Abstract
Objective
In this study, we aimed to assess the synergistic effects of cognitive frailty (CF) and comorbidity on disability among older adults.
Methods
Out of the 1318 participants from the Malaysian Towards Useful Aging (TUA) study, only 400 were included in the five-year follow-up analysis. A comprehensive interview-based questionnaire covering socio-demographic information, health status, biochemical indices, cognitive and physical function, and psychosocial factors was administered. Binary logistic regression analysis was employed to estimate the independent and combined odd ratios (ORs). Measures such as the relative excess risk due to interaction (RERI), the attributable proportion of risk due to the interaction, and the synergy index were used to assess the interaction between CF and comorbidity.
Results
Participants with CF (24.1%) were more likely to report disability compared to those without CF (10.3%). Synergistic effects impacting disability were observed between CF and osteoarthritis (OA) (OR: 6.675, 95% CI: 1.057–42.158; RERI: 1.501, 95% CI: 1.400–1.570), CF and heart diseases (HD) (OR: 3.480, 95% CI: 1.378–8.786; RERI: 0.875, 95% CI: 0.831–0.919), CF and depressive symptoms (OR: 3.443, 95% CI: 1.065–11.126; RERI: 0.806, 95% CI: 0.753–0.859), and between CF and diabetes mellitus (DM) (OR: 2.904, 95% Confidence Interval (CI): 1.487–5.671; RERI: 0.607, 95% CI: 0.577–0.637).
Conclusion
These findings highlight the synergism between the co-existence of CF and comorbidity, including OA, HD, DM, and depressive symptoms, on disability in older adults. Screening, assessing, and managing comorbidities, especially OA, HD, DM and depressive symptoms, when managing older adults with CF are crucial for reducing the risk of or preventing the development of disability.
Similar content being viewed by others
Introduction
Approximately 15% of the global population is estimated to have some form of disability due to the rapid rise in the global aging population and a parallel increase in the prevalence of chronic health conditions [1]. With the progressive surge in longevity and lifespan, disability is steadily becoming an integral factor of disease burden worldwide. Several chronic diseases, including ischemic heart disease, stroke, diabetes, and dementia in mid-life or late life, have been identified as causes of disability-adjusted life years (DALYs), which is the sum of years lost due to premature mortality [2]. Functional disability in late life appears to be linked with gradual age-related deterioration and the coexistence of multiple diseases [3, 4]. Consequently, this strongly predicts future needs for assisted living and long-term nursing care, which heavily burden the healthcare system in addition to economic and personal burdens [2]. Disability risk factors include gender, age, socioeconomic status, lifestyle, and chronic diseases [5, 6]. This phenomenon is also a known adverse outcome of both frailty and cognitive impairment in older adults [7, 8].
Notably, frailty and cognitive impairment were often viewed as two independent concepts in previous studies until cognitive frailty (CF) was introduced by the consensus group of the International Academy on Nutrition and Aging (IANA) and the International Association of Gerontology and Geriatrics (IAGG) [9]. The simultaneous coexistence of physical frailty and cognitive impairment, or CF, seems to entail a greater risk of all-cause mortality and adverse health outcomes than their respective effects alone, as reported in both community-based and population-based studies [10,11,12]. The higher prevalence and incidence of CF, specifically among community-dwelling Malaysian older adults (39.6%; 7.1 per 100 person-years), has become a worrisome issue as those with CF are predicted to develop disability incidence by fivefold as compared to frailty and mild cognitive impairment on its own, based on five years cohort study [13,14,15].
Both physical frailty and cognitive impairment have been identified as risk factors for physical disability [8, 15], where these may act independently or, more often, in synergistic combinations. Individuals with CF are more likely to experience difficulties in performing activities of daily living (ADLs) and instrumental activities of daily living (IADLs) by two- to fivefold, leading to functional impairment and dependence on others for care [16]. Chronic low-grade inflammation, often observed in individuals with CF, can impair the regeneration of muscle tissue following injury and exacerbate muscle mass loss and functional decline, limiting an individual’s ability to perform activities of daily living and subsequent disability incidence [15, 17].
Furthermore, the presence of chronic diseases in older adults with CF further exacerbates the decline of physiological reserve function in multiple systems, thereby increasing the risk of adverse health outcomes [18]. Different chronic disease profiles or comorbidity patterns, defined as the co-occurrence of two or more chronic conditions in an individual with CF, may impersonate clinically different etiologic pathways to the occurrence of disability in late life. The most common conditions among older adults with CF are diabetes mellitus, hypertension, depression, and cardiovascular disease [19,20,21]. The simultaneous presence of two or more chronic illnesses that include high depressive symptoms is associated with high rates of prospective ADL-IADL disability, potentially due to polypharmacy adverse reactions [22, 23]. Different comorbidity patterns may influence the pathways to disability in late life, accentuating the need for comprehensive assessment and management strategies tailored to the specific combination of chronic conditions in individuals with CF.
However, to date, the joint effect of CF and comorbidity on disability incidence has not been investigated. Seeing as Malaysia is on the cusp of transforming into an aging nation, assessing older adults with CF and comorbidity in this population may enable the identification of older adults who are more at risk for disability earlier to implement a more effective intervention. We hypothesised that the presence of comorbidity in older adults with CF has differential effects on the incidence of disability and may exceed the sum of their effects alone. Thus, the aim in this prospective cohort analysis was to evaluate the synergistic effects of CF and comorbidity on the incidence of disability among Malaysian older adults aged 60 years and above.
