Abstract
Background
Febrile illnesses are among the most important reasons for medical consultation in sub-Saharan Africa and are frequently treated with antimicrobials due to the unavailability of appropriate diagnostic tools. This practice leads to antimicrobial resistance, with increasing mortality and morbidity as result. One of the few accessible diagnostic tools available in low resource settings is malaria rapid diagnostic tests (mRDTs) which contributed to reducing the over-prescription of anti-malarials, but cannot guide antibiotic prescriptions. To circumvent this problem, we explored whether combined testing with mRDT and c-reactive protein (CRP) could improve the diagnosis of febrile illnesses and subsequent prescription of antibiotics.
Methods
Clinical specimens (blood, stool and urine) collected from 396 febrile children (axillary temperature of ≥ 37.5 °C) were analyzed with rapid diagnostic tests (malaria and CRP) and microbiology culture to establish the possible cause of fever. Actual antimicrobial prescriptions given to the children were compared with those that could be given based on combined CRP-malaria testing.
Results
In total, 68.7% (272/396) of malaria cases were diagnosed by mRDT-Pf-HRP-2. CRP test was positive in 84.3% (334/396) of the children, but bacterial infections were confirmed in 12.4% (49/396) of them. A possible cause of fever could not be established in 20.5% (81/396) of cases. Based on the diagnostic practice in place, 265 of the children with a positive mRDT-Pf-HRP-2 received anti-malarial treatment. Furthermore, 89.5% (111/124) of negative mRDT results received antibiotic treatment and 37.1% (46/124) received antimalarial treatment. Of these 124 cases, 80 had positive CRP tests and 44 negative CRP tests. If the results of CRP testing are considered, 44 CRP/mRDT negative children would not get antibiotic treatment, resulting in a 35.5% reduction in antibiotic prescriptions. However, 2 cases with a bacterial infection would be denied appropriate treatment.
Conclusion
Combining mRDT-PfHRP2 with CRP testing is particularly useful in children for whom both tests are negative as it results in a reduction of antibiotics prescriptions. However, there is a risk to miss potential severe bacterial infections and a close follow-up of these cases is strongly recommended.
Similar content being viewed by others
Background
In Burkina Faso, like in many other sub-Sahara African countries, febrile illnesses in children are amongst the foremost reasons for medical consultation [1,2,3]. In resource limited settings, with inadequate availability of appropriate diagnostic tools for a proper diagnosis of the actual cause of fever, antimicrobials are often systematically prescribed. This unwanted use of antimicrobials results in increasing resistance with as main consequence thousands of deaths caused by resistant pathogens in Africa and Asia [4, 5].
In Nanoro, a rural malaria-endemic area, many cases of fever have been reported in children under 5 years of age with many of them being malaria infection [1, 6]. Next to malaria, bacterial, viral, or other parasitic infections are also common and may cause fever [7, 8]. However, only bacterial febrile infections should be treated with antibiotics, as for other febrile infections the use of antibiotics may not be justified [5, 9]. In such context, proper diagnosis is therefore essential in order to make right treatment decisions. Nevertheless, in many rural and resource limited settings apart from the malaria rapid diagnostics tests (RDTs) [6, 9,10,11,12], there are not many diagnostic tools available to support the clinical diagnosis of other febrile diseases. Consequently, antibiotics are regularly prescribed to malaria-negative cases without knowing the actual cause of fever and this contributes to increasing antibiotic resistance.
In order to tackle antimicrobial resistance, there is a pressing need to develop better diagnostic strategies to improve the management of non-malaria fever in remote areas lacking suitable laboratory infrastructure. Next to malaria, it is highly relevant to develop diagnostic strategies for bacterial and viral infections as the later do not require treatment with antibiotics. C-reactive protein (CRP) is a relatively accurate and sensitive marker for inflammation and infection, and could be an indication of a (possible) bacterial infection [13,14,15]. The use of a RDT that can semi-quantitatively determine CRP levels could therefore support the diagnosis and management of febrile diseases and may reduce the inappropriate prescription and use of antimicrobials [16,17,18,19,20]. In bacterial infections with severe inflammations, CRP level is between 40 and 200 mg/L. Furthermore, in some severe bacterial infections or burns, CRP level can increase above 200 mg/L, after 48 h of the occurrence of an acute event [19]. In contrast, CRP level is in general between 10 and 40 mg/L in viral infections with mild inflammations [13, 14, 20].
