Abstract
Background
Carbapenem-resistant Acinetobacter baumannii (CRAB) is among the most concerning cause of healthcare-associated infections (HAI) due to its high level of antibiotic resistance and high mortality. In the era of the COVID-19 pandemic, the key priority of infection control committees is to contain the dissemination of antibiotic resistant Gram-negative bacteria. Here, we aimed to timely recognize the emergence of CRAB in COVID-19 cases admitted to the wards of a tertiary referral hospital and to identify the genetic relatedness of the isolates.
Methods
From 30 March to 30 May 2020, a total of 242 clinical samples from COVID-19 cases were screened for CRAB isolates using standard microbiologic and antibiotic susceptibility tests. The PCRs targeting oxa23, oxa24, oxa58, blaTEM and blaNDM-1 genes were performed. Two multiplex PCRs for identifying the global clones (GC) of A. baumannii were also performed. The sequence type of CRABs was determined using Institut Pasteur (IP) multilocus sequence typing (MLST) scheme.
Results
Eighteen CRAB isolates were recovered from COVID-19 patients with the mean age of 63.94 ± 13.8 years. All but 4 COVID-19 patients co-infected with CRAB were suffering from an underlying disease. Death was recorded as the outcome in ICUs for 9 (50%) COVID-19 patients co-infected with CRAB. The CRAB isolates belong to GC2 and ST2IP and carried the oxa23 carbapenem resistance gene.
Conclusion
This study demonstrated the co-infection of CRAB isolates and SARS-CoV-2 in the patients admitted to different ICUs at a referral hospital in Tehran. The CRAB isolates were found to belong to ST2IP, share the oxa23 gene and to have caused several outbreaks in the wards admitting COVID-19 patients.
Similar content being viewed by others
Background
Acinetobacter baumannii is an emerging Gram-negative pathogen that causes a variety of healthcare-associated infections (HAI), including ventilator-associated pneumonia (VAP), central line-associated bloodstream infections and catheter-associated urinary tract infections [1]. The outbreaks of A. baumannii infections tend to occur in intensive care units (ICUs) with critically ill patients [2].
Carbapenems are considered as the first-line antimicrobials for treatment of infections caused by antibiotic-resistant Gram-negative bacteria [3]. The carbapenem resistance emerged in A. baumannii shortly after the introduction and therapeutic use of carbapenems and disseminated globally [4, 5]. To date, two major clonal complexes, namely global clones 1 and 2 (GC1 and GC2), have been reported to be mostly responsible for the resistance of this microorganism [6]. The emergence of carbapenem-resistant A. baumannii (CRAB) has been a great concern in clinical practice, as it reduces the therapeutic options for patients [7]. The Centre for Disease Control (CDC) listed the multidrug-resistant Acinetobacter as “Serious threat” in 2013 [8]; however, it reported CRAB as “Urgent threat” in 2019. This threat level increased due to the lack of new antibiotics for treatment as well as the widespread dissemination of resistance among the isolates in healthcare settings [9]. The carbapenem resistance in A. baumannii is significantly associated with the carbapenem hydrolysing oxacillinases encoded by the oxa23, oxa24 and oxa58 genes which are found on mobile genetic elements and can be disseminated among bacteria [10, 11].
Following the first report of two cases of coronavirus disease of 2019 (COVID-19) in Qom province, Iran, in February 2019, other provinces including the capital city, Tehran, was also affected [12]. With the beginning of the first wave of COVID-19 infection and spreading throughout the country, the referral hospitals in the metropolitan area of Tehran started to provide therapeutic and diagnostic services for COVID-19 patients.
The presence of indwelling or invasive medical devices in severely ill patients receiving critical care, intubation or mechanical ventilation [13] and the length of stay (LOS) in the ICU are potentially associated with an increased risk of contracting HAIs, particularly VAP [13]. Due to the lack of FDA-approved treatment [14], the management of patients with COVID-19 will be highly problematic especially when co-infected with antibiotic-resistant bacteria commonly distributed in hospitals. Therefore, the timely recognition of antibiotic-resistant bacteria is important in order to combat the antibiotic resistance and implement the infection and prevention control (IPC) practices. Here, we aimed to detect the CRAB isolates in the wards with COVID-19 cases and determine the genetic relatedness of the CRAB isolates.