Methods
Study design and participants
This is a follow-up study of the Long-Term Research Grant Scheme – Towards Useful Aging (LRGS TUA) cohort [24] at five years endpoint. LRGS-TUA is a prospective cohort study of community-dwelling older adults aged 60 years and above in Malaysia. They were recruited through a multi-stage random sampling procedure from two states with the highest prevalence of older adults, namely Selangor and Perak (representing central and northern regions of Malaysia). The study employed a three-stage sampling process that involved selecting primary sampling units (PSUs) (i.e., states), followed by the selection of secondary sampling units (SSUs) (i.e., a random census circle within the state), and finally, the selection of tertiary sampling units (TSUs) (i.e., living quarters within the census circle). Probability sampling weights were performed at each stage to ensure that the study sample accurately represents the target population.
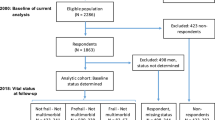
This study involved two data collection phases: baseline (collected in 2013) and after five years of follow-up (collected in 2018) prior to obtaining insights into the trajectory of participants’ disability status over the study period. From this process, a total of 815 participants who had complete physical frailty and cognitive statuses data at baseline were analyzed. At baseline, older adults diagnosed with dementia, known psychiatric conditions, severe vision, speech, and hearing problems, as well as those who were non-ambulant, were excluded to ensure the reliability of the data collected. The selected participants should be able to converse in either Malay, English, Chinese or Tamil languages and agree to sign the consent form to participate in this study.
A total of 400 participants (49.1%) were successfully followed up at five years. Whilst 4.8% had passed away, and 46.1% of the participants refused to participate or failed to be contacted. A prior study reported a fairly high drop-out rate among the participants who were older in age and lived alone, which restricted their participation, possibly due to a lack of support for acquiring care and transportation difficulties [14]. Furthermore, potential variations attributed to seasonal and regional factors were considered during the follow-up assessment, as the data collection was conducted within the same month as the baseline, spanning from August to April. The study has been approved by the Medical Research and Ethics Committee of the Universiti Kebangsaan Malaysia (UKM1.21.3/244/NN-2018-145). Before participation, each participant provided informed, written consent and was given the assurance of anonymity.
Data collection
Trained enumerators conducted structured interviews with the participants, and measurements were taken for various parameters at nearby community centers. The questionnaire used was to gather data on socio-demographic information, health status, neuropsychological and psychosocial functions, lifestyle, blood pressure, anthropometry, biochemical indices, and functional status. The baseline assessments were repeated five years later at follow-up. All procedures were conducted in compliance with relevant guidelines and regulations, as detailed in the study by Shahar et al. [24]. Participants were given rest breaks during the tests, and monetary incentives were provided for completing the assessments.
Operationalisation of cognitive frailty (CF)
As described in our prior report [13, 14], the classification of CF was based on the concurrent existence of physical pre-frailty/frailty and subjective cognitive decline/mild cognitive impairment (MCI) at baseline. Participants were then divided into two groups, CF and Non-CF groups.
Physical frailty
Physical frailty was assessed using Fried et al. [25] criteria and the cut-off points outlined in the Cardiovascular Health Study (CHS). The assessment’s variables were categorized as follows: (1) unintentional weight loss of more than 5 kg in the previous years; (2) self-reported exhaustion or tiredness based on two items of the Centre of Epidemiologic Studies Depression scale (CES-D): (a) ‘I felt that everything I did was an effort’ and (b) ‘I could not get going’; (the question was how often in the last week did you feel like this (rare = 0, some or little time (1–2 days) = 1, moderate (3–4 days) = 2, and most of the times = 3); 3) low physical activity assessed using the Physical Activity Scale for Elderly (PASE) [26]; 4) weakness measured using dominant hand grip strength (digital hand dynamometer; Jamar® Plus+, Patternson Medical, IL, USA); and 5) slowness, measured using the five-metre gait speed test. Participants who meet three out of the five criteria are typically classified as frail, while those who meet 1 to 2 of these criteria are generally categorized as pre-frail.
Mild cognitive impairment (MCI)
Mild cognitive impairment (MCI) is a clinical condition characterized by cognitive decline that is greater than expected for an individual’s age and educational background but does not significantly impair daily functioning or independence in activities of daily living. Participants were classified as having MCI if they exhibited subjective memory complaint (reported by the participants based on item ten of the 15-item Geriatric Depression Scale or their caregivers) along with objective memory impairment (at least 1.5 standard deviations below the mean for Rey Auditory Verbal Learning Test, RAVLT), but with minimal to no functional limitations in basic activities of daily living (at least 1.5 standard deviations below the mean). The subjective memory complaints are the self-reported cognitive symptoms, particularly memory complaints, for those who perceive a decline in their cognitive abilities. Additionally, they were required to maintain global cognitive function (indicated by a Malay version of Mini-Mental State Examination, M-MMSE score of ≥ 19) and not diagnosed with dementia by a physician at baseline. Those participants with M-MMSE < 19 were excluded from the study as it is generally considered indicative of moderate to severe cognitive impairment. These criteria were established based on Petersen et al. [27] and Lee et al. [28]. Participants who did not meet these criteria were categorized as normal.
Comorbidities
Self-reported data was employed to determine the presence of comorbidity, which is defined as the co-occurrence of two disorders within a single individual. Self-reported information on certain diseases (hypertension, hypercholesterolemia, diabetes mellitus, osteoarthritis, heart disease, chronic kidney disease, cancer) diagnosed by doctors in the prior years was recorded. Self-report of disease diagnoses has been frequently used in epidemiology studies and reported to be valid [29]. Meanwhile, depressive symptoms were assessed using the geriatric depression scale (GDS-15), where those with a score of five and above were categorized as depressed [30].
