Abstract
Background
Chronic cholecystitis, characterized by persistent inflammation of the gallbladder, predominantly stems from the prolonged presence of gallstones. Calculous cholecystitis has demonstrated a consistent escalation in its incidence over time.Gallbladder stones have been recognized as a predisposing factor for the development of biliary tract infections.Concomitantly, there have been substantial shifts in the distribution and resistance profiles of pathogenic microorganisms responsible for biliary tract infections. The timely acquisition of bile samples for pathogen analysis is of paramount importance, given its critical role in guiding judicious clinical pharmacotherapy and enhancing patient prognosis.
Case Presentation
We present a case involving a 66-year-old female patient who had previously undergone subtotal gastrectomy due to diffuse large B-cell lymphoma. The patient was admitted to our institution with complaints of abdominal pain. Subsequent diagnostic evaluation revealed concurrent choledocholithiasis and cholecystolithiasis. The patient underwent surgical cholecystectomy as the therapeutic approach. Histopathological examination of the excised gallbladder disclosed characteristic features indicative of chronic cholecystitis. Subsequent laboratory analysis of the patient’s bile specimen yielded Gram-positive cocci, subsequently identified through biochemical assays, mass spectrometry, and 16 S rRNA analysis as Vagococcus fluvialis. Further in vitro antimicrobial susceptibility testing using disk diffusion and microfluidic dilution showed that this strain exhibited inhibition zone diameters ranging from 12.0 to 32.0 mm in response to 26 antibiotics, including ampicillin, cefazolin, cefuroxime, cefotaxime, ceftriaxone, cefepime, ampicillin/sulbactam, piperacillin, ciprofloxacin, cefoperazone/sulbactam, imipenem, meropenem, piperacillin/tazobarb, penicillin, erythromycin, chloramphenicol, vancomycin, methotrexate/sulfamethoxazole, teicoplanin, linezolid, tigecycline, cefoxitin, ceftazidime, levofloxacin, minocycline and tobramycin. However, the inhibition zone diameters were 6.0 mm for amikacin, oxacillin, clindamycin, and tetracycline. The patient received ceftazidime anti-infective therapy both preoperatively and within 24 h postoperatively and was discharged successfully one week after surgery.
Conclusion
In this study, we present the inaugural isolation and identification of Vagococcus fluvialis from bile specimens of patients afflicted with calculous cholecystitis. This novel finding lays a substantial experimental groundwork for guiding clinically rational antimicrobial therapy and advancing the exploration of relevant pathogenic mechanisms pertaining to Vagococcus fluvialis infections.
Similar content being viewed by others
Background
Chronic cholecystitis typically emerges from prolonged gallbladder inflammation attributed to the presence of gallstones or the recurrent migration of acute cholecystitis. Clinical manifestations exhibit considerable variability, ranging from asymptomatic or recurrent right upper quadrant discomfort to abdominal pain, and in some cases, acute exacerbations. A study by [1] reported a 44% positive bile culture rate in patients with chronic cholecystitis. Classification is based on the presence or absence of gallstones, distinguishing between calculous and acalculous cholecystitis. In recent years, shifting dietary habits, lifestyle changes, and widespread use of antimicrobial agents have contributed to an escalating incidence of calculous cholecystitis. Gallstone formation obstructs bile drainage, facilitating the entry of enteric pathogens into the biliary tract via blood, lymphatics, or retrograde flow, thereby instigating biliary tract infections (biliary tract infection,BTI). Subsequent infection further exacerbates disease progression, intensifying its severity and impeding effective clinical management [2].
