for the prevention of malaria in pregnancy. N Engl J Med. 2016;374(10):928–39 PMID PM:26962728.
González R, García-Otero L, Pons-Duran C, Marbán-Castro E, Goncé A, Llurba E, et al. Hydroxychloroquine efficacy and safety in preventing SARS-CoV-2 infection and COVID-19 disease severity during pregnancy (COVID-Preg): a structured summary of a study protocol for a randomised placebo controlled trial. Trials. 2020;21(1):607.
Accrombessi M, Yovo E, Cottrell G, Agbota G, Gartner A, Martin-Prevel Y et al. Cohort profile: effect of malaria in early pregnancy on fetal growth in Benin (RECIPAL preconceptional cohort). 2018; 8(1):e019014.
United Nations.. World Population Prospects 2019 volume II: Demographic profiles. available at: [https://population.un.org/wpp/Publications/Files/WPP2019_Volume-II-Demographic-Profiles.pdf]. Accessed on 14 September 2020.
Babalola OJ, Sambo MN, Idris SH, Ajayi IO, Ajumobi O, Nguku P. Factors associated with utilization of LLINs among women of child-bearing age in Igabi, Kaduna State, Nigeria. Malar J. 2019;18(1):412.
Acknowledgments
We thank the participants of the PREGACT study, and the field team in Burkina Faso, and Université catholique de Louvain in Belgium for providing a Ph.D grant.
Funding
The PREGACT trial was funded by- the European and Developing Countries Clinical Trials Partnership, the Malaria in Pregnancy Consortium granted by the Bill and Melinda Gates Foundation - USA through Liverpool School of Tropical Medicine – UK, the Netherlands-African Partnership for Capacity Development and Clinical Interventions Against Poverty-related diseases (NACCAP) – the Netherlands, the Directorate-General for Development Cooperation (DGDC) – Belgium, and the Medical Research Council (MRC) – UK.
The funding institutions had no role in designing the trial, and in collecting, analyzing, interpreting the data, and in writing the manuscript.
BB is supported by a Ph.D. grant from UCLouvain and by a grant from ARES-Belgian Universities-cooperation with developing countries-Action PRD 2017 in Burkina Faso.
Author information
Authors and Affiliations
Contributions
UDA and JPV conceived the PREGACT trial. ZSH, TMC, VI, and HT collected the data; RR oversaw the conduct, monitoring, and data management of the PREGACT trial; BB and RA suggested the idea of the study. BB conducted the analyses and drafted the manuscript under the supervision of RA. All authors reviewed the manuscript and approved the version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The PREGACT study received approvals from- the Institutional Review Board of the Institute of Tropical Medicine, Antwerp, Belgium; the Ethics committee of the University Hospital, Antwerp, Belgium; the Institutional Ethics committee of Centre Muraz and the Ethics committee of the Ministry of Health, Burkina Faso.
All the participants provided a written informed consent form before being enrolled in the study. Datasets were anonymized.
Consent for publication
Not applicable
Competing interests
Authors declare having no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bihoun, B., Zango, S.H., Traoré-Coulibaly, M. et al. Age-modified factors associated with placental malaria in rural Burkina Faso. BMC Pregnancy Childbirth 22, 248 (2022). https://doi.org/10.1186/s12884-022-04568-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04568-4