Abstract
Background
Retention on lifelong antiretroviral therapy (ART) is essential in sustaining treatment success while preventing HIV drug resistance (HIVDR), especially in resource-limited settings (RLS). In an era of rising numbers of patients on ART, mastering patients in care is becoming more strategic for programmatic interventions. Due to lapses and uncertainty with the current WHO sampling approach in Cameroon, we thus aimed to ascertain the national performance of, and determinants in, retention on ART at 12 months.
Methods
Using a systematic random sampling, a survey was conducted in the ten regions (56 sites) of Cameroon, within the “reporting period” of October 2013–November 2014, enrolling 5005 eligible adults and children. Performance in retention on ART at 12 months was interpreted following the definition of HIVDR early warning indicator: excellent (>85%), fair (85–75%), poor (<75); and factors with p-value < 0.01 were considered statistically significant.
Results
Majority (74.4%) of patients were in urban settings, and 50.9% were managed in reference treatment centres. Nationwide, retention on ART at 12 months was 60.4% (2023/3349); only six sites and one region achieved acceptable performances. Retention performance varied in reference treatment centres (54.2%) vs. management units (66.8%), p < 0.0001; male (57.1%) vs. women (62.0%), p = 0.007; and with WHO clinical stage I (63.3%) vs. other stages (55.6%), p = 0.007; but neither for age (adults [60.3%] vs. children [58.8%], p = 0.730) nor for immune status (CD4351–500 [65.9%] vs. other CD4-staging [59.86%], p = 0.077).
Conclusions
Poor retention in care, within 12 months of ART initiation, urges active search for lost-to-follow-up targeting preferentially male and symptomatic patients, especially within reference ART clinics. Such sampling strategy could be further strengthened for informed ART monitoring and HIVDR prevention perspectives.
Similar content being viewed by others
Background
With a total of 145,038 adults and children receiving antiretroviral therapy (ART) out of 623,350 people living with HIV (PLHIV) in Cameroon, scalability of ART is a burning priority to the national AIDS programme [1, 2]. Of note, Cameroon recently adopted the 2013 World Health Organization (WHO) public health recommendations of the consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection, increasing eligibility of ART based on CD4 count (from the former threshold of ≤350 to ≤500 cells/mm3) and providing universal access to lifelong ART for HIV-infected children under five years and for HIV-infected pregnant women in the context of the prevention of mother-to-child transmission (PMTCT) of HIV (transitioning from Option-A to Option-B+) [3, 4]. These implications would lead to ~80% enrolment on ART among people diagnosed HIV positive, thus suggesting the need of innovative strategies for effective and successful programmatic ART uptakes [3, 5].
Ensuring a successful ART programme in this new therapeutic era requires evidence-based findings on programmatic, clinic and patient factors associated with national performance [5, 6]. Our experience in assessing these factors locally, using early warning indicators (EWI) of HIV drug resistance (HIVDR), consistently reveals pharmacy stock-outs and delayed pill pick-up as major factors favoring HIVDR emergence; while prescribing/dispensing practices remain appropriate, indicators of retention in care and lost to follow-up are fluctuating, making it challenging to design and implement reasonable public health interventions nationwide [7–9], especially with the changing paradigms in ART [5].
Retaining patients on lifelong ART, is an essential component in HIVDR prevention through adherence promotion, considerably improved the clinical and immunological outcomes [10, 11], reduced lost to follow-up and prolong the life expectancy of treated-patients [3]. As this indicator remains with uncertainty [7–9], it became crucial for the national AIDS programme to delineate the country performance in patient retention on ART as well as related determinants. Such investigation would provide a reliable representativeness of Cameroon’s capacity in retaining patients on ART and prompt real time corrective measures while transitioning to current treatment strategies [3, 4].
In a context of declining trends in HIVDR EWI, the number of HIV clinics with satisfactory performance in patient retention on ART dropped drastically (from 70 to 0%) in selected sites of our national ART programme [8]. Moreover, retention on ART varied significantly between urban and rural settings in Cameroon [9], thereby stressing the necessity of in-depth understanding of disparities surrounding this key indicator of patient adherence to ART program [5, 6].