Vagococcus fluvialis is a Gram-positive coccus that typically arranges singularly, in pairs, or in chains. It possesses flagella across its surface. It thrives within a temperature range of 10–40 °C and can tolerate growth in a 4% NaCl environment. However, it does not survive at 45 °C and in 6.5% NaCl. Additionally, exposure to 60 °C for 30 min is lethal for this organism [3]. As an opportunistic pathogen, Vagococcus fluvialis generally poses minimal threat to humans and other animals under standard conditions. Although predominantly isolated from animals or animal products [4,5,6,7,8,9,10], only rare instances of human infection have been reported [11,12,13,14,15]. Recently, our laboratory successfully isolated Vagococcus fluvialis from bile samples of patients with calculous cholecystitis. The isolated strain was subjected to biochemical assays, mass spectrometry identification, 16 S rRNA analysis, and antimicrobial susceptibility testing via disc diffusion and microbroth dilution methods. In view of the fact that there have been no reports of isolation of Vagococcus fluvialis from bile, the following is reported for the information of other laboratories.
Case Presentation
The patient, a 66-year-old female, underwent subtotal gastrectomy five years ago for gastric lymphoma, histopathologically diagnosed as diffuse large B-cell lymphoma. She was recently admitted to our medical facility due to abdominal pain. On admission day, a comprehensive physical examination and pertinent investigations were conducted. The patient’s vital signs were recorded as follows: body temperature of 36.3 °C, heart rate of 76 beats per minute, respiratory rate of 19 breaths per minute, and blood pressure of 117/76 mmHg. Magnetic resonance imaging of the upper abdomen, pancreas, and biliary system revealed multiple findings: a cyst in the right hepatic lobe, multiple stones in the distal common bile duct, gallbladder stones, segmental discontinuity at the distal common bile duct, and slight pancreatic duct dilation.The patient’s stool appeared yellow-brown, and her laboratory parameters were as follows: total bilirubin of 7.8µmol/L, alanine aminotransferase of 22U/L, aspartate aminotransferase of 34U/L, alkaline phosphatase of 109U/L, gamma-glutamyl transferase of 14.2U/L, amylase of 108 U/L, and lipase of 27U/L. Peripheral blood analysis indicated a white blood cell count of 3.5 × 10^9/L, with neutrophils accounting for 46.2% of the total count.Admission diagnosis was (1) choledocholithiasis (2) gallbladder stones 2. chronic cholecystitis.
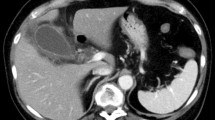
Three days following admission, the patient underwent surgical cholecystectomy as treatment. Preoperative prophylactic antibiotic therapy with ceftazidime was administered. The excised gallbladder was sent for pathological examination, revealing evidence of chronic cholecystitis. On the evening of the surgery, the patient’s peripheral blood white cell count was recorded at 18.5 × 10^9/L. Continued ceftazidime therapy was implemented for infection. By the subsequent day, the peripheral blood white cell count had decreased to 12.2 × 10^9/L.During the surgical procedure, bile samples were collected and subsequently subjected to general bacterial culture in the laboratory. The bile samples were inoculated into blood culture bottles and Columbia blood agar plates. After 24 h of incubation(at 35℃), pinpoint-sized, circular, raised colonies were observed on the Columbia blood agar plates, exhibiting a neat and gray-white appearance, accompanied by slight alpha-hemolysis. Extending the incubation to 72 h, the colonies continued to grow, transitioning from gray-white to gray-yellow in color (Fig. 1). Microscopic examination of Gram staining revealed small, Gram-positive cocci arranged mostly in pairs or short chains, occasionally as individual bacterium (Fig. 2).Subsequent identification of the isolated microorganism was conducted using both the VITEK 2 compact automated bacterial identification system (bioMérieux) and matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS, VITEK MS system, bioMérieux). These analyses yielded concordant results, identifying the organism as Vagococcus fluvialis with matching rates of 97.0% and 99.9% respectively. Biochemical reaction profiles and spectral peaks are illustrated in Figs. 3 and 4. Furthermore, 16 S rRNA sequencing analysis (The sequencing was conducted by Beijing Ruiboxingke Biotechnology Co., Ltd., using the Applied Biosystems sequencing platform, model 3730xl for DNA analysis.) displayed a remarkable 99.66% homology between the isolated strain and existing Vagococcus fluvialis sequences in the GenBank database(The sequencing report has been included in the supplementary material for the Editor’s reference).
