Abstract
Background
Edwardsiella tarda (E. tarda) is a Gram-negative facultative anaerobe belonging to Enterobacteriales and is commonly isolated from fishes and reptiles. Infection due to E. tarda is uncommon among humans, with a reported human retention rate of 0.001%. It can cause sepsis in the elderly or those with pre-existing conditions such as liver failure, autoimmune disease, or malignancy. E. tarda is susceptible to many antibiotics; however, a high mortality rate (approximately 40%) has been reported with sepsis.
Case presentation
A 65-year-old woman presented to our hospital with a chief complaint of fever and abdominal pain for 2 days. Her blood tests showed elevated inflammatory markers, and contrast-enhanced computed tomography showed distention and wall thickening of the gallbladder and inflammation of peri-gallbladder fat. Subsequently, a diagnosis of cholecystitis with systemic inflammatory response syndrome was made. Laparoscopic cholecystectomy was performed after starting antimicrobial therapy. Blood culture of samples obtained on admission were positive for E. tarda, which was also detected in bile juice culture. Therefore, she was diagnosed with bacteremia caused by E. tarda, and postoperative antimicrobial therapy was continued. The patient improved, and there were no complications.
Conclusions
We experienced an extremely rare case of acute cholecystitis caused by E. tarda. Only a few cases of acute cholecystitis due to E. tarda have been reported. Furthermore, similar to this case, no previous study has reported the detection of E. tarda in both blood and bile cultures in acute cholecystitis cases. In addition to appropriate surgical intervention, continuous administration of antibiotics based on culture results resulted in a favorable outcome.
Similar content being viewed by others
Background
Edwardsiella tarda (E. tarda) is a Gram-negative rod-shaped bacterium that belongs to the Enterobacteriaceae family. E. tarda is isolated from fish and reptiles as a normal inhabitant. Although rare, it can be transmitted to humans through ornamental fish, pet turtles, snakes, catfish, and other animals, with a reported human carriage rate of 0.001% [1]. E. tarda may cause both intestinal and extraintestinal infections. Generally, intestinal infections are spontaneously resolved, whereas extraintestinal infections can lead to meningitis, liver abscess, necrotizing, fasciitis, and wound infection. Although sepsis caused by E. tarda is rare, it has a rapid course and a high fatality rate (approximately 40%) [2, 3]. Herein, we report a case of acute cholecystitis with sepsis caused by E. tarda wherein laparoscopic cholecystectomy was performed.
Case presentation
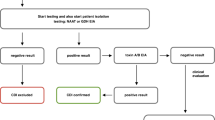
A 65-year-old woman presented to our hospital with fever and abdominal pain for 2 days. She had a history of asthma, depression, and irritable bowel syndrome. She had no history of keeping fish or other pets and had never traveled abroad. Upon presentation, her vital signs were as follows: temperature, 37.8 ℃, blood pressure, 103/84 mmHg, pulse rate, 124 beats/min, respiratory rate, 24 breaths/min, and oxygen saturation, 94% on room air. Her abdomen was flat and soft, but tenderness was noted in the right upper abdomen. Blood examination showed the following: leukocytes, 12,000/µL; and C-reactive protein, 37.40 mg/dL (Table 1). Contrast-enhanced computed tomography showed gallbladder distention, wall thickening, and inflammation of peri-gallbladder fat (Fig. 1). Magnetic resonance cholangiopancreatography did not show gallbladder or common bile duct stones (Fig. 2). Based on these tests, a diagnosis of acute cholecystitis with systemic inflammatory response syndrome was made. Our case was classified as moderate acute cholecystitis with marked local inflammatory findings (grade II) per the severity criteria of the Tokyo Guidelines 2018 Acute Cholecystitis [4]. After obtaining blood samples for culture, antibiotic therapy was started, and laparoscopic cholecystectomy was performed. Laparoscopy revealed an enlarged gallbladder; hence, puncture aspiration of bile, and decompression of the gallbladder were performed followed by laparoscopic cholecystectomy. Dark bloody bile was collected and submitted for culture examination. The wall of the removed gallbladder was partially necrotic, and no stones were found in the gallbladder (Fig. 3). Histopathological findings showed intense neutrophilic infiltration of all layers of the gallbladder epithelium and necrosis in some layers. At this time, the diagnosis was pyogenic and gangrenous cholecystitis (Fig. 4). Postoperatively, she had no complications. Results of blood and bile juice cultures were positive for E. tarda (Table 2). Based on the results of the antibiotic sensitivity test, cefmetazole was continued until the 7th postoperative day, and she was discharged home thereafter. After discharge, she continued receiving amoxicillin/clavulanate until postoperative day 15 without any complications (Fig. 5).