Methods
Setting and sampling
Between 30 March and 30 May 2020, a total of 242 clinical samples from COVID-19 patients admitted to one of the five different ICUs at a tertiary referral hospital in Tehran, Iran, were submitted to the laboratory for CRAB screening. This hospital is the largest hospital in Iran with more than 1000 active beds, which serves both admitted and non-admitted patients from Tehran and other cities. Prioritising COVID-19 patients, this hospital housed these patient following the official announcement of the SARS-CoV-2 outbreak in the country. The hospital laboratory began testing specimens obtained from cases suspected of COVID-19 using the reverse transcription-polymerase chain reaction (RT-PCR) kit (Sansure Biotech Inc., China) and targeting SARS-CoV-2. The members of the infection control committee at this hospital strictly adhered to infection control and cross transmission prevention measures.
Patients’ information including the age, gender, ward of admission, source, length of stay in ICU, antibiotic treatment, need for tracheal intubation and/or mechanical ventilation, history of underlying disease and outcome of patients before discharge was obtained from their medical files.
Isolates and identification
One isolate per COVID-19 patient was included in this study. A single colony of each isolate was identified based on the phenotypic tests. Genomic DNA extraction was performed using the standard phenol‐chloroform extraction method followed by PCR targeting oxa-Ab [15, 16].
Antibiotic susceptibility testing
The antibiotics susceptibility of isolates was determined using the disk diffusion method according to CLSI guidelines [17] and against the following antibiotics: imipenem (10 mg), ceftazidime (30 mg), ceftriaxone (30 mg), amikacin (30 mg), gentamicin (10 mg), tetracycline (30 mg), piperacillin/tazobactam (110 mg), ampicillin/sulbactam (20 mg), ciprofloxacin (5 mg), levofloxacin (5 mg) and trimethoprim/sulfamethoxazole (25 mg) (Mast Group Ltd, UK). The CRAB was defined when the isolate was resistant to imipenem [16].
Detection of OXA-type carbapenemases genes
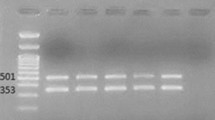
A multiplex PCR was performed to detect oxa23, oxa24 and oxa58 genes in A. baumannii isolates as previously described [18].
Detection of bla TEM and bla NDM-1
PCRs were performed to detect blaTEM and blaNDM-1 genes in A. baumannii isolates as previously described [19, 20].
Identification of global clones
Two multiplex PCR assays amplifying alleles of ompA, csuE and oxa-Ab were performed to identify group 1 (GC2) or group 2 (GC1) as previously described [15].
Multi-locus sequence typing (MLST)
Genetic relatedness of isolates was determined using the Institut Pasteur (IP) multilocus sequence typing scheme. Based on the IP scheme, seven housekeeping genes including cpn60, fusA, gltA, pyrG, recA, rplB, and rpoB were amplified and subjected to sequencing. A sequence type (ST) number was assigned to each isolate according to the allele sequences available on the MLST site (http://pubmlst.org/abaumannii/) [21].
Statistical analysis
Data analysis was performed using SPSS version 18.0 (SPSS Inc., USA). Descriptive results were shown as frequencies and mean. For comparison of the categorical variables, Chi-square and Fisher’s exact tests of nonparametric data were used.
