Abstract
Purpose
The aim of this study was to describe a population of very old people with heart failure (HF), to analyse the use of cardiovascular drugs over time, and to explore factors influencing cardiovascular drug treatment for this group.
Methods
All participants with information regarding HF diagnosis were selected from the Umeå 85+/Gerontological Regional Database (GERDA). The people in GERDA are all ≥85 years old. Trained investigators performed structured interviews and assessments. Information regarding medications and diagnoses was obtained from the participants and from medical records. Medical diagnoses were reviewed and confirmed by an experienced geriatrician.
Results
In this very old population, the prevalence of HF was 29.6% among women and 30.7% among men. Between 2000 and 2017, there was an increase in the use of renin-angiotensin (RAS) inhibitors (odds ratio [OR] 1.107, 95% confidence interval [CI] 1.072–1.144) and beta-blockers (BBs) (OR 1.123, 95% CI 1.086–1.161) among persons with HF, whereas the prevalence of loop diuretics (OR 0.899, 95% CI 0.868–0.931) and digitalis (OR 0.864, 95% CI 0.828–0.901) decreased (p < 0.001 for all drug classes). Higher age was associated with lower use of RAS inhibitors and BBs.
Conclusion
In this HF population, the use of evidence-based medications for HF increased over time. This may be a sign of better awareness among prescribers regarding the under-prescribing of guidelines-recommended treatment to old people. Higher age associated with a lower prevalence of RAS inhibitors and BBs. This might indicate that further improvement is possible but could also represent a more cautious prescribing among frail very old individuals.
Similar content being viewed by others
Introduction
Heart failure (HF) has been reported to affect about 1–2% of the population [1]. The condition is associated with high morbidity and mortality. Its prevalence increases with age, and it is a leading cause of hospitalisation among old people [2,3,4,5]. Old people have been poorly represented in randomised controlled trials (RCTs) for the management of HF, and even though there are some uncertainties regarding the effect of these treatments in the older population, the guidelines still apply to old people [6]. However, several studies have found that very old people are less likely to receive evidence-based treatment for HF [7,8,9,10,11,12,13].
Since their first publication, the European Society of Cardiology (ESC) guidelines have always recommended the use of renin-angiotensin (RAS) inhibitors and beta-blockers (BBs) for all patients with HF with reduced ejection fraction (HFrEF) and New York Heart Association (NYHA) class II–IV disease, as these drugs are known to reduce mortality and morbidity [1, 14,15,16,17,18,19]. Mineralocorticoid receptor antagonists (MRAs) have been recommended for NYHA class III–IV since the 1997 version of the guidelines [14], and for NYHA class II since the 2012 version [18]. The evidence for the same outcomes is weaker for loop diuretics. Loop diuretics have always been recommended to treat congestive symptoms, with the advice that the drug should be reduced to the lowest effective dose and, if possible, discontinued. Digitalis has also had a place in all HF guidelines as an additional option in patients with remaining symptoms [1, 14,15,16,17,18,19]. In addition to reducing mortality and hospital admission, adequate HF treatment may lead to relief of symptoms and improved quality of life [20].
Most previous studies describing very old people with HF and their drug treatment have been based on HF registries, while less has been published regarding real-life populations [13, 21, 22]. Due to the reported problems in implementing evidence-based treatment among old people with HF [23, 24], and because the majority of articles describing lower use of guideline-recommended treatment among old people are cross-sectional studies with data from only one time point [7, 8, 10, 11], we were interested in investigating time trends in drug use in a very old real-life population to see if the use of evidence-based therapy has changed over time.
Aim
The aim of this study was to describe a population of very old people with HF, to analyse the use of cardiovascular drugs over time, and to explore factors influencing cardiovascular drug treatment for this group.
Method
Setting and participants
The data in this study were derived from the Umeå 85+/Gerontological Regional Database (GERDA), which started with the objective of investigating the general health and living conditions of very old people in northern Sweden. The database was initiated in the year 2000, and data collection was conducted every five years. This study used cross-sectional data from the database collected at four different time points: 2000–2002 (T1), 2005–2007 (T2), 2010–2012 (T3), and 2015–2017 (T4). Potential participants were identified by using the population register from the Swedish Tax Agency.
Every second 85-year-old and all individuals aged 90 and ≥95 years living in one urban or five selected rural municipalities were invited to participate. An information letter was sent to those selected, and they were contacted via telephone one week later. Informed consent was obtained from all included participants. If the individual was not personally able to give consent, for example due to substantial cognitive impairment, a close person/relative was also consulted about participation. This approach made it possible to include people living at home as well as in nursing homes, and people with and without cognitive impairment. Participants could be included at multiple time points, and were then considered unique cases for each time point. The Umeå 85+/GERDA study is described in greater detail in previous publications [25,26,27]. For this study, all participants with information regarding HF diagnosis were selected. In total, 2186 of the 2814 invited individuals were included, giving a participation rate of 77.7%.
Procedure
Trained investigators conducted structured interviews with the participants during home visits. Physical tests were performed in addition to filling out questionnaires and assessment scales. The investigator was a medical doctor, medical student, nurse, or physiotherapist. For individuals with cognitive decline or living in nursing homes, the interviews were also held with partners, relatives, or staff.
