Abstract
Background
Patients with poor-grade aneurysmal subarachnoid hemorrhage (aSAH) often receive delayed or no aneurysm treatment, although recent studies suggest that functional outcome following early aneurysm treatment has improved. We aimed to systematically review and meta-analyze early predictors of functional outcome in poor-grade aSAH patients.
Methods
We included studies investigating the association of early predictors and functional outcome in adult patients with confirmed poor-grade aSAH, defined as World Federation of Neurological Surgeons (WFNS) grade or Hunt and Hess (H–H) grade IV-V. Studies had to use multivariable regression analysis to estimate independent predictor effects of favorable functional outcome measured with the Glasgow Outcome Scale or modified Rankin Scale. We calculated pooled adjusted odds ratios (aOR) and 95% confidence intervals (CI) with random effects models.
Results
We included 27 studies with 3287 patients. The likelihood of favorable outcome increased with WFNS grade or H–H grade IV versus V (aOR 2.9, 95% CI 1.9–4.3), presence of clinical improvement before aneurysm treatment (aOR 3.3, 95% CI 2.0–5.3), and intact pupillary light reflex (aOR 2.9, 95% CI 1.6–5.1), and decreased with older age (aOR 0.7, 95% CI 0.5–1.0, per decade), increasing modified Fisher grade (aOR 0.4, 95% CI 0.3–0.5, per grade), and presence of intracerebral hematoma on admission imaging (aOR 0.4, 95% CI 0.2–0.8).
Conclusions
We present a summary of early predictors of functional outcome in poor-grade aSAH patients that can help to discriminate between patients with favorable and with unfavorable prognosis and may aid in selecting patients for early aneurysm treatment.
Similar content being viewed by others
Background
Aneurysmal subarachnoid hemorrhage (aSAH) is a severe type of stroke that is associated with high morbidity and mortality [1, 2]. The clinical severity of aSAH is classified with the World Federation of Neurological Surgeons grade (WFNS) or Hunt and Hess grade (H–H), with a higher clinical grade indicating poorer prognosis. Patients with WFNS grade IV-V or H–H grade IV-V account for 18–24% of the SAH population and are referred to as “poor-grade patients” [3].
In agreement with current guidelines [4, 5], the majority of aSAH patients are being treated within 24 h [6]. Aneurysm treatment in poor-grade patients is often delayed until signs of neurological recovery to avoid providing futile therapies to moribund patients or adding to a high proportion of patients ending up in vegetative or functionally dependent state. However, subjecting poor-grade patients to delayed aneurysm treatment may result in rebleeding and potential loss of life. Especially, because rebleeding occurs most often in the hours following the ictus [7].
There is evidence that outcome following poor-grade aSAH is better than historically assumed. A recent meta-analysis investigating poor-grade patients has indicated that 76% of poor-grade patients may survive and 47% may experience favorable functional outcome [3]. In addition, some studies reported that emergency aneurysm treatment reduced the risk of rebleeding [3, 8] and improved functional outcome [8]. Other studies did not find improved functional outcome with aneurysm treatment within 24 h [3, 9, 10].
In conclusion, there is a need to identify early predictors of functional outcome to improve patient selection for (early) aneurysm treatment to avoid unnecessary rebleeding. Many predictors of functional outcome have been identified, but these have not been confirmed in a poor-grade population. In this systematic review and meta-analysis, we aimed to investigate early predictors of functional outcome in poor-grade aSAH patients.
Methods
We conducted a systematic review and meta-analysis according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (Additional file 1: Table 1) [11]. The study protocol was registered with the International Prospective Register of Systematic Reviews prior to study eligibility selection and was published on 08/13/2020 (available via: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020198603). We developed a comprehensive search strategy with the aid of a medical information specialist to systematically search Embase, Medline, Google Scholar, Web of Science Core Collection, and the Cochrane Central Register of Controlled Trials (Additional file 2: Methods 1). We searched from inception to present date and limited our search to peer-reviewed articles written in English. We conducted our primary search on 05/25/2020 and performed a re-run on 11/30/2020. Potentially eligible articles after title and abstract screening underwent full-text review (Additional file 3: Methods 2). We evaluated the bibliography of eligible studies for additional references. The selection process was recorded using Endnote X9 software.