Results
Characteristics of COVID-19 patients
Eighteen (7.4%) out of 242 COVID-19 patients were diagnosed with CRAB co-infection (mean age of 63.94 ± 13.8 years, 12 male and 6 female), of whom 14 were suffering from underlying diseases, such as asthma, cardiovascular diseases, lymphoma, hypothyroidism, diabetes, necrotizing fasciitis, hypertension or chronic kidney disease (Table 1). The mean LOS in ICU for co-infected patients was 13.55 ± 9.15 days and the majority of them (16 of 18) required mechanical ventilation and intubation. Despite different antimicrobial treatments shown in Table 1, death was recorded as the outcome in ICU for 9 (50%) COVID-19 patients co-infected with CRAB.
Properties of the CARB isolates
From 18 CRAB isolates, 11 (61.2%) isolates were recovered from tracheal discharge and the remaining 7 (38.8%) isolates were obtained from blood. The CRAB isolates had similar resistance profiles in the susceptibility test against ceftriaxone amikacin, gentamicin, ampicillin/sulbactam, piperacillin/tazobactam and ciprofloxacin. All CRAB isolates carried oxa23, whereas 5 of them harboured oxa24 (Table 1). All CRAB isolates belonged to GC2 and were found to contain the same MLST profile of 2-2-2-2-2-2-2, which corresponds to ST2IP. These isolates were obtained from COVID-19 patients who were admitted to different wards as follows: ICU1 (n = 1), ICU2 (n = 4), ICU3 (n = 5), ICU4 (n = 2) and ICU5 (n = 6). In the ICUs in which more than one CRAB isolates were found, the number of the isolates containing only oxa23 was higher than those carrying both oxa23 and oxa24. Three isolates contained blaTEM and no isolates carried bla NDM-1.
Discussion
CRAB is one of the emerging causes of HAI, particularly among patients who require devices such as ventilators and blood catheters [1]. In 2017, CRAB was grouped by World Health Organization (WHO) in the list of critical (priority 1) pathogens according to the urgent need for research and development on novel antimicrobial agents [22]. This bacterium causes untreatable infections due its high level of antibiotic resistance and as well as its arsenal of virulence factors, responsible for high mortality rates [23, 24]. Of major concern is that CRAB has the potential for transmission of resistance determinants via mobile genetic elements among the strains in healthcare settings [7]. Therefore, the timely recognition of CRAB, especially in the severely ill patients, is of prime importance. Here, we screened for CRAB among COVID-19 patients who were admitted to different wards in a hospital and investigated the clonal relatedness of the CRAB isolates.
This study showed that one-tenth of COVID-19 patients were co-infected with CRAB, regardless of the need for mechanical ventilation or intubation and of the LOS in ICU. Despite receiving monotherapy or combination therapy, death occurred in a half of patients who had the co-infection of SARS-CoV-2 and CRAB. Another study conducted in Qom, Iran, reported the bacterial co-infection in all COVID-19 patients (n = 19); of which, 90% died after enduring co-infection of multi-drug resistant A. baumannii and SARS-CoV-2 [25]. This rate of co-infection is significantly higher than what we found in the current study. There are also two studies from France [26] and South Africa [27], each reported one case of co-infection of A. buamannii and SARS-CoV-2 with an underlying disease. These studies, however, did not present the resistance profile of the A. baumannii isolate recovered from COVID-19 patients [26, 27]. Ramadan et al., reported the isolation of A. baumannii in 7 out of 260 patients with COVID-19 in Egypt and showed that 5 and 3 isolates were resistant to imipenem and meropenem respectively [28]. The limited therapeutic options against A. buamannii and SARS-CoV-2 highlight the importance of clinical management of complicated cases of COVID-19 when co-infected with antibiotic resistant A. baumannii [14]. The resistance profile of the A. baumannii isolates from COVID-19 patients was previously reported in a study by Sharifipour et al.; however, using phenotypic methods [25], it was unable to explain the possible mechanisms conferring resistance to carbapenems as the front-line treatment for antibiotic-resistant bacteria.