Photomicrograph of hematoxylin and eosin-stained gallbladder specimen. a Image shows full-thickness inflammation with partial degeneration, shedding of the gallbladder epithelium, and necrosis in some layers (magnification, 20 ×). b Image shows intense neutrophilic infiltration of the gallbladder epithelium (magnification, 200 ×)
Changes in the number of white blood cells and C-reactive protein levels. Both white blood cell counts and C-reactive protein levels improved following surgery and antibiotic therapy. Cefmetazole was continued until the 7th postoperative day, and amoxicillin/clavulanate was continued until the 15th postoperative day. The patient was discharged on the 7th postoperative day and did not develop any complications
Discussion
E. tarda is a Gram-negative facultative anaerobe belonging to Enterobacteriales and is isolated from turtles, fish, snakes, and lizards associated with fresh and saltwater [5,6,7]. E. tarda is a known pathogen of fish and reptiles and is uncommonly reported in humans. However, E. tarda can be transmitted to humans through contact with reptiles, amphibians, and other carriers of the disease as well as through ingestion of raw fish [8]. E. tarda infection in humans is rare, with a human retention rate of 0.001% [1]. A search of PubMed using “Edwardsiella tarda” and “acute cholecystitis” as search terms yielded several cases. Among them, only 12 cases of acute cholecystitis and Edwardsiella tarda-induced bacteremia have been reported [9,10,11,12]. Our case and its 12 cases are summarized in Table 3. The study population was relatively older, with a mean age of 74.6 years, and comprised 7 males and 6 females. In addition to antimicrobial therapy, we performed invasive gallbladder procedures such as PTGBD in 3 patients and surgery in 5 patients. Furthermore, there are no reports of E. tarda being detected in both blood and bile cultures in cases of acute cholecystitis, similar to the present case.
Intestinal infections account for approximately 80% of all E. tarda infections [13]. E. tarda is biochemically similar to Salmonella; it causes low-grade fever and intermittent watery diarrhea, similar to Salmonella enteritis [8, 9]. Generally, enteritis caused by E. tarda often resolves spontaneously with symptomatic treatment and is rarely clinically severe. However, intra-abdominal abscess, cholecystitis, cholangitis, cellulitis, necrotizing fasciitis, meningitis, and osteomyelitis have been reported as extraintestinal infections, although the number of reports is small [9,10,11, 14,15,16,17,18]. Meanwhile, bacteremia is rare, occurring in less than 5% of all cases of E. tarda infections [8]. However, the mortality from bacteremia caused by E. tarda is 44.6% [3]. Risk factors for severe E. tarda infection include age (≥ 65 years) and a history of underlying diseases such as malignancy, autoimmune disease, liver disease, and diabetes mellitus [3, 9, 11]. In these patients, mortality rates were reportedly more than four times higher especially in patients with cirrhosis [3, 19]. Additionally, deaths have been reported in cases of sepsis associated with soft tissue infections such as necrotizing fasciitis, which may be due to the difficulty in completely removing the infected lesion [3].
Regarding treatment, extraintestinal infections generally require antibiotic therapy. E. tarda is sensitive to several antibiotic agents, including β-lactams, aminoglycosides, quinolones, and tetracyclines [20]. However, in cases of bacteremia, which can be severe, it is necessary to continue antibiotic therapy even after symptoms improve. Therefore, it is important to administer antibiotics after culture testing to determine the appropriate antibiotic therapy. In our case, blood cultures were obtained before antibiotics were administered, and intraoperative bile cultures were also obtained. Results confirmed E. tarda infection, allowing treatment with the appropriate antibiotic agents. Additionally, due to the importance of complete removal of the infected lesion, surgical intervention would be appropriate.
