Abstract
Background paecilomyces
and Penicillium are considered as rare opportunistic pathogens in immunocompromised hosts, and pneumonia caused by Paecilomyces and Penicillium is rare. In this study, we present first case of severe pneumonia with pleural effusion caused by co-infection of Paecilomyces variotii (P. variotii) and Penicillium oxalicum (P. oxalicum) in a 66-year-old female with poorly controlled type 2 diabetes.
Case presentation
A 56-year-old woman patient presented to hospital for nausea, poor appetite, and vomiting for one day. On the second day of admission, blood culture and renal puncture fluid culture grew multidrug-resistant Escherichia coli (imipenem/cilastatin sensitive), and she received combination therapy with imipenem/cilastatin (1 g, every 8 h) and vancomycin (0.5 g, every 12 h). On the fourth day, she developed symptoms of respiratory failure. Pulmonary computed tomography (CT) showed an increase in pneumonia compared to before, with minor pleural effusion on both sides. Two fungi were isolated repeatedly from BALF culture, which were confirmed as P. variotii and P. oxalicum by Internal transcribed spacer (ITS) sequencing. Her pleural effusion was completely absorbed, pneumonia symptoms have significantly improved and discharged with receiving liposomal amphotericin B treatment for four weeks.
Conclusions
It is worth noting that clinicians and laboratory personnel should not simply consider Paecilomyces and Penicillium species as contaminants, especially in immunocompromised patients. Early fungal identification and antifungal drug sensitivity are crucial for clinical drug selection and patient prognosis.
Similar content being viewed by others
Introduction
P. variotii is a common environmental mould that is widespread in composts, soils and food products [1]. P. variotii is an emerging causative agent of hyalohyphomycosis in the immunocompromised patient [1]. P. variotii is associated with various types of infections in humans, with the most common sites affected being the peritoneum and the lungs [2]. It has also been reported to cause bloodstream infections [3], central nervous system infections [4], infective endocarditis [5], endophthalmitis [6], skin and soft tissue infections [7]. These infections can be life-threatening, particularly in critically ill patients with weakened immune systems or those with indwelling medical devices [2]. Penicillium is one of the most common fungi in the environment and is rarely a pathogen in humans. However, it has been increasingly recognized as an opportunistic pathogen in immunocompromised hosts, causing endophthalmitis [8], pulmonary infections [9], endocarditis [10], osteomyelitis [11], skin infections [12], and disseminated infections [13]. We present first case of severe pneumonia with pleural effusion caused by co-infection of P. variotii and P. oxalicum in a 56-year-old female with poorly controlled type 2 diabetes.
Case presentation
A 56-year-old woman patient presented to the emergency department of the People’s Hospital of Guangxi Zhuang Autonomous Region, China, due to nausea, poor appetite, and vomiting for one day. She had a history of poorly controlled type 2 diabetes for 5 years and hypertension for 10 years. Physical examination revealed fever, with 40 °C temperature peak, low blood pressure (63/39mmHg), and a palpable 6 × 4 cm mass in the lower abdomen. Laboratory results showed leukocytosis (24.48 × 10^9/L), thrombocytopenia (78 × 10^9/L), C-reactive protein of > 200.00 mg/L, Procalcitonin of > 50.00ng/ml, IL-6 of 532.00pg/ml, heparin binding protein of 124.8ng/ml and poor glycemic control (Glu 25.2 mmol/L, HbA1c 11.5%). She was diagnosed with diabetes ketoacidosis. Due to the severity of her condition, she was admitted to the ICU. Chest CT showed bilateral lungs minimal inflammation, and focal fibrotic opacities. Abdominal CT revealed right kidney enlargement and air accumulation, considering infectious lesion, not excluding emphysematous pyelonephritis; free gas is seen in the right kidney anterior compartment, considering lesion rupture. She received fluid infusion to improve circulation and active blood glucose control, combine with continuous pumping of norepinephrine 1ug/kg/min, hydrocortisone 2.5ug/kg/min and dobutamine 5ug/kg/min to maintain blood pressure. Cefoperazone sulbactam and teicoplanin were used for empirical anti-infection treatmen. Continuous renal replacement therapy and kidney puncture fistula surgery was performed at the bedside due to infection, reduced urine volume, acidosis, renal insufficiency and high lactate.
