Abstract
Background
Diverse mechanisms including infections, autoimmune inflammatory reactions, neoplasms, and degeneration are involved in the central nervous system in cases of acquired immune deficiency syndrome. In such cases, it is difficult to determine the precise pathogenesis by radiological examination and laboratory testing.
Case presentation
We report a 37-year-old Japanese woman who had untreated hypertension and gender identity disorder and had been taking testosterone injections since she was 19 years old. She developed a headache and visual field deficits together with elevated blood pressure. According to radiological findings, she was initially suspected as having posterior reversible encephalopathy syndrome in the right parieto-occipital lobe with reversible cerebral vasoconstriction syndrome. Human immunodeficiency virus antibody was positive and the CD4+ T-lymphocyte count was 140 cells/μl. Therefore, antiretroviral therapy was started. Antiretroviral therapy suppressed the activity of acquired immune deficiency syndrome but worsened her visual symptoms and expanding radiological lesions. Brain biopsy led to the diagnosis of CD8+ encephalitis, and she also fulfilled the diagnosis of paradoxical immune reconstitution inflammatory syndrome. Corticosteroid therapy alleviated her symptoms.
Conclusions
This is a rare case of CD8+ encephalitis, with an exacerbation owing to paradoxical immune reconstitution inflammatory syndrome after antiretroviral therapy, which radiologically mimicked posterior reversible encephalopathy syndrome. Corticosteroid therapy was effective; thus, it is important to provide a pathological diagnosis in such cases.
Similar content being viewed by others
Background
A variety of comorbidities including infections, autoimmune inflammatory reactions, neoplasms, and degeneration are involved in the central nervous system (CNS) in acquired immune deficiency syndrome (AIDS) patients [1,2,3]. It is difficult to determine the pathogenesis of such CNS complications by radiological examination and laboratory testing; therefore, brain biopsy is necessary [4]. Here, we report the case of a patient who developed bilateral posterior lesions together with elevated blood pressure, mimicking posterior reversible encephalopathy syndrome (PRES) [5]. However, the case showed recurrent and progressive symptoms, and brain biopsy was carried out.
Case presentation
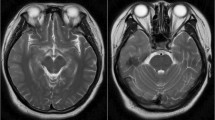
A 37-year-old Japanese woman had a history of gender identity disorder from childhood and had taken testosterone injections once every 2 weeks since she was 19 years old. She also had untreated high blood pressure. She had worked in the sex industry and had a tattoo on her right arm. In May 2017, she developed a headache and visual field deficits together with elevated blood pressure and was referred to our hospital. On admission, her blood pressure was 165/105 mmHg with regular heart rhythm. She was alert and well oriented. She had left homonymous hemianopia. Brain magnetic resonance imaging (MRI) showed a hyperintense lesion in the right parieto-occipital lobe on diffusion-weighted imaging (DWI), apparent diffusion coefficient (ADC) map, and fluid-attenuated inversion recovery (FLAIR) (Fig. 1a–c), which were not enhanced by contrast with gadolinium. MR angiography (MRA) showed steno-occlusive lesions in bilateral middle cerebral arteries (MCAs) (Fig. 1d). Three-dimensional contrast-enhanced angiography revealed occlusions of bilateral MCAs (Fig. 1e). She was initially suspected as having PRES related to reversible cerebral vasoconstriction syndrome (RCVS) and received treatment with an antihypertensive drug and 100 mg of aspirin. Routine blood testing showed the patient was HIV-1 antibody-positive. The CD4+ T-cell count was 140 cells/μl and the HIV viral load detected by PCR was 330,000 copies/ml. She underwent lumbar puncture, and no pleocytosis was found. Furthermore, PCR for herpes simplex virus (HSV), varicella-zoster virus (VZV), and JC virus in cerebrospinal fluid was negative. She had also developed pneumocystis pneumonia when she was diagnosed with AIDS. Antiretroviral therapy (ART) comprising dolutegravir sodium, emtricitabine, and tenofovir alafenamide fumarate was initiated, and she was discharged from the hospital. Two weeks later, she suffered a severe headache and worsening of visual disturbance in bilateral eyes. Her blood pressure was 153/93 mmHg and her visual acuities were finger counting. MRI showed the hyperintense lesion had expanded to bilateral posterior hemispheres (Fig. 2a–c). Stenotic lesions in bilateral MCAs remained on MRA and three-dimensional contrast-enhanced angiography (Fig. 2d, e). The CD4+ T-cell count at readmission was 189 cells/μl and HIV viral load was 94 copies/ml, indicating that AIDS activity was alleviated after ART. Although she was initially treated with edaravone, a free radical scavenger, and antihypertensive agents after readmission, her visual acuities fluctuated and contrast-enhanced MRI showed multiple punctate and linear gadolinium-enhanced lesions in the occipital and temporal lobes and the cerebellum (Fig. 2f). Brain biopsy was performed from the right occipital lobe. Histopathology showed severe tissue destruction, astrocytic gliosis, microglial activation, and vasculitis with marked lymphocytic infiltration in the cerebral white matter in the absence of multinucleated giant cells and lymphoma cells (Fig. 3a, b). Infiltrated lymphocytes were mostly CD8+ T-lymphocytes, while CD4+ T-lymphocytes were scarce (Fig. 3c, d). We finally diagnosed her as having CD8+ encephalitis, with an exacerbation caused by immune reconstitution inflammatory syndrome (IRIS) after ART. After brain biopsy, the patient was treated with 1000 mg of methylprednisolone intravenously for 3 consecutive days followed by 0.5 mg/kg/day of prednisolone. Her visual acuities and headache improved after corticosteroid treatment.
