Abstract
Introduction
Discontinuation of tuberculosis treatment (DTT) among children in sub-Saharan Africa is a major obstacle to effective tuberculosis (TB) control and has the potential to worsen the emergence of multi-drug resistant TB and death. DTT in children is understudied in Uganda. We examined the level and factors associated with DTT among children at four large health facilities in Kampala Capital City Authority and documented the reasons for DTT from treatment supporters and healthcare provider perspectives.
Methods
We conducted a retrospective analysis of records for children < 15 years diagnosed and treated for TB between January 2018 and December 2019. We held focus group discussions with treatment supporters and key informant interviews with healthcare providers. We defined DTT as the stoppage of TB treatment for 30 or more consecutive days. We used a stepwise generalized linear model to assess factors independently associated with DTT and content analysis for the qualitative data reported using sub-themes.
Results
Of 312 participants enrolled, 35 (11.2%) had discontinued TB treatment. The reasons for DTT included lack of privacy at healthcare facilities for children with TB and their treatment supporters, the disappearance of TB symptoms following treatment initiation, poor implementation of the community-based directly observed therapy short-course (CB-DOTS) strategy, insufficient funding to the TB program, and frequent stock-outs of TB drugs. DTT was more likely during the continuation phase of TB treatment compared to the intensive phase (Adjusted odds ratio (aOR), 5.22; 95% Confidence Interval (CI), 1.76–17.52) and when the treatment supporter was employed compared to when the treatment supporter was unemployed (aOR, 3.60; 95% CI, 1.34–11.38).
Conclusion
Many children with TB discontinue TB treatment and this might exacerbate TB morbidity and mortality. To mitigate DTT, healthcare providers should ensure children with TB and their treatment supporters are accorded privacy during service provision and provide more information about TB symptom resolution and treatment duration versus the need to complete treatment. The district and national TB control programs should address gaps in funding to TB care, the supply of TB drugs, and the implementation of the CB-DOTS strategy.
Similar content being viewed by others
Introduction
Tuberculosis (TB) remains one of the leading causes of death among children living with human immunodeficiency virus (HIV) and a major cause of antimicrobial resistance [1,2,3]. Global estimates indicated that 10 million people are newly diagnosed with TB disease on yearly basis, of which 1.2 million are children below 15 years of age. Nearly 650 children with TB die daily and four in every five of the deaths occur before the fifth birthday [4]. About a quarter of the global TB burden is in sub-Saharan Africa, mainly among children with TB/HIV [2]. The protection of children against TB is a cornerstone of social and family culture [5].
In Uganda, it is estimated that the annual incidence of bacteriologically confirmed pulmonary TB, both new and relapse cases, notified in 2019 is nearly 65,900 and the incidence of TB in all forms stands at 200 per 100,000 population [6]. Compared to adults with TB, in children, TB is associated with faster disease progression, severe and complicated forms of TB, and a higher risk of death [7]. Accordingly, prompt diagnosis, early treatment initiation, and treatment complication are important in preventing poor prognosis [7]. Discontinuation of TB treatment (DTT) among children remains a global public health problem [8] and is worst in the sub-Saharan Africa region (1). Several factors are associated with non-adherence and loss to follow-up among TB patients including children in developing countries leading to DTT among children and include among others, long treatment durations, high pill burden, medication-related side-effects, and symptom resolution [9]. DTT thus remains a major obstacle to efficient TB control in developing countries like Uganda and has the potential to worsen the emergence of multi-drug resistant TB and death [10, 11].
Some of the notable approaches to tackling DTT in children include the development of child-friendly policies, an integrated, family-based approach to TB care and services, addressing vulnerabilities faced by children with TB, providing support to their treatment supporters particularly women and the elderly, providing them with social protection, and promoting equitable access to child-friendly formulations of medicines to optimize treatment [12]. Other important approaches to preventing loss-to-follow up and non-adherence aimed at reducing DTT in children include committing to tracking the lost to follow-up children with TB, integrating TB efforts fully into relevant health services [9].