In the routine practice in Burkina Faso rural health centers, febrile children are screened with a malaria RDT based on the detection of Plasmodium falciparum specific histidine-rich protein 2 (mRDT-PfHRP2). RDT-positive cases are treated with appropriate anti-malaria drugs as recommended by the National Malaria Control Program (NMCP) guidelines [21]. Despite its relatively good sensitivity [6, 9,10,11,12], the use of PfHRP2 RDT alone does not allow for the diagnosis of all causes of fever. Consequently, febrile cases tested negative for malaria by RDT are often systematically treated with antibiotics, which contributes to overuse of antimicrobials [22,23,24,25]. Moreover, local health workers sometimes also tend to prescribe antibiotics to mRDT-PfHRP2-positive children in addition to antimalarials. This is might be due to the fact that the health workers want to be certain that they have adequately treated the febrile cases and that a child is not sent away with no or wrong medication [26]. This attitude contributes further to the over prescription of antibiotics. To circumvent this problem, we explored in this study whether a combination of screening with PfHRP2 RDT and a semi-quantitative CRP RDT could improve the diagnosis of febrile illnesses in a population of feverish children under 5 years of age in a rural area in Burkina Faso and increases the adequate prescription of antimicrobials.
Methods
Study design
We prospectively included 396 children under 5 years of age with an axillary temperature of ≥ 37.5 °C in this study. Recruitment was carried out from April to December 2016 in the Nanoro Health District catchment area (Burkina Faso). Nanoro is a malaria-endemic area, located in the Central–West region of Burkina Faso at approximately 100 km from Ouagadougou, the capital city. This study was conducted in the framework of a large project (RAPDIF: a rapid diagnostic test for undifferentiated fevers; which is supported by a grant from the Netherlands Organisation for Health Research and Development (ZonMw), project 205300005), which aims to improve the diagnosis and management of febrile illness in children under 5 years of age [8].
A whole blood sample was collected from each included child for malaria screening (at enrolment) and CRP testing with RDTs, for blood culture and for malaria microscopy. In total 396 blood samples were collected and analyzed in this manner. In addition, we collected 226 stool samples and 224 urine samples from these children for microbiological analyses. All laboratory analyses were performed according to established standard operating procedures (SOPs) of the Clinical Research Unit of Nanoro (CRUN) laboratory. A primary clinical diagnosis for the management of febrile children was done by health facility nurses following the Integrated Management of Childhood Illness (IMCI) guidelines [26]. The experimental procedures (microbiological analysis, CRP testing and microscopy) were not taken into account when treatment was installed at the primary health care facilities. The prescription of antimicrobials (i.e., either an anti-malarial as recommended by the Burkinabe NMCP, or antibiotics, or both) was recorded on case record form (CRF). Whenever results of laboratory testing became available, these were communicated to the health facilities staff to allow them to adjust treatments (if needed) and to ensure better case management.
Written informed consent was obtained from a parent or legal guardian of each child before enrollment. The study protocol was approved by the National Ethical Committee for Health Research of Burkina Faso (Deliberation No. 2014-11-130).
Laboratory procedures
To determine whether or not CRP testing added to malaria RDT testing could be helpful in defining the actual cause of febrile illness, we combined the result of the RDT-PfHRP2 RDT and that of semi-quantitative CRP test (results categorized in three groups: < 10 mg/L, 10–40 mg/L, and > 40 mg/L) with those of bacterial bloodstream infections, bacterial gastroenteritis, bacterial urinary tract infections, parasitic gastroenteritis, and viral gastroenteritis.
Infections caused by Salmonella species isolated from blood and stool samples, Escherichia coli from blood and urine, Streptococcus pneumoniae, Haemophilus influenzae b, and Enterobacter agglomerans from blood are considered as infections that require treatment with antibiotics. Gastroenteritis caused by enteropathogenic Escherichia coli (EPEC) is not treated with antibiotics in Burkina Faso like in the majority of West African Countries [27, 28].
Malaria rapid diagnostic test
Malaria diagnosis was performed at enrolment with a PfHRP2 protein based RDT (SD Ag Bioline Pf; Standard Diagnostics, Hagal-Dong, Korea) according to the manufacturer’s instruction. This RDT is recommended by the NMCP of Burkina Faso [21]. The results of mRDT-PfHRP2 were (for the purpose of the present study) used for the definition of a malaria case as this is the routine diagnostic practice in the participating health centers. Test results were recorded on study CRFs.
Microscopy
Thin and thick blood smears were prepared from blood collected in Ethylene Diamine Tetra Acetic acid (EDTA) tubes and fixed with ethanol (thin slides) and stained with 3% Giemsa solution (pH 7.2). Two certified expert microscopists independently read the blood smears in order to search for Plasmodium species. In case of discordance, the slides were read by a third independent expert microscopist whose conclusion was decisive.
C-reactive protein (CRP) rapid test
CRP testing was performed using the semi-quantitative Actim® CRP RDT (Oy Medix Biochemical, Joensuu, Finland). This RDT allows for the semi-quantitative determination of CRP serum concentrations into 4 categories: (i) < 10 mg/L; (ii) between 10 and 40 mg/L; (iii) between 40 and 80 mg/L; (iv) and > 80 mg/L. Tests were performed according to the manufacturer’s instructions and read by two technicians who independently recorded the test results. The Actim® CRP RDT has an internal control line, which confirms the performance (accuracy) of the test.
