Abstract
Background
Microbiological diagnosis of pulmonary tuberculosis (PTB) is hampered by a low pathogen burden, low compliance and unreliable sputum sampling. Although endobronchial ultrasound-guided transbronchoscopic lung biopsy (EBUS-TBLB) has been found to be useful for the assessment of intrapulmonary nodules in adults, few data are available for the clinical diagnosis of pulmonary tuberculosis. Here, we evaluated EBUS-TBLB as a diagnostic procedure in adult patients with radiologically suspected intrapulmonary tuberculous nodules.
Methods
This was a retrospective analysis of patients admitted with pulmonary nodules between January 2022 and January 2023 at Hangzhou Red Cross Hospital. All patients underwent EBUS-TBLB, and lung biopsy samples were obtained during hospitalization. All samples were tested for Mycobacterium tuberculosis using acid‒fast smears, Bactec MGIT 960, Xpert MTB/RIF, next-generation sequencing (NGS), and DNA (TB‒DNA) and RNA (TB‒RNA). The concordance between different diagnostic methods and clinical diagnosis was analysed via kappa concordance analysis. The diagnostic efficacy of different diagnostic methods for PTB was analysed via ROC curve.
Results
A total of 107 patients were included in this study. Among them, 86 patients were diagnosed by EBUS-TBLB, and the overall diagnostic rate was 80.37%. In addition, 102 enrolled patients had benign lesions, and only 5 were diagnosed with lung tumours. Univariate analysis revealed that the diagnostic rate of EBUS-TBLB in pulmonary nodules was related to the location of the probe. The consistency analysis and ROC curve analysis revealed that NGS had the highest concordance with the clinical diagnosis results (agreement = 78.50%, κ = 0.558) and had the highest diagnostic efficacy for PTB (AUC = 0.778). In addition, Xpert MTB/RIF + NGS had the highest concordance with the clinical diagnosis results (agreement = 84.11%, κ = 0.667) and had the highest efficacy in the diagnosis of PTB (AUC = 0.826).
Conclusion
EBUS-TBLB is a sensitive and safe method for the diagnosis of pathological pulmonary nodules. Xpert MTB/RIF combined with NGS had the highest diagnostic efficacy and can be used in the initial diagnosis of PTB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) is a chronic infectious disease caused by Mycobacterium tuberculosis (MTB) infection [1]. Pulmonary tuberculosis (PTB) is a major public health problem worldwide and one of the ten leading causes of death worldwide [2]. The results of an epidemiological analysis revealed that there were 748,000 new cases of tuberculosis and 52/100,000 cases of tuberculosis in China in 2022 (55/100,000 in 2021) [3]. Among the 30 countries with a high burden of TB worldwide, China ranks third in terms of the number of TB cases, accounting for 7.1% of the global incidence, second only to India (27%) and Indonesia (10%) [3]. Clinical studies have shown that the therapeutic effect of pulmonary tuberculosis is closely related to the timeliness of diagnosis [4]. Smear negativity is more common in patients with tuberculosis who are first diagnosed with pulmonary nodules, especially those without productive cough [5]. Intrapulmonary biopsy is of significant clinical importance in such difficult-to-diagnose patients [6]. In addition, the clinical manifestations of pulmonary tuberculosis are diverse, and individual differences are large and not characteristic, making its diagnosis difficult [7]. Sputum culture is the main diagnostic method, but negative sputum bacteria can only be used as a diagnostic reference and cannot be used as the final diagnostic basis. Bronchoscopic interventional biopsy is the gold standard for the diagnosis of pulmonary tuberculosis, but it is invasive and relatively time consuming. At present, the diagnosis of pulmonary tuberculosis can be made only by excluding other diseases and combining clinical manifestations, imaging and histopathology. Transbronchial lung biopsy (TBLB) is the main examination method for the diagnosis of pulmonary nodules [8]. However, the diagnostic yield of TBLB depends largely on operator experience and the quality of the biopsy samples [8]. When TBLB is unsuccessful, mediastinoscopy is an option, but it is highly invasive and expensive and is not recommended as a routine method for the diagnosis of pulmonary nodules [9]. Therefore, to ensure minimal trauma, it is essential to biopsy the most accessible site.
With the development and progress of medical technology, endobronchial ultrasound-guided transbronchial lung biopsy (EBUS-TBLB) has become an accurate, minimally invasive and safe technique for the diagnosis of peripheral lung lesions [10]. Extensive data have demonstrated the efficacy and safety of EBUS-TBLB in obtaining histopathology data for nodule diagnosis [11]. Tissue acquisition by flexible bronchoscopic sampling is the preferred modality [12]. However, at present, most studies have focused on the pathological analysis of biopsy tissues, and at present, the clinical diagnosis of tuberculosis via lung tissue pathology and lavage fluid specimens is mostly based on comprehensive methods such as bacteriology, immunology, serology and molecular biology [13].