On the second day of admission, blood culture and renal puncture fluid culture grew multidrug-resistant Escherichia coli (imipenem/cilastatin sensitive), suggesting a bloodstream infection of urinary tract origin. Given the high risk of catheter-related infection due to multiple invasive procedures, the anti-infection plan was modified to include combination therapy with imipenem/cilastatin (1 g, every 8 h) and vancomycin (0.5 g, every 12 h), which can cover Gram-positive bacteria, along with continuous drainage of renal infection site and used Extracorporeal Membrane Oxygenation (ECMO) to provide continuous extracorporeal respiration and circulation for patient.
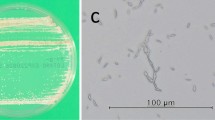
On the fourth day, she developed symptoms of respiratory failure. Chest radiography suggested pneumonia in the right lower lung and pleural effusion on the right side (Fig. 1A). Pulmonary CT showed an increase in pneumonia compared to before, with minor pleural effusion on both sides (Fig. 1B). The next day, the Gram staining of bronchoalveolar lavage fluid (BALF) revealed two different microscopic forms of hyphae (Fig. 2A and B). BALF culture showed two kinds of filamentous fungi grew on blood agar (Fig. 2C) and Sabouraud dextrose agar (Fig. 2D) after incubating at 35 °C for 48 h, of which one was yellow-brown colony (R30383), the other colony changed from white to green (R30383-1). Lactophenol cotton blue staining of the yellow-brown colony showed phialides are cylindrical or ellipsoidal, tapering abruptly into a long and cylindrical neck; conidia are subspherical, ellipsoidal to fusiform, hyaline, smooth-walled, and are produced in long divergent chains, which was suspected to be P. variotii (Fig. 2E). White to green colonies was suspected to be Penicillium based on flask-shaped phialides bear long unbranched chains of almost round conidia, with characteristic penicillus or brush appearance of the entire structure on the lactophenol cotton blue stain (Fig. 2F). Voriconazole was added for antifungal treatment.
The isolates obtained were identified by Internal transcribed spacer (ITS) sequencing. DNA extraction according to the manufacturer’s protocols of the fungal genomic DNA extraction kit produced by Jiangsu Kangwei Century Biotechnology Co., Ltd. Paecilomyces variotii primer pair ITS1 (5′- CATACGCTCGAGGATCGGAC-3′) and ITS4 (5′- AGCGTCATTGCTAACCCTCC-3′). Penicillium oxalicum primer pair ITS1 (5′-TGAAGAACGCAGCGAAATGC-3′) and ITS4 (5′-CTACAGAGCGGGTGACGAAG-3′). The obtained nucleotide sequence was compared with the nearest sequence at the National Center for Biotechnology Information GenBank database. The first homology sequence presenting the highest identity of R30383 was 100% nucleotide identity with Paecilomyces variotii (GenBank No.AY753336.1), and R30383-1 was 100% nucleotide identity with Penicillium oxalicum (GenBank No.OR342233.1). Maximum-likelihood phylogenetic tree based on the ITS sequences showing the relationship of isolated strain R30383 (Fig. 3) and R30383-1 (Fig. 4) with members within their genus, respectively.