Microbiology procedures
The microbiology procedures used for this study have been described in detail elsewhere [8]. Briefly, blood cultures were performed on 1 to 3 mL of venous blood samples collected in Pediatric blood culture bottles (BD BACTEC Peds PlusTM/F, Becton Dickinson, and Company, Sparks, Maryland, USA) from the enrolled children and incubated in a BACTEC 9050 instrument (Becton Dickinson) for 5 days according to the manufacturer’s instructions. Pathogens present in positive blood cultures were identified by standard microbiological and biochemical methods [29,30,31].
Fresh stool samples collected in sterile containers by study nurses were subject to culture, microscopy, and Rota/adenovirus RDT testing. Firstly, we cultured the stool on Sodium Selenite broth and on appropriate agar followed by an incubation at 35–37 °C for 18–24 h. Subsequently, we identified suspected colonies (i.e., Salmonella species, Shigella species, and enteropathogenic Escherichia coli [EPEC; only for children under 2 years]) by standard microbiological and biochemical methods (API system, bioMerieux Marcy-L’Etoile, France) [29,30,31]. Secondly, we performed a specific analysis of stools for the qualitative detection of group A rotavirus and adenovirus serotypes 40 and 41 in human stool samples using a Rota/Adenovirus antigen rapid diagnostic test (SD Bioline Rota/Adeno; Standard Diagnostic, Inc., Korea). Finally, we performed a microscopic examination of the stool to search for intestinal parasites.
Urine samples were collected in sterile containers and tested using urine dipsticks (Standard Diagnostics, Urocolor, Inc, Korea). All samples tested positive for leukocytes and nitrite were cultured on appropriate agar and incubated for 18–24 h at 35–37 °C. Samples that resulted pure bacterial growth of > 105 colonies forming units (CFU)/mL were considered significant bacteriuria [32] and we identified the bacterial isolates according to biochemical methods (API system, bioMerieux Marcy-L’Etoile, France).
Quality control procedures
To ensure the quality of the samples’ analysis, all experiments were conducted according to the standard laboratory operating procedures (SOPs) in place at CRUN laboratory. Furthermore, there was strict adherence to manufacturers’ instructions. For the semi-quantitative CRP rapid test and mRDT-PfHRP2, the internal control lines confirmed the correct performance of these tests. In addition, we perform monthly internal quality controls of reagents and equipment using American Type Culture Collection (ATCC) standard reference strains. It is important to mention that the CRUN laboratory is subjected to external quality control organized by world health organization (WHO) and national institute for communicable diseases (NICD, South Africa). Finally, at CRUN laboratory, microscopists are regularly submitted to an external quality control program on quarterly basis and only certified microscopists are allowed to perform malaria slide reading [33].
Data analysis
Data were double entered from study CRFs into OpenClinica software. The data were subsequently analyzed using STATA® statistical software version13 StataCorp LLC, College Station, TX, USA. Qualitative variables description was performed using the percentages. The median and mean were used for quantitative variables distribution. The baseline parasite density was described using geometric means.
Results
Characteristics of study participants
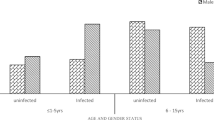
The characteristics of study participants are summarized in Table 1, which also presents the results for diagnostic testing for CRP and malaria by RDT or expert microscopy.
Results of microbiology laboratory analyses are also presented in Table 1 It was found that 64.0% (16/25) bGEs were caused by EPEC not requiring antibiotic treatment. However, 67.3% (33/49) of the bacterial infections must be treated with antibiotics (Table 2). Furthermore, non-bacterial infections (i.e., either a parasitic gastro-enteritis [pGE] or a viral gastro-enteritis [vGE]; see Table 2) were confirmed in 18.7% (74/396) of febrile children. Finally, there were 81 febrile cases (20.5%; 81/396) of whom a possible cause of febrile illness could not be established.
Laboratory results categorized according to CRP levels
Most of the children who were tested RDT positive for malaria also had a CRP positive test (93.4%; 254/272). But of those who were tested negative for malaria by RDT, 35.5% (44/124) also had a negative CRP test (see Table 2). In contrast, 80 (64.5%) cases that were mRDT negative had a positive CRP test. Furthermore, the majority of children for whom a bacterial infection was confirmed by microbiology analyses, were also tested positive with the CRP test (85.7%; 42/49). In the case of confirmed non-bacterial infections, positive CRP levels were found in 85.1% (63/74) of the febrile children. Altogether, a relatively low number of febrile cases with confirmed infection, either a bacterial infection (7/49; 14.3%) or a non-bacterial (11/74; 14.9%) were tested negative for CRP (< 10 mg/L).