Radiological observations on the first admission a–c. Brain magnetic resonance imaging (MRI) on the first admission shows a hyperintense lesion in the right parieto-occipital lobe on diffusion-weighted imaging (a), apparent diffusion coefficient map (b), and fluid-attenuated inversion recovery (c). d. MR angiography shows stenosis in bilateral middle cerebral arteries (MCAs). e. Three-dimensional contrast-enhanced angiography revealed occlusions in bilateral MCAs (yellow arrowheads)
Radiological observations on the second admission a–c. Brain magnetic resonance imaging (MRI) on the second admission shows hyperintense lesions in the bilateral occipital lobe on diffusion-weighted imaging (a), apparent diffusion coefficient map (b), and fluid-attenuated inversion recovery (c). d. MR angiography shows stenosis in bilateral middle cerebral arteries (MCAs). e. Three-dimensional contrast-enhanced angiography revealed occlusions in bilateral MCAs (yellow arrowheads). f. Contrast-enhanced MRI shows multiple punctate and linear gadolinium-enhanced lesions (red arrows) in the occipital and temporal lobes and cerebellum
Pathological study from brain biopsy samples a–d. Pathological findings from brain biopsy samples in the right occipital lobe show severe lymphocytic infiltration with vasculitis (a, hematoxylin and eosin) and activated microglia (b, Iba-1) in the white matter. Most lymphocytes were CD8 T-cells (c, CD8), and CD4 T-cells were scarce (d, CD4). Scale bars = 200 μm
Discussion and conclusions
The present patient, who had gender identity disorder and was taking testosterone injections, developed a headache, high blood pressure, progressive focal neurological deficits and showed posterior hyperintense lesions on DWI/ADC/FLAIR and multifocal intracranial artery stenosis on MRA, which was likely radiological findings of PRES together with RCVS at the first admission. It has been reported that PRES can occur in AIDS patients [6]. After ART, the patient’s symptoms worsened and radiological findings showed focal hyperintensity on T2/FLAIR imaging with punctate and curvilinear gadolinium enhancements, which are characteristic of CD8+ encephalitis, progressive multifocal leukoencephalopathy (PML), and lymphoma recognized in HIV patients [1,2,3,4, 7]. Interestingly, brain biopsy in our case revealed CD8+ encephalitis; thus, brain biopsy should be considered in AIDS patients when the clinical course is progressive and radiological studies are insufficient.
CD8+ encephalitis has been characterized as a progressive encephalopathy that occurs in HIV-infected patients with clinical features of headache, cognitive impairment, seizure, and reactivity to corticosteroid therapy [4, 8]. In particular, a previous histopathological study clearly demonstrated infiltration of CD8+ T-cells and microglia in perivascular areas and parenchyma, indicating CD8+ encephalitis. In addition, findings excluded diagnoses of PML owing to lacking JC virus inclusions, HIV encephalitis related to multinuclear giant cells, and lymphoma due to the absence of abnormal proliferated cells, as well as infiltration of CD3+ and CD4+ T-cells in chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids [2, 3, 9]. Furthermore, ART increased the CD4+ T-cell count and significantly reduced the HIV viral load, and occipital lesions on MRI expanded, indicating development of immune reconstitution in the brain; therefore, IRIS also might be involved in the pathogenesis of our case [1]. Our case developed a visual field defect as the initial symptom and right occipital lesion before ART, and fulfilled the diagnostic criteria for paradoxical IRIS [1]. Generally, AIDS patients with IRIS have concomitant infectious encephalitis or encephalopathy such as PML caused by JC virus, cryptococcal meningitis, VZV encephalitis, or tuberculosis. However, a previous case series demonstrated that few HIV cases, which were PCR-negative for HSV, VZV, and JC virus, developed CD8+ encephalitis and IRIS caused by noninfectious pathogens, which was consistent with our case [7, 8, 10]. These common mechanisms may be attributed to unbalanced reconstitution that proliferative CD8+ cytotoxic lymphocytes in the absence of CD4+ lymphocytes in CNS can be deleterious, despite the increase in systemic CD4+ lymphocytes after ART [8].