Outcome measure
Disability
The data on disability was measured at five-years follow up. To assess restrictions in daily activities and social participation resulting from health problems in the past month, The World Health Organization Disability Assessment Schedule (WHODAS, version 2.0), a 12-item questionnaire with a five-point Likert scale (ranging from 0 for none to 4 for very severe) was used [31]. WHODAS was used to evaluate disability, which covers six main areas, including self-care, participation, cognition, mobility, getting along, and life activities. The degree of disability was classified as follows: 0 (no disability), 1–4 (mild disability), 5–9 (moderate disability), and 10–48 or more (severe disability). In this study, participants were divided into two groups based on their disability status: those with severe disability and those without disability (all others).
Potential confounding factors
Multiple factors assessed at baseline were considered confounding factors that may affect the occurrence of disability over an extended period of time. These elements were previously addressed in detail [24], including:
Socio-demographic information and medical history
The information collected included the participant’s age, gender, ethnicity, level of education, household income, living situation (living alone or with others), and whether or not they smoked.
Nutritional status, body composition, and blood pressure
The study included various anthropometric measurements such as height, weight, waist circumference, mid-upper arm circumference (MUAC), and calf circumference. Body mass index (BMI) was calculated by dividing the body weight in kilograms by the square of the standing height in meters. Additionally, body composition was assessed using the Bio-electrical Impedance Analysis InBody S10 (Biospace, Seoul, Korea). Furthermore, systolic and diastolic blood pressure were recorded using a calibrated digital automatic blood pressure monitor (OMRON, Kyoto Japan).
Laboratory analysis
A certified phlebotomist took 20 ml of fasting peripheral venous blood using a butterfly syringe for the biochemical analysis, which included fasting blood sugar (FBS), Haemoglobin A1c (HbA1c), total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and albumin (ALB).
Psychosocial and functional assessments
The assessment of social support was conducted using the Medical Outcome Study Social Support Survey (MOSS) [32], while the functional status was evaluated using the Instrumental Activities of Daily Living (IADL) scale [33].
Statistical analysis
Descriptive statistics were utilized to identify differences in participant characteristics between the CF and Non-CF groups at baseline, in order to determine any potential confounding factors. Categorical variables were compared using the Chi-Square test (χ2), while continuous variables were compared using the independent t-test. The factors reported were based on the baseline data, rather than follow-up data. The findings were presented as n (%) for categorical data and mean ± standard deviation for normally distributed continuous data. These statistical analyses were conducted using SPSS version 23.0 (Licensed materials - Property of SPSS Incorporation an IBM Company Copyright 1989 and 2010 SPSS, Chicago, United States).
A binary logistic regression model (BLR) was conducted to estimate the independent effects of each health condition on the incidence of disability and adjusted for the confounding factors. Then, the hypothesis of the combined effect of CF and comorbidity on the disability incidence was further tested using BLR. To assess multicollinearity among predictor variables, tolerance and variance inflation factor (VIF) values were also computed. Tolerance values below 0.2 and VIF values exceeding 5 were considered indicative of potential multicollinearity.
Relative excess risk due to interaction (rERI)
Each model used three dummy (indicator) variables to represent the three comparisons made with the reference category of either having CF or having a comorbidity, or having both (RR11); CF without the comorbidity (RR10); and the comorbidity without CF (RR01). The three measures of synergism were calculated based on Rothman’s definitions [34]. The RERI, which stands for relative excess risk due to interaction, represents the additional risk that arises from the interaction between CF and comorbidity in individuals who have both conditions. This extra risk is calculated by subtracting the sum of the individual effects of each condition from the combined effect. This is calculated by the following equation: RERIRR = RR11 - RR10 - RR01 + 1. The AP, or attributable proportion due to interaction, refers to the portion of the combined RR (RR11) that results specifically from the interaction between the two conditions. While, the SI, or synergy index, is the ratio of the combined effect to the sum of the individual effects of the two conditions [34]. Additionally, the descriptive command was used to calculate the 95% confidence interval based on the standard error of the mean for RERI, AP, and SI.
The AP and the SI provide information on the magnitude of the impacts, while the RERI provides the direction of any synergistic effects [35]. The RERI is seen as the primary indicator that synergistic effects exist. A RERI of 0 denotes that the two conditions do not interact and act independently. When the RERI value is negative, it indicates that the two conditions are interacting in such a way that they lower the risk of the outcome. Conversely, a positive RERI value suggests that the interaction between the two conditions is increasing the risk of the outcome. The synergistic effect can account for 0–100% of the total RR, depending on the range of the AP from 0.0 to 1.0. If the SI is larger than 1.0, the combined impact of the conditions is greater than the sum of the individual effects. At the extreme, RERI and SI would approach infinity, and the AP would approach 1.0 when two conditions have no influence independently but a measurable effect when combined [34].
Results
Characteristics of the participants
Of the 815 participants enrolled at baseline, only 400 were included in the follow-up analysis. Table 1 compares the demographic characteristics of participants with CF (N = 158) and without CF, known as non-CF (N = 242). Participants with CF were older (mean: 68.61 ± 5.52 years old), mostly female (58.9%) and of non-Malay ethnicities (65.8%). CF participants had significantly lower years of education (5.41 ± 4.33 years) and household income (RM1340.85 ± 1660.38/USD304.74 ± 377.36) as compared to the non-CF participants (RM441.53 ± 2808.38/USD441.53 ± 638.27) (p < 0.05). Those with CF also had higher body fat percentage (39.98 ± 9.82% vs. 37.80 ± 10.22%), and lower skeletal muscle mass (19.80 ± 4.58 kg vs. 20.98 ± 5.00 kg), than the non-CF participants (p < 0.05). Additionally, CF participants were observed to have significantly lower social support (33.89 ± 15.58 vs. 38.92 ± 14.67), and poorer functional status (12.99 ± 1.68 vs. 13.26 ± 1.45), as compared to non-CF participants (p < 0.05).