In febrile children where no infection was diagnosed (20.5%; 81/396), and whose actual cause of fever remained unknown, the CRP test was positive in 63.0% (51/81) of the cases and negative in 37.0% (30/81) of the children (Table 2).
Distribution of mRDT-PfHRP2 and RDT-CRP results over non-malaria infections
A more detailed distribution over the number of positive/negative mRDT-PfHRP2 tests and CRP testing over the different types of non-malaria infections found by microbiology analysis is presented in Table 3. In febrile children with a positive mRDT-PfHRP2 test (68.7%; 272/396), we also diagnosed a total of 30 bacterial infections but all are not treated with antibiotics. Among those, 12 bBSI and 18 bGE were diagnosed of which 10 bGEs were caused by EPEC that is not treated in accordance with the Burkinabe treatment guidelines. Furthermore, we also diagnosed 52 non-bacterial infections in mRDT-PfHRP2 positive cases.
In febrile children with a confirmed bacterial infection and who were tested negative with mRDT-PfHRP2 (n = 19), there were 14 cases who were tested CRP positive and 5 were tested CRP negative. There were 22 cases of confirmed non-bacterial infection of whom 14 were tested mRDT-PfHRP2 negative but CRP positive and 8 who were tested negative for both RDTs.
Of the 81 cases who were tested negative with mRDT-PfHRP2 and for whom the cause of fever could not be explained by the identification of an infective agent, there were 51 cases (63.0%) with a positive CRP test and 30 cases (37.0%) with a negative CRP test.
Prescription of antimicrobials by health staff
All cases (n = 272; see Table 4) with a positive mRDT-PfHRP2 should have been treated with anti-malarials. Indeed, 265 (97.4%) of the children in this group did actual receive anti-malarials, but 7 children (2.6%) did not but the reason for this was not recorded in the CRFs (see Table 4). Furthermore, there were 147 (54.0%) malaria cases who were also additionally treated with one antibiotic and 10 (3.7%) with even 2 additional antibiotics (see Table 4).
Children who were tested negative with mRDT-PfHRP2 (n = 124) should not get anti-malarial treatment, but there were 46 children (37.1%; 46/124) who still received anti-malarials. In addition, 88 (71.0%; 88/124) mRDT-PfHRP2 negative children were treated with 1 antibiotic, 22 children (17.7%) in this group were treated with 2 antibiotics and 1 child even received treatment with 3 antibiotics, irrespective of knowing the actual cause of fever.
Based on the microbiology analyses we can also categorize what treatments were provided to the febrile children who actually had a bacterial infection. In the group of children with a confirmed bBSI (n = 23), there were 15 (65.2%) who received anti-malarials and 8 (34.8%) who did not. Importantly, 7 children (30.4%) with a confirmed bBSI did not receive antibiotic treatment, whereas 13 (56.5%) received 1 antibiotic and 3 (13.0%) were prescribed 2 antibiotics.
Nineteen children (76.0%; 19/25) with a confirmed bGE received anti-malarials. In terms of antibiotics prescriptions, there were 11 children (44.0%) with a bGE who did not receive antibiotics, 12 (48.0%) were prescribed one antibiotic and two children (8.0%) with bGE received two antibiotics.
One child with a bacterial urinary tract infection did not receive antimalarials, but did receive two antibiotics.
Effect of additional CRP testing on the prescription of antimicrobials
As a result of the customary diagnostic approach to manage febrile cases in place in the rural health centers in our study area, febrile children with a positive mRDT-PfHRP2 are treated with anti-malarials and those with a negative malaria RDT with antibiotics. Consequently, we diagnosed 272 malaria cases by mRDT, who should receive anti-malarial treatment as recommended by the NMCP guidelines of Burkina Faso. Of note is that within this positive mRDT-PfHRP2 group, 20 cases (7.4%) had also bacterial infection confirmed by microbiology analyses and that needed antibiotic treatment (see Table 5). However, due to the normal diagnostic approach in place, they have not been treated as such. In this respect, additional CRP testing will not improve the management of these particular 20 cases as per default they will only receive anti-malarial treatment on the basis of their positive mRDT result.
Within the group of 124 children with a negative mRDT (and who were given antibiotics for relief), there were 64.5% (80/124) had a positive CRP test and 35.5% (44/124) had a negative CRP test (see Table 3). Therefore, if the results of additional CRP testing were considered for the prescription of antibiotics, the 44 children with a negative CRP test would not have received antibiotic treatment. As a result, this would lead to a reduction of 35.5% of antibiotic prescriptions in the group of febrile children with a negative mRDT-PfHRP2. However, within this group, there were 2 febrile cases (a child with a non-typhoid salmonella blood infection and one with a urinary tract infection caused by E. coli), who actually needed antibiotic treatment, but would on the basis of the negative result of the semi-quantitative CRP test not receive it.
