Abstract
Histoplasmosis is a fungal infection most frequently seen in immunocompromised patients. It is endemic in Central and South America and in Africa. The infection is usually asymptomatic in a healthy individual. Extrapulmonary dissemination can be seen in immunocompromised hosts. Gastrointestinal manifestations frequently involve the terminal ileum and cecum, mimicking Crohn’s disease or malignancy. We describe the case of a 36-year-old healthy man from Cameroon, living in Switzerland for 13 years and without any medical nor surgical history, who presented peritonitis not responding to antibiotics. CT-scan showed bowel obstruction and signs of peritonitis. We opted for an explorative laparoscopy, which was converted to laparotomy with extensive adhesiolysis. Diagnostic of histoplasmosis was confirmed by histology and PCR analysis on biopsy. To our knowledge, this is the first described case of peritonitis as main outcome of a disseminated histoplasmosis involving the peritoneum in an immunocompetent patient.
Similar content being viewed by others
Background
Histoplasmosis is a fungal infection most frequently seen in immunocompromised patients or at extreme ages (weaker immune systems). It is endemic in areas such as Central and South America and is present around Mississippi river and in the Ohio River Valley region. It is also present in Sub-Saharan countries [1, 2]. It is transmitted by inhalation of spores of the fungus Histoplasma capsulatum that are present in birds or bats feces. In a healthy individual, the infection is usually asymptomatic or can cause flu-like syndrome [3]. In immunocompromised hosts it can rapidly spread to the lung leading to respiratory failure or extrapulmonary dissemination. This form is called disseminated histoplasmosis. Gastrointestinal manifestations are less frequent and involve mostly the terminal ileum and cecum, mimicking Crohn’s disease or malignancy. The treatment is based on Itraconazole for cases of mild to moderate severity and Amphotericin B for the most severe cases. This case report concerns an immunocompetent patient with peritoneal involvement.
Case history
A healthy 36-year-old man from Cameroun living in Switzerland for 13 years and without any medical nor surgical history, suffered of a worsening abdominal pain with bloating, vomiting and feeling feverish. Patient was immunocompetent, has no diabetes and is non-smoker. An abdominal CT-scan (Fig. 1) was performed showing infiltration of mesenteric fat and reactive mesenteric nodes with free abdominal fluid. A left-sided colitis was diagnosed, and the patient received a week of oral Amoxicillin/ clavulanic acid 1 g TID. A colonoscopy was scheduled 6 weeks later. Due to worsening of pain associated to perspiration, the patient presented himself to our emergency department 2 days later.
He described periumbilical pain with radiation to the left iliac fossa. It was the first time he had experienced this kind of pain. He described abdominal discomfort for a few months without diarrhea or weight loss. He worked as a scaffolding aid and did not leave Europe since he last visited Cameroun 13 years ago.
On examination, the abdomen was distended and painful to left abdominal palpation. He didn’t have fever and vital parameters were normal.
The blood test showed a CRP at 134 mg/L (N: <5) without leukocytosis (N: 4–10 G/L) and a slight alteration of liver function tests (ALAT at 88 U/L (N: <50) and gammaGT at 221 U/L) (N: 60)).
A new abdominal CT-scan (Fig. 2a and b) found a paralytic ileus picture with jejunal dilation and increased intra-abdominal effusion with signs of peritonitis. The peritoneum seemed to form a shell around all the intestinal loops. It also showed a pancolonic diverticulosis, diverticulitis could not be excluded. The patient was hospitalised for intravenous antibiotic, Ceftriaxone 2 g OD and Metronidazole 500 mg TID. Stool cultures including parasite screening were negative. Bloodwork follow-up showed an improvement of the inflammatory parameters. Given the clinical improvement, he was discharged with an oral treatment of ciprofloxacin 500 mg BID and metronidazole 500 mg TID for a total of 10 days.
Four weeks after the hospitalisation, he came back to the emergency with recurrence of strong abdominal pain and left guarding. He still had no fever, and vital signs were stable. Blood tests showed no inflammation and liver tests showed only a slight elevated gammaGT (leukocytes 5.2 G/L, CRP 3.9 mg/L, GGT 93 U/L). A new CT scan was performed (Fig. 3a and b), showing a worsening of the ileus and slightly less free fluid compared to the previous CT scan. Additional analyses were done, including Interferon-Gamma Release Assays for tuberculosis infection, stool cultures for Salmonella, Shigella, Campylobacter, and 3 search of parasites, that were all negative. The punction of free intraabdominal fluid was cultivated, which came back negative for bacteria, fungi, and mycobacteria. Unfortunately, no cell counts, nor biochemical analysis were performed. As the patient’s status was worrisome and not improving, a laparoscopic exploration was scheduled.
Material and surgical technique
Laparoscopic exploration was performed in the supine position and under general anaesthesia. We first opted for a laparoscopic approach due to a significant adhesion status, a midline laparotomy was performed. Bloody serous fluid was collected for microbiological cultures and peritoneal biopsies were sent for anatomo-pathologic examination. The entire small intestine was surrounded by a thick fibrous membrane, making the loops inseparable from each other (Fig. 4). Progressive and complete release of the small intestine from the last ileal loop to the angle of Treitz was achieved. The peritoneum was thickened and nodular in places. These nodules were excised. There were no signs of perforation or necrosis, and no abscesses or collections were found.