Bacteriological examination provides aetiological evidence for the diagnosis of tuberculosis and is an important basis for the diagnosis of pulmonary tuberculosis [14]. Acid-fast-stained smears are a traditional method of tuberculosis examination, but the positive rate is low, the detection limit is low, and misdiagnosis is easy [15]. Tuberculosis culture is considered the gold standard for the diagnosis of PTB, and its diagnostic sensitivity and specificity are greater than those of the smear method, but the detection cycle is longer [16]. The use of MGIT960 greatly shortens the culture cycle for Mycobacterium tuberculosis and is a widely used rapid culture method [17]. In recent years, fluorescence quantitative PCR has been gradually applied for the detection of tuberculosis because of its rapid and efficient diagnosis [18]. Real-time fluorescent nucleic acid thermostatic amplification detection techniques for DNA (TB-DNA) and RNA (TB-RNA) can indirectly detect the content of tubercle bacilli in samples via qPCR and can also distinguish tuberculosis from nontuberculous bacteria; thus, these methods have been widely popularized [19]. In addition, rifampicin-resistant real-time fluorescence quantitative nucleic acid amplification (Xpert MTB/RIF) and next-generation sequencing (NGS) technology have been widely used in the diagnosis of tuberculosis as the latest molecular diagnostic methods [19].
Therefore, the present study retrospectively analysed the diagnostic results of 107 patients with pulmonary nodules and compared the diagnostic value and advantages of different diagnostic methods for diagnosing pulmonary tuberculosis to provide a reference for the early diagnosis and treatment of pulmonary tuberculosis.
Materials and methods
Study population
This study conducted a retrospective analysis of patients ranging in age from 18 to 65 years via a standardized review of electronic health records from January 2022 to January 2023 at Hangzhou Red Cross Hospital.
The inclusion criteria were as follows: (1) suspected nodules in the periphery of the lung by imaging; (2) underwent EBUS-TBLB and complete pathological examination; and (3) all bronchial lavage samples were submitted for testing using acid-fast staining smears (microscopy), Bactec MGIT 960, Xpert MTB/RIF, NGS, TB-DNA, and TB-RNA.
The exclusion criteria were as follows: (1) patients with prior anti-tuberculosis therapy; (2) contaminated or unqualified biopsy specimens; and (3) the final diagnosis was equivocal.
All patients provided signed informed consent for the bronchial examination and biopsy. The patients’ electronic health records were reviewed for patient data including clinical examination symptoms at presentation, prior history of diagnosis and treatment for tuberculosis, and the anaesthesia regimen of the patients who received EBUS-TBLB.
Instruments
The instruments used in this study were as follows: an Olympus digital colour ultrasound diagnostic device, Olympus Evis mainframe, and ultrasound small probe ultrasonic fibre optic electronic bronchoscope BF-UC260FW (Olympus Corporation, Japan); an endoscopic ultrasound system (MAJ-P35), television imaging system and other supporting equipment (Olympus Corporation, Japan); a 20 MHz intracavitary ultrasound probe (UM-S20-17 S) with an external diameter of 1.4 mm and a guide sheath kit (K201) (Olympus, Japan); and medical image processing software (DirectPath). In addition, the MGIT960 Mycobacterium tuberculosis liquid culture instrument (BD Company, USA), a real-time fluorescent PCR analyser, an Xpert MTB/RIF tuberculosis rapid diagnosis instrument, a Hain tuberculosis rapid diagnosis instrument, and Mycobacterium tuberculosis rapid culture and first- and second-line drug susceptibility technology were used, along with advanced laboratory techniques such as those for the detection of drug resistance genes and nontuberculosis mycobacterium typing.
Diagnostic procedures
Routine preoperative examination data, including haematology, coagulation function, electrocardiogram and thin-slice CT results, were collected from the patients. The patients’ chest CT images, with a slice thickness less than 1 mm, were imported into the virtual navigation software to generate a virtual navigation map. After fasting and abstinence for 6 h and 2 h, respectively, intraoperative continuous oxygen inhalation, electrocardiogram monitoring, haemodynamic parameter monitoring, etc., testing were performed. The patient underwent a tracheoscopic procedure after intravenous inhalation of combined anaesthesia, and the operator used the virtual bronchoscopy navigation system in comparison with navigation under direct bronchoscopy to reach the bronchus with the suspected lesions. The location of the bronchial lesion was determined by assigning tracheal lesion grades, which were recorded from the main bronchus to the alveoli. For each bronchial branch, the tracheal grade at the site of the lesion was incremented by 1. An EBUS probe was then inserted into the suspected bronchus to detect peripheral lung lesions. After localization of the lesions, the guided sheath (GS) was fixed at the entrance of the tracheoscopic biopsy orifice, the operator withdrew the ultrasound probe from the sheath, TBLB was performed 6–8 times via the GS to obtain tissue samples, and the lavage fluid samples were subjected to acid‒fast smears and Bactec MGIT960, Xpert MTB‒RIF, NGS, TB‒DNA and TB‒RNA testing.
Acid fast-stained smear detection
Two volumes of digestive solution were added to the lavage samples, and then shaken thoroughly until there was no floc. The mixture was centrifuged at r/min for 5 min. The supernatants were removed and the remaining pellet samples were smeared, stained, dried, sealed and subjected to microscopic examination.
Specific MGIT 960 detection
A 0.8 mL mixture of nutritional additives and miscellaneous inhibitors was added to the culture tube. A total of 0.5 mL of the lavage solution sample was injected into the above culture tubes, and the tubes were incubated in Bactec MGIT-960 Tb. The instrument automatically outputs the test results.
Xpert MTB/RIF detection
If the volume of lavage solution was less than 5 mL, an equal volume of sample handling solution was added; if the volume of the lavage solution was greater than 5 mL, a portion of the supernatant was discarded by preliminary centrifugation, followed by centrifugation with the above protocol, and finally, the treatment solution was added to the precipitate. Two test samples were added to the kit (Cepheid, USA) using a new pipette and allowed to react adequately; the test results were read in the system test window.