Discussion
Our study aimed to assess whether the combination of semi-quantitative RDT-CRP testing with mRDT-PfHRP2 could improve the diagnosis of febrile illness in rural Burkina Faso, and consequently would lead to a more correct prescription of antimicrobials. Our present study indicates that this approach has proven to be of limited value in our study area. Most cases with malaria infection, also had a high CRP level, which confirms the results of other studies [14, 34, 35]. This makes difficult to detect an additional bacterial infection needing antibiotic treatment in child with a positive mRDT, particularly in our study area where the prevalence of malaria is very high. On the other hand, if the mRDT is negative and the CRP test is positive, malaria infection can indeed be ruled out in most cases. However, in such a case the prescription of antibiotics is not always warranted. For example, parasitic gastro-enteritis, for which antibiotic treatment is not indicated, can often increase the CRP levels [36]. Therefore, in the event of a suspected parasitic gastro-enteritis, microscopic examination of stool is highly recommended to better determine the actual cause of fever. In addition to this, microscopic testing for Plasmodium infection, the gold standard for malaria diagnosis, should be reconsidered in areas with high malaria prevalence and with the risk of significant numbers of false-positive mRDTs, in particular due to persisting HRP2 antigen [6, 11, 36]. Another potential drawback that threatens the use of HRP2-based mRDTs are potential false negatives results due to HRP2/HRP3 genes deletion or mutation [37]. However, according to a very recent systematic review and meta-analysis these mutations have not (yet) been found in Burkina Faso, but their potential occurrence needs to be carefully monitored [38].
The strength of combined mRDT and CRP testing is highlighted in our study in case both tests are negative. This was the case in 44 children of whom the majority of the children, did indeed not need either anti-malarial and/or antibiotics treatment. However, if this diagnostic approach is followed, two children will be denied essential antimicrobial treatment. In this respect, health policymakers, will have to consider whether not treating this particular small group of children outweighs the savings in prescribing antimicrobials in general or not.
In our study area, as was also previously reported malaria remains one of the most important causes of febrile illness [1, 39]. However, in this study, next to malaria, a significant proportion of febrile children were infected with bacterial pathogens or parasitic or viral gastroenteritis. There was also a group of children for whom the actual cause of febrile illness could not be established. A part of these children could have a viral infection responsible for fever, e.g., viral infection of the respiratory tract [39]. Unfortunately, we were not able to confirm these infections as our laboratory, like in many low-and middle-income countries, lacks the facilities to establish this, and this is a limitation of our study.
Another limitation of our work is that the current study design did not allow for statistical testing of sensitivity and specificity of the combined malaria and CRP testing. This is due to the fact that a majority of those recruited suffered from malaria and therefore will have inflammation ongoing. Perhaps performing a similar survey of the RDTs in a less malaria endemic region could indicate if the combined approach could be more useful.
According to the NMCP guidelines in Burkina Faso, a febrile child who is tested positive by mRDT should receive appropriate anti-malarial treatment. In our study, health workers tend to adhere well to this guideline and this is in line with previous observations done in the same study area [24, 40]. However, several mRDT negative children were also prescribed anti-malarials. Health workers are thought to do this in fear of missing a treatable cause of fever, in this case, malaria. Moreover, antibiotics are also widely prescribed to mRDT positive children in the present study. It is not known why health workers use this practice and a targeted social science study towards (changing) this behavior should be conducted to answer this question.
Although, in the present study, additional CRP testing did not provide a perfect solution to reduce over-prescription of antimicrobials. However, there is sufficient evidence that point of care CRP tests can contribute to control or reduce the unnecessary use of antibiotics and decreases the spread of antimicrobial resistance due to their ability to discriminate bacterial from non-bacterial infections in febrile patients [14, 41]. In some settings, where CRP testing is routinely performed in patients with respiratory tract infections, its use has led to a significant reduction of antibiotic prescriptions [42,43,44,45]. Furthermore, CRP testing can be cost-effective, it provides results within a reasonable period of time and it can be implemented in resource-limited settings [18, 46,47,48]. But its use as a single test is not advised in particular in settings where malaria is also highly prevalent [49]. Possibly a combination of mRDT with other acute-phase protein tests such as procalcitonin and/or white blood cell counts next to CRP testings, and supported by a thorough assessment of clinical signs and symptoms could further improve the management of febrile diseases and the prescription of antimicrobials in resource limited-settings [2, 14, 50, 51].
Conclusion
In high malaria-endemic areas, the combined testing of febrile cases with mRDT-PfHRP2 and CRP RDT is only useful in case both tests are negative and a malaria infection can be excluded. This approach could result in a reduction in antibiotic prescriptions in the group of febrile cases, although there is a risk of not treating children with an actual bacterial infection.
Availability of data and materials
The datasets and materials of our study are available from the corresponding author on reasonable request.