Across the Kampala Capital City Authority (KCCA) health facilities, the review of program data show that the majority of children with TB do not complete the entire 6-months of TB treatment, and data about DTT are limited despite being important in strengthening TB follow-up and retention and improving treatment completion rate. Therefore, we examined the level and factors associated with DTT among children with TB across four purposively selected KCCA health facilities and documented reasons for DTT from the treatment supporter and healthcare provider perspectives.
Methods and materials
Study design and setting
This retrospective study employed both quantitative and qualitative approaches and was conducted at four large TB diagnostic and treatment units in the KCCA between January 2018 and December 2019. The study sites included two health center fours (HC IVs) namely Kisenyi and Kawaala, and two HC IIIs thus Kisugu and Kitebi.
A HC IV is equivalent to a county-level health facility and serves a population of over 100,000 people while a HC III is a parish-level health facility and serves a population of over 40,000 people according to Uganda’s health system. The four study sites are located in the four divisions of Kampala which include; Central, Nakawa, Rubaga, and Makindye divisions. All these study sites provide TB diagnostic, health education, and TB counselling on daily basis, and capture data through the Ministry of Health TB unit registers, and provide TB treatment following the national guidelines. Children below 24 kg (Kgs) are treated with a 6-month anti-TB regimen that consists of 2 months of Isoniazid (I), Rifampicin (R), and Pyrazinamide (Z) as a fixed-dose combination and Ethambutol (E) as an independent tablet in the intensive phase and 4 months of HR in the continuation phase, shortened as 2RHZE, or the 8 months regime that consists of 2 months of RHZE and 6 months of HE abbreviated as 2RHZE/6HE before August 2017 [13]. However, as children approach a body weight of 25 Kgs, the adult doses of anti-TB regimen, a fixed-dose combination of 2RHZE and 4RH is used. For children with TB meningitis or bone TB, treatment lasts for 12 months thus 2 months of RHZE and 10 months of RH, shortened as 2RHZE/10RH.
Study population and sample size
The study population for the quantitative component included the records of all children < 15 years with or without HIV infection, initiated on TB treatment between January 2018 and December 2019. We excluded children with a documented transfer-out status because it was not logistically possible to obtain data about their treatment status. Furthermore, we excluded records for children documented to have multidrug-resistant TB because their treatment takes longer than 6 months, children transferred in but lacked sufficient clinical and treatment histories such as date of treatment initiation, records with missing age information, and children documented to have died.
No sample size was calculated because data were abstracted for a defined period and cohort of children. For the qualitative component, the study population included treatment supporters documented in the TB unit register as caregivers of children with TB and healthcare providers and the sample sizes depended on saturation [14]. Saturation was considered reached when further interviewing of the participants yielded no new information. The treatment supporters were selected purposively on TB clinic days and they were 38 participants in total (8 in the first FGD, 10 in the second FGD, 11 in the third FGD, and 9 in the fourth FGD). A treatment supporter was eligible for the FGD if he/she has been recorded in the TB unit register as the formal caregiver to the child with TB and if he/she was willing to participate in the discussion. We also purposively selected eight health workers within the TB clinic as key informants.
Data collection
Quantitative data were abstracted from the TB unit registers using a standardized data abstraction tool between May and August 2020. The qualitative data were collected through four focus group discussions (FGDs), each consisting of 8–12 treatment supports and key informant interviews with dedicated TB clinic healthcare workers. The FGDs were held within the premises of the health facility in the local language, “Luganda” spoken by the participants, by two research assistants, KA and OB who were trained in qualitative data collection skills and responsible conduct of research. The FGDs were moderated by KL while KA audio-recorded the sessions, took field notes, and probed whenever necessary. On average each FGD lasted for 40–60 min and all the participants were encouraged to ask questions irrespective of the correctness. Some FDG members’ dominance was handled by asking direct probing questions and comments to members who were engaging less. For key informant interviews (KIIs), two healthcare providers namely, one TB focal person and one nursing officer who provide TB treatment at the respective study sites were purposively selected and interviewed to provide expert opinions concerning DTT.
Each key informant interview lasted for 30–45 min, also conducted within the health facility premises in the English language, in a quiet and convenient room. The FGDs and KIIs were conducted until saturation was achieved [14].