Regarding the route of infection in this case, the patient had no history of keeping fish or reptiles as pets, and the possibility of contact infection was considered low. However, because of her habit of eating raw seafood on a daily basis, the possibility of infection by oral ingestion was considered possible. After the diagnosis of E. tarda infection, fecal culture was performed to reveal intestinal commensal bacterial; however, E. tarda was not detected because culture was performed after antibiotic therapy was started. Although the reported human retention rate is 0.001% [1], the possible presence of E. tarda cannot be ruled out due to the patient’s history of recurrent diarrhea, which was caused by irritable bowel syndrome. In our case, there were no gallbladder stones that could have caused cholecystitis. Gallbladder stones are the most common cause of acute cholecystitis development. Cholecystitis develops due to gallbladder duct obstruction and bile congestion caused by the fitting of a stone, which damages the mucosa of the gallbladder. Conversely, acute acalculous cholecystitis can occur in 3.7–14% patients with acute cholecystitis [21, 22]. Risk factors of cholecystitis include surgery, trauma, infection, burns, and transvenous nutrition [23, 24]. However, these risk factors were not relevant in our case. As diarrhea was previously observed in this case, the patient developed a retrograde biliary infection due to enteritis-induced increased intestinal pressure, which occurred due to irritable bowel syndrome; this could have further led to cholecystitis and then to bacteremia. There have been many reports of patients with a poor prognosis caused by E. tarda sepsis; however, in our case, she had a favorable prognosis. This may be attributed to the patient’s age, early and appropriate surgical intervention to completely remove the infected lesion, and continued systematic administration of antimicrobials based on the culture results, all of which prevented recurrence.
Conclusion
We report a case of sepsis secondary to acute cholecystitis caused by E. tarda that was treated with laparoscopic cholecystectomy. Although E. tarda rarely infects humans, it can occasionally cause sepsis, which can be severe, and result in death. Therefore, this infection needs to be recognized, and appropriate therapeutic interventions should be implemented early.
Availability of data and materials
The dataset supporting the conclusions of this article is available in the manuscript.
Abbreviations
- E. tarda :
-
Edwardsiella tarda
- WHO:
-
World Health Organization
- WBC:
-
White blood cell count
- RBC:
-
Red blood cell count
- PT:
-
Prothrombin time
- TP:
-
Total protein
- BUN:
-
Blood urea nitrogen
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- γ-GTP:
-
γ-Glutamyltranspeptidase
- LDH:
-
Lactate dehydrogenase
- T.Bil:
-
Total bilirubin
- D.Bil:
-
Direct bilirubin
- CRP:
-
C-reactive protein
- MIC:
-
Minimum inhibitory concentration
- CLSI:
-
Clinical and Laboratory Standards Institute
- GM:
-
Gentamicin
- ST:
-
Sulfamethoxazole–trimethoprim
- AMK:
-
Amikacin
- CAZ:
-
Ceftazidime
- CMZ:
-
Cefmetazole
- CTM:
-
Cefotiam
- CTX:
-
Cefotaxime
- FOM:
-
Fosfomycin
- IPM:
-
Imipenem
- ABPC:
-
Ampicillin
- CFPM:
-
Cefepime
- CPDX:
-
Cefpodoxime
- CPFX:
-
Ciprofloxacin
- AMPC/CVA:
-
Amoxicillin/clavulanate
- LVFX:
-
Levofloxacin
- MEPM:
-
Meropenem
- MINO:
-
Minocycline
- PIPC:
-
Piperacillin
- S:
-
Sensitive
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- PTGBD:
-
Percutaneous transhepatic gallbladder drainage
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
References
Onogawa T, Terayama T, Zen-yoji H, Amano Y, Suzuki K. Distribution of Edwardsiella tarda and hydrogen sulfide-producing Escherichia coli in healthy persons. Kansenshogaku Zasshi. 1976;50:10–7.
Wang IK, Kuo HL, Chen YM, Lin CL, Chang HY, Chuang FR, et al. Extraintestinal manifestations of Edwardsiella tarda infection. Int J Clin Pract. 2005;59:917–21.
Hirai Y, Asahata-Tago S, Ainoda Y, Fujita T, Kikuchi K. Edwardsiella tarda bacteremia: a rare but fatal water- and foodborne infection: review of the literature and clinical cases from a single centre. Can J Infect Dis Med Microbiol. 2015;26:313–8.
Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:41–54.
Nagel P, Serritella A, Layden TJ. Edwardsiella tarda gastroenteritis associated with a pet turtle. Gastroenterology. 1982;82:1436–7.
Vandepitte J, Lemmens P, De Swert L. Human Edwardsiellosis traced to ornamental fish. J Clin Microbiol. 1983;17:165–7.