Data regarding diagnoses, medical conditions, current drug use, and drug prescriptions were collected from the respondents and from medical records. The information on current drug use reported by the respondents was crosschecked with medical records. Information regarding doses and use of pro re nata medication was not available. An experienced geriatrician reviewed and confirmed all medical diagnoses by using all available data, including medical record data and assessments from the current study. Diagnoses of HF, stroke, hypertension, atrial fibrillation, transient ischemic attack (TIA), diabetes, myocardial infarction and angina pectoris were set according to ICD-10, while dementia disorders and depressive disorders were diagnosed according to DSM-IV-TR criteria.
Assessment scales
To assess dependency in personal activities of daily living (ADL), Barthel’s ADL index was used. The scale runs from 0 to 20, with lower scores indicating more dependence in ADL [28].
The Mini Mental State Examination (MMSE), with total scores of 0–30, was used to assess cognition. Higher scores indicate better cognitive function. Scores < 24 indicate cognitive impairment [29].
Nutritional status was assessed using the Mini Nutritional Assessment (MNA). Higher scores on a scale of 0–30 indicate better nutritional status [30].
Depressive symptoms were assessed using the 15-item version of the Geriatric Depression Scale (GDS-15). Total score ranges from 0 to 15, with higher scores indicating more depressive symptoms [31].
The Philadelphia Geriatric Centre Morale Scale (PGCMS) was used to assess the perceived morale dimension of quality of life. On the 17-point scale, higher scores indicate higher morale [32]. After a review by the British Geriatric Society of several quality of life assessment scales, the PGCMS scale was recommended to measure subjective well-being among old people [33].
The first question (“In general, how would you say your health is?”) of the 36-item Short Form Health Survey (SF-36) was used to assess self-rated health. The answers were given on a five-point Likert-type scale: 1 = excellent, 2 = very good, 3 = good, 4 = fair, and 5 = poor [34].
Statistics
To compare the groups with and without HF, Pearson’s chi-square test was used for dichotomous variables and t-test was used for continuous variables. Descriptive statistics were used to present the prevalence of drug use for T1–T4.
Within the group with HF, the use of selected drug classes at T1–T4 was compared. The World Health Organization Anatomical Therapeutic Chemical Index classification system was used to group the drugs. A multiple logistic regression model was conducted to evaluate time trends in drug use and to control for demographic differences between the samples, with drug class as dependent variable and year of data collection, age, and sex as independent variables. Drug classes included in the analyses were digitalis glycosides (C01A), loop diuretics (C03C), MRAs and other potassium-sparing agents (C03D) (referred to as MRAs throughout this article), BBs (C07), and RAS inhibitors (C09). Multiple logistic regression models were also used to investigate temporal trends in the use of these drug classes within the age groups 85, 90, and ≥95 years. Drug class was the dependent variable, and the year of data collection and sex were included as independent variables for all age groups. For the oldest group (≥95 years), age was also included as an independent variable to adjust for age differences.
To explore if different factors had an impact on drug use over time, another multiple logistic regression model was constructed. In this model, drug class was again the dependent variable, and year of data collection, age, sex, living in a nursing home, MMSE, Barthel’s ADL index, diabetes, hypertension, atrial fibrillation, depressive disorder, stroke and/or TIA, and ischemic heart disease (IHD) were included as independent variables. The diagnoses of stroke and TIA were summarised into one variable, and myocardial heart infarction and angina pectoris were also merged into one variable (IHD). This was done because treatment guidelines for the diagnoses in these groups are very similar.
Version 28 of the SPSS Statistics software package was used for data handling, analysis, and statistical calculations. A p-value of < 0.05 was considered statistically significant.
Results
The basic characteristics of the study population, assessments, and prevalence of certain diagnoses are presented in Table 1. The three age groups (85, 90, and > 95 years) included 782, 782, and 622 individuals, respectively. Of the total 2186 persons, 654 (29.9%) had HF. The prevalence of HF was 29.6% for women and 30.7% for men, and increased with higher age group (p < 0.001). A higher proportion of persons with HF lived in a nursing home (p < 0.001) compared to the group who did not have HF. In comparison to those without HF, persons with HF showed lower scores on the assessments of ADL (p < 0.001), MNA (p < 0.001), and PGCMS (p < 0.001), and higher scores on GDS (p < 0.001) and SF-36 self-rated health (p < 0.001). The diagnoses stroke (p = 0.003), atrial fibrillation (p < 0.001), diabetes (p < 0.001), myocardial infarction (p < 0.001), angina pectoris (p < 0.001), major neurocognitive disorder (NCD) (dementia according to DSM-IV-TR) (p = 0.016), and depressive disorder (p < 0.001) were more common in the HF group.
A description of the heart failure population regarding basic characteristics, assessments and diagnoses for each age group and time point of data collection is presented in Table 2.
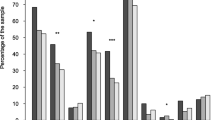
Differences in drug treatment over time among persons with HF
Use of the different drug classes in the HF group at T1–T4 is presented in Table 3 and illustrated in Fig. 1. Corrected for age and sex, the use of RAS inhibitors and BBs increased over time (p < 0.001), whereas the use of digitalis and loop diuretics decreased (p < 0.001). At T2, the use of loop diuretics and MRAs was higher than at T1, but the overall trends were declining. However, the trend for MRAs was not statistically significant. The logistic regression model including potential confounders is presented in Table 4.