Study variables
The dependent variable was DTT, defined as the stoppage of TB treatment for 30 or more consecutive days. The independent variables that were examined included sex, age of the child, type of person with TB namely new or previously treated, TB disease classification, type of directly observed therapy short-course (DOTS) strategy, anti-TB regimen prescribed, TB/HIV comorbidity, residence, referral, and phase of TB treatment. The treatment supporter variables examined included marital status, employment status, relationship with the child with TB, and whether the treatment supporter received pre-treatment counseling. The topics covered in the FGDs and KIIs included: level of knowledge on TB, distance to a health facility, means of transport, alcohol consumption, perceived TB stigma, debilitating illnesses of caregivers, psychosocial issues, knowledge of TB, and stigma and discrimination, and peer and community support.
Statistical analysis
Qualitative data
We identified major themes that emerge from the data. We used NVivo 11(SQR International, Melbourne, Australia) for systematic data management. The coding of the data proceeded as follows: 1) To identify the major codes, all the transcripts were read and coded by two independent reviewers (JI and SO) who have experience and expertise in mixed-methods research.
The independent coding prevented selective perception and interpretive bias and ensured a rigorous coding process; (2) Codes were then compared, and after resolving any discrepancies, a harmonized codebook was developed; and (3) Using the constant comparison method, we developed codes to capture emergent themes. The analysis continued with the refining of the major themes and codes through discussion between investigators.
Quantitative data
The filled data abstraction tool was checked for accuracy and completeness in real-time and then double-entered in Epi-Data version 3.1 [15], with quality control measures such as legal and range values, skip patterns, and alerts. We perform descriptive data analysis where categorical data like sex was summarized using frequencies and percentages, while continuous data like age were summarized using means and standard deviation. In the bivariate analysis, we examined differences in DTT with categorical data using the Chi-square or Fisher’s exact test. For continuous data, the student’s t-test or Wilcoxon-rank sum test was used. Variables with p < 0.15 at bivariate analysis were considered statistically significant for multivariate analysis to control for residual confounding. We used a stepwise generalized linear model, excluding variables that did not improve the fit of the regression model based on the log-likelihood to achieve model parsimony. The results were reported as unadjusted odds ratio (OR) and adjusted odds ratio (aOR), with the corresponding 95% confidence interval (CI). The final model showed a good fit namely, a low Akaike Information Criteria (AIC) of 211.5, statistically insignificant Hosmer-Lemeshow Chi-square test (degree of freedom = 8, statistic < 0.01, p = 1.000), and a large C-statistics or area under the receiver operating curve of 78.5%.
Ethical consideration
The study received ethical approval from Clarke International University Research Ethics Committee (REC number: CLARKE-2020-8). Administrative approval was granted by the Directorate of Public Health and Environment at KCCA. All the respondents provided informed consent after explaining the study purpose, processes, benefits, and potential harms.
Results
Study profile
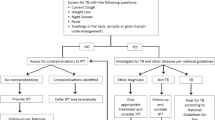
Between January 2018 and December 2019, there were 357 children diagnosed with and treated for TB across the study sites. Of these children with TB, we excluded 45 for the following reasons: 25 had transferred out, 8 were transferred-in, 5 had missing age, and 7 had died. Overall, we analysed data for 312 children with TB (Fig. 1).
Participant’s characteristics and DTT in children
Of 312 participants enrolled, 35 (11.2%) had discontinued TB treatment. 125 (40.1%) participants were aged 6–10 years, 203 (65.1%) females, 255 (81.7%) persons with new TB diagnosis, 178 (57.1%) were cases of CD-PTB and 296 (94.9%) received treatment under community-based DOTS (CB-DOTS). We observed statistically significant differences in DTT with regards to the type of person with TB (p = 0.018), type of DOTS (p = 0.023), TB/HIV co-infection (p = 0.039), and receipt of counselling by the caregiver at the time of TB treatment initiation (p = 0.042) (Table 1).