We performed data extraction with a data extraction form (available upon request). We contacted the corresponding authors in case of missing data. We performed quality assessment with the Quality In Prognosis Studies (QUIPS) tool for quality assessment [12]. Risk of bias (ROB) plots were created with the robvis ROB visualization tool [13]. A detailed description of the criteria to reach the final verdict on ROB is given elsewhere (Additional file 4: Methods 3). We performed the process of study selection, data extraction and quality assessment blinded and independently (J.W.,T.Y.C.). Any disagreements were solved by consulting a third reviewer (B.R. or H.F.L.).
The primary outcome was favorable functional outcome measured with the Glasgow Outcome Scale (GOS) or the modified Rankin Scale (mRS). We did not define favorable outcome or the time of outcome measurement (i.e., some studies defined favorable outcome as a mRS of 0–2 at 6 months, while others defined favorable outcome as a mRS of 0–3 at 1 year).
We summarized study characteristics and reported them as means with standard deviations or medians with interquartile ranges. We performed a systematic review of early predictors of functional outcome. Furthermore, for predictors which were adequately reported and uniformly defined in multiple studies, we performed a meta-analysis and calculated pooled adjusted odds ratios (aOR) and 95% confidence intervals (CI) with random effects models. The results of the meta-analysis were described with Forest plots. When multiple studies reported results based on the same study population, we included the study with the largest sample size [14,15,16,17,18,19,20]. We accounted for heterogeneity in the study design by performing post-hoc subgroup analyses stratifying for length of follow-up, for studies with a favorable outcome definition mRS 0–2 or GOS 4–5, and for studies including patients who have received aneurysm treatment and studies including patients who have not received aneurysm treatment. We defined early follow-up as follow-up up to six months and late follow-up as beyond six months after SAH. We assessed between-study heterogeneity with Higgin’s & Thompson’s I2 and influence plots, and publication bias by analyzing funnel plots and Eggers’ regression test for funnel plot asymmetry. We adjusted for publication bias with the trim-and-fill method [21]. We did not assess publication bias in meta-analyses including less than five studies. To offer a complete overview of available prognostic research, any study that was not eligible for meta-analysis is summarized separately in a descriptive manner. We performed analysis with R software (version 3.6.3, meta package version 5.1.1, metafor package version 3.0.2).
Results
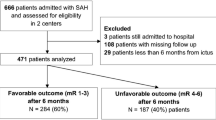
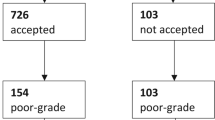
We included 27 studies (n = 3287) that met our selection criteria in our review (Additional file 5: Fig. 1) [14,15,16,17,18,19,20, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. Year of publication ranged from 1996 to 2020 (Additional file 6: Table 2). We did not identify additional studies through bibliographical review.
The median duration of follow up was 6 months (IQR 3–12, Table 1), the median sample size of the multivariable analysis was 104 (IQR 80–154), and 76% of patients received aneurysm treatment. One study did not report on how many patients were provided aneurysm treatment and in one study aneurysm treatment was not provided at all. Most studies had a single center (n = 17, 63%) and retrospective (n = 24, 89%) design.
The studies investigated 82 early predictors of functional outcome with multivariable regression analysis. Taking into account predictor definition, reporting quality, and, if present, categorization we were able to conduct a systematic review of sixteen predictors and meta-analysis of nine predictors. We meta-analyzed age per decade increase, sex, clinical grade on admisssion, pupillary light reflex, clinical improvement before aneurysm treatment, modified Fisher grade, and presence of hydrocephalus, intraventricular hemorrhage (IVH), and intracerebral hematoma (ICH) on admission imaging (Additional file 7: Table 3). Aneurysm size, aneurysm location, Glasgow Coma Scale (GCS), Fisher grade, other concomitant bleeding, brain infarction on admission imaging, and leukocytosis were suitable for systematic review (Additional file 8: Table 4).