NGS detection
Five millilitres of BALF were centrifuged to enrich for mycobacteria, the supernatant was discarded, and the sample was resuspended in 200 µL of lysate. Two hundred microlitres of sample was added to the beads for physical milling for 1 min. After milling, enzyme solutions such as lysozyme were added for lysis, and the lysate was used for subsequent nucleic acid extraction. The extraction was performed according to the standard method of the QIAamp DNA Microbial Group Kit (Qiagen). The extracted total nucleic acids were collected for independent construction of DNA and RNA libraries for each clinical sample and for nanopore sequencing. The NCBI database was searched for bioinformatics alignment of all sequences, the conserved regions of the sequences were identified, and primers were designed for the conserved regions. Bioinformatic comparison was performed on all the primers; primers such as those related to dimer differences and hairpin structures were removed, and new primers were redesigned until the conditions were met. Gradient touchdown PCR was used to amplify drug resistance genes. The reaction system was 50 µL in total volume and contained 5 µL of nucleic acid extract. The multiplex PCR product was purified by magnetic beads with a magnetic bead ratio of 0.6X and finally eluted with 30 µL of enzyme-free water. The purified products of the multiplex PCR were barcode labelled, and library construction was performed according to the standard method of the nanopore ligation library construction kit. Finally, 100 ng of the final prepared library was used for on-board sequencing, sequencing was performed via the GridION platform, and the sequencing data were acquired in real time via MinKNOW software.
Detection of TB-DNA and TB-RNA from Mycobacterium tuberculosis
The lavage mixture was sealed in a sterile container and subjected to testing; the reaction procedures such as liquefied nucleic acid extraction and PCR amplification were performed according to laboratory operating procedures. s. The results were interpreted according to the following criteria: an MTB-DNA positive result was based on an FAM channel detection Ct value ≤ 38.0; otherwise, the result was negative; and an mTB-RNA positive result was based on a Ct value ≤ 35, whereas 35 < Ct value < 40 warranted a retest, and no Ct value or a Ct value greater than 40 was considered negative.
Diagnostic criteria
A confirmed EBUS-TBLB diagnosis was considered in patients with a positive result for either pathology or aetiology after EBUS-TBLB. Failed EBUS-TBLB diagnosis was considered if the pathological specimen had no typical pathological findings or positive aetiological results after EBUS-TBLB examination, the patient was diagnosed by other means or by an experienced physician on the basis of clinical diagnostic criteria, or patient follow-up for more than 3 months after treatment showed absorption on chest images. A positive aetiological diagnosis was based on positive results for any of the combined indices, whereas a negative aetiological diagnosis was considered when all indices were negative.
Statistical methods
Statistical analysis was performed via SPSS 27.0 software. Age is expressed as the mean ± SD, and other enumeration data are described as percentages. Independent sample t tests and χ2 tests were used to compare the ages of the different groups, and P < 0.05 was considered to indicate statistical significance. Kappa concordance analysis was used to analyse the concordance between the different diagnostic methods and the clinical diagnosis results. The closer the kappa value is to 1, the better the agreement is, and the results were interpreted as follows: 0 < kappa ≤ 0.4 indicated poor agreement; 0.4 < kappa ≤ 0.75 indicated good agreement; and kappa > 0.75 indicated excellent agreement. ROC curves were used to analyse the diagnostic efficacy of the different diagnostic methods for PTB. The closer the area under the curve (AUC) is to 1, the greater the diagnostic power of the model.
Results
Sociodemographic characteristics and preliminary tuberculosis screening results
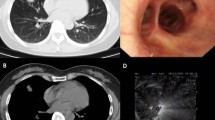
According to the inclusion and exclusion criteria, 107 patients with pulmonary nodules, 84 males and 23 females, with a mean age of 50.20 ± 17.03 years, were included in this study. The demographic characteristics and pulmonary nodule screening results of all included patients are presented in Table S1. There were 22 patients with a history of smoking or alcohol consumption. In addition, a total of 23 patients had underlying diseases, including 5 with hypertension, 12 with diabetes, 3 with hepatitis B, 2 with hypertension and diabetes, and 1 with diabetes mellitus with hepatitis B. The results of the pulmonary nodule screening indicated that 64 patients had nodules localized in the right lung, with 43 in the right upper lobe, 4 in the right middle lobe, and 17 in the right lower lobe. In addition, 42 patients had nodules in the left lung, including 31 in the left upper lobe, 1 in the left middle lobe, and 10 in the left lower lobe. The EBUS-TBLB probe was positioned at the center of the lesion in 58.88% of patients (63 patients), adjacent to the lesions in 34.58% of patients (37 patients), and no lesions were detected in 6.54% of patients (7 patients). Nondiagnostic EBUS-TBLB results revealed that 83.18% (89 patients) of the nodules were nodules or masses, 4.67% (5 patients) were solid shadows, 10.28% (10 patients) were patchy shadows, and 1.87% (2 patients) were ground glass opacities. The tracheal grades of the lesions were mainly grades 5–8, with the largest number of patients being grade 6 (35 patients), followed by grade 7 (30 patients), grade 5 (17 patients), grade 8 (14 patients), and grade 9 (3 patients). The number of patients with tracheal grade 3 lesions was the smallest, only 2. Pulmonary nodules were ≥ 2 cm in diameter in 63 patients. EBUS-TBLB was successfully completed in all patients without significant symptoms of discomfort. Representative patients with pulmonary nodules and suspected pulmonary tuberculosis are presented in Figure S1.