Disability status among CF and Non-CF participants after five years of follow-up
In this study, participants with CF more commonly reported manifestations of disability. CF participants reported more than double the percentage of experiencing disability at 24.1% as compared to 10.3% of the non-CF participants. Furthermore, Table 2 shows that the adjusted OR of reporting disability was 1.761 times greater (95% CI: 0.907, 3.422) among CF participants compared to those without CF (p < 0.05).
Independent associations between health conditions and incidence of disability
As shown in Table 2, the chronic health conditions included namely osteoarthritis (OR: 4.413, 95% CI: 1.082, 17.992), depression (OR: 1.866, 95% CI: 0.981, 3.546), heart diseases (OR: 1.844, 95% CI: 0.692, 4.909), and diabetes mellitus (OR: 1.536, 95% CI: 0.267, 5.075), were independently associated with increased adjusted OR of disability. Notably, osteoarthritis was associated with the highest independent OR of disability after adjusting for covariates (p < 0.05).
Combined associations and synergistic effects between CF and comorbidities on disability
Table 3 indicates that the combined effects of CF and all significant comorbidities are linked to a heightened risk of disability, surpassing the independent effects of each condition. In particular, a synergistic effect was observed between CF and osteoarthritis, with participants reporting both conditions being 6.675 times more likely to report disability (95% CI: 1.057, 42.158) compared to those without either condition. The RERI between the two conditions was 1.501 (95% CI: 1.400, 1.570), suggesting that the combined effects of CF and osteoarthritis on disability are greater than the sum of their independent effects. Moreover, 22.5% of the total OR was attributable to this interaction (AP: 0.225, 95% CI: 0.160, 0.290).
The synergistic effects between CF and heart diseases were also associated with an increased risk of disability incidence by 3.480 times greater (95% CI: 1.378, 8.786) than participants who did not report having either condition. The RERI was 0.875 (95% CI: 0.831, 0.919), also indicating that the synergistic effects of CF and heart diseases on disability are greater than the sum of the independent effects of each condition. Notably, 25% of the OR was attributable to this synergism (AP: 0.251, 95% CI: 0.207, 0.295).
The combined effects of CF and depression also increased the risk of disability by 3.443 (95% CI: 1.065, 11.126) times greater compared to those who did not report experiencing either condition. The RERI between the two conditions was 0.806 (95% CI: 0.753, 0.859), indicating that the synergistic effects of CF and depression on disability are greater than the sum of the independent effects of each condition. Of the total OR, 23.4% was attributable to this interaction (AP: 0.234, 95% CI: 0.181, 0.287). There were no synergistic effects between CF and other included comorbidity, including hypertension, hypercholesterolemia, chronic kidney disease, and cancer on the incidence of disability after five years follow up.
Synergistic effects were also observed between CF and diabetes mellitus, impacting the incidence of disability by 2.904 times greater (95% CI: 1.487, 5.671). The RERI was 0.607 (95% CI: 0.577, 0.637), indicating that the synergistic effects of CF and diabetes mellitus are greater than the sum of the independent effects of each condition. About 21% of the total OR was attributable to this synergism (AP: 0.209, 95% CI: 0.178, 0.239).
In the analysis, moderate multicollinearity was observed among the predictor variables, as indicated by the tolerance values ranging from 0.526 to 0.990 and corresponding VIF between 1.010 and 1.899. While these values suggest the presence of moderate collinearity, they remain below commonly accepted thresholds for severe multicollinearity, ensuring the reliability of the regression results.
Discussion
Generally, the findings of this study indicated that the combined effect of CF and comorbidities on the incidence of disability exceeds the sum of their separate effects. In scenarios where resources are limited, it may be most practical to focus on subgroups where the greatest impact on disability prevention or intervention is expected by targeting CF. Hence, methods for assessing additive interaction using SI, AP, and RERI [36] can help to achieve this objective. In the previous longitudinal study, the synergistic effects of depression and comorbidity were associated with increased disability and decreased quality of life among older adults in Singapore by three-fold [37]. Additionally, both frailty and cognitive impairment were reported to have a synergistic effect with comorbidity on disability occurrence; however, these two syndromes were studied independently [38, 39]. To date, this is the first study of its kind to investigate the synergistic effects between CF and comorbidity in relation to disability incidence through a cohort prospective study among community-dwelling older adults in Malaysia.
The combined effect of CF and osteoarthritis on disability incidence was observed to be the highest by six times more as compared to those who reported either one of the conditions. Both conditions share important common risk factors and have also been established as predictors of falls and disability in older adults [15, 40]. Older adults with osteoarthritis-related pain are more prone to have decreased confidence in their balance [41], delayed walking speeds and poorer handgrip values [42], heightened psychological concern related to falls, and are less likely to be physically active [41], which consequently exacerbates physical impairment leading to a downwards trajectory into disability. Furthermore, osteoarthritis and CF are often accompanied by depression and lower physical performance as related pain may restrict daily activities and heighten the risk of depressive symptoms [13, 14, 41]. Tai Chi, a traditional Chinese practice involving slow, coordinated movements, mindfulness, and controlled breathing, demonstrates potential in enhancing physical and psychological health in individuals with knee osteoarthritis [43, 44] and MCI [45]. Moreover, emerging evidence suggests the effectiveness of multidomain interventions in mitigating the risks and reversing cognitive frailty (CF) and comorbidity in older adults [46, 47]. Therefore, integrating exercises with cognitive stimulation, nutritional support, and psychosocial interventions holds promise in reducing disability risk associated with comorbidities while enhancing cognitive function and emotional well-being.