In terms of programmatic perspectives, an accurate mastering of patients in care provide a better accountability and planning for ARV drug procurement, thereby reducing events of discontinuous drug supply as previously reported [7–9]. Of note, drug shortage suggests ART interruption, which is a direct indicator of suboptimal ARV adherence and higher risks of HIVDR emergence in a context where low-genetic barrier drugs (i.e. lamivudine [3TC], emtricitabine [FTC], nevirapine [NVP], efavirenz [EFV]) are widely used for patient management [3, 4]. Therefore, poor retention on ART automatically results in higher lost to follow-up and HIVDR emergence and subsequent transmission to newly infected people within the communities [4, 5].
To minimize lost to follow-up and its associated risks of HIVDR, the WHO recommends to evaluate “retention in care at 12 months of ART” as part of five simplified EWIs (on- time pill pick-up; retention in care at 12 months; pharmacy stock-outs; dispensing practices; and virological suppression) [4, 5, 9]. Following the WHO sampling strategy, we earlier evaluated EWIs on selected ART clinics based on predefined criteria [4–9]. Following the WHO methodology during previous assessments, we found it difficult to identify specific programmatic factors associated with performance of retention in care at 12 months of ART at clinic-, at regional-, or at national-levels [7–9].
We aimed to ascertain the national ART programme performance on retention in care at 12 months of ART and associated factors in Cameroon, for the implementation of an optimal strategy against preventable HIVDR and for a mastering of ARV needs in an era of national treatment uptakes.
Methods
Study design and target populations
A cohort-study was conducted from February 23 to 06 March 06, 2015 in all the ten regions of Cameroon, among PLHIV initiating ART in the “enrolment period” ranging from October 2013 to December 2013 and followed-up for 12 months (i.e. October 2014 to December 2014). Thus, study “reporting period” ranges from October 2013 to November 2014.
Sampling method
Following a systematic random sampling with unequal probability at two-levels, all ten regions were systematically included in the survey, followed by a random selection of reference treatment centres and HIV management units in each region. Main exclusion criteria were sites with non-significant number of patients (<30) initiating ART within the defined “enrolment period”, calculated using the following formula:
With n = required minimum sample size; t = Z value at a confidence interval of 95% (1.96); p = assumed rate of retention at 12 months of ART; and m = error rate marge at 1% (0.01).
Overall, 56 sites were enrolled and their characteristics described: regional location, geographic settings (urban versus rural), and level of HIV clinic (reference treatment centre versus HIV management unit). In each selected site, patients initiating ART during the “enrolment period” were consecutively included until complete sampling for the study (for a total of 5005 in number).
Data collection
Data were abstracted from ART registers, medical files and pharmacy registers used to monitor patients at the respective ART clinic, and entered into EWI 2 abstraction tool as previously described [9]. Incoherent data were resolved by retrieving additional record documents available at the clinic.
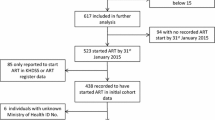
Quality assurance and data validation
To ensure reliability in collected data, only staff (statistician and experienced personnel) trained on HIV data management participated in the data abstraction process. Supervisors were Public Health experts from the central level with field experience on the collection and reporting of data in the ART programme. After on-site validation (mainly for data readability and completeness) on 5005 patient files, abstracted data were centralised at the national level, whereby a second validation (mainly for verifying data consistency) was conducted through a double electronic data-entry; leading to 66.91% inclusion in the final dataset (Fig. 1).
Data analysis
Interpretation of data was performed according to the definition of EWI 2 as described in Table 1. Chi Square test was used in assessing statistical associations, with p-value <0.01 considered significant.
Availability of data and materials
The data supporting the findings are provided in the main paper and in additional supporting files uploaded as supplement contents with this manuscript.
Results
Socio-demographic characteristics of the study population
Of all 3349 PLHIV in the validated dataset from the 56 study sites, distribution according to geographic settings showed that 2491 (74.4%) and 858 (25.6%) were respectively in the urban and rural settings. According to level of HIV clinic, 50.9% were enrolled in a reference treatment centre; while for regional distribution, the Centre, Northwest, Littoral, and Southwest regions were highly represented (17.2, 14.8, 13.8, and 12.3% respectively), as shown in supplemental digital content (Additional file 1: SDC 1).