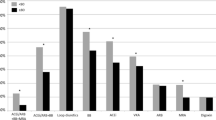
Drug treatment over time in different age groups
Figure 2a–e and sTables 1a–c in the online supplement present the prevalence of drug classes for the three age groups 85, 90, and > 95 years. The oldest group appeared to have lower treatment rates of MRAs, BBs, and RAS inhibitors.
Factors associated with the use of drug classes
In the logistic regression model including potential confounders (age, sex, living in a nursing home, ADL, MMSE, diabetes, hypertension, atrial fibrillation, depressive disorder, stroke and/or TIA, and IHD), the time trends in use of digitalis, loop diuretics, BBs, and RAS inhibitors persisted (Table 4 and online supplement sTable 2).
Higher age was associated with lower use of RAS inhibitors and BBs. Women were more likely to be prescribed RAS inhibitors than men, and higher ADL was associated with increased BB use. Persons with atrial fibrillation were more likely to use digitalis and RAS inhibitors. People with hypertension had a higher use of BBs and RAS inhibitors. Diabetes was associated with a higher prevalence of loop diuretics and RAS inhibitors. IHD was associated with higher prescribing of BBs but lower use of digitalis. Persons with depressive disorder were less likely to receive MRA treatment.
Discussion
In this analysis of cross-sectional data at four different time points between 2000 and 2017 among very old people, the major findings were that the use of the HF drugs RAS inhibitors and BBs increased over time, while the use of loop diuretics and digitalis decreased. In this population, the prevalence of HF was about 30%, irrespective of sex, and the prevalence of HF increased with age.
Description of the very old HF population
In common with other studies focusing on people ≥80 years old with HF, a majority of our participants were female [13, 24, 35]. Our finding of higher prevalences of cardiovascular comorbidities and diabetes among persons with HF is consistent with previously published literature [2, 36, 37]. Similar results are seen in the literature regarding higher prevalence of major NCD [36,37,38,39,40] and depressive disorder among people with HF [36, 40,41,42]. Malnutrition is also common among people with HF [43, 44], and in our material, the participants with HF had poorer nutrition status. In addition, quality of life has been reported to be lower among people with HF than the general population [1, 45, 46], which aligns with worse outcomes on the PGCMS scale and the SF-36 question about self-rated health in our HF population.
Temporal trends in HF treatment among the very old
A few previous studies have examined trends in HF drug treatment over time with a focus on, or subgroup analyses of, people ≥80 years old [13, 21, 24, 47]. The only conclusive change seen in all articles was increased prescribing over time for BBs, as in our results. Moreover, the use of digitalis decreased over time both in our results and in the studies where this drug class was included [24, 47]. This is in line with a long-term trend that has been seen in patients regardless of age [47,48,49,50,51].
For treatments other than BBs and digitalis, the results in the abovementioned articles were diverse. Parén et al. used the Swedish National Patient Register (NPR) and the Swedish Prescribed Drug Register to analyse HF drug use during the period 2005–2014 [47]. The NPR has a 99% coverage of all hospitalisations in Sweden [52]. A subgroup analysis was performed for the 27 662 participants who were 85–99 years old. During this time interval, the use of RAS inhibitors increased while the use of MRAs and loop diuretics decreased. Another study showed that the use of RAS inhibitors decreased and MRAs showed no statistically significant change over time for people > 80 years old [21]. That study selected all persons with EF < 40% from the Swedish HF Registry as their study population, and compared HF drug use over the years 2000–2018 among the age groups > 80, 70–79, and < 70 years. One study that recruited hospitals from 30 ESC countries showed that the use of both RAS inhibitors and MRAs was higher in 2005 than in 2000 [24]. That study compared HF treatment for people > 80 years old between the years 2000 (Euro Heart Failure Survey I, EHFS I) and 2005 (Euro Heart Failure Survey II, EHFS II).
One important factor that might explain the differences in the results is the time span studied. The material in Stolfo et al. and Parén et al. [21, 47] covered roughly the same years as our material, while Komajda et al. [24] looked at the early 2000s. The landmark study for MRAs, RALES, was published in 1999 [53]. Sharp increases were seen in the prescribing rates of MRAs in the years following the publication of RALES, but problems emerged with adverse events such as hyperkalaemia [54]. The benefits compared to the risks of using MRAs in the community were questioned [55, 56], which could explain the subsequent decline in prescribing of MRAs. This could also be the reason for the peaks in MRA prevalence found to occur in 2004 by Stolfo et al. [21], in 2005 by Komajda et al. [24], in 2006 by Parén et al. [47], and in 2005–2007 in our results; these peaks were followed by decreasing levels in all studies (except Komajda et al., whose study ended in 2005). The time factor could also explain divergent findings regarding whether or not the use of loop diuretics decreased. As guidelines have been implemented to a greater extent over time, resulting in higher use of evidence-based drug classes, the need for loop diuretics may not be as pronounced as before.
The differences in study populations could also affect the comparability of the studies.