This study also demonstrated the synergistic effect of older adults with CF and heart diseases on the incidence of disability by more than three-fold, as compared to those without both conditions. Heart diseases have been identified as the most common self-reported cause of the overall decline in functional status [48], which in turn progresses to disability in later life. Besides, research has demonstrated that reduced cerebral blood flow resulting from decreased cardiac output in individuals with heart failure can potentially lead to both sarcopenia and cognitive impairment [49, 50]. Furthermore, modifiable risk factors such as educational level, exercise capacity, sleep disturbance, and depressive symptoms are associated with an elevated likelihood of cognitive decline among individuals with heart failure, which can be addressed through non-pharmacological interventions [51, 52]. It has also been demonstrated that a combined program of aerobic exercise and cognitive training significantly improved verbal memory, self-care management, quality of life, and functional capacity in persons with heart failure [51, 53]. Thus, these findings highlights the potential effectiveness of multifaceted non-pharmacological interventions improving various aspects of well-being, with the potential to act as preventive measures against disability in later life.
Next, this study also reported that CF and depression had synergistic effects on disability incidence by three-fold greater than those who did not report either condition. A recent systematic review and meta-analysis indicated that the prevalence of CF with depression in older adults is high wherein both are mutually affected and share common physiologic processes (e.g. inflammation) and risk factors (e.g. physical inactivity) [54, 55]. Therefore, a possible pathological mechanism underlying these associations could be due to high inflammation levels, such as elevated interleukin-6 (IL-6), which impacts future adverse health problems, including the incidence of disability among older adults [56, 57]. Depressive symptoms have been identified as a significant predictor of CF incidence in previous research [13, 14], highlighting the importance of addressing depression in older individuals. Implementing interventions targeting depressive symptoms is crucial not only for mental health but also as a preventive measure against disability. Non-pharmacological interventions like psychotherapy, cognitive-behavioral therapy, and psychosocial support programs can be instrumental in treating depression among older adults [58], aiming to alleviate symptoms and enhance overall well-being, potentially reducing the risk of cognitive frailty and associated disabilities.
Among the older adults reported to have CF, diabetes mellitus demonstrated synergistic relationships with the incidence of disability. The combined effect of these two conditions is three-fold higher than these risk factors on its own, highlighting the importance of addressing the medical comorbidities in CF interventions. This is consistent with a published report that cognitive impairment and physical frailty are powerful prognostic factors in predicting disability and mortality among older adults with diabetes mellitus [59]. Metabolic and vascular dysregulation, characterized by hyperglycemia, dyslipidemia, and chronic inflammation, have been identified as the primary biological mechanisms underlying the observed synergistic relationship between diabetes and CF [60, 61]. Additionally, hypoglycemia in individuals with diabetes is linked to CF, depressive symptoms, low psychological well-being, and reduced quality of life. These factors can impede the performance of daily activities and increase the risk of disability [19]. Hence, prioritizing mental well-being through personalized care plans that include counseling, support groups, and fostering community connections is essential for improving overall resilience and quality of life among older adults confronting both cognitive frailty and diabetes mellitus.
To the best of our knowledge, this study is the first of its kind which specifically looks into the synergistic effects of individual comorbidities that co-occur with CF in Malaysian older adults on disability indices. After accounting for a broad range of confounding factors, the results of this longitudinal study shed light on the intricate and dynamic cause-and-effect relationship between the synergistic effects of CF and comorbidities on disability incidence among older adults in Malaysia. While the independent effects of CF and chronic diseases are expected, our findings are important as they highlight the multiplicative effects of co-existing CF and medical comorbidities on disability incidence. This study is not without its limitations. Firstly, data regarding the presence of comorbidities were self-reported which may be influenced by misunderstanding or inaccurate responses from the participants. However, it should be noted that self-reported disease diagnoses have been used widely and reported to be valid [29]. Secondly, it is important to note that we did not consider the interval between the initial diagnosis of comorbidities and the index date, as older adults with CF may not accurately provide this information. However, this data could have been obtained from the medical records of older adults, with prior instructions for them to bring along their medical follow-up records if available. Thirdly, the generalizability of the current findings to the general population may not be possible owing to the smaller sample size included in this analysis. Nonetheless, this study provides novel findings and can be a stepping stone for more in-depth, explorative future research undertakings. Hence, there is a need for future large-scale longitudinal studies with extended follow-up periods among older adults to validate our current findings. In future studies with a larger sample size, CF could be defined into several subtypes, and data could be stratified based on age, sex, educational levels, and regions to underscore the significance of cognitive frailty. Additionally, it is recommended that future research should prioritize interventional randomized controlled trials targeting both CF and comorbidities simultaneously as a proactive strategy to prevent, delay, or manage poor health outcomes among older adults.
Conclusions
In conclusion, the findings of our study highlights the synergistic effects of CF and comorbidities, such as OA, HD, depressive symptoms, and diabetes mellitus, heightening the risk of disability in later life. Early identification of individuals at risk for both CF and comorbidities is crucial for preventing or mitigating disability in older populations. In addition, implementing interdisciplinary interventions targeting CF and associated comorbidities can delay disability onset, emphasizing the importance of integrated care models and community-based support systems to enhance the well-being of older adults.
Data availability
The datasets generated and/or analysed during the current study are not publicly available to protect the confidentiality and anonymity of study participants but are available from the corresponding author at reasonable request.
References
World Health Organization. Noncommunicable Diseases Country Profiles. 2014 (2014). https://apps.who.int/iris/bitstream/handle/10665/128038/9789241507509_eng.pdf [Accessed March 15, 2023].