Out of 3256 PLHIV initiating ART whose gender and age were recorded in the 56 study sites, 2201 (67.6%) were female (gender ratio: two women for one man, p < 0.0001); mean age was 36.1 years (+/− 12.2), min-max: 0.16 – 74; and only 4.2% were children or adolescents aged <15 years (Additional file 1: SDC 2).
Clinical characteristics of the study population
Of the 2163 patients with available clinical classification at ART initiation, 1279 (59.1%) were at the WHO clinical stage III, with 60.0 and 58.7% respectively in the male and female populations.
Of the 2621 patients with available CD4 recorded at ART initiation, a median of 223 CD4 cells/mm3 [IQR: 52; 384] was recorded, and the majority (86.5%) had ≤ 350 CD4 cells/mm3, while <5% had a CD4 count >500 cells/mm3.
All 3349 patients had their initial ART regimens recorded, and predominant regimens were tenofovir (TDF)/3TC/EFV (44%) and zidovudine (AZT)/3TC/NVP (31.6%), as detailed in Table 2.
Performance in retention on ART
Retention according to geographic settings
Globally, the national level of retention in care 12 months after ART initiation was 60.4% (2023/3349), indicating an overall poor performance in patient retention shortly after ART initiation, with a significantly lower performance in urban (58.5%) compared to rural (66.0%) settings, p < 0,0001.
According to regions, retention capacity varied considerably, with the highest performance reported in the Littoral Region (75.1%), followed by the East, Centre and Adamawa regions (70.2, 64.8, and 63.4% respectively). Thus, no region in the country had an excellent/desirable performance, and only one region (Littoral) had a fair performance, while the West and Far-North regions that registered the poorest performances (42.8 and 47.4% respectively), as shown in Table 3.
Retention according to HIV clinic levels
According to clinic levels, reference treatment centres had an overall performance of 54.2% against 66.8% in HIV management units, indicating paradoxically a better capacity of low-level clinics in retaining patients on ART. Of note, the HIV management unit with the highest performance had 93.1% (in the East region) while the reference treatment centre with the highest performance had 83.5% (in the Littoral region), indicating respectively an excellent and a fair capacity for retention on ART (Additional file 1: SDC 3).
Factors associated with levels of retention on ART after 12 months
Association between demographic profile and retention on ART
The overall gender distribution at 12 months after ART initiation revealed that 62.0% (1405) women compared to 57.1% (618) men were still in care, indicating a significantly better adherence of women to the national ART program, p = 0.007. Similar trends were observed when comparing retention in care between women (68.3%) and men (63.6%) followed-up in HIV management units (p = 0.057), as well as in reference treatment centres (55.8% versus 50.9% respectively), p = 0.018.
According to age groups, paediatrics (children and adolescents < 15 years) had similar retention rates compared to older patients (58.8 and 60.3%, respectively, p = 0.730); with a slightly lower performance observed among children aged 5–9 years (47.2% versus 63% for other children age, p = 0.099), as shown in Table 4.
Association between clinical characteristics and retention on ART
Clinical analysis revealed that 12 months retention on ART seems decreasing from WHO clinical stage I to IV, with the highest performance (63.3%) reported among patients with at WHO clinical stage I while the poorest (55.4%) was among ones at WHO clinical stage IV, p = 0.007. With a median of 223 CD4 cells/mm3, we observed a slightly higher retention on ART at 12 months for patients who started treatment with 351–500 cells/mm3 (65.9%) compared to other categories (59.86% for ones with = <350 CD4 cells/mm3 and with >500 CD4 cells/mm3, p = 0.077). Overall, clinical parameters showed low rates of retention (below performance limit of 75%), thus indicating higher risk of HIVDR emergence (Table 5). However, retention performance at all clinical parameters was significantly greater in HIV management units compared to reference treatment centres (66.8% versus 54.2%, respectively); p < 0.0001.
Classification levels of retention on ART by health facilities
Overall, only six out of 56 (10.71%) health facilities had acceptable performance for retention on ART at 12 months, among which 5.36% (3/56) with excellent (>85%) performance (Ngaoundéré Presbyterian Hospital [93.1%], CBC of Mboppi [89.5%], PR Garoua Boulai [88%]), and 5.36% (3/56) with fair (75–85%) performance (HD Pette [83.9%], Douala Laquintinie Hospital [83.5%], and DH Mamfe [81.3%]), which were mostly HIV management units from diverse regions in Cameroon. Poorest performances were observed from an HIV management unit (NKAMBE DH [6.2%]) and a reference treatment centre (Yaoundé General Hospital [18.9%]). Thus, 89.29% of health facilities had a poor (<75%) performance in retention on ART at 12 months; indicating an overall high risk of HIVDR emergence in these ART clinics.
