Abstract
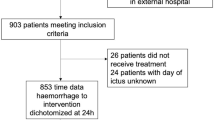
The most threatening early complication and predictor of poor outcome after an aneurysmal subarachnoid hemorrhage (aSAH) is a rebleed. To evaluate what proportion of rebleeds might be prevented by early treatment, we assessed the time interval from the initial hemorrhage to rebleed, and the location of the patient at the time of rebleed. Patient characteristics, World Federation of Neurological Surgeons grade on admission and modified Rankin Scale outcome scores, referring hospitals and time intervals from initial hemorrhage to treatment of 293 patients treated between 2008 and 2011 were evaluated. Time intervals to rebleeds and location of the patients at the time of rebleed were retrieved. Rebleeds were confirmed by CT in 12 % of patients, and an additional 4 % of patients was diagnosed as having a possible rebleed. Sixty percent of rebleeds occurred after admission to the treatment center. Almost all rebleeds occurred within 24 h, with a median time interval between initial hemorrhage and rebleed of 180 min. A significantly shorter time to treatment and a higher mortality were seen in the group of patients with a rebleed. Approximately, one in six patients with an aSAH had a rebleed, of which a majority might have been preventable because they occurred after admission to the treatment center. A reduction in the rebleed rate seems feasible by securing the aneurysm as soon as possible by improving in-hospital logistics for early aneurysm treatment. Alternative options, such as immediate administration of antifibrinolytics, are being explored in a multicenter trial.


Similar content being viewed by others
References
Baharoglu MI, Germans MR, Rinkel GJ, Algra A, Vermeulen M, van Gijn GJ, Roos YB (2013) Antifibrinolytic therapy for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev 8:CD001245
Bouckaert M, Lemmens R, Thijs V (2009) Reducing prehospital delay in acute stroke. Nat Rev Neurol 5:477–483
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A (1994) Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke 25:1342–1347
Cha KC, Kim JH, Kang HI, Moon BG, Lee SJ, Kim JS (2010) Aneurysmal rebleeding : factors associated with clinical outcome in the rebleeding patients. J Korean Neurosurg Soc 47:119–123
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737
Fujii Y, Takeuchi S, Sasaki O, Minakawa T, Koike T, Tanaka R (1996) Ultra-early rebleeding in spontaneous subarachnoid hemorrhage. J Neurosurg 84:35–42
Germans MR, Post R, Coert BA, Rinkel GJ, Vandertop WP, Verbaan D (2013) Ultra-early tranexamic acid after subarachnoid hemorrhage (ULTRA): study protocol for a randomized controlled trial. Trials 14:143
Guo LM, Zhou HY, Xu JW, Wang Y, Qiu YM, Jiang JY (2011) Risk factors related to aneurysmal rebleeding. World Neurosurg 76:292–298
Hillman J, Fridriksson S, Nilsson O, Yu Z, Saveland H, Jakobsson KE (2002) Immediate administration of tranexamic acid and reduced incidence of early rebleeding after aneurysmal subarachnoid hemorrhage: a prospective randomized study. J Neurosurg 97:771–778
Kwan J, Hand P, Sandercock P (2004) Improving the efficiency of delivery of thrombolysis for acute stroke: a systematic review. QJM 97:273–279
Laidlaw JD, Siu KH (2002) Ultra-early surgery for aneurysmal subarachnoid hemorrhage: outcomes for a consecutive series of 391 patients not selected by grade or age. J Neurosurg 97:250–258
Larsen CC, Sorensen B, Nielsen JD, Astrup J (2012) Reduced clot-stability during the first 6 hours after aneurysmal subarachnoid haemorrhage––a prospective case–control study. Thromb Res 129:e229–e232
Lindsberg PJ, Happola O, Kallela M, Valanne L, Kuisma M, Kaste M (2006) Door to thrombolysis: ER reorganization and reduced delays to acute stroke treatment. Neurology 67:334–336
Mikulik R, Kadlecova P, Czlonkowska A, Kobayashi A, Brozman M, Svigelj V, Csiba L et al (2012) Factors influencing in-hospital delay in treatment with intravenous thrombolysis. Stroke 43:1578–1583
Naidech AM, Janjua N, Kreiter KT, Ostapkovich ND, Fitzsimmons BF, Parra A, Commichau C et al (2005) Predictors and impact of aneurysm rebleeding after subarachnoid hemorrhage. Arch Neurol 62:410–416
Phillips TJ, Dowling RJ, Yan B, Laidlaw JD, Mitchell PJ (2011) Does treatment of ruptured intracranial aneurysms within 24 hours improve clinical outcome? Stroke 42:1936–1945
Rankin J (1957) Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J 2:200–215
Roos YB, Beenen LF, Groen RJ, Albrecht KW, Vermeulen M (1997) Timing of surgery in patients with aneurysmal subarachnoid haemorrhage: rebleeding is still the major cause of poor outcome in neurosurgical units that aim at early surgery. J Neurol Neurosurg Psychiatry 63:490–493
Skrifvars MB, Parr MJ (2012) Incidence, predisposing factors, management and survival following cardiac arrest due to subarachnoid haemorrhage: a review of the literature. Scand J Trauma Resusc Emerg Med 20:75
Starke RM, Connolly ES Jr (2011) Rebleeding after aneurysmal subarachnoid hemorrhage. Neurocrit Care 15:241–246
Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G (2013) European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis 35:93–112
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, De Villiers JC (1988) A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry 51:1457
van den Berg R, Foumani M, Schroder RD, Peerdeman SM, Horn J, Bipat S, Vandertop WP (2011) Predictors of outcome in World Federation of Neurologic Surgeons grade V aneurysmal subarachnoid hemorrhage patients. Crit Care Med 39:2722–2727
Walter S, Kostopoulos P, Haass A, Keller I, Lesmeister M, Schlechtriemen T, Roth C et al (2012) Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol 11:397–404
Weil AG, Zhao JZ (2012) Treatment of ruptured aneurysms: earlier is better. World Neurosurg 77:263–265
Wong GK, Boet R, Ng SC, Chan M, Gin T, Zee B, Poon WS (2012) Ultra-early (within 24 hours) aneurysm treatment after subarachnoid hemorrhage. World Neurosurg 77:311–315
Acknowledgments
We thank Jantien Hoogmoed and Stéphanie van Straaten for their help in the collection of data. This research received no specific Grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard
The author hereby declares that the research documented in the manuscript has been carried out in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Germans, M.R., Coert, B.A., Vandertop, W.P. et al. Time intervals from subarachnoid hemorrhage to rebleed. J Neurol 261, 1425–1431 (2014). https://doi.org/10.1007/s00415-014-7365-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7365-0