Importantly, our case exhibited bilateral MCA stenotic lesions on MRA, which led us to initially suspect PRES with RCVS. Whether CD8+ encephalitis with IRIS involves large intracranial arteries is presently unknown. RCVS is characterized by headache, stenotic changes in multiple intracranial large arteries for 1–3 months, and could simultaneously occur with PRES. [11] Alternatively, angiitis related to HIV, atherosclerotic changes owing to long-term hypertension, and administration of testosterone might be related to stenosis [12]. However, radiological observations after 3 months and pathological alterations in MCA were not investigated in our case; therefore, precise mechanisms remain unknown.
To our knowledge, this is a rare case of CD8+ encephalitis with an exacerbation owing to paradoxical IRIS after ART, which radiologically mimicked PRES. Corticosteroid therapy was effective; thus, it is important to provide a pathological diagnosis in such cases. However, involvement of cerebral large arteries is pathologically unknown, and further investigation is warranted.
Availability of data and materials
All the data supporting our findings are provided within the manuscript.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- AIDS:
-
Acquired immune deficiency syndrome
- ART:
-
Antiretroviral therapy
- CNS:
-
Central nervous system
- DWI:
-
Diffusion-weighted imaging
- FLAIR:
-
Fluid-attenuated inversion recovery
- IRIS:
-
Immune reconstitution inflammatory syndrome
- MCAs:
-
Middle cerebral arteries
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- PCA:
-
Posterior cerebral artery
- PML:
-
Progressive multifocal leukoencephalopathy
- PRES:
-
Posterior reversible encephalopathy syndrome
- RCVS:
-
Reversible cerebral vasoconstriction syndrome
References
Haddow LJ, Easterbrook PJ, Mosam A, et al. Defining immune reconstitution inflammatory syndrome: evaluation of expert opinion versus 2 case definitions in a south African cohort. Clin Infect Dis. 2009;49:1424–32.
Moll NM, Rietsch AM, Ransohoff AJ, et al. Cortical demyelination in PML and MS: similarities and differences. Neurology. 2008;70:336–43.
Michaels J, Price RW, Rosenblum MK. Microglia in the giant cell encephalitis of acquired immune deficiency syndrome: proliferation, infection and fusion. Acta Neuropathol. 1988;76:373–9.
Taieb G, Duran-Pena A, de Chamfleur NM, et al. Punctate and curvilinear gadolinium enhancing lesions in the brain: a practical approach. Neuroradiology. 2016;58:221–35.
Roth C, Ferbert A. The posterior reversible encephalopathy syndrome: what's certain, what's new? Pract Neurol. 2011;11:136–44.
Birner B, Hirzel C, Wagner F, Waldegg G. Posterior reversible encephalopathy syndrome in an HIV-infected patient on antiretroviral treatment: what is the risk factor? BMJ Case Rep. 2018;2018.
Lescure FX, Moulignier A, Savatovsky J, et al. CD8 encephalitis in HIV-infected patients receiving cART: a treatable entity. Clin Infect Dis. 2013;57:101–8.
Gray F, Lescure FX, Adle-Biassette H, et al. Encephalitis with infiltration by CD8+ lymphocytes in HIV patients receiving combination antiretroviral treatment. Brain Pathol. 2013;23:525–33.
Pittock SJ, Debruyne J, Krecke KN, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain. 2010;133:2626–34.
Ringelstein A, Oelschlaeger C, Saleh A, et al. Severe aseptic leucoencephalopathy as immune reconstitution inflammatory syndrome in Caucasian and African patients. AIDS. 2009;23 11:1435–137.
Ducros A, Boukobza M, Porcher R, et al. The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome. A prospective series of 67 patients. Brain. 2007;130:3091–101.
Ammar EM, Said SA, Hassan MS. Enhanced vasoconstriction and reduced vasorelaxation induced by testosterone and nandrolone in hypercholesterolemic rabbits. Pharmacol Res. 2004;50:253–9.
Acknowledgements
Not applicable.
Funding
This work was supported, in part, by the Japan Society for the Promotion of Science (grant number 20K07909 to Dr. Ueno).
Author information
Authors and Affiliations
Contributions
Study concept and design: YU. Acquisition of data: MI, YU, YI, MT, KM, GT, KD, AS, KY, TN, and NH. Analysis and interpretation of data: MI, YU, YI, MT, KM, GT, KY, TN, and NH. Drafting of the manuscript: MI and YU. Critical revision of the manuscript for important intellectual content: YU and NH. Study supervision: NH. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors declare that ethics approval was not required for this case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ishiguro, M., Ueno, Y., Ishiguro, Y. et al. CD8+ T-cell encephalitis mimicking PRES in AIDS: a case report. BMC Neurol 20, 179 (2020). https://doi.org/10.1186/s12883-020-01756-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-020-01756-7