Abstract
Background
Diagnosis and monitoring of leptomeningeal malignancy remain challenging, and are usually based on neurological, radiological, cerebrospinal fluid (CSF) and pathological findings. This study aimed to investigate the diagnostic performance of CSF metagenomic next-generation sequencing (mNGS) and chromosome copy number variations (CNVs) analysis in the detection of leptomeningeal malignancy.
Methods
Of the 51 patients included in the study, 34 patients were diagnosed with leptomeningeal malignancies, and 17 patients were diagnosed with central nervous system (CNS) inflammatory diseases. The Sayk’s spontaneous cell sedimentation technique was employed for CSF cytology. And a well-designed approach utilizing the CSF mNGS-CNVs technique was explored for early diagnosis of leptomeningeal malignancy.
Results
In the tumor group, 28 patients were positive for CSF cytology, and 24 patients were positive for CSF mNGS-CNVs. Sensitivity and specificity of CSF cytology were 82.35% (95% CI: 66.83-92.61%) and 94.12% (95% CI: 69.24-99.69%). In comparison, sensitivity and specificity of CSF mNGS-CNV were 70.59% (95% CI: 52.33-84.29%) and 100% (95% CI: 77.08-100%). There was no significant difference in diagnostic consistency between CSF cytology and mNGS-CNVs (p = 0.18, kappa = 0.650).
Conclusions
CSF mNGS-CNVs tend to have higher specificity compared with traditional cytology and can be used as a complementary diagnostic method for patients with leptomeningeal malignancies.
Similar content being viewed by others
Background
Leptomeningeal malignancy is a severe condition associated with metastatic solid tumors and hematologic malignancies [1]. The most common tumors involving leptomeninges are lung cancer, breast cancer, lymphoma and leukemia and primary brain tumors such as gliomas, medulloblastomas, and ependymomas [1,2,3]. The presence of leptomeningeal malignancies is frequently associated with exceptional morbidity and mortality [4, 5]. However, diagnosing and effectively managing these conditions pose significant challenges.
Cerebrospinal fluid (CSF) analysis offers valuable diagnostic insights into leptomeningeal lesions. As a conventional morphological test, CSF cytology is instrumental in identifying tumor cells in individuals with leptomeningeal malignancy [6,7,8]. In recent years, metagenomic next-generation sequencing (mNGS) of CSF has emerged as a frontline diagnostic test for patients with meningitis with unknown etiology, enabling the identification of infectious pathogens. The majority of sequences obtained from mNGS correspond to human DNA, providing clinicians with an opportunity to utilize this wealth of sequencing information [9, 10].
Copy number variations (CNVs) refer to the deletion or amplification of DNA fragments at least 1 kb in length compared to the reference genome [11, 12]. Previous studies have highlighted the association between CNVs and tumor risk [13,14,15]. The diverse range of CNVs, in terms of their number and genomic distribution, reflects early genomic variations during tumorigenesis. Moreover, these variations may be linked to selection pressures on the tumor genome, representing distinct evolutionary processes and pathways within the tumor genome [16, 17].
Tumor cells release DNA fragments that circulate in CSF [18, 19]. Leveraging CSF sequencing analysis allows for more robust tumor diagnosis, particularly in cases with clinical suspicion but insufficient evidence. In this study, we employed mNGS-CNVs to investigate pathogenic microorganisms and structural variants within the human genome using CSF samples. Our aim was to explore an integrated diagnostic approach for leptomeningeal malignancy and CNS inflammatory diseases based on a single CSF mNGS-CNVs procedure. We assessed the utility of mNGS-CNVs in characterizing and monitoring leptomeningeal malignancy while comparing its performance with CSF cytology. The findings of this study provide valuable diagnostic references for implementing this technique in clinical practice.
Methods
Patient enrollment
In this prospective cohort study, we collected data from 55 patients in the Department of Neurology, Peking Union Medical College Hospital from March 2022 to February 2023. The inclusion criteria were as follows: (1) clinical or radiological manifestations of meningeal involvement; (2) diagnosis of leptomeningeal malignancy was suspected by clinicians. The exclusion criteria were as follows: (1) contraindications for lumbar puncture; (2) refuse CSF mNGS-CNV test; (3) no definitive diagnosis ultimately. Finally, 4 patients were excluded for no definitive diagnosis, and a total of 51 patients were included for further analysis (Fig. 1). Among these patients, 34 patients were diagnosed with leptomeningeal malignancies (tumor group), and 17 patients were diagnosed with CNS inflammatory diseases (non-tumor group).