On the 7th and 8th day of admission, P. variotii and P. oxalicum were isolated repeatedly from BALF culture. However, on the 9th day of admission, it was observed that the patient was still experiencing significant difficulty in breathing and continued to have a persistently high fever. Multiple blood culture and urine culture negative. Furthermore, it was noticed that there was a noticeable progression in the severity of the pneumonia, with the consolidation and inflammation in the lungs worsening in comparison to the initial stages of the illness. Antifungal susceptibility testing was performed according to Clinical and Laboratory Standards Institute 38 methods, determining minimum inhibitory concentrations (MICs) of P. variotii and Penicillium oxalicum after 48 h incubation were illustrated in Table 1. According to the results of antifungal susceptibility, the antimicrobial treatments plan was revised to include amphotericin B cholesterol sulfate 400 mg/d (6 mg/kg/d, patient weight: 66.7 kg) for antifungal treatment. After four weeks of treatment, bilateral pneumonia had noticeably resolved compared to before, with complete absorption of pleural effusion, indicating improvement in the condition and the patient discharged.
A, B The Gram staining of bronchoalveolar lavage fluid (BALF) revealed two different microscopic forms of hyphae. C, D: BALF culture showed two kinds of filamentous fungi grew on blood agar (C) and Sabouraud dextrose agar (D) after incubating at 35 °C for 48 h, of which one was yellow-brown colony, the other colony changed from white to green. E Lactophenol cotton blue staining of the yellow-brown colonies showed phialides are cylindrical or ellipsoidal, tapering abruptly into a long and cylindrical neck; conidia are subspherical, ellipsoidal to fusiform, hyaline, smooth-walled, and are produced in long divergent chains, which was suspected to be P. variotii.F White to green colonies was suspected to be Penicillium based on flask-shaped phialides bear long unbranched chains of almost round conidia, with characteristic penicillus or brush appearance of the entire structure on the lactophenol cotton blue stain
Discussion and conclusions
Paecilomyces spp. is rare yet clinically significant pathogen and its infection cases have been gradually increasing in recent years. Paecilomyces genus includes several species, with Purpureocillium lilacinum (synonymy: Paecilomyces lilacinus) and P. variotii being the two most commonly associated with human diseases. The most frequent predisposing factor was presence of indwelling devices, particularly peritoneal catheters and prosthetic heart valve, and other predisposing factors included hematologic malignancies, solid organ transplantation, and diabetes [2]. P. variotii-related prosthetic heart valve infections and peritoneal dialysis-associated infections are most commonly seen in immunocompetent hosts, but P. variotii pneumonia is most frequently observed in solid organ transplant patients and diabetes patients [2]. Symptoms of P. variotii pneumonia are often non-specific, presenting fever, dyspnea and hypoxemia, which was difficult to distinguish from other fungal infections [2, 14]. Chest CT demonstrates nodules, ground-glass patchy consolidations and pleural effusion [15, 16].
P. lilacinus and P. variotii display similar morphological characteristics, but their susceptibility to drugs differs significantly. Thus, accurate identification of the specific species is vital for effective treatment. A multicenter study of in vitro antifungal susceptibility of 70 isolates Paecilomyces/Purpureocillium species isolated from clinical respiratory samples illustrated all P. lilacinum isolates showed growth inhibition at high MICs of amphotericin B (> 8 mg/L) and high minimal effective concentrations of echinocandins [17]. In contrast, P. variotii was exhibited low MICs of amphotericin B (≤ 0.5 mg/L), but their response to echinocandins was drug-dependant [17]. For azole drugs, posaconazole showed the best in vitro activity against P. lilacinum and P. variotii, with MICs ≤ 0.5 mg/L. Voriconazole and itraconazole were active in vitro against P. lilacinum, but showed poor in vitro activity against P. variotii [17]. In our case, P. variotii is sensitive to amphotericin B, but the mic value of voriconazole is very high. Meanwhile, the patient’s symptoms did not improve during treatment with voriconazole. Based on existing in vitro and clinical data, liposomal amphotericin B is recommended as first-line monotherapy for Paecilomyces infection, with posaconazole as salvage therapy [18]. Therefore, using posaconazole for empirical treatment may be a good choice when definitive species identification has not been confirmed, as in vitro data indicate that posaconazole exhibits good sensitivity against P. lilacinus and P. variotii [19]. Due to the lack of treatment guidelines, the duration of treatment must be adjusted based on clinical response. The clinical characterizations of P. variotii pneumonia described in the medical literature (Table 2).