We included fifteen studies in the systematic review of the early predictor age. Seven studies were eligible for meta-analysis (n = 865). The likelihood of favorable functional outcome decreased with older age (per decade, pooled aOR 0.7, 95% CI 0.5–1.0, Fig. 1) [24,25,26,27, 31, 38, 39]. We observed moderate funnel plot asymmetry, and after adjusting for publication bias the effect of age was no longer significant (p = 0.10, Additional file 9: Fig. 2A-B). In the eight studies not eligible for meta-analysis older age was often associated with worse functional outcome [14, 15, 19, 29, 35,36,37, 41].
We included six studies in the systematic review investigating the effect of sex on functional outcome. Five studies (n = 427) were eligible for meta-analysis [15, 23, 26, 32, 35]. We did not observe an association between sex and the likelihood of favorable functional outcome (pooled aOR 0.5, 95% CI 0.1–1.4, Fig. 2). One study was not eligible for meta-analysis and found no association between age and functional outcome [41].
We included thirteen studies in the systematic review of clinical grade on the likelihood of favorable functional outcome. Ten studies (n = 1471) were eligible for meta-analysis. The pooled aOR of WFNS grade IV versus V and H–H grade IV versus V was 2.9 (95% CI 1.9–4.3, Fig. 3) [17, 23,24,25, 27, 30, 34, 36, 37, 40]. The effect estimate for clinical grade was similar when including only studies investigating WFNS grade and not H–H grade [17, 24, 34, 36, 40]. In three studies not included in the meta-analysis higher clinical grade was associated with poorer outcome [14, 16, 18].
We included three studies (n = 560, (11%)) investigating the effect of clinical improvement before aneurysm treatment on the likelihood of favorable functional outcome [17, 30, 36]. The pooled aOR was 3.3 (95% CI 2.0–5.3, Fig. 4). Further, we reviewed GCS on admission as an early predictor. Three studies included in the systematic review reported an increased likelihood of favorable functional outcome with increasing GCS [15, 20, 31, 41].
We included three studies (n = 641) in the systematic review and meta-analysis of the effect of intact pupillary light reflex on admission [20, 26, 31]. The pooled aOR was 2.9 (95% CI 1.6–5.1, Fig. 5).
We included seven studies in the systematic review of the effect of presence of ICH on admission imaging on the likelihood of favorable functional outcome. Three studies (n = 355) were eligible for meta-analysis [23, 26, 34]. The pooled aOR was 0.4 (95% CI 0.2–0.8, Fig. 6). The remaining four studies did not report a significant effect of ICH on functional outcome [25, 28, 32, 41].
We included three studies (n = 726) in the meta-analysis of the effect of modified Fisher grade per grade on the likelihood of favorable functional outcome [18, 20, 31]. We found a pooled aOR of 0.4 (95% CI 0.3–0.5, Fig. 7). We included six studies in the systematic review investigating the effect of Fisher grade on functional outcome [19, 23, 25, 36, 37, 40, 41]. Three studies reported a significant association of higher Fisher grade with functional outcome.
We included five studies in the systematic review of the effect of presence of hydrocephalus before aneurysm treatment on functional outcome. Three studies (n = 321) were eligible for meta-analysis [23, 27, 39]. The pooled aOR was 1.0 (95% CI 0.3–2.7, Fig. 8). Two studies were not eligible for meta-analysis. Neither found a significant association with functional outcome [29, 40].
We included seven studies in the systematic review of the effect of presence of IVH on admission imaging on the likelihood of favorable functional outcome. Three studies were eligible for meta-analysis (n = 272) [16, 26, 41]. The pooled aOR was 1.8 (95% CI 0.3–12.8, Fig. 9). Four studies were not eligible for meta-analysis and analyzed in with systematic review. Two found an association of IVH with functional outcome [30, 32, 40, 41].
Additionally, we conducted a systematic review of aneurysm size, aneurysm location, presence of brain infarction on admission imaging, leukocytosis, and other concomitant bleeding in relation to function outcome (Additional file 8: Table 4).
We performed subgroup analyses for length of follow-up, for favorable outcome definition, and for studies including only patients that received aneurysm treatment for the predictors age, sex, and clinical grade, which showed similar results as the main analysis. The overall risk of bias as assessed with the QUIPS ROB tool for prognostic studies was high (Fig. 10, and Additional file 10: Fig. 3).