Standardized drug sensitivity testing protocols for Vagococcus fluvialis remain elusive. In our study, we sought to assess drug sensitivity through both the disc diffusion method (using Mueller-Hinton agar, antimicrobial discs from Oxoid, UK) and microbroth dilution method(The bacterial sensitivity testing cards were purchased from bioMérieux). The results indicated that this Vagococcus fluvialis strain exhibited inhibitory zone diameters ≥ 20.0 mm for 21 antimicrobial agents including ampicillin, cefazolin, cefuroxime, cefotaxime, ceftriaxone, cefepime, ampicillin/sulbactam, piperacillin, ciprofloxacin, cefoperazone/sulbactam, imipenem, meropenem, piperacillin/tazobarb, penicillin, erythromycin, chloramphenicol, vancomycin, methotrexate/sulfamethoxazole, teicoplanin, linezolid, and tigecycline, with inhibitory zone diameters ranging from 7.0 to 19.0 mm for cefoxitin, ceftazidime, levofloxacin, minocycline, and tobramycin, and 6.0 mm for amikacin, oxacillin, clindamycin, and tetracycline. Microbroth dilution results demonstrated that 10 antimicrobial agents, including gentamicin, penicillin, erythromycin, vancomycin, methotrexate/sulfamethoxazole, teicoplanin, tigecycline, linezolid, daptomycin, and moxifloxacin, exhibited minimum inhibitory concentrations (MICs) of ≤ 1 µg/ml. Levofloxacin exhibited an MIC range of ≥ 2 µg/ml to < 4 µg/ml. Oxacillin, clindamycin, and rifampicin exhibited MICs of ≥ 4 µg/ml. For detailed results, refer to Table 1.One week post-surgery, the patient’s peripheral blood white cell count had normalized to 7.4 × 10^9/L. Liver and kidney function, as well as amylase levels, remained within normal parameters. The patient’s recovery progressed favorably, prompting her discharge on the same day, attesting to a successful postoperative outcome.
Discussion and conclusion
The prevailing literature on pathogenic bacterial isolates from bile predominantly features Escherichia coli, Klebsiella pneumoniae, Enterococcus faecalis, Enterococcus faecium, and Pseudomonas aeruginosa [15]. However, instances of pathogenicity attributable to Vagococcus fluvialis have yet to be documented. Antimicrobial susceptibility test for strains isolated from bile culture were performed in 557 hospitals in china [16].WHONET 5.6 software was used for statistical analysis.Results A total of 13,596 bacterial strains were isolated, inclu-ding gram-positive cocci 3698 strains, accounting for 27.2%, gram-negative bacilli 9898 strains, accounting for 72.8%.The top two gram-positive cocci are Enterococcus faecalis 1237 strains (9.1%) and Entero-coccus faecium 1198 strains (8.8%).The top three gram-negative ba-cilli are Escherichia coli 4311 strains ( 31.7%), Klebsiella pneumoniae 1518 strains ( 11.2%) and Pseudomonas aeruginosa 839 strains (6.2%). These findings underscore Gram-negative bacteria as the primary pathogenic agents in chronic cholecystitis. The authors postulate that widespread antimicrobial use has led to an upsurge in bacterial resistance and an increase in mixed infections, thereby altering the spectrum of infectious agents and presenting novel challenges in the management of chronic cholecystitis. These findings prompt a focused approach towards preventing infections from gut microbiota, the main causative agents in chronic cholecystitis.