Diagnosis of pulmonary nodules via EBUS-TBLB
Among the 107 patients, 86 achieved a positive diagnosis via EBUS-TBLB, with a comprehensive diagnosis rate of 80.37%. The final diagnoses of the pulmonary nodules are presented in Table S2. All 102 enrolled patients had benign lesions, and only 5 were diagnosed with lung tumours. In addition, EBUS-TBLB diagnosed 80.0% of the lung tumours. Among patients with benign lesions, the diagnostic rate of tuberculosis was 87.0% (9 patients with tuberculosis were not detected), that of pneumonia was 62.5% (3 patients of pneumonia were not detected), that of pulmonary aspergillosis was 100.0%, and that of other benign lesions (mainly NTM lung disease) was 92.9% (1 patient was not detected). In addition, representative EBUS-TBLB image of the patient with pulmonary nodules suspected of pulmonary tuberculosis are shown in Fig. 1.
We subsequently analysed the factors influencing the diagnosis of pulmonary nodules by EBUS-TBLB. As shown in Table 1, the diagnostic yield of EBUS-TBLB for diagnosing pulmonary tuberculosis was not affected by the patient’s age, sex, nodule type, tracheal grade, or lesion size (all P > 0.05). Interestingly, the diagnostic yield of EBUS-TBLB for diagnosing pulmonary nodules correlated with the probe location. Compared with nondetected lesions, probe detection was more favourable for the diagnosis of pulmonary nodules via EBUS-TBLB (P < 0.05).
Representative EBUS-TBLB image of the patient with pulmonary nodules suspected of pulmonary tuberculosis. (A) The ultrasound probe was inserted into the lesion bronchus under the guidance of the guide sheath (GS), and the irregular annular consolidation was detected. The probe was located in the middle of the lesion. (B) The ultrasound probe was inserted into the lesion bronchus under the guidance of the guide sheath (GS). Irregular eccentric consolidation was detected, and the probe was adjacent to the lesion
Diagnostic value of different single diagnostic methods for pulmonary tuberculosis
After EBUS-TBLB pathological diagnosis, further lavage fluid samples were taken for aetiological analysis. On the basis of the final clinical diagnosis, we evaluated the diagnostic value of all single diagnostic modalities for PTB. First, we analysed the concordance between the different single diagnostic modalities and the clinical findings. As shown in Table S3, the concordance rates of microscopy, MGIT, TB-DNA and TB-RNA with the clinical diagnosis results were 48.60%, 51.40%, 61.68%, and 53.27% (all κ < 0.4), respectively, indicating that these diagnostic modalities have poor consistency in the diagnosis of PTB. In addition, the concordance between NGS and clinical diagnosis was the highest, at 78.50% (κ = 0.558), followed by Xpert, with 68.22% concordance (κ = 0.409). In 107 patients with pulmonary nodules, NGS was consistent with the clinical diagnosis in 84 patients and inconsistent in only 23 patients.
The diagnostic efficacy of different single diagnostic modalities for PTB was further analysed via the ROC curve. As shown in Fig. 2; Table 2, microscopy, MGIT, and TB-RNA did not have significant classification ability as diagnostic models for PTB (all P > 0.05). Moreover, the sensitivities of microscopy, MGIT and TB-RNA for the diagnosis of PTB were only 12.90%, 22.58% and 19.38%, respectively, suggesting that these three diagnostic methods have low diagnostic value for PTB. In addition, the classification effect of Xpert, NGS and TB-DNA as diagnostic models for PTB was significant (all P < 0.05). Although the specificity of Xpert and TB-DNA in the diagnosis of PTB was 100.00%, the diagnostic sensitivity was low, at only 45.16% and 37.10%, respectively, suggesting a high misdiagnosis rate for both Xpert and TB-DNA. In addition, the AUC of NGS for diagnosing PTB was as high as 0.778, and the diagnostic sensitivity and specificity were 82.26% and 73.33%, respectively. These results indicate that NGS has the highest efficacy in the diagnosis of PTB among the single diagnostic modalities.
Diagnostic value of different combined diagnostic methods for pulmonary tuberculosis
We subsequently evaluated the diagnostic value of different combined diagnostic modalities for PTB. As shown in Table 3, the concordance kappa values between the PTB diagnosis results and the clinical diagnosis results for the microscopy + Xpert, microscopy + NGS, MGIT + Xpert, MGIT + NGS, Xpert + NGS, Xpert + TB-DNA, Xpert + TB-RNA, NGS + TB-DNA, and NGS + TB-RNA combined methods were all greater than 0.4, suggesting good consistency. The highest concordance with the clinical diagnosis was found for the Xpert + NGS combination (84.11%, κ = 0.667). NGS + TB-DNA and NGS + TB-RNA had the next highest concordance (both agreement = 82.24%, κ = 0.630). In addition, the concordance between all combined diagnostic modalities and the clinical diagnosis results was greater than that between any of the single diagnostic modalities.
The diagnostic efficacy of the different combined diagnostic modalities for PTB was further analysed via the ROC curve. As shown in Fig. 3; Table 4, all the combined diagnostic models improved the diagnostic power for PTB compared with any single diagnostic method alone. Microscopy + MGIT and microscopy + TB-RNA had no significant effect on classification ability (all P > 0.05). Moreover, the sensitivities of the microscopy + MGIT and microscopy + TB-RNA combinations in the diagnosis of PTB were only 27.42% and 24.19%, respectively, suggesting that the diagnostic value of these two combined diagnostic models for PTB was low. The ROC curve revealed that the Xpert + NGS combination had the highest AUC (0.826) for the diagnosis of PTB, and the diagnostic sensitivity was as high as 91.94%, suggesting that the missed diagnosis rate of Xpert + NGS was low. Combined with the results of the concordance analysis, Xpert + NGS was the best combined diagnostic method for PTB.