Discussion
We systematically reviewed and meta-analyzed early predictors of functional outcome in poor-grade aSAH patients. In agreement with previous research, we confirmed that age, clinical grade, pupillary light reflex, presence of ICH, and modified Fisher grade were predictors of functional outcome [42,43,44,45,46,47,48]. In addition, we summarized available prognostic research of less well-known early predictors. In contrast to previous research, we did not find an association of functional outcome and sex, hydrocephalus, and IVH, and found little evidence of aneurysm size as an early predictor in this population [42,43,44,45, 47].
Overall, we found that higher level of consciousness and clinical improvement indicated better patient prognosis. Reassessing clinical condition after initial neurological resuscitation obtains more reliable prognostic estimates and may mandate re-evaluation of clinical management [49].
Not surprisingly, aSAH patients with intact pupillary light reflexes on admission had a greater likelihood of favorable functional outcome. However, seven of the included studies in the present systematic review excluded patients with absent brainstem reflexes [18, 24, 26, 30, 33, 38, 41]. A previous study advocated to add signs of brain stem herniation such as absent brainstem reflexes to the WFNS grade to improve prognosis prediction among grade V patients [50].
Many studies considered imaging-characteristics as predictors of functional outcome, with one-third of predictors evaluated being imaging-based. The widespread availability of imaging at baseline makes imaging-characteristics interesting for predicting prognosis. We observed that many studies used categorization and dichotomization, and applied different definitions for equal predictors. This has made the results of these studies unsuited for further meta-analysis. We advocate to adhere to the common data elements for SAH and unruptured intracranial aneurysms [51], and to limit categorization and dichotomization to enhance reproducibility and avoid losing valuable information within the data.
Nonetheless, we found that presence of ICH and modified Fisher grade were significantly associated with functional outcome. Presence of ICH was previously reported as a predictor of unfavorable outcome [52]. Prognosis of these patients may be intertwined with rapid hematoma evacuation. Denying surgical treatment because of poor expected outcome could lead to a self-fulfilling prophecy. Although, we found no association of other imaging-characteristics with functional outcome, due to lacking high-quality evidence, their prognostic value remains undetermined.
This study is strengthened by the comprehensive summary of prognostic research of early predictors of functional outcome in a poor-grade aSAH population. We confirmed predictors of outcome in a poor-grade population, and showed that there is an absence of high-quality prognostic evidence. Another strength is to limit study eligibility to those that performed multivariable analyses. This has added to the validity of the results.
Several limitations must be considered while interpreting this study. Methodological variation between the included studies led to considerable heterogeneity. For example, there was no uniform definition of favorable outcome in the included studies. This has made interpretation of the results of the meta-analysis more complicated and could have led to biased results.
Also, specific patient-characteristics may have guided the decision whether or not to pursue aggressive management. This may affect functional outcome and could have affected estimated predictor effects. However, most studies applied an aggressive treatment policy. This is illustrated by the high percentage of patients (76%) that received aneurysm treatment. Subgroup analysis for studies with a favorable outcome definition of mRS 0–2 and GOS 4–5, and for studies including exclusively patients who received aneurysm treatment did not indicate different findings than in the main analysis.
The results of our study could be affected by publication and reporting bias. When present, we aimed to adjust for publication bias. Not all studies reported non-significant aORs and CIs leading to a possible overestimation of the effect size estimates. Attempts to request the authors to provide this information were not successful.
Ultimately, the quality of the included studies determine the reliability of the results. Most studies had a small sample size and a high ROB. Because of this, the results have to be interpreted with caution.
Nevertheless, in this study, we obtained more valid and more precise estimates of predictors of functional outcome in a poor-grade aSAH population and summarized prognostic research for future prospective research. To date, no other intervention than aneurysm treatment can effectively minimize the risk of aneurysmal rebleeding. Poor-grade patients often receive delayed aneurysm treatment. Poor-grade patients that are most likely to achieve favorable outcome may be candidates for early aneurysm treatment. We argue that the early predictors of functional outcome that we present in this study could aid patient selection to avoid unnecessary rebleeding. Improving patient selection for early aneurysm treatment can both benefit patient outcome and ensure optimal allocation of limited health care resources.