Abbreviations
- bBSI:
-
Bacterial bloodstream infection
- bGE:
-
Bacterial gastro-enteritis
- bUTI:
-
Bacterial urinary tract infection
- CRF:
-
Case record form
- CRP:
-
C-reactive protein
- EPEC:
-
Enteropathogenic Escherichia coli
- NMCP:
-
National malaria control program
- Pf-HRP-2:
-
Plasmodium falciparum Specific histidine-rich protein 2
- pGE:
-
Parasitic gastro-enteritis
- RDT:
-
Rapid diagnostic test
- vGE:
-
Viral gastro-enteritis
References
Sondo P, Biebo B, Kazienga A, Valea I, Sorgho H, Ouedraogo J. La part du paludisme dans les maladies fébriles en saison sèche dans la région de Nanoro, Burkina Faso. West Afr J Res Health. 2015;4:29–32.
Lubell Y, Althaus T, Blacksell SD, Paris DH, Mayxay M, Pan-Ngum W, et al. Modelling the impact and cost-effectiveness of biomarker tests as compared with pathogen-specific diagnostics in the management of undifferentiated fever in remote tropical settings. PLoS ONE. 2016;11(3): e0152420.
Prasad N, Sharples KJ, Murdoch DR, Crump JA. Community prevalence of fever and relationship with malaria among infants and children in low-resource areas. Am J Trop Med Hyg. 2015;93(1):178–80.
O'Neill J. Tackling drug-resistant infections globally: final report and recommendations: Government of the United Kingdom; 2016.
CDC. Antibiotic resistance threats in the United States. Centers for Disease Control and Prevention; US Department of Health and Human Services: Atlanta, GA, USA, 2013.
Kiemde F, Bonko MA, Tahita MC, Lompo P, Rouamba T, Tinto H, et al. Accuracy of a Plasmodium falciparum specific histidine-rich protein 2 rapid diagnostic test in the context of the presence of non-malaria fevers, prior anti-malarial use and seasonal malaria transmission. Malar J. 2017;16:294s.
D’acremont V, Kilowoko M, Kyungu E, Philipina S, Sangu W, Kahama-Maro J, et al. Beyond malaria—causes of fever in outpatient Tanzanian children. N Eng J Med. 2014;370(9):809–17.
Kiemde F, Spijker R, Mens PF, Tinto H, Boele M, Schallig HD. Aetiologies of non-malaria febrile episodes in children under 5 years in sub-Saharan Africa. Trop Med Int Health. 2016;21(8):943–55.
Gould IM, Bal AM. New antibiotic agents in the pipeline and how they can help overcome microbial resistance. Virulence. 2013;4(2):185–91.
Halidou T, Olivier S, Innocent V, Ferdinand L, Sandrine Y, Palpouguini L, et al. Field evaluation of SD Bioline Malaria Antigen Pf® for Plasmodium falciparum malaria diagnosis in Nanoro, Burkina Faso. Afr J Parasitol Res. 2015;4(11):161–5.
Maltha J, Guiraud I, Lompo P, Kabore B, Gillet P, Van Geet C, et al. Accuracy of PfHRP2 versus Pf-pLDH antigen detection by malaria rapid diagnostic tests in hospitalized children in a seasonal hyperendemic malaria transmission area in Burkina Faso. Malar J. 2014;13:20.
WHO. Malaria rapid diagnostic test performance. Results of WHO product testing of malaria RDTs: round 7 (2015–2016). World Health Organization: Geneva, Switzerland, 2017.
Ansar W, Ghosh S. C-reactive protein and the biology of disease. Immunol Res. 2013;56(1):131–42.
Lubell Y, Blacksell SD, Dunachie S, Tanganuchitcharnchai A, Althaus T, Watthanaworawit W, et al. Performance of C-reactive protein and procalcitonin to distinguish viral from bacterial and malarial causes of fever in Southeast Asia. BMC Infect Dis. 2015;15(1):511.
Hirschfield G, Pepys M. C-reactive protein and cardiovascular disease: new insights from an old molecule. Q J Med. 2003;96(11):793–807.
Althaus T, Greer RC, Swe MMM, Cohen J, Tun NN, Heaton J, et al. Effect of point-of-care C-reactive protein testing on antibiotic prescription in febrile patients attending primary care in Thailand and Myanmar: an open-label, randomised, controlled trial. Lancet Glob Health. 2019;7(1):e119–31.
Diez-Padrisa N, Bassat Q, Morais L, O’Callaghan-Gordo C, Machevo S, Nhampossa T, et al. Procalcitonin and C-reactive protein as predictors of blood culture positivity among hospitalised children with severe pneumonia in Mozambique. Trop Med Int Health. 2012;17(9):1100–7.
Joshi A, Perin DP, Gehle A, Nsiah-Kumi PA. Feasibility of using C-reactive protein for point-of-care testing. Technol Health Care. 2013;21(3):233–40.
Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999;17(6):1019–25.
Chew KS. What’s new in Emergencies Trauma and Shock? C-reactive protein as a potential clinical biomarker for influenza infection: More questions than answers. J Emerg Trauma Shock. 2012;5(2):115–7.
Ministry of Health BF. Directives nationales pour la prise en charge du paludisme dans les formations sanitaires du Burkina Faso. Programme National de Lutte contre le Paludisme; World Health Organization: Geneva, Switzerland, 2014. Mars 2014:1–31.
Msellem MI, Mårtensson A, Rotllant G, Bhattarai A, Strömberg J, Kahigwa E, et al. Influence of rapid malaria diagnostic tests on treatment and health outcome in fever patients, Zanzibar—a crossover validation study. PLoS Med. 2009;6(4): e1000070.
D’Acremont V, Kahama-Maro J, Swai N, Mtasiwa D, Genton B, Lengeler C. Reduction of anti-malarial consumption after rapid diagnostic tests implementation in Dar es Salaam: a before-after and cluster randomized controlled study. Malar J. 2011;10(1):107.
Bonko MDA, Kiemde F, Tahita MC, Lompo P, Some AM, Tinto H, et al. The effect of malaria rapid diagnostic tests results on antimicrobial prescription practices of health care workers in Burkina Faso. Ann Clin Microbiol Antimicrob. 2019;18(1):5.
Hopkins H, Bruxvoort KJ, Cairns ME, Chandler CI, Leurent B, Ansah EK, et al. Impact of introduction of rapid diagnostic tests for malaria on antibiotic prescribing: analysis of observational and randomised studies in public and private healthcare settings. BMJ. 2017;356: j1054.
WHO. IMCI Chart Booklet. Geneva: World Health Organization; 2014.
Ministry of Health BF. Guidelines of diagnostic and treatment of Burkina. Geneva: World Health Organization; 2009.
Dupont C. Diarrhées aiguës de l’enfant. J Pediatr Pueric. 2010;23(2):84–95.
Mahon C, Manuselis G, Lehman D. Textbook of diagnostic microbiology. 2nd ed. Philadelphia: Pa WB Saunders; 2000.
Winn WC. Koneman’s color atlas and textbook of diagnostic microbiology. Philadelphia: Lippincott williams & wilkins; 2006.
Versalovic J, Carroll KC, Landry ML, Funke G, Jorgensen JH. Manual of clinical microbiology. 10th ed. Washington: American Society of Microbiology; 2011.
Hinman F. The meaning of significant bacteriuria. JAMA. 1963;184(9):727–8.
Tinto H, Valea I, Sorgho H, Tahita MC, Traore M, Bihoun B, et al. The impact of clinical research activities on communities in rural Africa: the development of the Clinical Research Unit of Nanoro (CRUN) in Burkina Faso. Malar J. 2014;13:113.
Mahende C, Ngasala B, Lusingu J, Mårtensson T, Lushino P, Lemnge M, et al. Profile of C-reactive protein, white cells and neutrophil populations in febrile children from rural north-eastern Tanzania. Pan Afr Med J. 2017;26:51.
Sarfo BO, Hahn A, Schwarz NG, Jaeger A, Sarpong N, Marks F, et al. The usefulness of C-reactive protein in predicting malaria parasitemia in a sub-Saharan African region. PLoS ONE. 2018;13(8): e0201693.
Al-Ezzy AIA, Abood WN, Hussein RA. C-reactive protein as an immunopathological prognostic marker for Giardia lamblia and Entamoeba histolytica associated diarrhea among children of Baghdad Governorate. IJASR. 2015;1(01):33–7.
Rogier E, McCaffery JN, Nace D, Svigel SS, Assefa A, Hwang J, et al. Plasmodium falciparum pfhrp2 and pfhrp3 Gene deletions from persons with symptomatic malaria infection in Ethiopia, Kenya, Madagascar, and Rwanda. Emerg Infect Dis. 2022;28(3):608–16.
Molina-de la Fuente I, Pastor A, Herrador Z, Benito A, Berzosa P. Impact of Plasmodium falciparum pfhrp2 and pfhrp3 gene deletions on malaria control worldwide: a systematic review and meta-analysis. Malar J. 2021;20(1):276.
Kiemde F, Tahita MC, Lompo P, Rouamba T, Some AM, Tinto H, et al. Treatable causes of fever among children under five years in a seasonal malaria transmission area in Burkina Faso. Infect Dis Poverty. 2018;7(1):60.
Ruizendaal E, Schallig HD, Scott S, Traore-Coulibaly M, Bradley J, Lompo P, et al. Evaluation of malaria screening during pregnancy with rapid diagnostic tests performed by community health workers in Burkina Faso. Am J Trop Med Hyg. 2017;97(4):1190.