Diagnosis of CNS tumors
The diagnosis of CNS tumors was primarily based on the fifth edition of the WHO Classification of Tumors of the Central Nervous System (CNS) guidelines and the Chinese expert consensus on the diagnosis of meningeal carcinomatosis. To establish the diagnosis, the following criteria were considered: (1) Identification of malignant cells through pathological specimens obtained from surgery, biopsy, or CSF cytology; (2) Presence of typical neurological symptoms or signs of the disease, accompanied by MRI enhancement scans indicating the presence of lesions or meningeal enhancement; and (3) Reasonable exclusion of other diseases.
CSF cytology
CSF samples for cytology were collected through lumbar puncture when patients presented with neurological symptoms and leptomeningeal malignancies were suspected. For patients with high suspicion of leptomeningeal malignancies but negative CSF cytology, some underwent lumbar puncture again for cytology test with informed consent. The Sayk’s spontaneous cell sedimentation technique was employed for further analysis. Briefly, 0.5 mL of CSF was placed into the spontaneous sedimentation chamber and stored overnight at 4 °C. The cells precipitated onto the slides. Then, the slides were air-dried and stained with May–Grunwald–Giemsa staining [7]. The morphological characteristics of tumor cells in CSF cytology were assessed, including cell morphology, cytoplasmic features, nucleus characteristics, presence of pigment granules or vacuoles in the cytoplasm, regularly or clustered arrangement of cells, and distinct morphological variations observed in tumor cells from different sources.
Procedure and analysis of mNGS-CNVs
CSF samples for mNGS-CNVs detection were collected from the first lumbar puncture. The collected samples were centrifuged at room temperature, and then stored in the − 80 °C refrigerator. DNA was extracted from CSF using commercially available automated nucleic acid extraction kits. Following the extraction, library preparation was conducted using end-repair, ligation adaptor and other necessary procedures. Subsequently, CSF mNGS DNA sequencing was performed on the Illumina Nextseq platform (Illumina Nextseq CN550) at the V-Medical laboratory in China. To ensure the accuracy of the sequencing data, a rigorous quality control process was implemented.
The obtained sequencing reads were aligned to the human reference genome (hg19) using BWA-MeM software (version: 0.7.17-r1188) to identify both human and nonhuman sequences present in the samples. The nonhuman sequences were subjected to analysis using MiTopia-PAI, a self-built metagenomic data analysis software. This analysis aimed to identify pathogenic microorganisms and recognize clinical pathogenic microorganisms with high confidence.
For CNV analysis, the human sequences within the samples were analyzed using CNVkit (version: 0.9.9). To establish the baseline for CNV analysis, a dataset of tumor-negative samples was used. These baseline samples consisted of CSF samples obtained from patients diagnosed with autoimmune encephalitis. The results of the CNV analysis were visualized by setting the window size and applying a filtering threshold [20]. We determined the possibility of tumor when large CNVs (> 10 Mb) were detected.
Statistical analysis
SPSS 29 (Statistical Package for the Social Sciences, version 29.0, IBM, New York, USA) was applied to the statistical analysis of the data. Data were expressed as proportions for categorical variables. Sensitivity and specificity, along with their corresponding 95% confidence intervals (CIs) of mNGS-CNVs were calculated. McNemar test was performed for statistical analysis. P < 0.05 was used to indicate statistical significance.
Results
Basic information
In total, 51 patients were included in the study (Fig. 1). The baseline characteristics are shown in Table 1. Tumor types in the study were as follows: leptomeningeal metastases of lung cancer (n = 10); leptomeningeal metastases of breast cancer (n = 6); leptomeningeal metastases of leukemia (n = 1); leptomeningeal metastases of gastrointestinal tumors (n = 1); B-cell lymphoma (n = 6); T-cell lymphoma (n = 1); diffuse midline glioma (n = 1); pleomorphic xanthoma astrocytoma(n = 1); rhabdomyosarcoma (n = 1); primitive neuroectodermal tumor (n = 2); spinal tumor (n = 1); primary tumor unknown (n = 3).