Reasons for DTT in children
Five sub-themes emerged as reasons for DTT from the qualitative study: 1) no privacy at the healthcare facility to people with TB and their treatment supporters; 2) the disappearance or symptom of TB reduction makes most people with TB discontinue treatment; 3) Poor implementation of CB-DOTS hinders treatment continuation; 4) Insufficient funding prevents the follow-up of lost patients to continue TB treatment, and 5) Frequent stock out of TB drugs frustrates people with TB from continuing with treatment (Table 2).
Factors associated with DTT in children
In the unadjusted analysis (Table 3), we observed CB-DOTS (OR, 0.25; 95% CI, 0.08–0.83) and counselling of treatment supporters at the time of treatment initiation (OR, 0.40; 95% CI, 0.18–0.93) as associated with a lower likelihood of DTT. DTT was more likely among retreatment TB cases compared to the new cases of TB (OR, 2.69; 95% CI, 1.22–5.72) and among children with TB/HIV compared to HIV-negative children with TB (OR, 2.43; 95% CI, 1.10–5.14).
DTT was not associated with being in the age categories of 6–10 years (OR, 0.46; 95% CI, 0.18–1.12) or 11–15 years (OR, 0.69; 95% CI, 0.29–1.62), male sex (OR, 1.90; 95% CI, 0.93–3.87), being a PCD (OR, 0.71; 95% CI, 0.31–1.70) or EPTB case (OR, 2.08; 95% CI, 0.79–5.50), treatment with 2RHZE/4RH (OR, 2.02; 95% CI, 0.90–5.18), being an urban resident (OR, 0.55; 95% CI, 0.27–1.13), referral from health facility (OR, 0.53; 95% CI, 0.16–2.38) and the continuation phase of TB treatment (OR, 2.01; 95% CI, 0.87–4.36). Concerning treatment supporter factors, DTT was not associated with being single (OR, 0.45; 95% CI, 0.10–1.37) or separated (OR, 1.67; 95% CI, 0.71–3.68), employed (OR, 1.99; 95% CI, 0.98–4.12), biological parent (OR, 1.33; 95% CI, 0.47–4.76) or other relative (OR, 1.37; 95% CI, 0.44–5.20).
In the adjusted analysis results (Table 3), DTT was more likely during the continuation phase of TB treatment compared to the intensive phase (aOR, 5.22; 95% CI, 1.76–17.52) and when the treatment supporter was employed compared to when the treatment supporter was unemployed (aOR, 3.60; 95% CI, 1.34–11.38). CB-DOTS showed a tendency toward lower DTT compared to facility-based DOTS (FB-DOTS) but the result remained statistically insignificance (aOR, 0.33; 95% CI, 0.10–1.16).
Discussion
The focus of this study is on DTT among children in Kampala Uganda. Our data show that for every ten children with TB, at least one discontinues TB treatment. The commonest reasons for DTT include lack of privacy at healthcare facilities for children with TB and their treatment supporters, the disappearance of TB symptoms following treatment initiation, poor implementation of the CB-DOTS, insufficient funding to the TB program, and frequent stock-outs of TB drugs. DTT is more likely in the continuation phase of TB treatment and when the treatment supporter is employed. We observed a tendency towards a lower likelihood of DTT when treatment is under CB-DOTS strategy compared to FB-DOTS strategy although the association did not reach statistical significance.
Few studies have looked at DTT among children in Uganda and the sub-Saharan African region. However, the prevalence of DTT in the present study is comparable to that in a previous study in western Uganda [16] but slightly more than half the prevalence of DTT in a Nigerian study [17]. The differences in DTT might be attributable to the study population. The focus of the present study is on children with TB, who mostly depend on adults for continuity of care while the study in Nigeria and Uganda focused on adults with TB who often make independent decisions regarding their health. In general, the high prevalence of DTT among children should be a central concern for the TB control program as it potentially leads to severe forms of TB, TB-related complications, and an increased risk of morbidity and mortality among children with TB. Lack of privacy to people with TB and treatment supporters at the healthcare facilities, the disappearance or reduction in the symptoms of TB symptoms after treatment initiation, the poor implementation of CB-DOTS strategy, insufficient funding that prevents the follow-up of lost patients, and frequent stock-outs of TB drugs were reasons for DTT. To the best of our knowledge, these factors are not unique.