Gaynes R, Levy S. Improving outpatient antibiotic prescribing for respiratory tract infections: results of new algorithms used in European trials. Infect Control Hosp Epidemiol. 2015;36(6):725–9.
Huang Y, Chen R, Wu T, Wei X, Guo A. Association between point-of-care CRP testing and antibiotic prescribing in respiratory tract infections: a systematic review and meta-analysis of primary care studies. Br J Gen Pract. 2013;63(616):e787–94.
Minnaard MC, van de Pol AC, Broekhuizen BD, Verheij TJ, Hopstaken RM, van Delft S, et al. Analytical performance, agreement and user-friendliness of five C-reactive protein point-of-care tests. Scand J Clin Lab Invest. 2013;73(8):627–34.
Oppong R, Jit M, Smith RD, Butler CC, Melbye H, Mölstad S, et al. Cost-effectiveness of point-of-care C-reactive protein testing to inform antibiotic prescribing decisions. Br J Gen Pract. 2013;63(612):e465–71.
Cals JW, Schot MJ, de Jong SA, Dinant G-J, Hopstaken RM. Point-of-care C-reactive protein testing and antibiotic prescribing for respiratory tract infections: a randomized controlled trial. Ann Fam Med. 2010;8(2):124–33.
Hunter R. Cost-effectiveness of point-of-care C-reactive protein tests for respiratory tract infection in primary care in England. Adv in Ther. 2015;32(1):69–85.
Aabenhus R, Jensen J-US, Jørgensen KJ, Hróbjartsson A, Bjerrum L. Biomarkers as point-of-care tests to guide prescription of antibiotics in patients with acute respiratory infections in primary care. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD010130.pub2.
Kokko E, Korppi M, Helminen M, Hutri-Kahonen N. Rapid C-reactive protein and white cell tests decrease cost and shorten emergency visits. Pediatr Int. 2014;56(5):698–701.
Escadafal C, Incardona S, Fernandez-Carballo BL, Dittrich S. The good and the bad: using C reactive protein to distinguish bacterial from non-bacterial infection among febrile patients in low-resource settings. BMJ Glob Health. 2020;5(5): e002396.
Bertoli G, Ronzoni N, Silva R, Spinicci M, Perlini C, Omega L, et al. Usefulness of C-Reactive protein and other host biomarker point-of-care tests in the assessment of non-malarial acute febrile illnesses: a systematic review with meta-analysis. Am J Trop Med Hyg. 2020;103(5):1797.
Ivaska L, Niemelä J, Leino P, Mertsola J, Peltola V. Accuracy and feasibility of point-of-care white blood cell count and C-reactive protein measurements at the pediatric emergency department. PLoS ONE. 2015;10(6): e0129920.
Acknowledgements
We would like to thank all study staff from “Institut de Recherche en Sciences de la Santé- Direction Régionale du Centre-Ouest/Unité de Recherche Clinique de Nanoro, Burkina Faso”, the participating rural health facilities (Nanoro, Godo, Nazoanga, and Seguedin), the hospital CMA Saint Camille de Nanoro and the Laboratory for Experimental Parasitology at the Amsterdam UMC their contributions to the work. We are indebted to the parents or guardians of the recruited children for providing informed consent and allowing their children to participate in our study.
Funding
The work was funded by a grant from The Netherlands Organization for Health Research and Development (ZonMw), Project 205300005; RAPDIF: a rapid diagnostic test for undifferentiated fever; and by a Discovery Award granted to the research team from the NESTA foundation (London, United Kingdom) to support research on antibiotic resistance.
Author information
Authors and Affiliations
Contributions
MB, FK, MT, PM, HT, and HS conceived and designed the study. Recruitment of children and clinical specimen collection was supervised by MB, IK, and MT, the latter also being responsible for the supervision of laboratory testing of the samples collected from febrile children. MB, IK, FK, SY, LP, and MT supervised patient enrollment and study nurses who obtained the informed consent from parents or legal guardians at enrollment of febrile children and who collected specimens for laboratory analyses. Laboratory analyses were performed by MB, IK, ZG, FK, SY, and LP, checked and validated by MT. MB and HS analyzed the data. MB and HS drafted the manuscript and this was reviewed by all other authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was received and approved by the National Ethical Committee in Health Research of Burkina Faso (Deliberation No. 2014-11-130). Written informed consent for the participation of the febrile children was obtained from parents or legal guardians prior their enrolment in the study.
Consent for publication
Not applicable.
Competing interests
The authors report who they have not competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bonko, M.d.A., Karama, I., Kiemde, F. et al. Could combined rapid diagnostic testing for malaria and c-reactive protein be helpful for the diagnosis and management of febrile illnesses in children under-5 years of age in rural Burkina Faso?. BMC Infect Dis 22, 952 (2022). https://doi.org/10.1186/s12879-022-07638-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07638-2