Clinically isolated penicillium, which is commonly viewed as a “contaminant”, can actually be a pathogenic organism in individuals with weakened immune systems. It is important for both clinicians and microbiologists to recognize the potential for severe and potentially fatal penicillium infections. A review of 45 cases of invasive fungal infections caused by penicillium indicated that the majority of these cases were associated with invasive pulmonary infections [13, 24,25,26,27,28,29]. The specific penicillium species reported to cause pulmonary infections include P. citrinum [13], P. chrysogenum [24], P. digitatum [25], P. janthinellum [26], P. oxalicum [27], P. notatum [28], and P. capsulatum [29]. Factors that increase the risk of infection include systemic lupus erythematosus (SLE), diabetes, hematologic malignancies, and HIV [13, 24,25,26,27,28,29]. Interestingly, P. oxalicum, which is typically a pathogenic organism that affects plants, has recently been identified as a causative agent of invasive fungal disease. In 2015, Anuradha Chowdhary et al. reported three cases of invasive fungal disease caused by P. oxalicum in patients with acute myeloid leukemia, diabetes, and chronic obstructive pulmonary disease [27]. Furthermore, a study conducted by Lyratzopoulos et al. demonstrated that penicillium can cause a range of lung diseases, including disseminated parenchymal infection, lobar pneumonia, localized granuloma, fungus balls, bronchiolitis obliterans, pneumonia, and pleural effusion [30].
It is worth noting that currently reported strains of penicillium have shown higher MICs for voriconazole, a commonly used antifungal medication [27]. Antifungal susceptibility of 39 isolates of Penicillium species from clinical samples in the United States showed terbinafine and the echinocandins showed the best in vitro activity against Penicillium species [31]. Amphotericin B showed intermediate antifungal activity, while the azoles showed various levels of activity [31]. As a result, voriconazole should not be considered as the first-line empirical treatment option for penicillium infections. While there are currently no standardized treatment guidelines for penicillium infections, liposomal amphotericin B is the preferred treatment option [15]. The potent in vitro activity of echinocandins and terbinafine against Penicillium species might offer a good therapeutic alternative for the treatment of infections caused by these fungi [31]. Voriconazole, posaconazole, and itraconazole may be considered as alternative treatment options if they demonstrate susceptibility to the specific penicillium strains in vitro [15, 31].
According to our report, this case represents the first report of pneumonia and pleural effusion caused by a mixed infection of P. variotii and P. oxalicum, with poorly controlled type 2 diabetes and indwelling catheters as the main risk factors for infection. It is worth noting that clinicians and laboratory personnel should not simply consider Paecilomyces and Penicillium species as contaminants, especially in immunocompromised patients. Early fungal identification and antifungal drug sensitivity are crucial for clinical drug selection and patient prognosis.
Data availability
The sequencing data of the isolated Paecilomyces variotii (R30383) and Penicillium oxalicum (R30383-1) have been deposited into the National Center for Biotechnology Information GenBank database. GenBank accession number for Paecilomyces variotii (R30383) nucleotide sequences was PP892052. GenBank accession number for Penicillium oxalicum (R30383-1) nucleotide sequences was PP892053. The datasets generated and/or analysed during the current study are available in the National Center for Biotechnology Information GenBank database.
References
Houbraken J, Verweij PE, Rijs AJ, Borman AM, Samson RA. Identification of Paecilomyces Variotii in clinical samples and settings. J Clin Microbiol. 2010;48(8):2754–61.
Sprute R, Salmanton-García J, Sal E, Malaj X, Falces-Romero I, Hatvani L, Heinemann M, Klimko N, López-Soria L, Meletiadis J, et al. Characterization and outcome of invasive infections due to Paecilomyces Variotii: analysis of patients from the FungiScope® registry and literature reports. J Antimicrob Chemother. 2021;76(3):765–74.