Nonetheless, it should be noted that average improved functional outcome does not equal individual patient benefit. Individual treatment (strategy) effects can vary within the population. To provide absolute estimates of individual treatment benefit we have to model for heterogeneity of treatment effects which can only be performed using randomized data [53]. First, larger prospective observational research is needed to confirm these predictors of functional outcome in a poor-grade aSAH population. Next steps would be to implement these predictors of outcome in a prediction rule for clinical practice to provide estimates of expected benefit of early versus delayed aneurysm treatment in terms of functional outcome.
Conclusions
We found that WFNS and H–H grade IV as opposed to V on admission, lower modified Fisher grade, the absence of intracerebral hematoma, intact pupillary light reflexes, and clinical improvement before aneurysm treatment were predictors of favorable functional outcome in poor-grade aSAH patients. These predictors can help discriminate between poor-grade aSAH patients with favorable and with unfavorable prognosis and may aid in selecting patients for early aneurysm treatment. The present study can serve as a stepping-stone for future decision modeling research focusing on selecting poor-grade aSAH patients for early aneurysm treatment.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its additional files.
Abbreviations
- aOR:
-
Adjusted odds ratio
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- CI:
-
Confidence interval
- GCS:
-
Glasgow Coma Scale
- GOS:
-
Glasgow Outcome Scale
- H–H:
-
Hunt and Hess
- ICH:
-
Intracerebral hemorrhage
- IVH:
-
Intraventricular hemorrhage
- IQR:
-
Interquartile range
- mRS:
-
modified Rankin Scale
- QUIPS:
-
Quality In Prognosis Studies
- ROB:
-
Risk of bias
- WFNS:
-
World Federation of Neurological Surgeons
References
Rinkel GJ, Algra A. Long-term outcomes of patients with aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2011;10(4):349–56.
Rinkel GJ, Gijn J. Subarachnoid hemorrhage. Neurology. 1994;44(1):191–2.
Han Y, Ye F, Long X, Li A, Xu H, Zou L, et al. Ultra-Early Treatment for Poor-Grade Aneurysmal Subarachnoid Hemorrhage: A Systematic Review and Meta-Analysis. World Neurosurg. 2018;115:e160–71.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711–37.
Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G, et al. European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 2013;35(2):93–112.
de Winkel J, van der Jagt M, Lingsma HF, Roozenbeek B, Calvillo E, Chou SH, et al. International Practice Variability in Treatment of Aneurysmal Subarachnoid Hemorrhage. J Clin Med. 2021;10(4):762.
Germans MR, Coert BA, Vandertop WP, Verbaan D. Time intervals from subarachnoid hemorrhage to rebleed. J Neurol. 2014;261(7):1425–31.
Park J, Woo H, Kang DH, Kim YS, Kim MY, Shin IH, et al. Formal protocol for emergency treatment of ruptured intracranial aneurysms to reduce in-hospital rebleeding and improve clinical outcomes. J Neurosurg. 2015;122(2):383–91.
Rawal S, Alcaide-Leon P, Macdonald RL, Rinkel GJ, Victor JC, Krings T, et al. Meta-analysis of timing of endovascular aneurysm treatment in subarachnoid haemorrhage: inconsistent results of early treatment within 1 day. J Neurol Neurosurg Psychiatry. 2017;88(3):241–8.
Oudshoorn SC, Rinkel GJ, Molyneux AJ, Kerr RS, Dorhout Mees SM, Backes D, et al. Aneurysm treatment <24 versus 24–72 h after subarachnoid hemorrhage. Neurocrit Care. 2014;21(1):4–13.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61.
Mocco J, Ransom ER, Komotar RJ, Schmidt JM, Sciacca RR, Mayer SA, et al. Preoperative prediction of long-term outcome in poor-grade aneurysmal subarachnoid hemorrhage. Neurosurgery. 2006;59(3):529–38 discussion -38.