This study revealed that oxa23 was linked to the carbapenem resistance as all CRAB isolates carried this gene. The oxa24 gene also is associated with the carbapenem resistance in some isolates tested here. Although several studies show that oxa23 is the most prevalent gene conferring resistance to carbapenem worldwide [29, 30], it mainly enters into chromosomes or plasmids via transposons [7] compared with oxa24 which is commonly found to be located on plasmids [31,32,33]. As a limitation, this study did not determine the genetic contexts of oxa23 and oxa24 to show whether they were implicated in the dissemination of carbapenemase genes among different isolates in the hospital. Ramadan et al., detected the resistance genes other than OXA genes, including NDM-1, TEM and CTX-M in A. baumannii isolated from COVID-19 patients [28]. We found TEM in three isolates and NDM-1 in none of the isolates.
The assessment of clonal relatedness of the CRAB isolates recovered form COVID-19 patients in different wards at a hospital in Tehran showed that the CRAB isolates belonged to GC2 and the same sequence type (ST2 or ST2IP according to Institut Pasteur scheme). Based on the available genome sequences, ST2 is the most frequent sequence type globally [7]. Previous studies in non-COVID-19 patients showed that the A. baumannii belonging to ST2 of GC2 caused outbreaks in hospital settings [34,35,36]. As yet, there is no study showing the clonal distribution of A. baumannii isolated from COVID-19 patients. Although the CRAB isolates examined here were obtained from patients in different ICUs, they shared oxa23, the sequence type and the phenotypic resistance to several antibiotics. However, a subset of isolates was found to harbour oxa24. This finding may explain the possible colonization of the hospital which is either with the CRAB belonged to ST2 or with the CRAB entered the hospital at some time and subsequently undergone the genetic events resulting in the emergence of the isolates carrying oxa24. This hypothesis needs to be confirmed by metagenomic analysis of the isolates in future studies.
Information on the circulation of CRAB in different ICUs of the hospital before the pandemic revealed the existence of 25 CRAB isolates within 6 months (September 2019 to February 2020); of which, 22 belonged to GC2 and the remaining 3 isolates were non-typeable using multiplex PCRs for identifying the global clone (data not shown). Considering the number (n = 25) of CRAB isolates within 6 months, recovery of 18 isolates during two months in the first wave of the pandemic is unexpected and may imply an outbreak.
Conclusion
This study provided evidence that CRAB isolates belonging to ST2IP and sharing the oxa23 gene have caused several outbreaks in COVID-19 patients. Although the main characteristics of these isolates represented their clonal relatedness, they differ in the antibiotic resistance genes which are mainly encoded on plasmids.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- bla :
-
β-Lactamase
- CTX-M:
-
Cefotaximase-Munich
- CDC:
-
Centers for Disease Control and Prevention
- CRAB:
-
Carbapenem-resistant Acinetobacter baumannii
- FDA:
-
U.S. Food and Drug Administration
- GC:
-
Global clones
- HAI:
-
Health care-associated infections
- IPC:
-
Infection and prevention control
- IP:
-
Institut Pasteur (IP)
- MLST:
-
Multi-locus sequence typing
- ICU:
-
Intensive care unit
- LOS:
-
Length of stay
- oxa :
-
Oxacillinases
- ST:
-
Sequence type
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- RT-PCR:
-
Reverse transcription-polymerase chain reaction
- VAP:
-
Ventilator-associated pneumonia
References
Peleg AY, Hooper DC. Hospital-acquired infections due to Gram-negative bacteria. N Engl J Med. 2010;362(19):1804–13.
Wieland K, Chhatwal P, Vonberg R-P. Nosocomial outbreaks caused by Acinetobacter baumannii and Pseudomonas aeruginosa: results of a systematic review. N Engl J Med. 2018;46(6):643–8.
Codjoe FS, Donkor ES. Carbapenem resistance: a review. Med Sci. 2018;6(1):1.
Paton R, Miles R, Hood J, Amyes S. ARI 1: β-lactamase-mediated imipenem resistance in Acinetobacter baumannii. Int J Antimicrob Agents. 1993;2(2):81–7.
Scaife W, Young HK, Paton RH, Amyes SG. Transferable imipenem-resistance in Acinetobacter species from a clinical source. J Antimicrob Chemother. 1995;36(3):585–6.