Sakazaki R. A proposed group of the family Enterobacteriaceae, the Asakusa group. Int Bull Bacteriol Nomencl Taxon. 1965;15:45–7.
Janda JM, Abbott SL. Infections associated with the genus Edwardsiella: the role of Edwardsiella tarda in human diseases. Clin Infect Dis. 1993;17:742–8.
Kamiyama S, Kuriyama A, Hashimoto T. Edwardsiella tarda bacteremia, Okayama, Japan, 2005–2016. Emerg Infect Dis. 2019;25:1817–23.
Tonosaki K, Yonenaga K, Mikami T, Mizuno T, Oyama S. Acute cholecystitis, sepsis, and disseminated intravascular coagulation caused by Edwardsiella tarda in an elderly woman. Tokai J Exp Clin Med. 2021;46:51–3.
Hasegawa K, Kenya M, Suzuki K, Ogawa Y. Characteristics and prognosis of patients with Edwardsiella tarda bacteremia at a single institution, Japan, 2005–2022. Ann Clin Microbiol Antimicrob. 2022;21:56.
Ding Y, Men W. A case report and review of acute cholangitis with septic shock induced by Edwardsiella tarda. Ann Clin Microbiol Antimicrob. 2022;21:33.
Jordan GW, Hadley WK. Human infection with Edwardsiella tarda. Ann Intern Med. 1969;70:283–8.
Pham K, Wu Y, Turett G, Prasad N, Yung L, Rodriguez GD, et al. Edwardsiella tarda, a rare human pathogen isolated from a perihepatic abscess: implications of transient versus long term colonization of the gastrointestinal tract. IDCases. 2021;26:e01283.
Yamamuro T, Fukuhara A, Kang J, Takamatsu J. A case of necrotizing fasciitis following Edwardsiella tarda septicemia with gastroenteritis. J Infect Chemother. 2019;25:1053–6.
Yamanoi K, Yasumoto K, Ogura J, Hirayama T, Suginami K. A case of pelvic abscess caused by Edwardsiella tarda followed by laparoscopic resection of a hematoma derived from cesarean section. Infect Dis. 2018;2018:4970854.
Miyazawa Y, Murakami K, Kizaki Y, Itaya Y, Takai Y, Seki H. Maternal peripartum septic shock caused by intrauterine infection with Edwardsiella tarda: a case report and review of the literature. J Obstet Gynaecol Res. 2018;44:171–4.
Makino T, Sugano I, Kamitsukasa I. An autopsy case of Edwardsiella tarda meningoencephalitis. Case Rep Neurol. 2018;10:252–60.
Arvaniti V, D’Amico G, Fede G, Manousou P, Tsochatzis E, Pleguezuelo M, et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology. 2010;139:1246–56.
Stock I, Wiedemann B. Natural antibiotic susceptibilities of Edwardsiella tarda, E. ictaluri, and E. hoshinae. Antimicrob Agents Chemother. 2001;45:2245–55.
Wang AJ, Wang TE, Lin CC, Lin SC, Shih SC. Clinical predictors of severe gallbladder complications in acute acalculous cholecystitis. World J Gastroenterol. 2003;9:2821–3.
Ryu JK, Ryu KH, Kim KH. Clinical features of acute acalculous cholecystitis. J Clin Gastroenterol. 2003;36:166–9.
Laurila J, Syrjälä H, Laurila PA, Saarnio J, Ala-Kokko TI. Acute acalculous cholecystitis in critically ill patients. Acta Anaesthesiol Scand. 2004;48:986–91.
Theodorou P, Maurer CA, Spanholtz TA, Phan TQ, Amini P, Perbix W, et al. Acalculous cholecystitis in severely burned patients: incidence and predisposing factors. Burns. 2009;35:405–11.
Acknowledgements
We thank ENAGO (https://www.enago.jp) for editing the draft of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
CH, TT, and YK are the surgeons who operated and treated the patient. The manuscript was drafted by CH. TT and AY supervised the preparation of this case report. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures followed were in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its subsequent amendments.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hara, C., Tanaka, T., Nishiwada, S. et al. Acute cholecystitis with sepsis due to Edwardsiella tarda: a case report. surg case rep 9, 184 (2023). https://doi.org/10.1186/s40792-023-01763-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01763-z