CSF pressure (> 180 mmH2O) was increased in 20.59% of the tumor group and 35.29% of the nontumor group. Increased total protein was present in 64.71% of the tumor group and 76.47% of the non-tumor group. In the tumor group, 20 patients completed enhanced MRI examinations, with 19 (95.00%) patients displaying enhanced lesions or meningeal involvement. In the non-tumor group, 7 patients completed MRI, and 6 (85.71%) patients had abnormal signals.
CSF cytology and CNVs analysis
In the tumor group, 28 (82.35%) patients had positive CSF cytology, and representative positive results are presented in Fig. 2. Among the 6 (17.65%) patients with negative cytology, one patient was diagnosed with meningeal carcinomatosis (MC), 3 patients with CNS lymphoma, and 1 patient with a primitive neuroectodermal tumor. Additionally, 24 (70.59%) patients had positive CSF CNV results, and some examples are presented in Fig. 3. The median CNV segment size was 10.5 (range: 1 ~ 49). No CNV segments larger than 10 Mb were detected in the remaining 10 (29.41%) patients with negative CNV results. Among those with negative CNV results, 3 patients were diagnosed with MC, 6 patients with CNS lymphoma, and 1 patient with glioma (Table 2).
In the non-tumor group, the CSF cytology of 16 (94.12%) patients showed inflammatory changes, and the cytology of 1 (5.89%) patient reported atypical-abnormal cells, which were considered tumor cells. All 17 patients exhibited negative CSF CNV results.
CSF cytology of leptomeningeal malignancies. CSF cytology of tumor cells (spontaneous cell sedimentation technique, May-Gruwald-Giemsa staining ×200). (A) Patient 8: leptomeningeal metastases of breast cancer. (B) Patient 23: diffuse midline glioma. (C) Patient 30: CNS B-cell lymphoma. (D) Patient 34: rhabdomyosarcoma
CSF CNV analysis in patients with leptomeningeal malignancies. CNV segments in patients with leptomeningeal malignancies. (A) Patient 8: leptomeningeal metastases of breast cancer, 32 CNV segments. (B) Patient 23: diffuse midline glioma, 12 CNV segments. (C) Patient 30: CNS B-cell lymphoma, 5 CNV segments. (D) Patient 34: rhabdomyosarcoma, 5 CNV segments
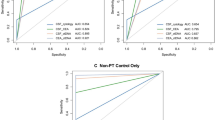
Sensitivity and specificity
The results demonstrated that for the diagnosis of leptomeningeal malignancy, CSF cytology exhibited a sensitivity of 82.35% (95% CI: 66.83-92.61%) and specificity of 94.12% (95% CI: 69.24-99.69%). Similarly, CSF mNGS-CNVs displayed a sensitivity of 70.59% (95% CI: 52.33-84.29%) and a specificity of 100% (95% CI: 77.08-100%). Moreover, two patients exhibited CNV segments larger than 3 Mb but smaller than 10 Mb. Adjusting the CNV length reference to 3 Mb resulted in a sensitivity of 76.47% (95% CI: 58.43-88.62%) for CSF mNGS-CNVs. Importantly, no significant difference in diagnostic consistency was observed between CSF cytology and mNGS-CNVs (p = 0.18, kappa = 0.650).
Discussion
In this study, we applied CSF mNGS-CNVs analysis and cytological examinations in a cohort of 51 patients diagnosed with leptomeningeal malignancies and CNS inflammatory diseases. The main findings are summarized as follows. Firstly, we established a well-designed approach for the analysis of the CSF mNGS-CNV technique, which detected both neoplasms and pathogenic microorganisms and provided results in hours to facilitate the earlier diagnosis of leptomeningeal malignancies. Secondly, there was no significant difference of diagnostic consistency between CSF cytology and mNGS-CNVs, which suggested that mNGS-CNVs may be considered as an auxiliary examination in hospitals that do not have the conditions to undertake CSF cytological testing. Lastly, mNGS-CNVs does not require intact CSF cells and can provide highly specific results without the need for repeated lumbar puncture.