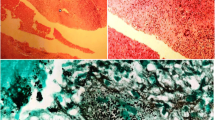
Pathological findings
The histopathological examination revealed inflammatory large, ovoid granulomatous lesions with few giant cells and central necrosis. On Grocott’s stain (Fig. 5), numerous spore-like mycelial elements with morphology suggestive of Histoplasma capsulatum. As the piece was not directly sent for microbiology culture, real-time Polymerase Chain Reaction assay (PCR) of fungal DNA (18 S) on the paraffin block was secondary performed. Results can not differentiate between Histoplasma capsulatum or Blastomyces sp, but serology studies showed positive serum antibodies against Histoplasma capsulatum (immunodiffusion). Urine Histoplasma capsulatum antigen (ELISA) was negative. Considering the histopathological finding and the positive serum antibodies assay against Histoplasma capsulatum, the diagnosis of histoplasmosis was retained. A chest CT-scan excluded mediastinal lymph nodes involvement or intra-parenchymal lung lesions. By reviewing the abdominal CT scan, we did not find any hepatic or splenic involvement. The patient only presented peritoneal involvement. HIV serology was negative, and CD4 lymphocytes were within normal range (674 G/l, 45%). Protein electrophoresis was also within the normal range.
Postoperative course and follow-up
A nasogastric tube was maintained until post-operative day (POD) 3 and refeeding began at POD 4. Progressive food intake was well tolerated, and the patient was discharged at POD 8 without any post-operative complication. Symptoms were partially relieved after surgery.
Due to the relatively good health of the patient, the extrapulmonary localization of the fungal infection and the long duration of symptoms (more than one month), antifungal therapy with oral itraconazole was started (200 mg BID). Further evolution was favorable: tolerance to treatment was good, abdominal pain decreased and completely resolved upon 10 months of therapy. Itraconazole blood level was monitored and stayed in steady state. As both serum antibody and urinary antigen control at 12 months were negative, the antifungal therapy could be discontinued. One month after treatment withdrawal, the patient remaind asymptomatic and remains so at one year follow up. Urine antigen and serum antibodies remain negative. We planned a clinical and serological monitoring for at least 12 months after the end of treatment, according to guidelines [4].
Discussion
Histoplasmosis in immunocompetent patients involving digestive tract is rare. It may present as an asymptomatic infection, a localized infection or can be part of a disseminated disease. Y. Dang et al. [5] found 9 immunocompetent patients with DH and digestive involvement in their literature review. Seven of them touching the colon including 4 of them the terminal ileum. All but one needed antifungal treatment. One patient required thoracotomy for oesophageal involvement secondary to mediastinal histoplasmosis [6]. In addition, we found only 4 other reported cases, which are summarized in Table 1. DH in immunocompetent patients is probably largely misdiagnosed and therefore underreported for several reasons. Most of the patients may be asymptomatic or mildly symptomatic, presenting only transient flu-like symptoms [3]. Usually, symptoms of DH with gastrointestinal involvement are nonspecific (fever, diarrhoea, diffuse abdominal pain). It may mimic inflammatory bowel disease as it usually involves the terminal ileum [7]. In addition, awareness of this infection and low access to diagnostic tests outside but also in endemic areas probably partly explain the underdiagnosis of this disease [2]. Interestingly, Bassey E. Ekeng et al. conducted a descriptive review of cases of gastrointestinal histoplasmosis from 2001 to 2021 and found 212 cases. They found that the clinical presentation was non-specific and differed only slightly between the HIV and non-HIV groups in terms of abdominal pain, which was significantly more frequent in HIV patients [8]. Patients with acute abdomen were described in only 3.1% of cases but without finding peritonitis.
Amphotericin B and azoles, like itraconazole, are the 2 main classes of antifungal drugs used in the treatment of histoplasmosis [4]. Amphotericin B eradicated fungemia faster than itraconazole, as serum levels reach steady state faster [9], but toxicity is higher. Therefore, it is mainly used for patients with severe disease including unstable patients. The liposomal preparation of amphotericin B is preferred to the deoxycholate for its comparable efficacy and fewer adverse effects (i.e. nephrotoxicity) [1]. Oral switch to itraconazole can be performed after clinical improvement. Itraconazole alone can be administered for mild to moderate forms. Duration of therapy depend on clinical manifestation, usually for at least 12 months [6, 10]. The need of surgery is rare.
In the literature, we found two cases of patients having bowel obstruction requiring surgical intervention. The patient described by Nawaz et al [11], was on immunosuppressants methotrexate and adalimumab and presented bowel distention due to intestinal obstruction by an intraluminal mass caused by histoplasmosis, requiring ileocecal resection with end ileostomy.
Badyal and al [12] describe a case of bowel distension and peritonitis following perforating colitis. It also led to surgery, with right hemicolectomy and end ileostomy.