Discussion
As an indicator of potential loss to follow-up in ART programs and a tool for estimates in ARV procurement and supply, patient retention in care also serves in tailoring adherence support towards a better control of preventable HIVDR [5, 6]. As compared to previous studies in Cameroon [7–9], our findings provide a prime estimate of the country capacity both in enrolling and in retaining patients on care 12 months after ART initiation. Importantly, the random sampling, across 56 ART clinics from all 10 regions of Cameroon, is innovative as it generates more meaningful evidence-based interventions, compared to the WHO primary sampling strategy [5, 6].
From this random sampling, only 60% of patients were still in care at 12 months after ART initiation, resulting in a poor national performance (i.e. <75%) for patient retention on ART, translated into 40% potential lost to follow-up [12]. As loss to follow-up are known as possible HIVDR, national ART programs in SA has ~40% likelihood of experiencing HIVDR emergence in a short-medium run [10, 11]. Of note, only 10.71% ART clinics and only one region (Littoral) had acceptable performances (excellent or fair), suggesting that ~90% of ART clinics as well as 90% of regions are experiencing high risks of HIVDR due to poor retention on ART, similar to findings from other SSA-settings [13]. The high performance observed in a reference centre of the Littoral is likely due to ongoing project that provides additional support for patient monitoring onsite, thus fostering adherence to care, as earlier addressed [9]. Compared to recently conducted EWI survey, performance was lower (10.71% versus 76.92%), and worse in urban settings [9]; a disparity likely attributed to the random sampling that gives broaden and in-depth appraisals of program functioning at all levels. Retention was also significantly lower (p < 0.0001) in HIV reference treatment centres than in management units. This outcome could be partly attributed to the burnout syndrome (heavy workload) which appears higher in reference treatment centres as we earlier reported within this national context (74.4% patients versus 25.6% in management units), calculated per site based on the number of trained physicians, nurses, pharmacists/clerks, biologists/laboratory technicians, counsellors, data managers, community relay agents involved on the routine management of PLHIV [8]. Advanced implementation of task shifting and decentralisation might help alleviating the burnout syndrome [8, 13–15]. Retention at 12 months of ART was also problematic in African countries and beyond, supporting the needs to explore other local factors (geographical landscape around a single ART clinic, availability of transportation facilities, effectiveness of decentralisation, etc.) that may be warrant public health actions [12–19].
Our study delineates additional reasons underscoring this poor national retention on ART. Of note, poor retention was more concerning in men (p = 0.007), thus requiring intensified adherence support to men on ART following their daily realities and challenges [18]. As previously reported, African women are generally known to be more adherent to ART programs [20, 21]; this might also be attributed to attention offered to women through the PMTCT program and cascade of health care for mother and child (an information not captured in our dataset), and the eventual non-adherence of male patients [22]. Due to the limited representativeness of children (<15 years), retention on ART according to age merits further investigations, with linkage to virological suppression according to age groups [21, 23].
The significant risk (p = 0.007) of poor retention on ART among potential symptomatic patients (i.e. 55.6% WHO clinical stages I/II/III:) versus potential healthy/asymptomatic patients (i.e. 59.1% WHO clinical stage I) indicates the need to implement an active monitoring/tracking system for patients suffering of any disease at ART initiation, as well as social and financial barriers [21, 23]. This underscores that early ART initiation would promote retention on ART [21]. Moreover, median CD4 (223 cells/mm3) indicates an overall delay initiation of ART (though better than previous reports: 123 and 163 CD4 cells/mm3) [12, 24], which in turns predict poor outcomes both in retention and in clinical benefits [21, 25]. Despite no significance between CD4 range and retention levels (p = 0.077), severely immune compromised patients would likely default from care due to clinical manifestations [23, 26], thus implying policies for timely ART initiation as we transition to ≤500 CD4 cells/mm3 for initiation [3, 4, 19].