All participants in Stolfo et al. had EF < 40% [21], while we and other studies included participants irrespective of EF [13, 24, 47]. Since there were no evidence-based treatment recommendations for HF with preserved EF (HFpEF) during the time span studied [19], this could be a contributing factor to the relatively low levels of RAS inhibitors and BBs among our participants. The higher prevalence of HFpEF among old people with HF has been suggested as an explanation for the discrepancies regarding the use of evidence-based treatment between younger and older persons [8]. In a population comprising all patients with a diagnosis of HF between 2010 and 2019 from the Heart Centre or Department of Internal Medicine at Umeå University Hospital in northern Sweden, 47% had HFpEF [57]. In our very old population, the prevalence of HFpEF was possibly even higher. As a consequence of not knowing the proportions with different classes of EF, it is not possible to state which levels of evidence-based medications are satisfactory. Nevertheless, recently published studies have shown that old people with HF are under-prescribed evidence-based HF treatment even in populations limited to HFrEF [7, 21, 58]. Moreover, even after adjusting for additional factors such as comorbidities, NYHA classification, and renal function, the age differences in receiving guideline-recommended treatment were still present in these studies [21, 58]. In our material, the use of evidence-based HF medications appeared to be lowest in the oldest group (≥95 years). However, the differences between age groups were not statistically tested.
The importance of person-centred therapy must also be underlined, and taken into consideration when interpreting the results, as very old people with HF have a high prevalence of comorbidities, polypharmacy, frailty, and risk of adverse medication events, which may affect the possibility of following guidelines [6]. Extra attention regarding drug treatment is required among people ≥80 years with HF, due to these factors as well as declining renal function with age, and so dose reductions may be needed [59]. We can speculate that the prescribers prioritised RAS inhibitors among people with very low renal function who may not have tolerated treatment with both RAS inhibitors and MRAs, resulting in very low levels of MRAs among the oldest in our population. It might have been a challenge to start treatment with MRAs in this group due to the risk of adverse events like hyperkalaemia.
The overall increasing levels of evidence-based HF treatment among very old people over time, seen in our material and previously published studies, may be an indication of increased awareness among prescribers of the age differences and an attempt to even these out.
Factors associated with drug classes
Atrial fibrillation was strongly associated with digitalis in our material. This is logical, as this drug class has long been recommended as a rate-controlling substance for the condition [60]. Unexpectedly, atrial fibrillation was not associated with BBs; however, as expected, IHD was associated with a higher prevalence of BBs. This reflects the treatment guidelines, where BBs have been recommended to most patients with stable angina or after a myocardial infarction [61, 62]. Associations were also found between hypertension and both BBs and RAS inhibitors, again reflecting the guidelines where people with hypertension and HF have been recommended to use RAS inhibitors and BBs [63]. RAS inhibitors were suggested as the first-line treatment of hypertension among persons with HF and/or diabetes as early as the beginning of the 2000s [64], which aligns with the association found between diabetes and RAS inhibitors. Diabetes was also associated with higher use of loop diuretics. In a previous Danish study, a suggested explanation was that increased use of loop diuretics, which can be seen as a reflection of the severity of HF, was a risk factor for developing diabetes [65]. However, since we do not know if the use of loop diuretics preceded the diagnosis of diabetes, we were not able to determine whether there was a cause-effect association in our population.
Age was associated with lower use of BBs and RAS inhibitors. Under-prescribing of BBs and RAS inhibitors to old people has been reported in several articles. Patient-related factors such as comorbidities, poor tolerance, or frailty, as well as prescriber-related factors such as lack of awareness of guidelines, fear of adverse effects, reluctance to make changes in very old people’s treatment, and focus on improved symptoms rather than outcome, have been suggested to explain why these drugs are less used among old people [7, 9, 24, 58, 66,67,68].
There was an association between female sex and higher prescribing of RAS inhibitors in our material. Similar results have been shown in a recent Swedish study [21], the authors of which hypothesised that sex-related differences in patient characteristics could explain the discrepancy. Older age, higher heart rate, higher blood pressure, and more symptoms have been shown among women compared to men in the Swedish HF registry. Aside from older age, which is not relevant in the present study as we adjusted for age, this might be the case in our material as well.
An association between depressive disorders and lower use of MRAs was seen in our results. While one might speculate that individuals with depression could be less interested in proceeding to more intense treatment for their other disorders, this finding could also represent a chance association.
Strengths and limitations
As there were no exclusion criteria connected to health status, cognitive function, or living conditions in the GERDA study, our population is expected to be representative of the sampled age groups in northern Sweden. The population register from the Swedish National Tax Agency is highly accurate, which made it easy to identify and contact eligible participants. The sample size is large in the context of the very old age group, and a relatively high proportion of the invited persons chose to take part. However, we selected people aged 85, 90, and ≥95, and cannot say for sure that these groups reflect the heterogeneity of all individuals aged ≥85.
Trained investigators thoroughly conducted all tests and assessments of the participants. To prevent loss of data, information regarding health and medication use was collected directly from the participants or someone very close to them, in addition to the information that was extracted from medical records.