The timely diagnosis of leptomeningeal malignancy remains challenging, often requiring prompt CSF cytology, tumor tissue pathology, gene mutation detection, and other auxiliary examinations [21,22,23]. While cytology is a classical method in the diagnosis of leptomeningeal malignancy, its diagnostic accuracy may vary and heavily relies on experienced cytopathologists [22,23,24]. Moreover, the positive rate of cytology from a single lumbar puncture has its limitations. In certain centers, standardized procedures for CSF cytology may not be uniformly implemented. Therefore, to explore more suggestive diagnostic techniques that offer greater diagnostic accuracy for leptomeningeal malignancies is meaningful.
Previous studies have demonstrated that gene profiles in CSF can provide valuable insights into CNS tumors [19, 25, 26]. Recently, researchers have found that mNGS of human peripheral blood, bronchoalveolar lavage fluid, CSF or other body fluids provide clues on distinguishing malignancies [27,28,29] from infectious/inflammatory diseases [30,31,32]. This approach was mainly based on CNV analysis, which exhibits relatively high specificity. Gu et al. [10] reported that the mNGS-CNVs had a sensitivity of 71% and a specificity of 100% in detecting CNS malignant tumors by using the earliest CSF specimens. Fifty-five patients of CNS malignant neoplasms were included in the study, while 65.5% of them were diagnosed with lymphomas, which may not seem to be comprehensive enough to cover various neoplasms’ CNVs and cytological characteristics.
In our study, moderate sensitivity and high specificity of the CSF mNGS-CNVs technique compared with cytology provide evidence for its feasibility and potential as an auxiliary method in the diagnosis of leptomeningeal malignancies. Additionally, CSF mNGS testing contains information of suspicious microorganisms for differential diagnosis of infectious encephalitis or meningitis. In addition, mNGS-CNVs analysis require smaller CSF volume and do not rely on the integrity of cells and repeated lumber punctures.
However, CNV analysis can be affected by some confounding factors, such as the complexity of tumor samples and the detection thresholds. Challenges from the complex tumor samples including tumor types, the aneuploidy of the genome and tumor fraction [33]. Different tumor types have different CNV patterns [34, 35]. For example, the number of CNV was higher in aggressive tumors than indolent ones [36]. We noticed that large CNVs of CNS lymphoma was rarely detected in our study. Given this perspective, we speculated that these tumors may harbor lower fractions of circulating tumor DNA or less whole genome doubling events. Besides, CNS lymphoma is difficult to diagnose relying on single auxiliary test [23], and reasonable combination of CSF cytology, CNVs, flow cytometry and other diagnostic tests to establish the diagnosis is recommended.
On the other hand, there is no consensus on the setting of criteria for CNV detection threshold. In our study, the sensitivity of CSF mNGS-CNVs was 70.59% when using 10 Mb as large CNVs threshold, which is similar to Gu et al. [10] with the same threshold. In previous studies, region of 3 Mb in the human genome contains one gene or only a few genes, and may be detected in the tumor genetic variations [37]. When adjusting the cutoff value to 3 Mb, the diagnostic sensitivity of mNGS-CNVs increased to 76.47% in this study. This phenomenon may have some implications for future research.
Conclusions
Accurate detection of CNVs in the human genome and subsequent analysis of the biological implications of these variations hold significant importance for tumor diagnosis. Overall, our study employed a well-designed and comprehensive approach to analyze CSF samples, which can contribute to the differential diagnosis of CNS malignancies and infectious diseases. Nevertheless, further research with larger sample sizes is warranted to validate and expand upon these findings, ensuring a more robust understanding of the diagnostic capabilities of mNGS-CNVs analysis in various types of CNS tumors.
Data availability
The datasets generated during the current study has been uploaded to CNCB database, https://www.cncb.ac.cn/ (Accession: PRJCA023198).
References
Wang N, Bertalan MS, Brastianos PK. Leptomeningeal metastasis from systemic cancer: review and update on management. Cancer. 2018;124(1):21–35.
Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. 1999;25(2):103–19.
Walker DA, Meijer L, Coyle B, Halsey C. Leptomeningeal malignancy of childhood: sharing learning between childhood leukaemia and brain tumour trials. Lancet Child Adolesc Health. 2020;4(3):242–50.