Discussion
Although studies on the route of transmission and pathogenesis of pulmonary tuberculosis have been well established, the occult nature of tuberculosis infection has led to missed diagnoses in many early-stage patients [20]. The pathological manifestations of tuberculosis are complex and can manifest as nodules, consolidations, lymphadenopathies and other pathological types [21]. For nodular tuberculosis, the size and diameter of a single tuberculous nodule are small and difficult to observe either macroscopically or radiographically [21]. With an increasing number of nodules, multiple tuberculous nodules can coalesce to form larger nodules [21]. In some patients, tuberculous nodules may be isolated, and both imaging similarity to lung tumours and a lack of clinical symptoms in such patients hinder the diagnosis of tuberculosis. Although imaging plays an important role in such sputum-negative, non-sputum-producing patients with suspected tuberculosis, it is still difficult to serve as a direct basis for starting anti-tuberculosis therapy [22,23,24].
Existing diagnostic techniques have their own advantages and disadvantages, but the limited timeliness of the overall diagnosis increases the difficulty of tuberculosis treatment [25]. Ultrasonography, as an important component of medical imaging, has also been used in the diagnosis and treatment of pulmonary tuberculosis [25]. Unlike TBLB, EBUS-TBLB can confirm the puncture site via an ultrasound probe and can accurately and efficiently be used to obtain specific cytological or biopsy samples [26]. EBUS-TBLB allows precise access to the lesion and the acquisition of diseased tissue via preoperative CT modelling as well as real-time ultrasound observation during the procedure [27]. In addition, EBUS-TBLB is considered safe because of its small wound size and low incidence of related complications [28]. Moreover, the introduction of EBUS has resulted in good cost-effectiveness in biopsy sampling and the diagnosis of pulmonary nodules [10]. EBUS-TBLB has been widely used in the diagnosis of pulmonary nodular and neoplastic diseases considering its advantage of high-precision samples for pathological examination [27, 28]. Therefore, this study evaluated the application value of EBUS-TBLB for diagnosing pulmonary nodules via retrospective analysis of patient data, and further analysed the diagnostic value of different aetiological examination methods for diagnosing pulmonary tuberculosis.
Understanding the relationship between the probe and the lesion is important for “visualizing” pulmonary nodules, greatly improves the accuracy of the biopsy tissue, and significantly improves the positive diagnostic rate of pulmonary lesions [29]. Additionally, the study was conducted by bronchoscopists with relevant professional qualifications and at least 10 years of practical experience. This expertise is crucial for preventing complications such as Rasmussen aneurysms in large nodules. If a Rasmussen aneurysm was suspected, the biopsy procedure was immediately halted. The results of this study confirm that the diagnostic yield of EBUS-TBLB for pulmonary nodules is related to probe location. The detection of lesions with the probe is more useful for the diagnosis of pulmonary nodules via EBUS-TBLB than is the absence of lesions. EBUS-TBLB is mainly used to differentiate between benign and malignant pulmonary nodules and masses. In addition, only 5 patients in this study had malignant lesions, and the remaining lesions were benign. Since Herth et al. first used EBUS-guided bronchoscopic lung biopsy in 2007, several studies have shown that EBUS-TBLB has a diagnostic yield of 53–80% for the diagnosis of lung lesions [30,31,32]. A total of 107 patients were included in this study, and a total of 86 patients achieved a positive diagnosis via EBUS-TBLB, with a combined diagnosis rate of 80.37%, which is consistent with the results of previous studies. Interestingly, none of the patients who underwent EBUS-TBLB in this study experienced significant complications. A positive diagnosis was not achieved in some lesions, possibly because (1) the ultrasound probe could not reach the segmental bronchus where the lesion was located; (2) the lesion was close to the visceral pleura and it was difficult for the ultrasound probe to enter the peripheral bronchus; (3) the ultrasound probe could not get close to the lesion because the lesion was far away from the ultrasound probe and could not be displayed; (4) the density of the lesions was low and ground-glass, which is difficult to visualize via the ultrasound probe; or (5) the lesion was a nonsolid lesions, which can interfere with ultrasound imaging because of their low and uneven density and large amount of surrounding air.