We acknowledge that there are limitations in our study, the major one being the lack of information regarding EF and NYHA classes. These factors are the most important to determine which HF treatment is recommended. Therefore, we cannot tell how many of the participants should have been treated with the drugs that are recommended for HFrEF. Also, since this data collection was initiated already in the year 2000, the conditions and opportunities for diagnosing HF may have changed over time, which in turn could affect the prevalence of HF.
Other important factors where information was not accessible are impaired renal function and risk of hypotension or bradychardia. This could limit the use of HF medications in our population, and must be considered when interpreting the results.
Information regarding use of pro re nata medication was not available. Among the drug classes investigated, loop diuretics can be recommended as such, and so there is a risk of under-reporting of loop diuretics in our material. Regarding the trend over time, if the decline in the use of loop diuretics was partly based on an increased pro re nata use later in time, this would still be a sign of improved treatment, as loop diuretics should be used in as low doses as possible, and self-management is encouraged to treat fluid retention according to guidelines [1, 14,15,16,17,18,19]. Further, the use of other diuretics might have had an impact in the use of loop diuretics, which should be taken into account when reading the results.
It was not possible to obtain information regarding how many participants used MRAs from the group with potassium-sparing agents. We assume that MRAs accounted for most of the drug use in the group, but this could be an overestimation of MRA users.
Conclusion
In our material, comprising very old people, about 30% of both men and women had HF. The prevalence of HF increased with higher age. Both cardiovascular and non-cardiovascular comorbidities were more common among the persons with HF compared to those without HF, and those with HF also reported lower quality of life.
In the HF population, the use of evidence-based medications for HF increased over time. Between 2000 and 2017, there was an increase in the use of RAS inhibitors and BBs among persons with HF, in parallel with a decrease in the use of loop diuretics and digitalis. The improved use of HF drugs over time may be a sign of better awareness among prescribers regarding the under-prescribing of guidelines-recommended treatment to old people.
Among several factors associated with cardiovascular drug use in the HF population, we found that age correlated with a lower prevalence of RAS inhibitors and BBs. This may be an indication that under-prescribing to some extent remains. However, the lower use of these medications could also indicate cautious prescribing to very old and frail individuals, and while it might be possible to further improve prescribing it is also increasingly important to individually tailor drug treatment in advanced age.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to issues of individual privacy but are available from the corresponding author on reasonable request.
References
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726. https://doi.org/10.1093/eurheartj/ehab368.
Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. 2023;118(17):3272–87. https://doi.org/10.1093/cvr/cvac013.
Thomas S, Rich MW. Epidemiology, pathophysiology, and prognosis of heart failure in the elderly. Clin Geriatr Med. 2007;23(1):1. https://doi.org/10.1016/j.cger.2006.08.001.
Skrzypek A, Mostowik M, Szeliga M, Wilczyńska-Golonka M, Dębicka-Dąbrowska D, Nessler J. Chronic heart failure in the elderly: still a current medical problem. Folia Med Cracov. 2018;58(4):47–56.
Lazzarini V, Mentz RJ, Fiuzat M, Metra M, O’Connor CM. Heart failure in elderly patients: distinctive features and unresolved issues. Eur J Heart Fail. 2013;15(7):717–23. https://doi.org/10.1093/eurjhf/hft028.
Warner V, Nguyen D, Bayles T, Hopper I. Management of heart failure in older people. J Pharm Pract Res. 2022;52(1):72–9. https://doi.org/10.1002/jppr.1796.
Vidal J-S, Guibert E, Pesce A, Beauplet B, Roger J-D, Carrière I, et al. National survey on the management of heart failure in individuals over 80 years of age in French geriatric care units. BMC Geriatr. 2019;19(1):204–204. https://doi.org/10.1186/s12877-019-1215-y.
Bosco-Levy P, Favary C, Jove J, Lassalle R, Moore N, Droz-Perroteau C. Pharmacological treatment patterns in heart failure: a population-based cohort study. Eur J Clin Pharmacol. 2020;76(1):97–106. https://doi.org/10.1007/s00228-019-02758-2.
Holmström A, Sigurjonsdottir R, Edner M, Jonsson Å, Dahlström U, Fu M. Increased comorbidities in heart failure patients ≥ 85 years but declined from > 90 years: data from the Swedish Heart failure Registry. Int J Cardiol. 2013;167(6):2747. https://doi.org/10.1016/j.ijcard.2012.06.095.
Forman DEMD, Cannon CPMD, Hernandez AFMDMHS, Liang LP, Yancy CMD, Fonarow GCMD. Influence of age on the management of heart failure: findings from get with the guidelines–Heart failure (GWTG-HF). Am Heart J. 2009;157(6):1010–7. https://doi.org/10.1016/j.ahj.2009.03.010.
Muntwyler J, Cohen-Solal A, Freemantle N, Eastaugh J, Cleland JG, Follath F. Relation of sex, age and concomitant diseases to drug prescription for heart failure in primary care in Europe. Eur J Heart Fail. 2004;6(5):663–8. https://doi.org/10.1016/j.ejheart.2004.03.011.
Oh GC, Cho H-J, Lee SE, Kim M-S, Kim J-J, Choi J-O, et al. Management and prognosis of heart failure in octogenarians: final report from the korahf registry. J Clin Med. 2020;9(2):501. https://doi.org/10.3390/jcm9020501.