Decreasing retention was observed with periods of ART initiation (October-December, p <0.02), suggesting further understanding of related temporal barriers on defaulters or lost to follow-up [24], especially in the frame of the current “90-90-90” goals in RLS [27]. Thus, innovative approaches (community-based test-and-treat, mobile clinics, use of SMS for recalls, adherence clubs, and point-of-care monitoring) are highly necessary to curve the epidemic, especially within SSA settings [27–33].
Study strengths
Including 56 ART clinics, in all the ten national regions, gives room for greater country representativeness (compared to previous studies [7–9]), further strengthened by random sampling at regional level. Findings would directly contribute for planning, monitoring and evaluation of national ART program, and for policy-implementation in other RLS with similar challenges [5, 6].
Study limitations
Data rejection (~33%) weakens our expected study strengths, thus indicating needs for continuous training on data reporting in the continuum of ART programs within such RLS. Rural settings were limited, suggesting a two-level systematic sampling, followed by randomisation only within unique geographical strata (urban vs. rural; reference centre vs. management units, etc.) [33]. Study-period (1-year) was a limited to assess retention rates according to different ART-regimens, thus requiring long-term cohort-studies while transitioning towards new ART recommendations [4]. Predictors of delayed ART initiation, and other aspects of adherence to ART (on-time drug pickup, pill count, self-reported adherence, and/or drug dosage) should be covered subsequently, for optimal policies.
Context-specific programmatic lessons
Despite the high capacity of the national AIDS program in enrolling patients on ART, poor performance in retaining these patients in care is a serious treat for ART effectiveness and coverage. Interestingly, results predict a better life expectancy for women over men, who appear less likely than women to seek and adhere to ART [22]. On a separate note, active search for patients out of care is mandatory, including community engagement, to sustain ART cohorts and routine drug procurement. Accelerating task shifting and decentralisation would alleviate the tentative heavy workload. Therefore, in routine practice, follow-up/adherence support should mainly target male and symptomatic patients initiating ART nationwide. Programmatic assessments may integrate quality of care indicators [34], affordable monitoring assays [35–37], and simplified/cost-effective ARV drug provision strategies [38, 39] for the national ART performance, in a context of increasing risks of HIVDR [40–42].
Conclusions
One year after ART initiation in Cameroonian clinical settings, retention in care remains below acceptable standards, suggesting risks of HIVDR emergence nationwide. Adherence interventions should focus primarily on male and symptomatic patients, especially within reference ART clinics. Such systematic-random sampling strategy should be further strengthened, in the frame of the global perspectives for HIVDR prevention in RLS.
Abbreviations
- 3TC:
-
Lamivudine
- ART:
-
Antiretroviral therapy
- ARV:
-
Antiretroviral
- AZT:
-
Zidovudine
- EFV:
-
Efavirenz
- EWI:
-
Early warning indicators
- FTC:
-
Emtricitabine
- HIV:
-
Human immunodeficiency virus
- HIVDR:
-
HIV drug resistance
- NVP:
-
Nevirapine
- PLHIV:
-
People living with HIV
- PMTCT:
-
Prevention of mother-to-child transmission
- TDF:
-
Tenofovir
- WHO:
-
World Health Organization
References
Joint United Nations Programme on HIV/AIDS. The Gap report. Geneva: UNAIDS; 2014. [cited 2015 Jun 15]. Available from: http://www.unaids.org/en/resources/campaigns/2014gapreport.
National AIDS Control Committee (NACC). Global Aids Response Progress (GARP). Yaoundé: NACC; 2014. [cited 2015 Jun 15]. Available from: http://www.unaids.org/sites/default/files/country/documents/CMR_narrative_report_2014.pdf.
World Health Organisation. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. Geneva: World Health Organisation; 2013. [cited 2015 Jun 15]. Available from: http://www.who.int/hiv/pub/guidelines/arv2013/en/.
République du Cameroun, Ministère de la Santé Publique. Directives nationales de prévention et de prise en charge du VIH au Cameroun. Yaoundé: Ministry of Public Health; 2014. [cited 2015 Jun 15].
World Health Organisation. HIV drug resistance report 2012. Geneva: World Health Organisation; 2012. [cited 2015 Jun 15]. Available from: http://www.who.int/hiv/pub/drugresistance/report2012/en/.
