Abstract
Background
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis (AE) is a common cause of nonviral infectious encephalitis, which can be triggered by herpes simplex virus infection. Previous studies have shown that approximately 27% of herpes simplex encephalitis (HSE) patients produce anti-NMDAR antibodies within 3 months. Immunotherapy is recommended in this situation, but some symptoms usually remain in the 1-year follow-up.
Case presentation
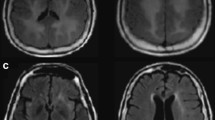
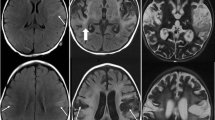
A previously healthy 23-year-old Chinese young woman developed epileptic attack followed by psychiatric symptoms of confusion and irritation as well as cognitive deficits. Brain MRI showed hyperintense lesions of the right temporal lobe on DWI and T2 without contrast enhancement effects. Twenty-one days of acyclovir was administered based on the primary diagnosis of HSE. The anti-NMDAR antibody (IgG) was detected positively on day 11 after disease onset. She had improved cognitive function but suffered another grand mal epilepsy after the first course of intravenous immunoglobulin (IVIG) therapy combined with 1000 mg intravenous methylprednisolone. After discussion, another course of IVIG was started for 5 days. Her symptoms were well controlled with only mild cognitive deficits at the 1-year follow-up (mRS = 1).
Conclusions
Our case indicated that anti-NMDAR antibodies could develop earlier after HSE compared with previous data from adults. We suggested detecting AE antibodies simultaneously with each CSF analysis. Meanwhile, the second course of IVIG therapy was reasonable when symptoms were not controlled after the first course of IVIG combined with IV steroid treatment.


Similar content being viewed by others
References
Dalmau J, Tüzün E, Wu H-y, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR (2007) Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61:25–36
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R (2011) Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 10:63–74
Lynch DR, Rattelle A, Dong YN, Roslin K, Gleichman AJ, Panzer JA (2018) Anti-NMDA receptor encephalitis: clinical features and basic mechanism. Adv Pharmacol 82:235–260
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:1091–1098
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, Cortese I, Dale RC, Gelfand JM, Geschwind M, Glaser CA, Honnorat J, Höftberger R, Iizuka T, Irani SR, Lancaster E, Leypoldt F, Prüss H, Rae-Grant A, Reindl M, Rosenfeld MR, Rostásy K, Saiz A, Venkatesan A, Vincent A, Wandinger KP, Waters P, Dalmau J (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404
Peng Y, Liu X, Pan S, Xie Z, Wang H (2017) Anti-N-methyl-D-aspartate receptor encephalitis associated with intracranial Angiostrongylus cantonensis infection: a case report. Neurol Sci 38:703–706
Martinez HR, Olguin-Ramirez LA, Camara-Lemarroy CR (2018) Lyme borreliosis as a trigger for NMDA receptor encephalitis? Neurol Sci 39:1815–1817
Iizuka T, Sakai F, Ide T, Monzen T, Yoshii S, Iigaya M, Suzuki K, Lynch DR, Suzuki N, Hata T, Dalmau J (2008) Anti-NMDA receptor encephalitis in Japan: long-term outcome without tumor removal. Neurology 70:504–511
Viaccoz A, Desestret V, Ducray F, Picard G, Cavillon G, Rogemond V, Antoine JC, Delattre JY, Honnorat J (2014) Clinical specificities of adult male patients with NMDA receptor antibodies encephalitis. Neurology 82:556–563
Nosadini M, Mohammad SS, Corazza F, Ruga EM, Kothur K, Perilongo G, Frigo AC, Toldo I, Dale RC, Sartori S (2017) Herpes simplex virus-induced anti-N-methyl-d-aspartate receptor encephalitis: a systematic literature review with analysis of 43 cases. Dev Med Child Neurol 59:796–805
Leypoldt F, Titulaer MJ, Aguilar E, Walther J, Bönstrup M, Havemeister S, Teegen B, Lütgehetmann M, Rosenkranz M, Magnus T, Dalmau J (2013) Herpes Simplex virus-1 Encephalitis Can Trigger anti-NMDA Receptor Encephalitis Case Report. Neurology 81:1637–1639
Armangue T, Spatola M, Vlagea A, Mattozzi S, Cárceles-Cordon M, Martinez-Heras E, Llufriu S, Muchart J, Erro ME, Abraira L, Moris G, Monros-Giménez L, Corral-Corral Í, Montejo C, Toledo M, Bataller L, Secondi G, Ariño H, Martínez-Hernández E, Juan M, Marcos MA, Alsina L, Saiz A, Rosenfeld MR, Graus F, Dalmau J, Aguilera-Albesa S, Amado-Puentes A, Arjona-Padillo A, Arrabal L, Arratibel I, Aznar-Laín G, Bellas-Lamas P, Bermejo T, Boyero-Durán S, Camacho A, Campo A, Campos D, Cantarín-Extremera V, Carnero C, Conejo-Moreno D, Dapena M, Dacruz-Álvarez D, Delgadillo-Chilavert V, Deyà A, Estela-Herrero J, Felipe A, Fernández-Cooke E, Fernández-Ramos J, Fortuny C, García-Monco JC, Gili T, González-Álvarez V, Guerri R, Guillén S, Hedrera-Fernández A, López M, López-Laso E, Lorenzo-Ruiz M, Madruga M, Málaga-Diéguez I, Martí-Carrera I, Martínez-Lacasa X, Martín-Viota L, Martín Gil L, Martínez-González MJ, Moreira A, Miranda-Herrero MC, Monge L, Muñoz-Cabello B, Navarro-Morón J, Neth O, Noguera-Julian A, Nuñez-Enamorado N, Pomar V, Portillo-Cuenca JC, Poyato M, Prieto L, Querol L, Rodríguez-Rodríguez E, Sarria-Estrada S, Sierra C, Soler-Palacín P, Soto-Insuga V, Toledo-Bravo L, Tomás M, Torres-Torres C, Turón E, Zabalza A (2018) Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol 17:760–772