GBD 2019 Diseases and Injuries Collaborators. Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
McHugh D, Gil J. Senescence and aging: causes, consequences, and therapeutic avenues. J Cell Biol. 2018;217(1):65–77. https://doi.org/10.1083/jcb.201708092.
Fidecki W, Wysokiński M, Ochap M, Wrońska I, Przylepa K, Kulina D, et al. Selected aspects of life quality of nurses at neurological wards. JNNN. 2016;5(4):151–5. https://doi.org/10.15225/PNN.2016.5.4.4.
Song H. Risk factors for functional disability among community dwelling elderly. Korean J Health Educ Promotion. 2015;32(3):109–20. https://doi.org/10.14367/kjhep.2015.32.3.109.
Liu H, Jiao J, Zhu C, et al. Potential associated factors of functional disability in Chinese older inpatients: a multicenter cross-sectional study. BMC Geriatr. 2020;20:319. https://doi.org/10.1186/s12877-020-01738-x.
Makizako H, Shimada H, Doi T, Tsutsumimoto K, Suzuki T. Impact of physical frailty on disability in community-dwelling older adults: a prospective cohort study. BMJ open. 2015;5(9):e008462. https://doi.org/10.1136/bmjopen-2015-008462.
Shimada H, Makizako H, Doi T, Tsutsumimoto K, Lee S, Suzuki T. Cognitive impairment and disability in older Japanese adults. PLoS ONE. 2016;11(7):e0158720. https://doi.org/10.1371/journal.pone.0158720.
Kelaiditi E, Cesari M, Canevelli M, van Kan GA, Ousset PJ, Gillette-Guyonnet S, Ritz P, Duveau F, Soto ME, Provencher V, Nourhashemi F, Salvà A, Robert P, Andrieu S, Rolland Y, Touchon J, Fitten JL, Vellas B. (2013). Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. The Journal of Nutrition, Health & Aging, 17(9):726–734. https://doi.org/10.1007/s12603-013-0367-2.
St John PD, Tyas SL, Griffith LE, Menec V. The cumulative effect of frailty and cognition on mortality - results of a prospective cohort study. Int Psychogeriatr. 2017;29(4):535–43. https://doi.org/10.1017/S1041610216002088.
Feng L, Nyunt MS, Gao Q, Feng L, Lee TS, Tsoi T, Chong MS, Lim WS, Collinson S, Yap P, Yap KB, Ng TP. (2017). Physical Frailty, Cognitive Impairment, and the risk of neurocognitive disorder in the Singapore Longitudinal Ageing studies. The journals of Gerontology. Series A, Biological sciences and medical sciences, 72(3):369–75. https://doi.org/10.1093/gerona/glw050.
Esteban-Cornejo I, Cabanas-Sánchez V, Higueras-Fresnillo S, Ortega FB, Kramer AF, Rodriguez-Artalejo F, Martinez-Gomez D. (2019). Cognitive frailty and mortality in a national cohort of older adults: The role of physical activity. Mayo Clinic Proceedings, 94(7):1180–1189. https://doi.org/10.1016/j.mayocp.2018.10.027.
Rivan NFM, Shahar S, Rajab NF, Singh D, Din NC, Hazlina M, Hamid T. Cognitive frailty among Malaysian older adults: baseline findings from the LRGS TUA cohort study. Clin Interv Aging. 2019;14:1343–52. https://doi.org/10.2147/CIA.S211027.
Rivan NFM, Shahar S, Rajab NF, Singh D, Che Din N, Mahadzir H, Mohamed Sakian NI, Ishak WS, Abd Rahman MH, Mohammed Z, You YX. Incidence and predictors of cognitive Frailty among older adults: A Community-based Longitudinal Study. Int J Environ Res Public Health. 2020;17(5):1547. https://doi.org/10.3390/ijerph17051547.
Rivan NFM, Singh DKA, Shahar S, et al. Cognitive frailty is a robust predictor of falls, injuries, and disability among community-dwelling older adults. BMC Geriatr. 2021;21:593. https://doi.org/10.1186/s12877-021-02525-y.
Tang KF, Teh PL, Lee SWH. Cognitive Frailty and Functional Disability among Community-Dwelling older adults: a systematic review. Innov Aging. 2023;7(1):igad005. https://doi.org/10.1093/geroni/igad005. PMID: 36908650; PMCID: PMC9999676.
Solfrizzi V, Scafato E, Lozupone M, Seripa D, Giannini M, Sardone R, et al. Additive role of a potentially reversible cognitive frailty model and inflammatory state on the risk of disability: the Italian longitudinal study on aging. Am J Geriatr Psychiatry. 2017;25(11):1236–48.
Deng Y, Li N, Wang Y, Xiong C, Zou X. Risk factors and Prediction Nomogram of Cognitive Frailty with Diabetes in the Elderly. Diabetes Metab Syndr Obes. 2023;16:3175–85. https://doi.org/10.2147/DMSO.S426315. PMID: 37867632; PMCID: PMC10588717.
Abdelhafiz AH, Sinclair AJ. Cognitive Frailty in older people with type 2 diabetes Mellitus: the Central Role of Hypoglycaemia and the need for Prevention. Curr Diab Rep. 2019;19(4):15. https://doi.org/10.1007/s11892-019-1135-4.
Wang C, Zhang J, Hu C, Wang Y. Prevalence and risk factors for cognitive Frailty in Aging Hypertensive patients in China. Brain Sci. 2021;11(8):1018. https://doi.org/10.3390/brainsci11081018.