Starke RM, Komotar RJ, Kim GH, Kellner CP, Otten ML, Hahn DK, et al. Evaluation of a revised Glasgow Coma Score scale in predicting long-term outcome of poor grade aneurysmal subarachnoid hemorrhage patients. J Clin Neurosci. 2009;16(7):894–9.
Zhao B, Tan X, Zhao Y, Cao Y, Wu J, Zhong M, et al. Variation in Patient Characteristics and Outcomes Between Early and Delayed Surgery in Poor-Grade Aneurysmal Subarachnoid Hemorrhage. Neurosurgery. 2016;78(2):224–31.
Zhao B, Yang H, Zheng K, Li Z, Xiong Y, Tan X, et al. Preoperative and postoperative predictors of long-Term outcome after endovascular treatment of poor-grade aneurysmal subarachnoid hemorrhage. J Neurosurg. 2017;126(6):1764–71.
Zhao B, Zhao Y, Tan X, Cao Y, Wu J, Zhong M, et al. Factors and outcomes associated with ultra-early surgery for poor-grade aneurysmal subarachnoid haemorrhage: A multicentre retrospective analysis. BMJ Open. 2015;5(4):e007410.
Zheng K, Zhao B, Tan XX, Li ZQ, Xiong Y, Zhong M, et al. Comparison of Aggressive Surgical Treatment and Palliative Treatment in Elderly Patients with Poor-Grade Intracranial Aneurysmal Subarachnoid Hemorrhage. BioMed Res Int. 2018;2018:5818937.
Zheng K, Zhong M, Zhao B, Chen SY, Tan XX, Li ZQ, et al. Poor-grade aneurysmal subarachnoid hemorrhage: Risk factors affecting clinical outcomes in intracranial aneurysm patients in a multi-center study. Front Neurol. 2019;10:123.
Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Anqi X, Ruiqi C, Yanming R, Chao Y. Elevated hemoglobin is associated with poor prognosis in Tibetans with poor-grade aneurysmal subarachnoid hemorrhage after clipping: A Retrospective Case-Control Study. Neurochirurgie. 2019;65(6):365–9.
Das KK, Singh S, Sharma P, Mehrotra A, Bhaisora K, Sardhara J, et al. Results of Proactive Surgical Clipping in Poor-Grade Aneurysmal Subarachnoid Hemorrhage: Pattern of Recovery and Predictors of Outcome. World Neurosurg. 2017;102:561–70.
Fukuda H, Hayashi K, Moriya T, Nakashita S, Lo BW, Yamagata S. Intrasylvian hematoma caused by ruptured middle cerebral artery aneurysms predicts recovery from poor-grade subarachnoid hemorrhage. J Neurosurg. 2015;123(3):686–92.
Hsieh PC, Wu YM, Wang AY, Chen CC, Chang CH, Chin SC, et al. The venous delay phenomenon in computed tomography angiography: a novel imaging outcome predictor for poor cerebral perfusion after severe aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018;129(4):876–82.
Inamasu J, Nakae S, Ohmi T, Kogame H, Kawazoe Y, Kumai T, et al. The outcomes of early aneurysm repair in World Federation of Neurosurgical Societies grade V subarachnoid haemorrhage patients with emphasis on those presenting with a Glasgow Coma Scale score of 3. J Clin Neurosci. 2016;33:142–7.
Ironside N, Buell TJ, Chen CJ, Kumar JS, Paisan GM, Sokolowski JD, et al. High-Grade Aneurysmal Subarachnoid Hemorrhage: Predictors of Functional Outcome. World Neurosurg. 2019;125:e723–8.
Kaneko J, Tagami T, Unemoto K, Tanaka C, Kuwamoto K, Sato S, et al. Functional Outcome Following Ultra-Early Treatment for Ruptured Aneurysms in Patients with Poor-Grade Subarachnoid Hemorrhage. J Nippon Med Sch. 2019;86(2):81–90.
Konczalla J, Seifert V, Beck J, Guresir E, Vatter H, Raabe A, et al. Outcome after Hunt and Hess Grade V subarachnoid hemorrhage: a comparison of pre-coiling era (1980–1995) versus post-ISAT era (2005–2014). J Neurosurg. 2018;128(1):100–10.