Miller KD, Ostrom QT, Kruchko C, Patil N, Tihan T, Cioffi G, et al. Brain and other central nervous system tumor statistics, 2021. CA Cancer J Clin. 2021;71(5):381–406.
Cohen AR. Brain tumors in children. N Engl J Med. 2022;386(20):1922–31.
Glass JP, Melamed M, Chernik NL, Posner JB. Malignant cells in cerebrospinal fluid (CSF): the meaning of a positive CSF cytology. Neurology. 1979;29(10):1369–75.
Fan S, Ren H, Wang C, Guan H. Continuing Use of Sayk’s spontaneous cell sedimentation technique for Cerebrospinal Fluid Cytology in China. Eur Neurol. 2018;79(1–2):76–8.
Chamberlain M, Junck L, Brandsma D, Soffietti R, Rudà R, Raizer J, et al. Leptomeningeal metastases: a RANO proposal for response criteria. Neuro Oncol. 2017;19(4):484–92.
Gu W, Miller S, Chiu CY. Clinical metagenomic next-generation sequencing for Pathogen Detection. Annu Rev Pathol. 2019;14:319–38.
Gu W, Rauschecker AM, Hsu E, Zorn KC, Sucu Y, Federman S, et al. Detection of Neoplasms by Metagenomic Next-Generation sequencing of Cerebrospinal Fluid. JAMA Neurol. 2021;78(11):1355–66.
Redon R, Ishikawa S, Fitch KR, Feuk L, Perry GH, Andrews TD, et al. Global variation in copy number in the human genome. Nature. 2006;444(7118):444–54.
Freeman JL, Perry GH, Feuk L, Redon R, McCarroll SA, Altshuler DM, et al. Copy number variation: new insights in genome diversity. Genome Res. 2006;16(8):949–61.
Miller AM, Shah RH, Pentsova EI, Pourmaleki M, Briggs S, Distefano N, et al. Tracking tumour evolution in glioma through liquid biopsies of cerebrospinal fluid. Nature. 2019;565(7741):654–8.
Pereira B, Chin SF, Rueda OM, Vollan HK, Provenzano E, Bardwell HA, et al. The somatic mutation profiles of 2,433 breast cancers refines their genomic and transcriptomic landscapes. Nat Commun. 2016;7:11479.
DeVries AA, Dennis J, Tyrer JP, Peng PC, Coetzee SG, Reyes AL, et al. Copy number variants are ovarian Cancer risk alleles at known and novel risk loci. J Natl Cancer Inst. 2022;114(11):1533–44.
Beroukhim R, Mermel CH, Porter D, Wei G, Raychaudhuri S, Donovan J, et al. The landscape of somatic copy-number alteration across human cancers. Nature. 2010;463(7283):899–905.
Negrini S, Gorgoulis VG, Halazonetis TD. Genomic instability–an evolving hallmark of cancer. Nat Rev Mol Cell Biol. 2010;11(3):220–8.
Orzan F, De Bacco F, Lazzarini E, Crisafulli G, Gasparini A, Dipasquale A, et al. Liquid Biopsy of Cerebrospinal Fluid enables selective profiling of Glioma Molecular subtypes at First Clinical Presentation. Clin Cancer Res. 2023;29(7):1252–66.
Pentsova EI, Shah RH, Tang J, Boire A, You D, Briggs S, et al. Evaluating Cancer of the Central Nervous System through Next-Generation sequencing of Cerebrospinal Fluid. J Clin Oncol. 2016;34(20):2404–15.
Talevich E, Shain AH, Botton T, Bastian BC, CNVkit. Genome-wide Copy Number Detection and visualization from targeted DNA sequencing. PLoS Comput Biol. 2016;12(4):e1004873.
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the Central Nervous System: a summary. Neuro Oncol. 2021;23(8):1231–51.
Ozcan G, Singh M, Vredenburgh JJ. Leptomeningeal Metastasis from Non-small Cell Lung Cancer and Current Landscape of treatments. Clin Cancer Res. 2023;29(1):11–29.
Scott BJ, Douglas VC, Tihan T, Rubenstein JL, Josephson SA. A systematic approach to the diagnosis of suspected central nervous system lymphoma. JAMA Neurol. 2013;70(3):311–9.