World Health Organization. Report of the Early Warning Indicator Advisory Panel Meeting. Meeting Report on Assessment of World Health Organization HIV Drug Resistance Early Warning Indicators. Geneva: World Health Organisation; 2014. [cited 2015 Jun 15]. Available from: http://www.who.int/hiv/pub/meetingreports/ewi_meeting_report/en/.
Billong SC, Fokam J, Nkwescheu AS, et al. Early warning indicators for HIV drug resistance in Cameroon during the year 2010. PLoS ONE. 2012;7(5):e36777. doi:10.1371/journal.pone.0036777.
Fokam J, Billong SC, Bissek ZKA, et al. Declining trends in early warning indicators for HIV drug resistance in Cameroon from 2008 to 2010: lessons and challenges for low-resource settings. BMC Public Health. 2013;8(13):308. doi:10.1186/1471-2458-13-308.
Fokam J, Elat JB, Billong SC, et al. Monitoring HIV drug resistance early warning indicators in Cameroon: a study following the revised world health organization recommendations. PLoS ONE. 2015;10(6):e0129210. doi:10.1371/journal.pone.0129210.
Focà E, Odolini S, Sulis G, et al. Clinical and immunological outcomes according to adherence to first-line HAART in a urban and rural cohort of HIV-infected patients in Burkina Faso, West Africa. BMC Infect Dis. 2014;14:153. doi:10.1186/1471-2334-14-153.
Kiwuwa-Muyingo S, Walker AS, Oja H, et al. The impact of first year adherence to antiretroviral therapy on long-term clinical and immunological outcomes in the DART trial in Uganda and Zimbabwe. Trop Med Int Health. 2012;17(5):584–94. doi:10.1111/j.1365-3156.2012.02974.x.
Billong SC, Fokam J, Aghokeng AF, et al. Population-based monitoring of emerging HIV-1 drug resistance on antiretroviral therapy and associated factors in a sentinel site in Cameroon: low levels of resistance but poor programmatic performance. PLoS ONE. 2013;8(8):e72680. doi:10.1371/journal.pone.0072680. eCollection 2013.
Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: a systematic review. PLoS Med. 2007;4(10):e298.
Suzan-Monti M, Blanche J, Boyer S, et al. Benefits of task-shifting HIV care to nurses in terms of health-related quality of life in patients initiating antiretroviral therapy in rural district hospitals in Cameroon [Stratall Agence Nationale de Recherche sur le SIDA (ANRS) 12110/Ensemble pour une Solidarité Thérapeutique Hospitalière en Réseau (ESTHER) substudy]. HIV Med. 2015;16(5):307–18. doi:10.1111/hiv.12213.
Rasson S, Boyer S, Fugon L, et al. Decentralization of access to antiretroviral therapy in Cameroon: correlates of HIV physicians’ knowledge in HIV care. Antivir Ther. 2011;16(3):423–8. doi:10.3851/IMP1773.
Bennett DE, Jordan MR, Bertagnolio S, et al. HIV drug resistance early warning indicators in cohorts of individuals starting antiretroviral therapy between 2004 and 2009: World Health Organization global report from 50 countries. Clin Infect Dis. 2012;54–4:S280–9.
Sigaloff KC, Hamers RL, Menke J, et al. Early warning indicators for population-based monitoring of HIV drug resistance in 6 African countries. Clin Infect Dis. 2012;54(4):S294–9.
Hall HI, Gray KM, Tang T, Li J, Shouse L, Mermin J. Retention in care of adults and adolescents living with HIV in 13 U.S. areas. J Acquir Immune Defic Syndr. 2012;60(1):77–82. doi:10.1097/QAI.0b013e318249fe90.
Fleishman JA, Yehia BR, Moore RD, Korthuis PT, Gebo KA, HIV Research Network. Establishment, retention, and loss to follow-up in outpatient HIV care. J Acquir Immune Defic Syndr. 2012;60(3):249–59. doi:10.1097/QAI.0b013e318258c696.
Boullé C, Kouanfack C, Laborde-Balen G, et al. Gender differences in adherence and response to antiretroviral treatment in the stratall trial in rural district hospitals in Cameroon. J Acquir Immune Defic Syndr. 2015;69(3):355–64. doi:10.1097/QAI.0000000000000604.