Desena A, Graves D, Warnack W, Greenberg BM (2014) Herpes simplex encephalitis as a potential cause of anti-N-methyl-D-aspartate receptor antibody encephalitis: report of 2 cases. JAMA Neurol 71:344–346
Armangue T, Leypoldt F, Málaga I, Raspall-Chaure M, Marti I, Nichter C, Pugh J, Vicente-Rasoamalala M, Lafuente-Hidalgo M, Macaya A, Ke M, Titulaer MJ, Höftberger R, Sheriff H, Glaser C, Dalmau J (2014) Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann Neurol 75:317–323
Pistacchi M, Marsala SZ, Gioulis M, Sanson F, Giometto B (2015) Uncommon relapse after post-herpes simplex encephalitis: an atypical case report. Acta Neurol Belg 115:691–695
Moris G, Armangue T, Extremera VC, Conde CE, Erro ME, Rostasy K, Cuenca JCP, Turón-Viñas E, Málaga I, Muñoz-Cabello B, CarmenTorres-Torres SL, González-Gutiérrez-Solana L, González G, Casado-Naranjo I, Rosenfeld M, Graus F, Dalmau J, On behalf of the Spanish Prospective Multicentric Study of Autoimmunity in Herpes Simplex Encephalitis (2015) Autoimmune post-herpes simplex encephalitis of adults and teenagers. Neurology 85:1746–1743
Morris NA, Kaplan TB, Linnoila J, Cho T (2016) HSV encephalitis-induced anti-NMDAR encephalitis in a 67-year-old woman: report of a case and review of the literature. J Neuro-Oncol 22:33–37
Schein F, Gagneux-Brunon A, Antoine JC, Lavernhe S, Pillet S, Paul S, Frésard A, Boutet C, Grange R, Cazorla C, Lucht F, Botelho-Nevers E (2017) Anti-N-methyl-D-aspartate receptor encephalitis after herpes simplex virus-associated encephalitis: an emerging disease with diagnosis and therapeutic challenges. Infection 45:545–549
Dorcet G, Benaiteau M, Bost C, Mengelle C, Bonneville F, Martin-Blondel G, Pariente J (2020) Two cases of late-onset anti-NMDAr auto-immune encephalitis after herpes simplex virus 1 encephalitis. Front Neurol 11:38
Hjalmarsson A, Blomqvist P, Sköldenberg B (2007) Herpes simplex encephalitis in Sweden, 1990-2001: incidence, morbidity, and mortality. Clin Infect Dis 45:875–880
Fujinami RS, von Herrath MG, Christen U, Whitton JL (2006) Molecular mimicry, bystander activation, or viral persistence: infections and autoimmune disease. Clin Microbiol Rev 19(1):80–94
Pruss H, Finke C, Holtje M, Hofmann J, Klingbeil C, Probst C et al (2012) N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 72:902–911
Westman G, Studahl M, Ahlm C, Eriksson BM, Persson B, Ronnelid J et al (2016) N-methyl-d-aspartate receptor autoimmunity affects cognitive performance in herpes simplex encephalitis. Clin Microbiol Infect 22:934–940
Malter MP, Helmstaedter C, Urbach H, Vincent A, Bien CG (2010) Antibodies to glutamic acid decarboxylase define a form of limbic encephalitis. Ann Neurol 67:470–478
Xu et al (2012) CMV-associated encephalitis and antineuronal autoantibodies - a case report. BMC Neurol 12:87
Niehusmann P, Widman G, Eis-Hubinger AM, Greschus S, Robens BK, Grote A et al (2016) Non-paraneoplastic limbic encephalitis and central nervous HHV-6B reactivation: causality or coincidence? Neuropathology 36:376–380
Hargrave DR, Webb DW (1998) Movement disorders in association with herpes simplex virus encephalitis in children: a review. Dev Med Child Neurol 40:640–642
Al-Obaidi MMJ, Bahadoran A, Wang SM, Manikam R, Raju CS, Sekaran SD (2018) Disruption of the blood brain barrier is vital property of neurotropic viral infection of the central nervous system. Acta Virol 62:16–27
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, Honig LS, Benseler SM, Kawachi I, Martinez-Hernandez E, Aguilar E, Gresa-Arribas N, Ryan-Florance N, Torrents A, Saiz A, Rosenfeld MR, Balice-Gordon R, Graus F, Dalmau J (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165
Hau L, Csábi G, Tényi T (2015) Anti-N-methyl-D aspartate receptor encephalitis guideline to the challenges of diagnosis and therapy. Psychiatr Hung 30(4):402–408
Kong SS, Chen YJ, Su IC, Lin JJ, Chou IJ, Chou ML, Hung PC, Hsieh MY, Wang YS, Chou CC, Wang HS, Lin KL, CHEESE Study Group (2019) Immunotherapy for anti-NMDA receptor encephalitis: experience from a single center in Taiwan. Pediatr Neonatol 60:417–422
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, S., Lan, T., Bai, R. et al. HSV encephalitis triggered anti-NMDAR encephalitis: a case report. Neurol Sci 42, 857–861 (2021). https://doi.org/10.1007/s10072-020-04785-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04785-9