Faulkner KM, Uchmanowicz I, Lisiak M, Cichoń E, Cyrkot T, Szczepanowski R. Cognition and Frailty in patients with heart failure: a systematic review of the Association between Frailty and Cognitive Impairment. Front Psychiatry. 2021;12:713386. https://doi.org/10.3389/fpsyt.2021.713386. PMID: 34276454; PMCID: PMC8282927.
Sheridan PE, Mair CA, Quiñones AR. Associations between prevalent multimorbidity combinations and prospective disability and self-rated health among older adults in Europe. BMC Geriatr. 2019;19(1):198. https://doi.org/10.1186/s12877-019-1214-z.
Lu J, Guo QQ, Wang Y, Zuo ZX, Li YY. The Evolutionary Stage of Cognitive Frailty and Its Changing Characteristics in Old Adults. J Nutr Health Aging. 2021;25(4):467–478. https://doi.org/10.1007/s12603-020-1560-8. PMID: 33786564.
Shahar S, Omar A, Vanoh D, Hamid TA, Mukari SZ, Din NC, Rajab NF, Mohammed Z, Ibrahim R, Loo WH, Meramat A, Kamaruddin MZ, Bagat MF, Razali R. Approaches in methodology for population-based longitudinal study on neuroprotective model for healthy longevity (TUA) among Malaysian older adults. Aging Clin Exp Res. 2016;28(6):1089–104. https://doi.org/10.1007/s40520-015-0511-4.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol Biol Sci Med Sci. 2001;56(3):M146–56. https://doi.org/10.1093/gerona/56.3.m146.
Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–62.
Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med. 2014;275(3):214–28. https://doi.org/10.1111/joim.12190.
Lee LK, Shahar S, Chin AV, Mohd Yusoff NA, Rajab NF, Abdul Aziz S. Prevalence of gender disparities and predictors affecting the occurrence of mild cognitive impairment (MCI). Arch Gerontol Geriatr. 2012;54:185–91.
Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc. 2004;52(1):123–7. https://doi.org/10.1111/j.1532-5415.2004.52021.x.
Teh EE, Hasanah CI. (2004). Validation of malay version of geriatric Depression Scale among Elderly inpatients. Penang Hospital and School of Medical Sciences, Universiti Sains Malaysia, September 2004. Available online at: https://www.priory.com/psych/MalayGDS.htm [Accessed on March 20, 2023].
Andrews G, Kemp A, Sunderland M, Von Korff M, Ustun TB. Normative data for the 12 item WHO disability assessment schedule 2.0. PLoS ONE. 2009;4(12):1–6. https://doi.org/10.1371/journal.pone.0008343.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. https://doi.org/10.1016/0277-9536(91)90150-b.
Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. 2008;108(4):52–62.
Rothman KJ. Measuring interactions. Epidemiology: an introduction. Oxford: University; 2002. pp. 168–80.
Andersson T, Alfredsson L, Kallberg H, et al. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20:575–9.
Greenland S, Lash TL, Rothman KJ. Concepts of interaction. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia, USA: Lippincott Williams & Wilkins; 2008. pp. 71–83.
Ho C, Feng L, Fam J, et al. Coexisting medical comorbidity and depression: multiplicative effects on health outcomes in older adults. Int Psychogeriatr. 2014;26:1221–9.
Lee WJ, Peng LN, Lin CH, Lin HP, Loh CH, Chen LK. The synergic effects of frailty on disability associated with urbanization, multimorbidity, and mental health: implications for public health and medical care. Sci Rep. 2018;8(1):14125. https://doi.org/10.1038/s41598-018-32537-5.
Xiang X, An R. The impact of cognitive impairment and Comorbid Depression on disability, Health Care utilization, and costs. Psychiatr Serv. 2015;66(11):1245–8. https://doi.org/10.1176/appi.ps.201400511.
Stubbs B, Binnekade T, Eggermont L, et al. Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95:175–e879.
Stubbs B, Aluko Y, Myint PK, Smith TO. (2016). Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing, 45(2):228–35. http://www.ncbi.nlm.nih.gov/pubmed/26795974 (Accessed January 15, 2023).
Arnold CM, Faulkner RA. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007;7:17.
Lee AC, Harvey WF, Wong JB, Price LL, Han X, Chung M, Driban JB, Morgan LPK, Morgan NL, Wang C. Effects of Tai Chi versus physical therapy on mindfulness in knee osteoarthritis. Mindfulness (N Y). 2017;8(5):1195–205. https://doi.org/10.1007/s12671-017-0692-3.
Hall M, Dobson F, Van Ginckel A, Nelligan RK, Collins NJ, Smith MD, Ross MH, Smits E, Bennell KL. Comparative effectiveness of exercise programs for psychological well-being in knee osteoarthritis: a systematic review and network meta-analysis. Semin Arthritis Rheum. 2021;51(5):1023–32.
Yang GY, Hunter J, Bu FL, Hao WL, Zhang H, Wayne PM, Liu JP. Determining the safety and effectiveness of Tai Chi: a critical overview of 210 systematic reviews of controlled clinical trials. Syst Rev. 2022;11(1):260.
Rosenberg MD, Scheinost D, Greene AS, Avery EW, Kwon YH, Finn ES, Ramani R, Qiu M, Constable RT, Chun MM. Functional connectivity predicts changes in attention observed across minutes, days, and months. Proc Natl Acad Sci U S A. 2020;117(7):3797–807. https://doi.org/10.1073/pnas.1912226117. Epub 2020 Feb 4. PMID: 32019892; PMCID: PMC7035597.