Koole O, Tsui S, Wabwire-Mangen F, et al. Retention and risk factors for attrition among adults in antiretroviral treatment programmes in Tanzania, Uganda and Zambia. Trop Med Int Health. 2014;19(12):1397–410. doi:10.1111/tmi.12386.
Bor J, Rosen S, Chimbindi N, et al. Mass HIV treatment and Sex disparities in life expectancy: demographic surveillance in rural South Africa. PLoS Med. 2015;12(11):e1001905. discussion e1001905. doi: 10.1371/journal.pmed.1001905. eCollection 2015 Nov.
Yehia BR, Rebeiro P, Althoff KN, et al. Impact of age on retention in care and viral suppression. J Acquir Immune Defic Syndr. 2015;68(4):413–9. doi:10.1097/QAI.0000000000000489.
Yehia BR, Stewart L, Momplaisir F, et al. Barriers and facilitators to patient retention in HIV care. BMC Infect Dis. 2015;15:246. doi:10.1186/s12879-015-0990-0.
Ndawinz JD, Anglaret X, Delaporte E, et al. New indicators for delay in initiation of antiretroviral treatment: estimates for Cameroon. Bull World Health Organ. 2015;93(8):521–8.
Yehia BR, French B, Fleishman JA, et al. Retention in care is more strongly associated with viral suppression in HIV-infected patients with lower versus higher CD4 counts. J Acquir Immune Defic Syndr. 2014;65(3):333–9. doi:10.1097/QAI.0000000000000023.
Joint United Nations Programme on HIV/AIDS. An ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS; 2014. [cited 2015 Oct 15]. Available from: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf.
Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS care panel. Ann Intern Med. 2012;156(11):817–294. doi:10.7326/0003-4819-156-11-201206050-00419.
Christopoulos KA, Riley ED, Tulsky J, et al. A text messaging intervention to improve retention in care and virologic suppression in a U.S. urban safety-net HIV clinic: study protocol for the Connect4Care (C4C) randomized controlled trial. BMC Infect Dis. 2014;14:718. doi:10.1186/s12879-014-0718-6.
Elul B, Lahuerta M, Abacassamo F, et al. A combination strategy for enhancing linkage to and retention in HIV care among adults newly diagnosed with HIV in Mozambique: study protocol for a site-randomized implementation science study. BMC Infect Dis. 2014;14:549. doi:10.1186/s12879-014-0549-5.
Nabukeera-Barungi N, Elyanu P, Asire B, et al. Adherence to antiretroviral therapy and retention in care for adolescents living with HIV from 10 districts in Uganda. BMC Infect Dis. 2015;15:520. doi:10.1186/s12879-015-1265-5.
Holtzman CW, Kathleen A, et al. Retention in care and medication adherence: current challenges to antiretroviral therapy success. Drugs. 2015;75(5):445–54. doi:10.1007/s40265-015-0373-2.
Unge C, Södergård B, Marrone G, et al. Long-term adherence to antiretroviral treatment and program drop-out in a high-risk urban setting in sub-Saharan Africa: a prospective cohort study. PLoS ONE. 2010;5(10):e13613. doi:10.1371/journal.pone.0013613.
Johnston S, Kendall C, Hogel M, McLaren M, Liddy C. Measures of quality of care for people with HIV: a scoping review of performance indicators for primary care. PLoS ONE. 2015;10(9):e0136757. doi:10.1371/journal.pone.0136757. eCollection 2015.
Sigaloff KC, de Wit TF. ART in sub-Saharan Africa: the value of viral load monitoring. Lancet HIV. 2015;2(7):e261–2. doi:10.1016/S2352-3018(15)00109-5.
Nanfack AJ, Agyingi L, Noubiap JJ, Ngai JN, Colizzi V, Nyambi PN. Use of amplification refractory mutation system PCR assay as a simple and effective tool to detect HIV-1 drug resistance mutations. J Clin Microbiol. 2015;53(5):1662–71. doi:10.1128/JCM.00114-15.
Fokam J, Salpini R, Santoro MM, et al. Performance evaluation of an in-house human immunodeficiency virus type-1 protease-reverse transcriptase genotyping assay in Cameroon. Arch Virol. 2011;156(7):1235–43. doi:10.1007/s00705-011-0982-3.