Currently, the acid-fast smear method is rapid and straightforward but has limitations, such as its inability to differentiate between nontuberculous mycobacteria and its requirement for a high bacterial count in the sample. Typically, a minimum of 10,000 tubercle bacilli per milliliter is needed for detection. Additionally, the MGIT 960 culture method has a longer incubation period. The Xpert MTB/RIF assay, with a specificity exceeding 95% for MTB detection, serves as a valuable adjunctive diagnostic tool for tuberculosis [33]. However, the sensitivity of Xpert MTB/RIF remains limited in comparison to culture methods and Xpert MTB/RIF itself, necessitating the use of clinical diagnosis as a reference standard when evaluating tuberculosis diagnostic tests. Next-generation sequencing (NGS), a high-throughput sequencing technique, allows for rapid sequencing of DNA or RNA base pairs and is increasingly used in pulmonary tuberculosis diagnosis. Despite this, there is a lack of studies guiding the choice of MTB testing methods for bronchial lavage fluid samples obtained via EBUS-TBLB. In this study, concordance analysis demonstrated that the agreement of Xpert MTB/RIF, NGS, TB-DNA, and TB-RNA with clinical diagnosis was superior to that of microscopy and Bactec MGIT 960, indicating that molecular diagnostic methods outperform traditional culture techniques. NGS exhibited the highest concordance with clinical diagnosis (agreement = 78.50%, κ = 0.558). In comparison, the Xpert MTB/RIF assay showed an agreement of 51.40%, consistent with the findings of Rachow et al. [34]. The PTB assay results indicated that Xpert MTB/RIF had a sensitivity of 45.16% and a specificity of 100.00%, aligning with previous studies [33]. Nonetheless, a PTB meta-analysis reported a pooled sensitivity of 89% and specificity of 99% for Xpert MTB/RIF [35]. The discrepancy may be attributed to the large sample size of 9,557 patients from various countries in the meta-analysis, contrasting with the smaller sample size and potential selection bias of our retrospective study. Additionally, all cases included in this study involved small peripheral lesions, contributing to lower diagnostic sensitivity. Consistent with the concordance analysis results, NGS demonstrated the highest diagnostic efficacy for PTB (ROC AUC = 0.778), with a sensitivity of 82.26% and specificity of 73.33%, indicating its superior clinical diagnostic value among the single diagnostic modalities. Chao et al. reported sensitivity and agreement of NGS at 81.8% and 89.0%, respectively, with a kappa of 0.78, similar to our findings [36]. Conversely, Liu et al. found NGS diagnostic sensitivity to be only 59.9% for PTB, potentially due to the detection of Mycobacterium tuberculosis complex [37].
Combining different detection methods is an effective method to increase the positive rate of PTB aetiological diagnosis. In this study, Xpert MTB/RIF + NGS had the highest concordance with the clinical diagnosis of PTB (agreement = 84.11%, κ = 0.667). NGS + TB-DNA and NGS + TB-RNA were next best (both agreement = 82.24%, κ = 0.630). Consistent with the results of the concordance analysis, Xpert MTB/RIF + NGS had the highest diagnostic AUC for PTB (0.826). In addition, the diagnostic efficacy of any of the combined diagnostic methods for PTB patients was greater than that of any corresponding single diagnostic method, suggesting that combined diagnosis can significantly improve the detection rate of PTB. By comparing the AUC, we confirmed that Xpert MTB/RIF in combination with NGS was the best protocol for the diagnosis of PTB in pathological specimens obtained via EBUS-TBLB.
There are several limitations to this study as follows: (1) due to the need to perform many different diagnostic methods for PTB, this study included few cases and a small sample size; and (2) this study is a retrospective study and can reflect only the research status of this specific research institution during this time period. A prospective multiregional and multicentre cooperative study should be conducted to further test and explore the accuracy of the examined tests; (3) Since the patients included in this study were selected based on a high suspicion of tuberculosis following imaging studies, the findings are not applicable to tuberculosis screening in the general population.
Conclusion
This study confirms the utility, safety, and feasibility of EBUS-TBLB in patients with suspected pulmonary tuberculous nodules on imaging. Of all the single diagnostic modalities, NGS yielded higher MTB positivity in the biopsy results. The combination of NGS and Xpert MTB/RIF showed the highest diagnostic efficacy in the diagnosis of PTB. Therefore, EBUS-TBLB combined with NGS and Xpert MTB/RIF can help to diagnose patients with suspected pulmonary tuberculosis more accurately and can be used as the initial diagnostic method for patients with suspected pulmonary tuberculosis, providing new ideas for the early diagnosis and treatment of pulmonary tuberculosis.
Data availability
Data generated or analyzed during this study are provided in full within the present manuscript.
References
Jia Z, Cheng S, Ma Y, Zhang T, Bai L, Xu W, et al. Tuberculosis burden in China: a high prevalence of pulmonary tuberculosis in household contacts with and without symptoms. BMC Infect Dis. 2014;14:64. https://doi.org/10.1186/1471-2334-14-64.
Sossen B, Richards AS, Heinsohn T, Frascella B, Balzarini F, Oradini-Alacreu A, et al. The natural history of untreated pulmonary tuberculosis in adults: a systematic review and meta-analysis. Lancet Respiratory Med. 2023;11(4):367–79. https://doi.org/10.1016/s2213-2600(23)00097-8.
Margarit A, Simó S, Rozas L, Deyà-Martínez À, Barrabeig I, Gené A, et al. Adolescent tuberculosis; a challenge and opportunity to prevent community transmission. Pediatr (Barc). 2017;86(3):110–4. https://doi.org/10.1016/j.anpedi.2016.03.009.
Teo AKJ, Singh SR, Prem K, Hsu LY, Yi S. Delayed diagnosis and treatment of pulmonary tuberculosis in high-burden countries: a systematic review protocol. BMJ open. 2019;9(7):e029807. https://doi.org/10.1136/bmjopen-2019-029807.
Mustafa H, Shah NN, Shahnawaz M, Yousuf M. Role of Gene Xpert in smear negative pulmonary tuberculosis. Indian J Tuberc. 2022;69(4):552–7. https://doi.org/10.1016/j.ijtb.2021.08.035.
Chen X, Zhao J, Chen L, Chen Y, Liu J. Pulmonary Talaromyces marneffei misdiagnosed as smear-negative pulmonary tuberculosis. Clin Respir J. 2023;17(8):816–8. https://doi.org/10.1111/crj.13661.