Murukesu RR, Singh DKA, Shahar S, Subramaniam P. Physical activity patterns, Psychosocial Well-Being and coping strategies among older persons with cognitive Frailty of the WE-RISE trial throughout the COVID-19 Movement Control Order. Clin Interv Aging. 2021;16:415–29. PMID: 33692620; PMCID: PMC7939500.
Kucharska-Newton A, Griswold M, Yao ZH, Foraker R, Rose K, Rosamond W, Wagenknecht L, Koton S, Pompeii L, Windham BG. Cardiovascular Disease and patterns of change in functional Status over 15 years: findings from the atherosclerosis risk in communities (ARIC) Study. J Am Heart Assoc. 2017;6(3):e004144. https://doi.org/10.1161/JAHA.116.004144.
Josiak K, Jankowska EA, Piepoli MF, Banasiak W, Ponikowski P. Skeletal myopathy in patients with chronic heart failure: significance of anabolic-androgenic hormones. J Cachexia Sarcopenia Muscle. 2014;5:287–96.
Suzuki H, Matsumoto Y, Ota H, Sugimura K, Takahashi J, Ito K, et al. Hippocampal blood flow abnormality associated with depressive symptoms and cognitive impairment in patients with chronic heart failure. Circ J. 2016;80:1773–80.
Gary, R. A., Paul, S., Corwin, E., Butts, B., Miller, A. H., Hepburn, K., … Waldrop-Valverde,D. (2019). Exercise and Cognitive Training as a Strategy to Improve Neurocognitive Outcomes in Heart Failure: a pilot study. The American Journal of Geriatric Psychiatry.doi:10.1016/j.jagp.2019.01.211.
Zhao Q, Liu X, Wan X, Yu X, Cao X, Yang F, Cai Y. Non-pharmacological interventions for cognitive impairment in older adults with heart failure: a systematic review. Geriatr Nurs 2023 May-Jun;51:378–87. https://doi.org/10.1016/j.gerinurse.2023.04.008.
Gary RA, Paul S, Corwin E, Butts B, Miller AH, Hepburn K, Waldrop D. Exercise and cognitive training intervention improves Self-Care, Quality of Life and functional capacity in persons with heart failure. J Appl Gerontol. 2022;41(2):486–95. https://doi.org/10.1177/0733464820964338.
Zhou W, Zhang L, Wang T, Li Q, Jian W. Influence of social distancing on physical activity among the middle-aged to older population: evidence from the nationally representative survey in China. Front Public Health. 2022;10:958189. https://doi.org/10.3389/fpubh.2022.958189.
Gleeson M, Bishop NC, Stensel DJ, et al. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11:607–15.
Vaughan L, Corbin AL, Goveas JS. Depression and frailty in later life: a systematic review. Clin Interv Aging. 2015;10:1947–58. https://doi.org/10.2147/CIA.S69632.
Tsutsumimoto K, Doi T, Nakakubo S, Kim M, Kurita S, Ishii H, Shimada H. Cognitive Frailty as a risk factor for Incident Disability during Late Life: a 24-Month Follow-Up longitudinal study. J Nutr Health Aging. 2020;24(5):494–9. https://doi.org/10.1007/s12603-020-1365-9.
Gramaglia C, Gattoni E, Marangon D, Concina D, Grossini E, Rinaldi C, Panella M, Zeppegno P. Non-pharmacological approaches to Depressed Elderly with no or mild cognitive impairment in Long-Term Care facilities. A systematic review of the literature. Front Public Health. 2021;9:685860. https://doi.org/10.3389/fpubh.2021.685860.
Thein FS, Li Y, Nyunt MSZ, Gao Q, Wee SL, Ng TP. Physical frailty and cognitive impairment is associated with diabetes and adversely impact functional status and mortality. Postgrad Med. 2018;130(6):561–7. https://doi.org/10.1080/00325481.2018.1491779.
Feinkohl I, Price JF, Strachan MWJ, Frier BM. The impact of diabetes on cognitive decline: potential vascular, metabolic, and psychosocial risk factors. Alzheimers Res Ther. 2015;7(1):46.
Barzilay JI, Blaum C, Moore T, Xue QL, Hirsch CH, Walston JD, et al. Insulin Resistance and inflammation as precursors of Frailty. Arch Intern Med. 2007;167(7):635–41.
Acknowledgements
We would like to express our gratitude to all the co-researchers, field workers, staff, local authorities, enumerators and participants for their involvement in this study.
Funding
This work was supported by the Long-term Research Grant Scheme (LGRS) provided by the Ministry of Higher Education, Malaysia (LRGS/1/2019/ UM-UKM/1/4, LRGS/BU/2012/UKM-UKM/K/01) and Grand Challenge Grant Project 1 and Project 2 (DCP-2017-002/1, DCP-2017-002/2) and Research University Grant (GUP-2018-066) funded by Universiti Kebangsaan Malaysia.
Author information
Authors and Affiliations
Contributions
NFMR, DKAS, and SS contributed to the conception and design of the study. NFMR organized the database. NFMR and TCO performed the statistical analysis. NFMR wrote the first draft of the manuscript. PS, RR, TCO, NFR, SS, and MZAK wrote sections of the manuscript. All authors contributed to the manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval
The study has been approved by the Medical Research and Ethics Committee of the Universiti Kebangsaan Malaysia (UKM1.21.3/244/NN-2018-145) and in accordance with the Declaration of Helsinki. We verify that all procedures were conducted in compliance with applicable guidelines and regulations. All participants provided informed consent prior to participation.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fatin Malek Rivan, N., Murukesu, R., Shahar, S. et al. Synergistic effects of cognitive frailty and comorbidities on disability: a community-based longitudinal study. BMC Geriatr 24, 448 (2024). https://doi.org/10.1186/s12877-024-05057-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05057-3