Vorilhon C, Chenaf C, Mulliez A, Pereira B, Clerfond G, Authier N, et al. Heart failure prognosis and management in over-80-year-old patients: data from a French national observational retrospective cohort. Eur J Clin Pharmacol. 2015;71(2):251–60. https://doi.org/10.1007/s00228-014-1794-7.
Task Force of the Working Group on Heart Failure of the European Society of Cardiology. The treatment of heart failure. Eur Heart J. 1997;18(5):736–53. https://doi.org/10.1093/oxfordjournals.eurheartj.a015339.
Remme WJ, Swedberg K. Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J. 2001;22(17):1527–60. https://doi.org/10.1053/euhj.2001.2783.
Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the Task Force for the diagnosis and treatment of Chronic Heart failure of the European Society of Cardiology. Eur Heart J. 2005;26(11):1115–40. https://doi.org/10.1093/eurheartj/ehi204.
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJV, Ponikowski P, Poole-Wilson PA, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur J Heart Fail. 2008;10(10):933–89. https://doi.org/10.1016/j.ejheart.2008.08.005.
McMurray JJV, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the diagnosis and treatment of Acute and Chronic Heart failure 2012 of the European Society of Cardiology. Developed in collaborati. Eur J Heart Fail. 2012;14(8):803–69. https://doi.org/10.1093/eurjhf/hfs105.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975. https://doi.org/10.1002/ejhf.592.
Daamen MAMJ, Hamers JPH, Gorgels APM, Tan FES, Schols JMGA, Brunner-La Rocca H. Treatment of heart failure in nursing home residents. J Geriatr Cardiol. 2016;13(1):44–50. https://doi.org/10.11909/j.issn.1671-5411.2016.01.001.
Stolfo D, Lund LH, Becher PM, Orsini N, Thorvaldsen T, Benson L, Hage C, Dahlström U, Sinagra G, Savarese G. Use of evidence-based therapy in heart failure with reduced ejection fraction across age strata. Eur J Heart Fail. 2022;24(6):1047–62. https://doi.org/10.1002/ejhf.2483.
Brunner-La Rocca HP, Linssen GC, Smeele FJ, van mmelen AA, Schaafsma HJ, Westendorp PH, et al. Contemporary drug treatment of Chronic Heart failure with reduced ejection Fraction the CHECK-HF Registry. JACC Heart Fail. 2019;7(1):13–21. https://doi.org/10.1016/j.jchf.2018.10.010.
Swedberg K, Ekman I. Integrating heart failure guidelines into clinical practice. Eur Heart J. 2005;suppl–J:J21–5. https://doi.org/10.1093/eurheartj/sui059.
Komajda M, Hanon O, Hochadel M, Lopez-Sendon JL, Follath F, Ponikowski P, et al. Contemporary management of octogenarians hospitalized for heart failure in Europe: Euro Heart failure survey II. Eur Heart J. 2009;30(4):478–86. https://doi.org/10.1093/eurheartj/ehn539.
von Heideken P, Gustavsson JMC, Lundin-Olsson L, Kallin K, Nygren B, Lundman B, et al. Health status in the oldest old. Age and sex differences in the Umeå 85 + study. Aging Clin Exp Res. 2006;18(2):116–26. https://doi.org/10.1007/bf03327426.
Burman M, Hörnsten C, Öhlin J, Olofsson B, Nordström P, Gustafson Y. Prevalence of obesity and malnutrition in four cohorts of very old adults, 2000–2017. J Nutr Health Aging. 2022;26(7):706–13. https://doi.org/10.1007/s12603-022-1820-x.
Weidung B, Lövheim H, Littbrand H, Wahlin J, Olofsson B, Gustafson Y. Temporal dementia and cognitive impairment trends in the very old in the 21st Century. J Alzheimers Dis. 2023;93(1):61–74. https://doi.org/10.3233/JAD-220915.
Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10(2):61–3. https://doi.org/10.3109/09638288809164103.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. https://doi.org/10.1016/0022-3956(75)90026-6.
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, Albarede J-L. The mini nutritional assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15(2):116–22. https://doi.org/10.1016/S0899-9007(98)00171-3.
Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–73. https://doi.org/10.1300/J018v05n01_09.
Lawton MP. The Philadelphia Geriatric Center Morale Scale: a revision. J Gerontol. 1975;30(1):85–9. https://doi.org/10.1093/geronj/30.1.85.
Royal College of Physicians of London, B. G. S. (1992). Standardized assessment scales for elderly people. A report of joint workshops in the Research Unit of the Royal College of Physicians of London and the British Geriatrics Society. London.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Mahjoub H, Rusinaru D, Soulière V, Durier C, Peltier M, Tribouilloy C. Long-term survival in patients older than 80 years hospitalised for heart failure. A 5-year prospective study. Eur J Heart Fail. 2008;10(1):78–84. https://doi.org/10.1016/j.ejheart.2007.11.004.
Buddeke J, Bots ML, Van Dis I, Visseren FLJ, Hollander M, Schellevis FG, Vaartjes I. Comorbidity in patients with cardiovascular disease in primary care: a cohort study with routine healthcare data. Br J Gen Pract. 2019;69(683):E398–406. https://doi.org/10.3399/bjgp19X702725.