Our patient had unexplained peritonitis with unclear and progressive bowel dysfunction The surgery was performed primarily for diagnostic purposes. During the operation, we found significant inflammation of the peritoneum with scattered nodules, without any intestinal obstruction. It required extensive adhesiolysis with peritoneal biopsies which established the diagnosis.
To our knowledge, this is the first described case of an immunocompetent patient presenting histoplasmosis with peritonitis as unique manifestation. Because of the symptoms, neither oesophago-gastroduodenoscopy nor colonoscopy could be performed. We cannot exclude that these examinations could have found intraluminal involvement and possibly avoided surgery. We believe that our patient has contracted the infection during his younger age in Cameroon and that it progressed slowly over the years. We have not found any underlying immunosuppressive condition that could have facilitate the disease.
Conclusion
We described the case of an immunocompetent patient with peritonitis as the only manifestation of histoplasmosis. Digestive involvement of histoplasmosis in immunocompetent patient is rare and likely underdiagnosed. Gastrointestinal involvement is uncommon and mostly affects the colon or the terminal ileum, mimicking other medical conditions. Clinicians should be aware of this condition, especially for patients originating from or having travelled to endemic countries and not only for immunocompromised patients.
Long term antifungal treatment is necessary for all patients having disseminated histoplasmosis. For responders, serology monitoring should continue for one to two years after treatment withdrawal to avoid relapse.
Data availability
All data generated or analysed during this study are included in this published article.
References
Araúz AB, Papineni P, Histoplasmosis. Infect Dis Clin North Am. 2021;35(2):471–91.
Antinori S. Histoplasma capsulatum: more widespread than previously thought. Am J Trop Med Hyg. 2014;90(6):982–3.
Staffolani S, Buonfrate D, Angheben A, Gobbi F, Giorli G, Guerriero M, et al. Acute histoplasmosis in immunocompetent travelers: a systematic review of literature. BMC Infect Dis. 2018;18(1):673.
Wheat J, Sarosi G, McKinsey D, Hamill R, Bradsher R, Johnson P, Loyd J, Kauffman C. Practice guidelines for the management of patients with histoplasmosis. Clin Infect Dis. 2000;30(4):688–95.
Dang Y, Jiang L, Zhang J, Pan B, Zhu G, Zhu F, et al. Disseminated histoplasmosis in an immunocompetent individual diagnosed with gastrointestinal endoscopy: a case report. BMC Infect Dis. 2019;19(1):992.
Chaudhari D, McKinney J, Hubbs D, Young M. Mediastinal histoplasmosis presenting as dysphagia: a case report with literature review. Clin J Gastroenterol. 2013;6(4):315–8.
Dahiya D, Kichloo A, Singh J, Albosta M, Wani F. Histoplasmosis and inflammatory bowel disease: a case report. World J Gastrointest Endosc. 2021;13(1):24–32.
Ekeng BE, Itam-Eyo AE, Osaigbovo II, Warris A, Oladele RO, Bongomin F, Denning DW. Gastrointestinal histoplasmosis: a descriptive review, 2001–2021. Life. 2023;13(3):689. https://doi.org/10.3390/life13030689.
Wheat LJ, Cloud G, Johnson PC, Connolly P, Goldman M, Le Monte A, et al. Clearance of fungal burden during treatment of disseminated histoplasmosis with liposomal amphotericin B versus itraconazole. Antimicrob Agents Chemother. 2001;45(8):2354–7.
Nyffenegger L, Abbas M, Gex G, Schrenzel EB, Bouchuiguir- J K, Wafa et al. Cas importés d’histoplasmose. Revue médicale Suisse. 2009;5:2418-23.
Nawaz Z, Martin S, Reichstein AR. Gastrointestinal histoplasmosis as an obstructing Ileocecal Mass. Cureus. 2020;12(12):e12277.
Badyal RK, Gupta R, Vaiphei K. Diffuse perforated necrotising amoebic colitis with histoplasmosis in an immunocompetent individual presenting as an acute abdomen. BMJ Case Rep. 2013;2013.
Acknowledgements
The authors would like to thank Dr Jeanne Hirt (Dpt of visceral Surgery, Lausanne University Hospital, Switzerland) for revising the manuscript.
Funding
Drs Thomas Jaugey, Michael Schneider, Cristina Bellini, Stephane Yerly, Edgardo Pezzetta have no funding to disclose.
Open access funding provided by University of Lausanne
Author information
Authors and Affiliations
Contributions
T.J. and M.S. Data collection, wrote the main manuscript text. E.P. and C.B. supervised the redaction. C.S. and S.Y. prepared figures All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval is not necessary for this case report. Patient was free to participate. Written consent was obtained for publication.
Consent for publication
Written informed consent was obtained from the patient for publication of the case report and the images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jaugey, T., Schneider, M., Bellini, C. et al. Histoplasmosis peritonitis in an immunocompetent patient: case report. BMC Infect Dis 24, 201 (2024). https://doi.org/10.1186/s12879-024-09083-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09083-9