A previous study in eastern Uganda reports that inadequate financing of the TB control program and deficiencies in the implementation of the CB-DOTS strategy is associated with suboptimal treatment success [18]. The study further showed that the disappearance of symptoms of TB especially after treatment initiation results in DTT [18]. Physical and economic barriers have been reported in a previous study as one of the reasons for not completing required sputum smear monitoring visits [19], emphasizing that people with TB face several barriers along the pathway to continuing with treatment. These reasons underscore the importance of strengthening the health system in ensuring adequate financing and sustainable supply of drugs and equipment, among others [20]. The findings further highlight the importance of involving persons with TB and their treatment supporters in TB care [21].
The finding that DTT is more likely in the continuation phase compared to the intensive phase is consistent with previous studies in sub-Saharan Africa [17, 22]. This finding could be explained by several plausible reasons. In the intensive phase of TB treatment, people with TB and their treatment supporters are required to visit TB clinics every 2 weeks to receive health education and treatment. In the continuation phase, the visits occur monthly. This implies that people with TB and their treatment supporters have less contact with health workers in the continuation phase compared to the intensive phase. This possibly might have contributed to laxity among the treatment supporters in helping the children with TB to continue with treatment. Another plausible explanation is that in the continuation phase, most of the symptoms of TB tend to resolve and people with TB feel much better and stronger. The urge to discontinue TB treatment is thus potentially high. One study in eastern Uganda reports that people with TB tended to discontinue treatment when they no longer have symptoms of TB or when they felt better [19]. This finding implies that there is a need to continue providing key messages about TB treatment such as the benefits of treatment completion and the risks associated with DTT in the continuation phase.
There is also a need to explore additional options for the effective delivery of TB treatment in the continuation phase. For example, prospective studies should explore the feasibility and acceptability of multi-month dispensing of TB drugs and the effect on treatment outcomes through implementation science research.
Our study shows that DTT is more likely among treatment supporters with employment compared to the unemployed consistent. No previous study in our setting and elsewhere report similar findings. However, the most socially plausible explanation might be that employed treatment supporters face difficulties in getting time off from their work to travel to TB clinics on regular basis. This potentially leads to DTT.
We found a tendency towards a lower likelihood of DTT for participants under the CB-DOTS strategy compared to the FB-DOTS strategy, which is not surprising. Previous systematic reviews and meta-analyses indicate that the CB-DOTS strategy is associated with favorable treatment outcomes, namely high treatment completion and success rates, and lower mortality and loss to follow-up [23,24,25]. This is because the CB-DOTS strategy improves access to TB treatment since drug refills are done within the community where people with TB and their treatment supporters live and work. In other words, the CB-DOTS strategy overcomes physical and economic barriers that hinder access to TB care and that impact negatively on TB treatment outcomes. Although further research is needed to understand this finding, it could potentially be attributable to the smaller number of participants in the FB-DOTS compared to the CB-DOTS group or disease severity, with those FB-DOTS being sicker than those on CB-DOTS hence at higher risk of adverse outcomes including death. Our finding thus highlights the importance of strengthening the implementation of the CB-DOTS strategy.
Our study has several strengths. This study is among the first few studies to determine DTT among children in Uganda and sub-Saharan Africa. The use of qualitative data to underscore reasons for DTT from the treatment supporter and healthcare provider perspectives further strengthens the quantitative evidence. However, there are limitations to consider. Our study was conducted among children in an urban setting so the findings might not be generalized to a rural setting where access to healthcare is problematic due to longer travel distances. Since we analyzed secondary data, there is a possibility of missing data entries in the TB registers. The study sample size had merely a 45% chance of finding a statistically significant difference assuming DTT is the same in the continuation phase. Our study thus is underpowered to detect a statistically significant difference. The purposive selection of participants could have possibly biased the findings. Also, the lack of individual data from each of the DTT patients to know their reasons is another limitation.