Bellanger AP, Cervoni JP, Faucher JF, Weil-Verhoeven D, Ginet M, Deconinck E, Grenouillet F. Paecilomyces Variotii Fungemia in a patient with Lymphoma needing liver transplant. Mycopathologia. 2017;182(7–8):761–5.
Kantarcioğlu AS, Hatemi G, Yücel A, De Hoog GS, Mandel NM. Paecilomyces Variotii central nervous system infection in a patient with cancer. Mycoses. 2003;46(1–2):45–50.
Senior JM, Saldarriaga C. [Endocarditis due to infection by Paecilomyces Variotii]. Biomedica. 2009;29(2):177–80.
Anita KB, Fernandez V, Rao R. Fungal endophthalmitis caused by Paecilomyces Variotii, in an immunocompetent patient, following intraocular lens implantation. Indian J Med Microbiol. 2010;28(3):253–4.
Vasudevan B, Hazra N, Verma R, Srinivas V, Vijendran P, Badad A. First reported case of subcutaneous hyalohyphomycosis caused by Paecilomyces Variotii. Int J Dermatol. 2013;52(6):711–3.
Kanda K, Takayama K, Enoki T, Takeuchi M. Chronic postcataract endophthalmitis caused by Penicillium species in an immunocompetent patient. Int Med case Rep J. 2018;11:259–62.
Beena H, Gupta M, Kindo AJ. Pulmonary infection with Penicillium Citrinum in a patient with multiple myeloma. Indian J Med Microbiol. 2021;39(2):259–61.
DelRossi AJ, Morse D, Spagna PM, Lemole GM. Successful management of Penicillium endocarditis. J Thorac Cardiovasc Surg. 1980;80(6):945–7.
Santos PE, Piontelli E, Shea YR, Galluzzo ML, Holland SM, Zelazko ME, Rosenzweig SD. Penicillium piceum infection: diagnosis and successful treatment in chronic granulomatous disease. Med Mycol. 2006;44(8):749–53.
López-Martínez R, Neumann L, González-Mendoza A. Case report: cutaneous penicilliosis due to Penicillium Chrysogenum. Mycoses. 1999;42(4):347–9.
Mok T, Koehler AP, Yu MY, Ellis DH, Johnson PJ, Wickham NW. Fatal Penicillium Citrinum pneumonia with pericarditis in a patient with acute leukemia. J Clin Microbiol. 1997;35(10):2654–6.
Feldman R, Cockerham L, Buchan BW, Lu Z, Huang AM. Treatment of Paecilomyces Variotii pneumonia with posaconazole: case report and literature review. Mycoses. 2016;59(12):746–50.
Jacobs SE, Wengenack NL, Walsh TJ. Non-aspergillus Hyaline molds: emerging causes of sino-pulmonary fungal infections and other Invasive mycoses. Semin Respir Crit Care Med. 2020;41(1):115–30.
Abolghasemi S, Tabarsi P, Adimi P, Kiani A, Dolatshahi S, Mansouri D. Pulmonary paecilomyces in a Diabetic patient. Tanaffos. 2015;14(4):268–71.
Monpierre L, Aït-Ammar N, Valsecchi I, Normand AC, Guitard J, Riat A, Huguenin A, Bonnal C, Sendid B, Hasseine L et al. Species identification and in Vitro Antifungal susceptibility of Paecilomyces/Purpureocillium species isolated from clinical respiratory samples: a Multicenter Study. J fungi (Basel Switzerland) 2022, 8(7).
Chamilos G, Kontoyiannis DP. Voriconazole-resistant disseminated Paecilomyces variotii infection in a neutropenic patient with leukaemia on voriconazole prophylaxis. J Infect. 2005;51(4):e225–228.
Hoenigl M, Salmanton-García J, Walsh TJ, Nucci M, Neoh CF, Jenks JD, Lackner M, Sprute R, Al-Hatmi AMS, Bassetti M, et al. Global guideline for the diagnosis and management of rare mould infections: an initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect Dis. 2021;21(8):e246–57.
