Abstract
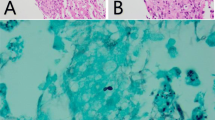
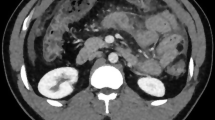
Histoplasma capsulatum, a dimorphic fungus often, is asymptomatic in the immunocompetent but can cause life threatening infection in immunocompromised patients. It is uncommon in the solid organ transplant recipients with an incidence of < 1%, majority occurring within 2 years of transplantation. It can be either endogenous reactivation of latent infection, de novo acquisition, or donor-derived infection. Disseminated infection is common, with non-specific symptoms, fever being the commonest. None of the available tests is 100% accurate. Modification of immunosuppression and anti-fungal can achieve 90% success rate. We report a liver transplant recipient, 3 months post-transplantation on everolimus, prednisolone, mycophenolate, and tacrolimus who had isolated hepatic histoplasmosis and responded to treatment. Liver biopsy revealed epithelioid granulomas with narrow-based budding yeast, suggesting histoplasma. Contrast CT abdomen revealed normal attenuation of graft liver few small non-enhancing hypodense lesions seen scattered in both lobes. And this patient was managed with just reduction of immunosuppressive doses as the patient was having renal dysfunction; starting itraconazole will lead to further deterioration in the clinical course and also interact with calcineurin inhibitors and mycophenolate mofetil.

Similar content being viewed by others
References
Assi M, Martin S, Wheat LJ et al (2013) Histoplasmosis after solid organ transplant. Clin Infect Dis 57:1542–1549
Kauffman CA (2007) Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev 20:115–132
Cuellar-Rodriguez J, Avery RK, Lard M et al (2009) Histoplasmosis in solid organ transplant recipients: 10 years of experience at a large transplant center in an endemic area. Clin Infect Dis 49:710–716
Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey D, Loyd JE, Kauffman CA, Infectious Diseases Society of America (2007) Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 45:807–825
Washburn L, Galván NT, Dhingra S, Rana A, Goss JA (2017) Histoplasmosis hepatitis after orthotopic liver transplantation. J Surg Case Rep 2017(12):rjx232 Published online 2017 Dec 11
Shallot J, Pursell KJ, Bartolone C, Williamson P, Benedetti E, Layden TJ, Wiley TE (1997) Disseminated histoplasmosis after orthotopic liver transplantation, liver transplantation and surgery. 3(4):433–434
Wheat LJ, Kohler RB, Tewari RP (1986) Diagnosis of disseminated histoplasmosis by detection of Histoplasma capsulatum antigen in serum and urine specimens. N Engl J Med 314:83–88
Kaufman L (1992) Laboratory methods for the diagnosis and confirmation of systemic mycosis. Clin Infect Dis 14(supp 1):23–29
Acknowledgements
The research was performed at the Department of Surgical Gastroenterology and Liver Transplant, Global Hospitals, Hyderabad.
Contribution Details
All authors contributed almost equally in preparing this case report starting from concept, design, data collection, literature search, to manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maharaj, R., Kapoor, D., Dekate, J. et al. Histoplasmosis After Liver Transplantation—a Skate on Thin Ice if Left Undiagnosed. Indian J Surg 82, 695–697 (2020). https://doi.org/10.1007/s12262-019-02048-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-02048-2