Vagococcus fluvialis, a species within the Vagococcus genus, was initially reported by Collins et al. in 1989 [17]. Subsequent investigations demonstrated its presence in human blood, peritoneal fluid, wounds [18], oral cavity lesions [19], infectious endocarditis [20], and skin, tissue, and joint infections, particularly in patients with diabetes [14]. These studies suggest that, like other opportunistic pathogens, Vagococcus fluvialis has the potential to cause human infections under specific circumstances such as changes in colonization sites, compromised immunity, or microbial imbalances. In our study, Vagococcus fluvialis was isolated from the bile of a patient with calculous cholecystitis. This patient, who had undergone gastric lymphoma surgery, exhibited compromised immunity. Without timely surgical intervention, the risk of developing Vagococcus fluvialis-related biliary tract infection was imminent.
Currently, the identification methods for Vagococcus fluvialis primarily include biochemical identification, MALDI-TOF MS, and 16 S rRNA sequencing [14, 17, 20]. In this study, all three methods were employed to identify the isolated strain, each yielding highly confident results (97%, 99.9%, and 99.66%). This ensured the reliability of the identification outcomes. Considering operational convenience, the laboratory may preferentially opt for the biochemical identification method and MALDI-TOF MS to identify this strain.
Currently, reports on the drug sensitivity of Vagococcus fluvialis vary. Teixeira et al. [18] initially conducted MIC-based drug sensitivity testing for 25 antibiotics in 1997 and found that the four isolated strains were sensitive to ampicillin, cefotaxime, methotrexate/sulfamethoxazole and vancomycin, while being resistant to clindamycin, lomifioxacin and ofloxacin. In 2021, Racero L employed the Vitek™ 2 C automated system to conduct drug sensitivity testing and identified the best-performing antibiotics as ampicillin, methotrexate/sulfamethoxazole, vancomycin, teicoplanin, and linezolid [14]. In 2019, Chinese researchers [21] conducted Kirby-Bauer disk diffusion testing using Mueller-Hinton agar for Vagococcus fluvialis isolated from bone infections and found that linezolid, erythromycin, tetracycline, ampicillin, and chloramphenicol exhibited inhibition zones larger than 20.0 mm, while cefazolin, penicillin, levofloxacin, vancomycin, ciprofloxacin, gentamicin and ceftriaxone displayed inhibition zones ranging from 10.0 to 20.0 mm. Clindamycin, oxacillin and methotrexate/sulfamethoxazole displayed inhibition zones of 6.0 mm. Our laboratory’s results from both the disk diffusion method and the microdilution method showed that this bacterium was sensitive to most antibiotics, but resistant to amikacin, oxacillin, clindamycin, and tetracycline, in line with the aforementioned studies [14, 21, 22]. Notably, the results of antibiotic susceptibility testing obtained from both methods demonstrated good concordance. Seven antibiotics, including penicillin, erythromycin, vancomycin, linezolid, teicoplanin, and tigecycline, exhibited inhibition zones ≥ 20.0 mm and MICs ≤ 1 µg/ml; levofloxacin exhibited an inhibition zone of 19.0 mm and MIC of 2 µg/ml; while oxacillin and clindamycin exhibited inhibition zones of 6.0 mm and MICs ≥ 4 µg/ml. These findings indicate a strong correlation between the two methods of drug sensitivity testing. Based on operational feasibility, the laboratory may select either the disk diffusion method or the microdilution method for conducting drug sensitivity testing, depending on the specific circumstances.
Patients with chronic cholecystitis typically do not necessitate antibiotic treatment [22]. However, in cases of acute exacerbations, empirical antibiotic therapy can be considered, followed by tailored antibiotic selection based on pathogen identification and susceptibility testing [23]. In this case, the patient received prophylactic antimicrobial treatment with cefotetan for 24 h on the day of surgery. Following the surgery, and after two days when antibiotic susceptibility results became available, the patient did not receive any further antibiotic treatment. The patient recovered and was discharged one week postoperatively. Therefore, it is postulated that this Vagococcus fluvialis might be a normal resident of the biliary tract or a colonic organism that retrogradely entered the biliary tract.