Holt K, Kenyon JJ, Hamidian M, Schultz MB, Pickard DJ, Dougan G, et al. Five decades of genome evolution in the globally distributed, extensively antibiotic-resistant Acinetobacter baumannii global clone 1. Microb Genomics. 2016. https://doi.org/10.1099/mgen.0.000052.
Hamidian M, Nigro SJ. Emergence, molecular mechanisms and global spread of carbapenem-resistant Acinetobacter baumannii. Microb Genomics. 2019. https://doi.org/10.1099/mgen.0.000306.
www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.
www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf.
Mugnier PD, Poirel L, Naas T, Nordmann P. Worldwide dissemination of the blaOXA-23 Carbapenemase gene of Acinetobacter baumannii. Emerg Infect Dis. 2010;16(1):35.
Poirel L, Pitout JD, Nordmann P. Carbapenemases: molecular diversity and clinical consequences. Future Microbiol. 2007;2(5):501–12.
Takian A, Raoofi A, Kazempour-Ardebili S. COVID-19 battle during the toughest sanctions against Iran. Lancet (London, England). 2020;395(10229):1035.
Meng L, Qiu H, Wan L, Ai Y, Xue Z, Guo Q, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology. 2020;132(6):1317–32.
Gan CS, RAI V, Rosenthal VD, Chai See LUM L, Wenceslao Orellano P, Hasan MS, et al. Impact of a multidimensional International Nosocomial Infection Control Consortium (INICC) approach on ventilator-associated pneumonia rates and mortality in Intensive Care Units in a Malaysian hospital. Can J Infect Control. 2016;31(4): 230–6.
Drożdżal S, Rosik J, Lechowicz K, Machaj F, Kotfis K, Ghavami S, et al. FDA approved drugs with pharmacotherapeutic potential for SARS-CoV-2 (COVID-19) therapy. Drug Resist Updat. 2020;53:100719.
Turton J, Gabriel S, Valderrey C, Kaufrnann M, Pitt T. Use of sequence-based typing and multiplex PCR to identify clonal lineages of outbreak strains of Acinetobacter baumannii. Clin Microbiol Infect. 2007;13(8):807–15.
CLSI. Performance standards for antimicrobial susceptibility testing. 30th ed. CLSI supplement M100. Wayne PCalSI, 2020.
Woodford N, Ellington MJ, Coelho JM, Turton JF, Ward ME, Brown S, et al. Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int J Antimicrob Agents. 2006;27(4):351–3.
Bailey JK, Pinyon JL, Anantham S, Hall RM. Distribution of the blaTEM gene and blaTEM-containing transposons in commensal Escherichia coli. J Antimicrob Chemother. 2011;66:745–51.
Nordmann P, Poirel L, Carrër A, Toleman MA, Walsh TR. How to detect NDM-1 producers. J Clin Microbiol. 2011;49(2):718–21.
Diancourt L, Passet V, Nemec A, Dijkshoorn L, Brisse S. The population structure of Acinetobacter baumannii: expanding multiresistant clones from an ancestral susceptible genetic pool. PLoS ONE. 2010;5(4):e10034.
WHO. Global priority list of antibiotic-resistant bacteria to guide research and development of new antibiotics; 2017. Geneva: World Health Organisation (WHO).
Ramirez MS, Bonomo RA, Tolmasky ME. Carbapenemases: transforming Acinetobacter baumannii into a yet more dangerous menace. Biomolecules. 2020;10(5):720.
Sarshar M, Behzadi P, Scribano D, Palamara AT, Ambrosi C. Acinetobacter baumannii: an ancient commensal with weapons of a pathogen. Pathogens. 2021;10(4):387.
Sharifipour E, Shams S, Esmkhani M, Khodadadi J, Fotouhi-Ardakani R, Koohpaei A, et al. Evaluation of bacterial co-infections of the respiratory tract in COVID-19 patients admitted to ICU. BMC Infect Dis. 2020;20(1):1–7.