Le Roux PD, Elliott JP, Newell DW, Grady MS, Winn HR. Predicting outcome in poor-grade patients with subarachnoid hemorrhage: a retrospective review of 159 aggressively managed cases. J Neurosurg. 1996;85(1):39–49.
Liu J, Xiong Y, Zhong M, Yang Y, Guo X, Tan X, et al. Predicting Long-Term Outcomes After Poor-Grade Aneurysmal Subarachnoid Hemorrhage Using Decision Tree Modeling. Neurosurgery. 2020;87(3):523–9.
Panni P, Colombo E, Donofrio CA, Barzaghi LR, Albano L, Righi C, et al. Hemorrhagic burden in poor-grade aneurysmal subarachnoid hemorrhage: a volumetric analysis of different bleeding distributions. Acta Neurochir (Wien). 2019;161(4):791–7.
Ridwan S, Kristof R. Cardiac Arrest in Patients with Poor-Grade Aneurysmal Subarachnoid Hemorrhage: A Single-Center Experience. J Neurol Surg A Cent Eur Neurosurg. 2019;80(6):409–12.
Schuss P, Hadjiathanasiou A, Borger V, Wispel C. Poor-grade aneurysmal subarachnoid hemorrhage: factors influencing functional outcome—a single-center series. World neurosurgery. 2016;85:125–9.
Schwartz C, Pfefferkorn T, Ebrahimi C, Ottomeyer C, Fesl G, Bender A, et al. Long-term Neurological Outcome and Quality of Life after World Federation of Neurosurgical Societies Grades IV and V Aneurysmal Subarachnoid Hemorrhage in an Interdisciplinary Treatment Concept. Neurosurgery. 2017;80(6):967–74.
Shirao S, Yoneda H, Kunitsugu I, Ishihara H, Koizumi H, Suehiro E, et al. Preoperative prediction of outcome in 283 poor-grade patients with subarachnoid hemorrhage: a project of the Chugoku-Shikoku Division of the Japan Neurosurgical Society. Cerebrovasc Dis. 2010;30(2):105–13.
Szklener S, Melges A, Korchut A, Zaluska W, Trojanowski T, Rejdak R, et al. Predictive model for patients with poor-grade subarachnoid haemorrhage in 30-day observation: a 9-year cohort study. BMJ Open. 2015;5(6):e007795.
Tsuang FY, Chen JY, Lee CW, Li CH, Lee JE, Lai DM, et al. Risk profile of patients with poor-grade aneurysmal subarachnoid hemorrhage using early perfusion computed tomography. World Neurosurg. 2012;78(5):455–61.
van den Berg R, Foumani M, Schroder RD, Peerdeman SM, Horn J, Bipat S, et al. Predictors of outcome in World Federation of Neurologic Surgeons grade V aneurysmal subarachnoid hemorrhage patients. Crit Care Med. 2011;39(12):2722–7.
Wang X, Han C, Xing D, Wang C, Ding X. Early management of poor-grade aneurysmal subarachnoid hemorrhage: A prognostic analysis of 104 patients. Clin Neurol Neurosurg. 2019;179:4–8.
Wostrack M, Sandow N, Vajkoczy P, Schatlo B, Bijlenga P, Schaller K, et al. Subarachnoid haemorrhage WFNS grade V: is maximal treatment worthwhile? Acta Neurochir (Wien). 2013;155(4):579–86.
Jaja BN, Cusimano MD, Etminan N, Hanggi D, Hasan D, Ilodigwe D, et al. Clinical prediction models for aneurysmal subarachnoid hemorrhage: a systematic review. Neurocrit Care. 2013;18(1):143–53.
Jaja BNR, Saposnik G, Lingsma HF, Macdonald E, Thorpe KE, Mamdani M, et al. Development and validation of outcome prediction models for aneurysmal subarachnoid haemorrhage: the SAHIT multinational cohort study. BMJ. 2018;360:j5745.
Lo BW, Fukuda H, Nishimura Y, Farrokhyar F, Thabane L, Levine MA. Systematic review of clinical prediction tools and prognostic factors in aneurysmal subarachnoid hemorrhage. Surg Neurol Int. 2015;6:135.