In essence, this study marks the pioneering isolation of Vagococcus fluvialis from bile samples of individuals with calculous cholecystitis. The identification process involved three distinct methods: biochemical reactions, mass spectrometry, and 16 S rRNA analysis. Furthermore, the bacterial strain’s antimicrobial susceptibility was assessed through both the Kirby-Bauer disk diffusion method and the minimum inhibitory concentration (MIC) approach. These findings hold crucial clinical significance, serving as a guide for rational antibiotic usage and enhancing patient outcomes. Simultaneously, they lay a solid experimental foundation for guiding judicious antibiotic strategies and investigating the underlying pathogenic mechanisms associated with Vagococcus fluvialis infections.
Data Availability
The results of 16 S rRNA sequencing (Beijing Ruibo Xingke Biotechnology Co., Ltd.) analysis in this study have been provided in the Supplementary Material and are available for editorial review.
References
KIMURA Y, TAKADA T, KAWARADA Y, et al. Definitions, patho-physiology, and epidemiology of acute cholangitis and cholecystitis. Tokyo guidelines [J]. J Hepatobiliary Pancreat Surg. 2007;14(1):15–26.
Jang DK, Kim J, Park WB et al. Increasing burden of biliary tract Infection caused by extended-spectrum betalactamase-producing organisms in Korea: a nationwide population-based study[J]. J Gastroenterol Hepatol, 2020, 35.
Zuzana Rosenbergová,Thomas F, Oftedal,Kirill V, Ovchinnikov, et al. Identification of a Novel two-peptide Lantibiotic from Vagococcus fluvialis. [J] Microbiol Spectr. 2022;10(4):e0095422.
Lai YGJYX-H et al. Vagococcus xieshaowenii sp. nov., isolated from snow finch (Montifringilla taczanowskii) cloacal content. [J] Int J Syst Evol Microbiol 2020,70(4):2493–8.
Carlos Emilio Cabrera Matajira,Andre Pegoraro Poor,Luisa Zanolli Moreno. Vagococcus sp. a porcine pathogen: molecular and phenotypic characterization of strains isolated from diseased pigs in Brazil. [J] J Infect Dev Ctries. 2020;14(11):1314–9.
Stephan Wullschleger,Christoph Jans,Clelia Seifert. Vagococcus teuberi sp. nov., isolated from the Malian artisanal sour milk fènè. [J] Syst Appl Microbiol 2018,41(2):65–72.
Silvia Giannattasio-Ferraz,Adriana Ene,Laura Maskeri. Vagococcus fluvialis isolation and sequencing from urine of healthy cattle. [J].G3 (Bethesda),2021,11(1).
Kshitij Chandel,Rasesh Y, Parikh,Murlidhar J, Mendki, et al. Isolation and characterization of Vagococcus Sp from midgut of Culex quinquefasciatus (say) mosquito. [J] J Vector Borne Dis. 2015;52(1):52–7.
Kim D-WHEJTPS, et al. Description of Vagococcus coleopterorum sp. nov., isolated from the intestine of the diving beetle, Cybister lewisianus, and Vagococcus hydrophili sp. nov., isolated from the intestine of the dark diving beetle, Hydrophilus Acuminatus, and emended description of the genus Vagococcus. [J] J Microbiol. 2021;59(2):132–41.
Lawson PA, Foster G, Falsen E et al. Vagococcus lutrae sp. nov., isolated from the common otter (Lutra lutra). [J] Int J Syst Bacteriol 1999 49 Pt 3:1251–4.
Ana R et al. Jimenez,Nadège Guiglielmoni,Lise Goetghebuer,. Comparative genome analysis of Vagococcus fluvialis reveals abundance of mobilegenetic elements in sponge-isolated strains. [J].BMC Genomics,2022,23(1):618.