Conclusions and recommendations
This study shows that at least 10% of children with TB discontinue treatment and this might exacerbate TB morbidity and mortality. The main reasons for DTT include lack of privacy at healthcare facilities for people with TB and their treatment supporters, the disappearance or reduction in symptoms of TB symptoms after treatment initiation, poor implementation of CB-DOTS strategy, insufficient funding which prevents the healthcare system from initiating and conducting follow-ups for lost patients, and frequent stock-outs of TB drugs which frustrates people with TB from continuing with treatment. DTT is more likely in the continuation phase of TB treatment and when the treatment supporter is employed. To mitigate DTT, we recommend that healthcare providers should ensure children with TB and their treatment supporters are accorded privacy during service provision and provide more information about TB symptom resolution and treatment duration versus the need to complete treatment.
The district and national TB control programs should address gaps in funding to TB care, the supply of TB drugs, and the implementation of the CB-DOTS strategy.
Availability of data and materials
To protect participant’s anonymity, data will be shared at reasonable request. The contact person is: Stephen Okoboi: okoboi25@gmail.com. A statement to confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Abbreviations
- CB-DOTS:
-
Community-based Directly Observed Therapy Short course
- FB-DOTS:
-
Facility-based Directly Observed Therapy Short course
- DTT:
-
Discontinuation of tuberculosis treatment
References
Mandalakas AM, Kay AW, Bacha JM, Devezin T, Golin R, Simon KR, et al. Tuberculosis among children and adolescents at HIV treatment centers in sub-Saharan Africa. Emerg Infect Dis. 2020;26(12):2933–43.
World Health Organization. Global Tuberculosis Report 2020. Geneva: WHO; 2020. p. 1–2. 6–7
Dodd PJ, Yuen CM, Sismanidis C, Seddon JA, Jenkins HE. The global burden of tuberculosis mortality in children: a mathematical modelling study. Lancet Glob Health. 2017;5(9):e898–906. https://doi.org/10.1016/S2214-109X(17)30289-9.
Roadmap towards ending TB in children and adolescents. http://www.who.int/tb/publications/2018/tb-childhoodroadmap/en/. Accessed 23 Mar 2021.
Fry SH, Barnabas SL, Cotton MF. Tuberculosis and HIV-an update on the “cursed duet” in children. Front Pediatr. 2019;7:159. https://doi.org/10.3389/fped.2019.00159.
Tuberculosis profile: Uganda. https://worldhealthorg.shinyapps.io/tb_profiles/?_inputs_&entity_type=%22country%22&lan=%22EN%22&iso2=%22UG%22. Accessed 23 Mar 2021.
World Health Organization: Guidelines for treatment of drug-susceptible tuberculosis and patient care. 2017.
Babiarz KS, Suen SC, Goldhaber-Fiebert JD. Tuberculosis treatment discontinuation and symptom persistence: an observational study of Bihar, India's public care system covering >100,000,000 inhabitants. BMC Public Health. 2014;14(1):418. https://doi.org/10.1186/1471-2458-14-418.
Habteyes Hailu T, Azar T, Shojaeizadeh D, Garmaroudi G. Tuberculosis treatment non-adherence and lost to follow up among TB patients with or without HIV in developing countries: a systematic review. Iran J Public Health. 2015;44(1):1.
Wobudeya E, Jaganath D, Sekadde MP, Nsangi B, Haq H, Cattamanchi A. Outcomes of empiric treatment for pediatric tuberculosis, Kampala, Uganda, 2010–2015. BMC Public Health. 2019;19(1):1–6.
Kasozi S, Kirirabwa NS, Kimuli D, Luwaga H, Kizito E, Turyahabwe S, et al. Addressing the drug-resistant tuberculosis challenge through implementing a mixed model of care in Uganda. PLoS One. 2020;15(12):e0244451. https://doi.org/10.1371/journal.pone.0244451.
Best Practices in Child and Adolescent Tuberculosis Care. https://www.finddx.org/wp-content/uploads/2018/09/Best-Practices-Child-Adolescent-TB-Care.pdf. Accessed 23 Mar 2021.
Republic of Uganda. Uganda National Tuberculosis and Leprosy Control Program: Manual for management and control of Tuberculosis and Leprosy. 3rd ed. Kampala: Ministry of Health; 2017. p. 22–30.