Adelborg K, Szépligeti S, Sundbøll J, Horváth-Puhó E, Henderson VW, Ording A, et al. Risk of stroke in patients with heart failure: a Population-based 30-Year Cohort Study. Stroke (1970). 2017;48(5):1161–8. https://doi.org/10.1161/STROKEAHA.116.016022.
Heckman GA, Patterson CJ, Demers C, St Onge J, Turpie ID, McKelvie RS. Heart failure and cognitive impairment: challenges and opportunities. Clin Interv Aging. 2007;2(2):209–18.
Yang M, Sun D, Wang Y, Yan M, Zheng J, Ren J. Cognitive impairment in Heart failure: Landscape, challenges, and future directions. Front Cardiovasc Med. 2022;8:831734–831734. https://doi.org/10.3389/fcvm.2021.831734.
Oud FMM, Spies PE, Braam RL, van Munster BC. Recognition of cognitive impairment and depressive symptoms in older patients with heart failure. Neth Heart J. 2021;29(7–8):377–82. https://doi.org/10.1007/s12471-020-01527-6.
Sbolli M, Fiuzat M, Cani D, O’Connor CM. Depression and heart failure: the lonely comorbidity. Eur J Heart Fail. 2020;22(11):2007–17. https://doi.org/10.1002/ejhf.1865.
Wu Y, Zhu B, Chen Z, Duan J, Luo A, Yang L, Yang C. New insights into the Comorbidity of Coronary Heart Disease and Depression. Curr Probl Cardiol. 2021;46(3):100413–100413. https://doi.org/10.1016/j.cpcardiol.2019.03.002.
Aquilani R, Opasich C, Verri M, Boschi F, Febo O, Pasini E, Pastoris O. Is nutritional intake adequate in chronic heart failure patients? J Am Coll Cardiol. 2003;42(7):1218–23. https://doi.org/10.1016/S0735-1097(03)00946-X.
Lv S, Ru S. The prevalence of malnutrition and its effects on the all-cause mortality among patients with heart failure: a systematic review and meta-analysis. PLoS ONE. 2021;16(10):e0259300–0259300. https://doi.org/10.1371/journal.pone.0259300.
Comin-Colet J, Anguita M, Formiga F, Almenar L, Crespo-Leiro MG, Manzano L, et al. Health-related quality of life of patients with chronic systolic heart failure in Spain: results of the VIDA-IC Study/Calidad de vida relacionada con la Salud De Los pacientes con insuficiencia cardiaca cronica sistolica en Espana: resultados del estudio VIDA-IC. Rev Esp Cardiol (Engl Ed). 2016;69(3):256. https://doi.org/10.1016/j.rec.2015.07.030.
Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W, Haass M. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Br Heart J. 2002;87(3):235–41. https://doi.org/10.1136/heart.87.3.235.
Paren P, Rosengren A, Zverkova Sandstrom T, Schaufelberger M. Decrease in loop diuretic treatment from 2005 to 2014 in Swedish real-life patients with chronic heart failure. Eur J Clin Pharmacol. 2019;75(2):247–54. https://doi.org/10.1007/s00228-018-2574-6.
Svahn S, Lövheim H, Isaksson U, Sandman P-O, Gustafsson M. Cardiovascular drug use among people with cognitive impairment living in nursing homes in northern Sweden. Eur J Clin Pharmacol. 2020;76(4):525–37. https://doi.org/10.1007/s00228-019-02778-y.
Cubbon RM, Gale CP, Kearney LC, Schechter CB, Brooksby WP, Nolan J, et al. Changing characteristics and mode of death associated with chronic heart failure caused by left ventricular systolic dysfunction a study across therapeutic eras. Circ Heart Fail. 2011;4(4):396–403. https://doi.org/10.1161/CIRCHEARTFAILURE.110.959882.
Joffe SW, Dewolf M, Shih J, McManus DD, Spencer FA, Lessard D, Gore JM, Goldberg RJ. Trends in the medical management of patients with heart failure. J Clin Med Res. 2013;5(3):194–204. https://doi.org/10.4021/jocmr1376w.
de Peuter OR, Lip GYH, Souverein PC, Klungel OH, de Boer A, Büller HR, Kamphuisen PW. Time-trends in treatment and cardiovascular events in patients with heart failure: a pharmacosurveillance study. Eur J Heart Fail. 2011;13(5):489–95. https://doi.org/10.1093/eurjhf/hfq228.
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim J-L, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11(1):450–450. https://doi.org/10.1186/1471-2458-11-450.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med. 1999;341(10):709.
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA. Rates of Hyperkalemia after publication of the randomized aldactone evaluation study. N Engl J Med. 2004;351(6):543–51. https://doi.org/10.1056/NEJMoa040135.
Lund LH, Svennblad B, Melhus H, Hallberg P, Dahlström U, Edner M. Association of spironolactone use with all-cause mortality in heart failure a propensity scored cohort study. Circ Heart Fail. 2013;6(2):174–83. https://doi.org/10.1161/CIRCHEARTFAILURE.112.000115.