Risselada R, Lingsma HF, Bauer-Mehren A, Friedrich CM, Molyneux AJ, Kerr RS, et al. Prediction of 60 day case-fatality after aneurysmal subarachnoid haemorrhage: results from the International Subarachnoid Aneurysm Trial (ISAT). Eur J Epidemiol. 2010;25(4):261–6.
Risselada R, Lingsma HF, Molyneux AJ, Kerr RS, Yarnold J, Sneade M, et al. Prediction of two month modified Rankin Scale with an ordinal prediction model in patients with aneurysmal subarachnoid haemorrhage. BMC Med Res Methodol. 2010;10:86.
Rosengart AJ, Schultheiss KE, Tolentino J, Macdonald RL. Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2007;38(8):2315–21.
Stienen MN, Germans M, Burkhardt JK, Neidert MC, Fung C, Bervini D, et al. Predictors of In-Hospital Death After Aneurysmal Subarachnoid Hemorrhage: Analysis of a Nationwide Database (Swiss SOS [Swiss Study on Aneurysmal Subarachnoid Hemorrhage]). Stroke. 2018;49(2):333–40.
Giraldo EA, Mandrekar JN, Rubin MN, Dupont SA, Zhang Y, Lanzino G, et al. Timing of clinical grade assessment and poor outcome in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2012;117(1):15–9.
Raabe A, Beck J, Goldberg J, Z Graggen WJ, Branca M, Marbacher S, et al. Herniation world federation of neurosurgical societies scale improves prediction of outcome in patients with poor-grade aneurysmal subarachnoid hemorrhage. Stroke. 2022. https://doi.org/10.1161/STROKEAHA.121.036699.
Bijlenga P, Morita A, Ko NU, Mocco J, Morel S, Murayama Y, et al. Common Data Elements for Subarachnoid Hemorrhage and Unruptured Intracranial Aneurysms: Recommendations from the Working Group on Subject Characteristics. Neurocrit Care. 2019;30(Suppl 1):20–7.
Guresir E, Beck J, Vatter H, Setzer M, Gerlach R, Seifert V, et al. Subarachnoid hemorrhage and intracerebral hematoma: incidence, prognostic factors, and outcome. Neurosurgery. 2008;63(6):1088–93 discussion 93–4.
Kent DM, van Klaveren D, Paulus JK, D’Agostino R, Goodman S, Hayward R, et al. The Predictive Approaches to Treatment effect Heterogeneity (PATH) Statement: Explanation and Elaboration. Ann Intern Med. 2020;172(1):W1–25.
Acknowledgements
The authors wish to thank Elise Krabbendam and Sabrina Meertens-Gunput, medical information specialists, from the Erasmus MC Medical Library for developing and updating the search strategies.
Funding
The authors have not received funding relevant for this study.
Author information
Authors and Affiliations
Contributions
Conception and design: Cras, Lingsma, Roozenbeek, de Winkel. Acquisition of data: Cras, Lingsma, Roozenbeek, de Winkel. Analysis and interpretation of data: Lingsma, Roozenbeek, de Winkel. Drafting the article: de Winkel. Critically revising the article: All authors. Statistically analysis: de Winkel. Study supervision: Lingsma, Roozenbeek. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not appicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competings interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
PRISMA checklist.
Additional file 2: Methods 1.
Search strategy.
Additional file 3: Methods 2.
Eligibility criteria.
Additional file 4: Methods 3.
Risk of bias criteria for final verdict.
Additional file 5:
Figure 1. PRISMA Flow chart.
Additional file 6:
Table 2. Study characterization.
Additional file 7: Table 3.
Meta-analysis.
Additional file 8: Table 4.
Systematic review.
Additional file 9: Figure 2A.
Funnel plots of meta-analysis of age before trim-and-fill. Figure 2B. Funnel plots of meta-analysis of age after trim-and-fill.
Additional file 10: Figure 3.
Risk of bias traffic light plot.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Winkel, J., Cras, T. ., Dammers, R. et al. Early predictors of functional outcome in poor-grade aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. BMC Neurol 22, 239 (2022). https://doi.org/10.1186/s12883-022-02734-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-022-02734-x