Feng JY, Lin CJ, Wang JY, Chien ST, Lin CB, Huang WC, et al. Nucleic acid amplification tests reduce delayed diagnosis and misdiagnosis of pulmonary tuberculosis. Sci Rep. 2022;12(1):12064. https://doi.org/10.1038/s41598-022-16319-8.
Pourabdollah M, Shamaei M, Karimi S, Karimi M, Kiani A, Jabbari HR. Transbronchial lung biopsy: the pathologist’s point of view. Clin Respir J. 2016;10(2):211–6. https://doi.org/10.1111/crj.12207.
Zou X, Zhu Y, Hu Q, Qi Q, Hua H, Fei F, et al. Diagnostic value of ultrasound-guided transbronchial lung biopsy in peripheral tuberculous pulmonary lesions. Diagn Cytopathol. 2022;50(12):572–8. https://doi.org/10.1002/dc.25041.
Lin CK, Fan HJ, Yu KL, Chang LY, Wen YF, Keng LT, et al. Effectiveness of Endobronchial Ultrasound-guided Transbronchial Biopsy Combined with tissue culture for the diagnosis of Sputum Smear-negative pulmonary tuberculosis. Front Microbiol. 2022;13:847479. https://doi.org/10.3389/fmicb.2022.847479.
Lim V, Chin RYZ, Kee A, Ng J, See KC. Diagnostic yield and safety of CP-EBUS-TBNA and RP-EBUS-TBLB under moderate sedation: a single-center retrospective audit. Diagnostics (Basel Switzerland). 2022;12(11). https://doi.org/10.3390/diagnostics12112576.
Hong KS, Lee KH, Chung JH, Shin KC, Jin HJ, Jang JG, et al. Utility of Radial Probe Endobronchial Ultrasound guided Transbronchial Lung Biopsy in Bronchus sign negative Peripheral Pulmonary lesions. J Korean Med Sci. 2021;36(24):e176. https://doi.org/10.3346/jkms.2021.36.e176.
Acharya B, Acharya A, Gautam S, Ghimire SP, Mishra G, Parajuli N, et al. Advances in diagnosis of tuberculosis: an update into molecular diagnosis of Mycobacterium tuberculosis. Mol Biol Rep. 2020;47(5):4065–75. https://doi.org/10.1007/s11033-020-05413-7.
Migliori GB, Caminero Luna J, Kurhasani X, van den Boom M, Visca D, D’Ambrosio L, et al. History of prevention, diagnosis, treatment and rehabilitation of pulmonary sequelae of tuberculosis. Presse Med. 2022;51(3):104112. https://doi.org/10.1016/j.lpm.2022.104112.
Kong L, Xie B, Liu Q, Hua L, Bhusal A, Bao C, et al. Application of acid-fast staining combined with GeneXpert MTB/RIF in the diagnosis of non-tuberculous mycobacteria pulmonary disease. Int J Infect Diseases: IJID: Official Publication Int Soc Infect Dis. 2021;104:711–7. https://doi.org/10.1016/j.ijid.2020.12.091.
Bhirud P, Joshi A, Hirani N, Chowdhary A. Rapid laboratory diagnosis of pulmonary tuberculosis. Int J Mycobacteriology. 2017;6(3):296–301. https://doi.org/10.4103/ijmy.ijmy_61_17.
Sivaramakrishnan G, Subramanyam B, Kumar MP, Golla R, Tripathy SP, Mondal R. Validation of bedaquiline drug-susceptibility testing by BACTEC MGIT 960 system for Mycobacterium tuberculosis. Int J Mycobacteriology. 2019;8(4):329–32. https://doi.org/10.4103/ijmy.ijmy_151_19.
Govindan SA, Yadav R, Vaidya PC, Sethi S, Mehra N, Das RR, et al. Comparison of performances of loop-mediated isothermal amplification, XPERT MTB/RIF and BACTEC MGIT in the diagnosis of childhood tuberculosis. J Paediatr Child Health. 2021;57(6):847–53. https://doi.org/10.1111/jpc.15334.
Zou X, Zhu Y, Qin Y, Fei F, Chen Y, Wang P, et al. Value analysis of next-generation sequencing combined with Xpert in early precise diagnosis of pulmonary tuberculosis. Diagn Microbiol Infect Dis. 2023;107(1):115921. https://doi.org/10.1016/j.diagmicrobio.2023.115921.
Galamay LC, Chee CBE, Khin Mar KW, Lau BQ, Wang YT. Smear-positive pulmonary tuberculosis patients with previously abnormal chest radiographs: missed opportunities for early diagnosis. Singap Med J. 2021;62(6):296–9. https://doi.org/10.11622/smedj.2020027.
Afsar I, Gunes M, Er H, Gamze Sener A. Comparison of culture, microscopic smear and molecular methods in diagnosis of tuberculosis. Rev Esp Quimioter. 2018;31(5):435–8.
Cardona PJ. Pathogenesis of tuberculosis and other mycobacteriosis. Enfermedades infecciosas y microbiologia clinica. (English ed). 2018;36(1):38–46. https://doi.org/10.1016/j.eimc.2017.10.015.
Bouzeyen R, Javid B. Therapeutic vaccines for tuberculosis: an overview. Front Immunol. 2022;13:878471. https://doi.org/10.3389/fimmu.2022.878471.