Takahiro Matsuo,Nobuyoshi Mori,Fujimi Kawai. Vagococcus fluvialis as a causative pathogen of bloodstream and decubitus Ulcer Infection: case report and systematic review of the literature. [J] J Infect Chemother. 2021;27(2):359–63.
Patricia L, Shewmaker,Anne M, Whitney,Christopher A, Gulvik, et al. Vagococcus bubulae sp. nov., isolated from ground beef, and Vagococcus Vulneris sp. nov., isolated from a human foot wound. [J] Int J Syst Evol Microbiol. 2019;69(8):2268–76.
Racero L et al. Claudia Barberis,Germán Traglia,. Infections due to Vagococcus spp. Microbiological and clinical aspects and literature review. [J].Enferm Infecc Microbiol Clin (Engl Ed),2021,39(7):335–339.
Tian Qin,Lu Xi Jiang,Hong Yu Ren. Isolation and characterization of Vagococcus fluvialis from bats. [J] Biomed Environ Sci 2021,34(10):834–7.
Zhi WANG, Pengyuan LI, Wei et al. Composition and drug resistance analysis of bile culture pathogens in tertiary hospitals nationwide in 2012[J]. Chin J Clin Pharmacol,2015(11):1038–41. (in Chinese).
Collins MD, Ash C, Farrow JA, et al. 16S ribosomal ribonucleic acid sequence analyses of lactococci and related taxa. Description of Vagococcus fluvialis gen. nov., sp. nov. [J]. J Appl Bacteriol. 1989;67(4):453–60.
Teixeira,M LM, G Carvalho VL, Merquior, et al. Phenotypic and genotypic characterization of Vagococcus fluvialis, including strains isolated from human sources. [J] J Clin Microbiol. 1997;35(11):2778–81.
Schirrmeister F, et al. Characterization of the first oral vagococcus isolate from a root-filled tooth with periradicular lesions. [J] Curr Microbiol. 2008;57(3):235–8. Klaus Pelz,Jörg.
Jadhav KP, Praveen G, Pai, et al. A rare infective endocarditis caused by Vagococcus fluvialis. [J] J Cardiol Cases. 2019;20(4):129–31.
Ting ZHOU, Yu CAO, Xiaolei DUAN et al. First isolation of Coccidioides fluvialis from postoperative infected puncture fluid of human left lower femur[J]. Chin J Hosp Infect 2019,29(18):2825–9,2846.(in Chinese).
YAN WB, XU XE ZHOU LF. Mod Diagn Treat. 2013;24(17):3857–8. (in Chinese). Comparison analysis of 188 cases of acute and chronic cholecystitis bacterial culture and antibiotics sensitivity [J].
Editorial Committee of Chinese Journal of Gastroenterology,Hepatobiliary Diseases Collaborative Group of the Division of Digestive Diseases of the Chinese Medical Association. Consensus opinion on internal medicine diagnosis and treatment of chronic cholecystitis and gallbladder stones in China (2018)[J]. Chin J Gastroenterol 2019,39(2):73–9. (in Chinese).
Acknowledgements
The authors thank all the clinical staff contributed to the study.
Funding
This work was supported byWuhan Municipal Health Commission Scientific Research Project (WX21D49). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Litao Zhang designed the paper. Dan Zhang and Xiaosu Wang drafted the manuscript. Jingdan Yu, Zheng Dai,Qichao Li analyzed the data. Dan Zhang and Xiaosu Wang revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical review committee of the Wuhan Asia General Hospital Affiliated to Wuhan University of Science and Technology. Written informed consent was obtained from patients in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent for publication was obtained from participants for publication of the data collected during the study, including any identifiable information.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, D., Wang, X., Yu, J. et al. A case of Vagococcus fluvialis isolated from the bile of a patient with calculous cholecystitis. BMC Infect Dis 23, 689 (2023). https://doi.org/10.1186/s12879-023-08696-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08696-w