Fonarow GC, Albert NM, Curtis AB, Gheorghiade M, Liu Y, Mehra MR, O’Connor CM, Reynolds D, Walsh MN, Yancy CW. Incremental reduction in risk of death Associated with Use of Guideline-recommended therapies in patients with heart failure: a nested case-control analysis of IMPROVE HF. J Am Heart Assoc. 2012;1(111):16–26. https://doi.org/10.1161/xJAHA.111.000018.
Hakansson E, Brunstrom M, Norberg H, Sjalander S, Lindmark K. Prevalence and treatment of diabetes and pre-diabetes in a real-world heart failure population: a single-centre cross-sectional study. Open Heart. 2022;9(2). https://doi.org/10.1136/openhrt-2022-002133.
Veenis J, Brunner-La Rocca HP, Linssen GCM, Geerlings PR, van Gent MWF, Aksoy I, et al. Age differences in contemporary treatment of patients with chronic heart failure and reduced ejection fraction. Eur J Prev Cardiol. 2019;26(13):1399–407. https://doi.org/10.1177/2047487319835042.
Mewton N, Girerd N, Boffa J-J, Courivaud C, Isnard R, Juillard L, et al. Practical management of worsening renal function in outpatients with heart failure and reduced ejection fraction: Statement from a panel of multidisciplinary experts and the heart failure Working Group of the French Society of Cardiology. Arch Cardiovasc Dis. 2020;113(10):660–70. https://doi.org/10.1016/j.acvd.2020.03.018.
(2001) ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: Executive summary - A report of the American College of Cardiology American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients with Atrial Fibrillation). Circulation 104 (17): 2118–2150.
López-Sendó J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al. Expert consensus document on β-adrenergic receptor blockers: the Task Force on Beta-blockers of the European Society of Cardiology. Eur Heart J. 2004;25(15):1341–62. https://doi.org/10.1016/j.ehj.2004.06.002.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77. https://doi.org/10.1093/eurheartj/ehz425.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104. https://doi.org/10.1093/eurheartj/ehy339.
Lopez-Sendon J, Swedberg K, Torp-Pedersen C, McMurray J, Tamargo J, Maggioni AP, et al. Expert consensus document on angiotensin converting enzyme inhibitors in cardiovascular disease: the Task Force on ACE-inhibitors of the European Society of Cardiology. Eur Heart J. 2004;25(16):1454–70. https://doi.org/10.1016/j.ehj.2004.06.003.
Demant MN, Gislason GH, Køber L, Vaag A, Torp-Pedersen C, Andersson C. Association of heart failure severity with risk of diabetes: a Danish nationwide cohort study. Diabetologia. 2014;57(8):1595–600. https://doi.org/10.1007/s00125-014-3259-z.
Mariani M, Vella G, Bianchi C, Verde S, De Maria R, Pirelli S. Implementation of Beta-blockade in Elderly Heart failure patients: role of the nurse specialist. Eur J Cardiovasc Nurs. 2008;3196–203. https://doi.org/10.1016/j.ejcnurse.2007.09.006.
Miani DMD, Fresco CMD, Lucci DP, Albanese MCMD, Gonzini LP, Fioretti PMMD, et al. Clinical characteristics, management, and prognosis of octogenarians with acute heart failure admitted to cardiology wards: results from the Italian survey on Acute Heart failure. Am Heart J. 2009;158(1):126–32. https://doi.org/10.1016/j.ahj.2009.04.011.
Mogensen UM, Ersbøll M, Andersen M, Andersson C, Hassager C, Torp-Pedersen C, et al. Clinical characteristics and major comorbidities in heart failure patients more than 85 years of age compared with younger age groups. Eur J Heart Fail. 2011;13(11):1216–23. https://doi.org/10.1093/eurjhf/hfr116.
Acknowledgements
We wish to thank all of the Umea85+/GERDA participants, their relatives, and nurses, and all indviduals who helped with data collection, for their fundamental contributions to the study.
Funding
This work was supported by the Swedish Research Council (grant no. K2014–99X-22610–01–6); a regional agreement between Umeå University and Västerbotten County Council on cooperation in the fields of medicine, odontology and health; the Research Foundation of the Faculty of Medicine and Odontology at Umeå University; the Swedish Dementia Association; the Strategic Research Area Health Care Science (SFO-V); the European Union and Regional Development Fund: and the Interreg IIIA Mitt-Scandia and the Bothnia-Atlantica Program.
Open access funding provided by Umea University.
Author information
Authors and Affiliations
Contributions
YG and BO initiated the database and conducted the collection of data. All authors contributed to the study design and concept. SS and HL analysed the data. SS, MG and LA drafted the manuscript. All authors contributed to critical review and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Swedish Ethical Review Authority (registration number 2019–03757). The Umeå 85+/GERDA study had previously received approval from the Regional Ethical Review Board in Umeå (registration numbers 99–326, 05–063 M, 09–178 M, 2014-221-31 M).
Consent for publication
Not applicable.
Informed consent
Informed consent was obtained from all participants before inclusion. A close person/relative was also consulted regarding consent in each case of diagnosed or suspected cognitive impairment.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Svahn, S., Appelblad, L., Lövheim, H. et al. Prevalence of heart failure and trends in its pharmacological treatment between 2000 and 2017 among very old people. BMC Geriatr 24, 701 (2024). https://doi.org/10.1186/s12877-024-05307-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05307-4