Lescure FX, Bouadma L, Nguyen D, Parisey M, Wicky P-H, Behillil S, et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. 2020. https://doi.org/10.1016/S1473-3099(20)30200-0.
Naidoo P, Naidoo Y. COVID-19, Gram-negative sepsis and a pleuro-peritoneal leak. Pan Afr Med J. 2020. https://doi.org/10.11604/pamj.2020.37.21.25311.
Ramadan HK-A, Mahmoud MA, Aburahma MZ, Elkhawaga AA, El-Mokhtar MA, Sayed IM, et al. Predictors of severity and co-infection resistance profile in COVID-19 patients: first report from Upper Egypt. Infect Drug Resist. 2020;13:3409.
Nigro SJ, Hall RM. Structure and context of Acinetobacter transposons carrying the oxa23 carbapenemase gene. J Antimicrob Chemother. 2016;71(5):1135–47.
Poirel L, Bonnin RA, Nordmann P. Genetic basis of antibiotic resistance in pathogenic Acinetobacter species. IUBMB Life. 2011;63(12):1061–7.
Merino M, Acosta J, Poza M, Sanz F, Beceiro A, Chaves F, et al. OXA-24 carbapenemase gene flanked by XerC/XerD-like recombination sites in different plasmids from different Acinetobacter species isolated during a nosocomial outbreak. Antimicrob Agents Chemother. 2010;54(6):2724–7.
Pailhoriès H, Kempf M, Belmonte O, Joly-Guillou M-L, Eveillard M. First case of OXA-24-producing Acinetobacter baumannii in cattle from Reunion Island, France. Int J Antimicrob Agents. 2016;48(6):763.
Sarı AN, Biçmen M, Gülay Z. The first report on the outbreak of OXA-24/40-like carbapenemase-producing Acinetobacter baumannii in Turkey. Jpn J Infect Dis. 2013;66(5):439–42.
Kanamori H, Parobek CM, Weber DJ, van Duin D, Rutala WA, Cairns BA, et al. Next-generation sequencing and comparative analysis of sequential outbreaks caused by multidrug-resistant Acinetobacter baumannii at a large academic burn center. Antimicrob Agents Chemother. 2016;60(3):1249–57.
Kubo Y, Komatsu M, Tanimoto E, Sugimoto K, Tanaka S, Migita S, et al. Spread of OXA-23-producing Acinetobacter baumannii ST2 and ST246 in a hospital in Japan. J Med Microbiol. 2015;64(7):739–44.
Raible KM, Sen B, Law N, Bias TE, Emery CL, Ehrlich GD, et al. Molecular characterization of β-lactamase genes in clinical isolates of carbapenem-resistant Acinetobacter baumannii. Ann Clin Microbiol Antimicrob. 2017;16(1):1–10.
Acknowledgements
We would like to thank the staff at Laboratory of Microbiology in Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran, for their contribution to this study. The authors would also like to thank Mrs Fariba Zamani for copyediting of this manuscript.
Funding
This research has been supported by grant from Tehran University of Medical Sciences & Health Services (Grant Number: 47508-101-1-99).
Author information
Authors and Affiliations
Contributions
AA has provided the grant. AA did the experiments and wrote a draft. MRS was the clinical advisor of the study. MNS contributed to data collection including the demographic and medical ones. SG did the confirmatory experiments. MD conceptualized the study, reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study proposal was approved by the local ethical committee of Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1399.167). All patients have signed an informed consent for giving the specimens for research. No intervention has been done in diagnosis or treatment of COVID-19 cases. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abdollahi, A., Aliramezani, A., Salehi, M. et al. Co-infection of ST2IP carbapenem-resistant Acinetobacter baumannii with SARS-CoV-2 in the patients admitted to a Tehran tertiary referral hospital. BMC Infect Dis 21, 927 (2021). https://doi.org/10.1186/s12879-021-06642-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06642-2