Liebenberg D, Gordhan BG, Kana BD. Drug resistant tuberculosis: implications for transmission, diagnosis, and disease management. Front Cell Infect Microbiol. 2022;12:943545. https://doi.org/10.3389/fcimb.2022.943545.
Yan L, Xiao H, Zhang Q. Systematic review: Comparison of Xpert MTB/RIF, LAMP and SAT methods for the diagnosis of pulmonary tuberculosis. Tuberc (Edinb Scotl). 2016;96:75–86. https://doi.org/10.1016/j.tube.2015.11.005.
Huang CT, Tsai YJ, Ho CC, Yu CJ. Atypical cells in pathology of endobronchial ultrasound-guided transbronchial biopsy of peripheral pulmonary lesions: incidence and clinical significance. Surg Endosc. 2019;33(6):1783–8. https://doi.org/10.1007/s00464-018-6452-1.
Zhan P, Zhu QQ, Miu YY, Liu YF, Wang XX, Zhou ZJ, et al. Comparison between endobronchial ultrasound-guided transbronchial biopsy and CT-guided transthoracic lung biopsy for the diagnosis of peripheral lung cancer: a systematic review and meta-analysis. Translational lung cancer Res. 2017;6(1):23–34. https://doi.org/10.21037/tlcr.2017.01.01.
Lee J, Kim C, Seol HY, Chung HS, Mok J, Lee G, et al. Safety and Diagnostic Yield of Radial Probe Endobronchial Ultrasound-guided biopsy for peripheral lung lesions in patients with idiopathic pulmonary fibrosis: a Multicenter cross-sectional study. Respiration. 2022;101(4):401–7. https://doi.org/10.1159/000520034.
Xia Y, Li Q, Zhong C, Wang K, Li S. Inheritance and innovation of the diagnosis of peripheral pulmonary lesions. Ther Adv Chronic Dis. 2023;14:20406223221146723. https://doi.org/10.1177/20406223221146723.
Herth FJ, Ernst A, Becker HD. Endobronchial ultrasound-guided transbronchial lung biopsy in solitary pulmonary nodules and peripheral lesions. Eur Respir J. 2002;20(4):972–4. https://doi.org/10.1183/09031936.02.00032001.
Zaric B, Stojsic V, Sarcev T, Stojanovic G, Carapic V, Perin B, et al. Advanced bronchoscopic techniques in diagnosis and staging of lung cancer. J Thorac Dis. 2013;5(Suppl 4):S359–70. https://doi.org/10.3978/j.issn.2072-1439.2013.05.15.
Tay JH, Irving L, Antippa P, Steinfort DP. Radial probe endobronchial ultrasound: factors influencing visualization yield of peripheral pulmonary lesions. Respirology. 2013;18(1):185–90. https://doi.org/10.1111/j.1440-1843.2012.02276.x.
Organization WH, WHO Guidelines Approved by the Guidelines Review Committee. Automated real-time nucleic acid amplification technology for Rapid and Simultaneous Detection of Tuberculosis and Rifampicin Resistance: Xpert MTB/RIF assay for the diagnosis of pulmonary and extrapulmonary TB in adults and children. Policy Update. Geneva; 2013.
Rachow A, Zumla A, Heinrich N, Rojas-Ponce G, Mtafya B, Reither K, et al. Rapid and accurate detection of Mycobacterium tuberculosis in sputum samples by Cepheid Xpert MTB/RIF assay–a clinical validation study. PLoS ONE. 2011;6(6):e20458. https://doi.org/10.1371/journal.pone.0020458.
Steingart KR, Henry M, Laal S, Hopewell PC, Ramsay A, Menzies D, et al. Commercial serological antibody detection tests for the diagnosis of pulmonary tuberculosis: a systematic review. Postgrad Med J. 2007;83(985):705–12.
Chao Y, Li J, Gong Z, Li C, Ye M, Hong Q, et al. Rapid discrimination between tuberculosis and sarcoidosis using next-generation sequencing. Int J Infect Dis. 2021;108:129–36. https://doi.org/10.1016/j.ijid.2021.05.028.
Liu X, Chen Y, Ouyang H, Liu J, Luo X, Huang Y, et al. Tuberculosis diagnosis by Metagenomic Next-generation sequencing on Bronchoalveolar Lavage Fluid: a cross-sectional analysis. Int J Infect Dis. 2021;104:50–7. https://doi.org/10.1016/j.ijid.2020.12.063.
Funding
This work was supported by the following funds: 1. Hangzhou biomedical and health industry development support science and technology special project. (2023WJC100). 2. Zhejiang Provincial Health Science and Technology Plan, the application value of ultrasound bronchoscopy frozen lung biopsy combined with Xpert in tuberculous peripheral lung lesions. (2022KY989).
Author information
Authors and Affiliations
Contributions
XWZ and HMX: Conceptualization, Data analysis, Methodology, Writing-original draft; QH: Methodology, Software, Validation, Writing - review & editing; QQ, XQM and QSC: Data analysis, Validation, Writing - review & editing; YLZ: Conceptualization, Supervision, Writing - review & editing. All authors read and approved the final manuscript. All authors agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance with the tenets of the Helsinki Declaration, and has been approved by the ethnical committee of Hangzhou Red Cross Hospital.
Consent for publication
All participants were consent for the publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zou, X., Xu, H., Hu, Q. et al. Diagnostic efficacy of endobronchial ultrasound-guided transbronchoscopic lung biopsy for identifying tuberculous nodules. BMC Infect Dis 24, 861 (2024). https://doi.org/10.1186/s12879-024-09761-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09761-8