Byrd RP, Roy TM, Fields CL, Lynch JA. Paecilomyces Varioti pneumonia in a patient with diabetes mellitus. J Diabetes Complicat. 1992;6(2):150–3.
Das A, MacLaughlin EF, Ross LA, Monforte HL, Horn MV, Lam GL, Mason WH. Paecilomyces Variotii in a pediatric patient with lung transplantation. Pediatr Transplant. 2000;4(4):328–32.
Steiner B, Aquino VR, Paz AA, Silla LM, Zavascki A, Goldani LZ. Paecilomyces variotii as an Emergent Pathogenic Agent of Pneumonia. Case Reports in Infectious Diseases 2013, 2013:273848.
Asif AA, Roy M, Ahmad S. Paecilomyces Pneumonia despite Voriconazole Prophylaxis: a Case Report and Literature Review. Eur J case Rep Intern Med. 2021;8(7):002651.
D’Antonio D, Violante B, Farina C, Sacco R, Angelucci D, Masciulli M, Iacone A, Romano F. Necrotizing pneumonia caused by Penicillium Chrysogenum. J Clin Microbiol. 1997;35(12):3335–7.
Oshikata C, Tsurikisawa N, Saito A, Watanabe M, Kamata Y, Tanaka M, Tsuburai T, Mitomi H, Takatori K, Yasueda H, et al. Fatal pneumonia caused by Penicillium digitatum: a case report. BMC Pulm Med. 2013;13:16.
Li X, Zong L, Zhu Y, Li Y, Zhou Y, Zhou H. Penicillium Janthinellum Pneumonia in an SLE patient: a Case Study. Infect drug Resist. 2020;13:2745–9.
Chowdhary A, Kathuria S, Agarwal K, Sachdeva N, Singh PK, Jain S, Meis JF. Voriconazole-resistant Penicillium oxalicum: an Emerging Pathogen in Immunocompromised hosts. Open Forum Infect Dis. 2014;1(2):ofu029.
Shokouhi S, Tehrani S, Hemmatian M. Mixed pulmonary infection with Penicillium notatum and pneumocystis jiroveci in a patient with Acute myeloid leukemia. Tanaffos. 2016;15(1):53–6.
Chen M, Houbraken J, Pan W, Zhang C, Peng H, Wu L, Xu D, Xiao Y, Wang Z, Liao W. Pulmonary fungus ball caused by Penicillium Capsulatum in a patient with type 2 diabetes: a case report. BMC Infect Dis. 2013;13:496.
Lyratzopoulos G, Ellis M, Nerringer R, Denning DW. Invasive infection due to penicillium species other than P. Marneffei. J Infect. 2002;45(3):184–95.
Guevara-Suarez M, Sutton DA, Cano-Lira JF, García D, Martin-Vicente A, Wiederhold N, Guarro J, Gené J. Identification and Antifungal susceptibility of Penicillium-Like Fungi from Clinical samples in the United States. J Clin Microbiol. 2016;54(8):2155–61.
Acknowledgements
We would like to acknowledge the reviewers for their helpful comments on this paper.
Funding
This study was supported by the Guangxi Natural Science Foundation under Grant No. 2024GXNSFBA010122.
Author information
Authors and Affiliations
Contributions
Xiuri Wang contributed to the data collection, wrote the manuscript. Yunxiao Liang and Xingchun Chen contributed to the data collection. Liuyang Hu contributed to critical revision and gave final approval of the clinical picture. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the medical ethics committee of The People’s Hospital of Guangxi Zhuang Autonomous Region. We identified this patient during routine clinical practice and the patient consented to participate. Written informed consent was obtained from the patient for publication of this case report.
Consent for publication
Written informed consent was obtained from the patien for the publication of the case details.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, X., Chen, X., Liang, Y. et al. Severe pneumonia with pleural effusion caused by co-infection of Paecilomyces variotii and Penicillium oxalicum in a diabetic patient. BMC Infect Dis 24, 605 (2024). https://doi.org/10.1186/s12879-024-09496-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09496-6