Orrell C, Dipenaar R, Killa N, Tassie JM, Harries AD, Wood R. Simplifying HIV cohort monitoring--pharmacy stock records minimize resources necessary to determine retention in care. J Acquir Immune Defic Syndr. 2013;62(3):e106–8.
Shrestha RK, Gardner L, Marks G, et al. Estimating the cost of increasing retention in care for HIV-infected patients: results of the CDC/HRSA retention in care trial. J Acquir Immune Defic Syndr. 2015;68(3):345–50. doi:10.1097/QAI.0000000000000462.
Aghokeng AF, Kouanfack C, Laurent C, et al. Scale-up of antiretroviral treatment in sub-Saharan Africa is accompanied by increasing HIV-1 drug resistance mutations in drug-naive patients. AIDS. 2011;25(17):2183–8. doi:10.1097/QAD.0b013e32834bbbe9.
Fokam J, Salpini R, Santoro MM, et al. Drug resistance among drug-naive and first-line antiretroviral treatment-failing children in Cameroon. Pediatr Infect Dis J. 2011;30(12):1062–8. doi:10.1097/INF.0b013e31822db54c.
Aghokeng AF, Kouanfack C, Eymard-Duvernay S, et al. Virological outcome and patterns of HIV-1 drug resistance in patients with 36 months’ antiretroviral therapy experience in Cameroon. J Int AIDS Soc. 2013;16:18004. doi:10.7448/IAS.16.1.18004.
Acknowledgements
We thank the staff (Public Health experts, Epidemiologists, Biostatisticians, Monitoring and Evaluation experts, data managers, and data clerks) of the central and regional working group of the National AIDS Control Committee (CNLS) in Cameroon, for their technical assistance in the field collection, statistical analysis and review of the manuscript.
Funding
The National AIDS Control Committee (CNLS) in Cameroon conducted this study, through funding allocated by the Global Fund to Fight AIDS, Tuberculosis and Malaria, for monitoring and evaluation of HIV/AIDS programmatic activities.
Availability of data and materials
The datasets generated during the current study are not publicly available, as these constitute part of the country database of the National AIDS Control Committee in Cameroon. However, the datasets are available on reasonable request from the corresponding author.
Authors’ contributions
Conceived and designed the study: SCB, JF, DKS, ACZKB, JBEN; Acquired and analyzed the data: CIP, SA, DKS; Interpreted the data: SCB, JF, VC, AN, EB, CIP; Drafted the manuscript: SCB, JF, DKS, CIP; Revised the manuscript: ACZKB, JBEN, VC, AN, EB; Approved the final version of the manuscript: All authors (SCB, JF, CIP, SA, DKS, EB, VC, AN, ACZKB, JBEN). Agreed to be accountable for all aspects of the work related to the accuracy or integrity: All authors (SCB, JF, CIP, SA, DKS, EB, VC, AN, ACZKB, JBEN).
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was institutionally approved by the Cameroon Ministry of Public Health (N°1915/2014/NS/MINSANTE/CAB/STBP/CNLS/GTC/SP/SPSE/sa), with a waiver of informed consent as per the retrospective design of the investigation and its considerations as a national activity of the planning, monitoring and evaluation of the ART program under the National AIDS Control Committee (CNLS), in Cameroon.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
SDC 1. Distribution of the study population by geographic settings, by level of HIV clinic, and by region. Geographical setting is reported as rural or urban; level of HIV clinic is reported as reference treatment centres or HIV management units; regions represent all ten geographical regions of Cameroon. All data are reported for male, female and the overall population. SDC 2. Distribution of study population by gender and by age. Data are represented in age range of five years; an aggregated data for adults versus children is also provided. All data are reported for male, female and the overall population. SDC 3. Retention on ART by level of HIV clinic. Retention in care is provided for reference treatment centres and for HIV management units, reported for each region and for the overall geographical regions of Cameroon. (DOCX 111 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Billong, S.C., Fokam, J., Penda, C.I. et al. Predictors of poor retention on antiretroviral therapy as a major HIV drug resistance early warning indicator in Cameroon: results from a nationwide systematic random sampling. BMC Infect Dis 16, 678 (2016). https://doi.org/10.1186/s12879-016-1991-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-1991-3