Moser A, Korstjens I. Series: practical guidance to qualitative research. Part 3: sampling, data collection and analysis. Eur J Gen Pract. 2018;24(1):9–18. https://doi.org/10.1080/13814788.2017.1375091.
Lauritsen J. EpiData (version 3.1). A comprehensive tool for validated entry and documentation of data; 2004.
Mulogo EM, Nahabwe C, Bagenda F, Batwala V. Determinants of treatment completion among rural smear positive pulmonary tuberculosis patients: a cross-sectional survey conducted in South-Western Uganda. Infect Dis Poverty. 2017;6(1):104. https://doi.org/10.1186/s40249-017-0313-3.
Daniel OJ, Oladapo OT, Alausa OK. Default from tuberculosis treatment programme in Sagamu, Nigeria. Niger J Med. 2006;15(1):63–7. https://doi.org/10.4314/njm.v15i1.37119.
Izudi J, Tamwesigire IK, Bajunirwe F. Explaining the successes and failures of tuberculosis treatment programs; a tale of two regions in rural eastern Uganda. BMC Health Serv Res. 2019;19(1):979. https://doi.org/10.1186/s12913-019-4834-2.
Izudi J, Tamwesigire IK, Bajunirwe F. Treatment supporters and level of health facility influence completion of sputum smear monitoring among tuberculosis patients in rural Uganda: a mixed-methods study. Int J Infect Dis. 2020;91:149–55. https://doi.org/10.1016/j.ijid.2019.12.003.
World Health Organization: Everybody’s business--strengthening health systems to improve health outcomes: WHO’s framework for action. 2007.
Uplekar M, Weil D, Lonnroth K, Jaramillo E, Lienhardt C, Dias HM, et al. WHO’s new end TB strategy. Lancet. 2015;385(9979):1799–801. https://doi.org/10.1016/S0140-6736(15)60570-0.
Tweya H, Feldacker C, Estill J, Jahn A, Ng'ambi W, Ben-Smith A, et al. Are they really lost? “true” status and reasons for treatment discontinuation among HIV infected patients on antiretroviral therapy considered lost to follow up in urban Malawi. PLoS One. 2013;8(9):e75761. https://doi.org/10.1371/journal.pone.0075761.
Arshad A, Salam RA, Lassi ZS, Das JK, Naqvi I, Bhutta ZA. Community based interventions for the prevention and control of tuberculosis. Infect Dis Poverty. 2014;3(1):27. https://doi.org/10.1186/2049-9957-3-27.
Wright CM, Westerkamp L, Korver S, Dobler CC. Community-based directly observed therapy (DOT) versus clinic DOT for tuberculosis: a systematic review and meta-analysis of comparative effectiveness. BMC Infect Dis. 2015;15(1):210. https://doi.org/10.1186/s12879-015-0945-5.
Zhang H, Ehiri J, Yang H, Tang S, Li Y. Impact of community-based DOT on tuberculosis treatment outcomes: a systematic review and meta-analysis. PLoS One. 2016;11(2):e0147744. https://doi.org/10.1371/journal.pone.0147744.
Acknowledgments
We acknowledge Clarke International University Research Ethics Committee for the wonderful comments and the Research Assistants for their support in data collection.
Funding
None.
Author information
Authors and Affiliations
Contributions
LK and SO: Study conception and design. LK: Acquisition of data. JI: Analysis and interpretation of data. LK, JI, and SO: Drafting of manuscript. JI and SO: Critical revision. LK, JI, and SO: Final approval of manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics and consent to participate
This study was approved by Clarke International University Research Ethics Committee and was assigned the number CLARKE-2020-8. Written informed consent was obtained from all treatment supporters and health care workers that participated in the focus group discussions and key informant interview. Informed consent for secondary data was waived off by Clarke International University Research Ethics Committee (CLARKE-2020-8). No patient’s identifiers were collected during data abstraction. We confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kibirige, L., Izudi, J. & Okoboi, S. Discontinuation of tuberculosis treatment among children in the Kampala Capital City Authority health facilities: a mixed-methods study. BMC Infect Dis 21, 511 (2021). https://doi.org/10.1186/s12879-021-06244-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06244-y