Pentheroudakis G, Pavlidis N. Management of leptomeningeal malignancy. Expert Opin Pharmacother. 2005;6(7):1115–25.
Li YS, Jiang BY, Yang JJ, Zhang XC, Zhang Z, Ye JY, et al. Unique genetic profiles from cerebrospinal fluid cell-free DNA in leptomeningeal metastases of EGFR-mutant non-small-cell lung cancer: a new medium of liquid biopsy. Ann Oncol. 2018;29(4):945–52.
De Mattos-Arruda L, Mayor R, Ng CKY, Weigelt B, Martínez-Ricarte F, Torrejon D, et al. Cerebrospinal fluid-derived circulating tumour DNA better represents the genomic alterations of brain tumours than plasma. Nat Commun. 2015;6:8839.
Guan H, Shen A, Lv X, Yang X, Ren H, Zhao Y, et al. Detection of virus in CSF from the cases with meningoencephalitis by next-generation sequencing. J Neurovirol. 2016;22(2):240–5.
Fan S, Ren H, Wei Y, Mao C, Ma Z, Zhang L, et al. Next-generation sequencing of the cerebrospinal fluid in the diagnosis of neurobrucellosis. Int J Infect Dis. 2018;67:20–4.
Wang S, Chen Y, Wang D, Wu Y, Zhao D, Zhang J, et al. The feasibility of Metagenomic Next-Generation sequencing to identify pathogens causing tuberculous meningitis in Cerebrospinal Fluid. Front Microbiol. 2019;10:1993.
Su J, Han X, Xu X, Ding W, Li M, Wang W, et al. Simultaneous Detection of Pathogens and Tumors in patients with suspected infections by Next-Generation sequencing. Front Cell Infect Microbiol. 2022;12:892087.
Lin P, Chen Y, Xu J, Huang X, Wen W, Zhang L, et al. A multicenter-retrospective cohort study of chromosome instability in lung cancer: clinical characteristics and prognosis of patients harboring chromosomal instability detected by metagenomic next-generation sequencing. J Thorac Dis. 2023;15(1):112–22.
Gu W, Talevich E, Hsu E, Qi Z, Urisman A, Federman S, et al. Detection of cryptogenic malignancies from metagenomic whole genome sequencing of body fluids. Genome Med. 2021;13(1):98.
Pagès M, Rotem D, Gydush G, Reed S, Rhoades J, Ha G, et al. Liquid biopsy detection of genomic alterations in pediatric brain tumors from cell-free DNA in peripheral blood, CSF, and urine. Neuro Oncol. 2022;24(8):1352–63.
Steele CD, Abbasi A, Islam SMA, Bowes AL, Khandekar A, Haase K, et al. Signatures of copy number alterations in human cancer. Nature. 2022;606(7916):984–91.
Taylor AM, Shih J, Ha G, Gao GF, Zhang X, Berger AC, et al. Genomic and functional approaches to understanding Cancer Aneuploidy. Cancer Cell. 2018;33(4):676–e893.
Kogure Y, Kameda T, Koya J, Yoshimitsu M, Nosaka K, Yasunaga JI, et al. Whole-genome landscape of adult T-cell leukemia/lymphoma. Blood. 2022;139(7):967–82.
Krijgsman O, Carvalho B, Meijer GA, Steenbergen RD, Ylstra B. Focal chromosomal copy number aberrations in cancer-needles in a genome haystack. Biochim Biophys Acta. 2014;1843(11):2698–704.
Acknowledgements
The authors appreciate the patients and their families for their participation in this study.
Funding
This study was funded by National High Level Hospital Clinical Research Funding (2022-PUMCH-B-120).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Le Zhang, Kechi Fang, Haitao Ren, Siyuan Fan, Jing Wang and Hongzhi Guan. The first draft of the manuscript was written by Le Zhang and Kechi Fang, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Peking Union Medical College Hospital (ZS-3588). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, L., Fang, K., Ren, H. et al. Comparison of the diagnostic significance of cerebrospinal fluid metagenomic next-generation sequencing copy number variation analysis and cytology in leptomeningeal malignancy. BMC Neurol 24, 223 (2024). https://doi.org/10.1186/s12883-024-03655-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03655-7