Key summary points
Multimorbidity, phenotypic prefrailty and frailty are frequent in ageing populations
AbstractSection FindingsThis long-term follow-up of home-dwelling older men reveals the relationship of phenotypic frailty to long-term prognosis, independently of the presence of significant chronic diseases and disability.
AbstractSection MessageAssessment of phenotypic frailty and already prefrailty provides extra clinical value for the assessment of prognosis in old age.
Abstract
Purpose
Multimorbidity, prefrailty, and frailty are frequent in ageing populations, but their independent relationships to long-term prognosis in home-dwelling older people are not well recognised.
Methods
In the Helsinki Businessmen Study (HBS) men with high socioeconomic status (born 1919–1934, n = 3490) have been followed-up from midlife. In 2000, multimorbidity (≥ 2 conditions), phenotypic prefrailty and frailty were determined in 1365 home-dwelling men with median age of 73 years). Disability was assessed as a possible confounder. 18-year mortality follow-up was established from registers and Cox regression used for analyses.
Results
Of the men, 433 (31.7%) were nonfrail and without multimorbidity at baseline (reference group), 500 (36.6%) and 82 (6.0%) men had prefrailty or frailty, respectively, without multimorbidity, 84 (6.2%) men had multimorbidity only, and 201 (14.7%) and 65 (4.8%) men had prefrailty or frailty together with multimorbidity. Only 30 (2.2%) and 86 (6.3%) showed signs of ADL or mobility disability. In the fully adjusted analyses (including ADL disability, mental and cognitive status) of 18-year mortality, frailty without multimorbidity (hazard ratio 1.62, 95% confidence interval 1.13–2.31) was associated with similar mortality risk than multimorbidity without frailty (1.55, 1.17–2.06). The presence of both frailty and multimorbidity indicated a strong mortality risk (2.93, 2.10–4.07).
Conclusion
Although multimorbidity is generally considered a substantial health problem, our long-term observational study emphasises that phenotypic frailty alone, independently of disability, may be associated with a similar risk, and a combination of multimorbidity and frailty is an especially strong predictor of mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multimorbidity, is an increasingly frequent condition in ageing societies although its prevalence naturally depends upon the definition of the conditions counted [1,2,3,4]. The prevalence has two sharply rises, first one around 50–60 years of age when chronic diseases start to appear, and second one in older age. Consequently, multimorbidity is gaining increasing attention, because it complicates treatment leading to greater susceptibility to failures of care delivery and co-ordination. Multimorbidity is often associated with polypharmacy predisposing to potential drug interactions, and is overall connected with impaired prognosis.
Frailty, on the other hand, is a clinical geriatric syndrome with a prevalence of 10–12% among populations aged 70 years or older, the prevalence further increasing in older age groups [5, 6]. Frailty is characterised by increased vulnerability to inner and outer stressors and is a risk factor of disability, hospitalisation and death [6, 7]. Frailty still lacks a consensus definition, but the two most frequent ways to define frailty are the phenotype method [8] and the calculation of cumulative deficits or frailty index [9].
The relationships between multimorbidity and frailty are complex, but considered multidirectional: multimorbidity predisposes to frailty and vice-versa [10,11,12,13,14,15]. Disability has also been shown to predict mortality independently of multimorbidity [16]. Consequently, the relationship between multimorbidity, frailty and mortality is quite obvious, if frailty index of cumulative deficits is used, because the definition also includes various diseases and disabilities [9]. Therefore, frailty as a phenotype is of special interest, because it is not considered a disability state [5] and offers an additional method, independently of diagnosed diseases to predict mortality and outcome risk. Because there are few long-term studies on this, we explored their relationships during a 18-year follow-up in the longitudinal Helsinki Businessmen Study (HBS) [17]. At baseline, these older men were home-dwelling with low prevalence of disability.
Material and methods
Study overview
We report a secondary analysis of the Helsinki Businessmen Study (HBS), a cohort of men born between 1919 and 1934 (original n = 3490), who have been followed-up since the 1960s [17, 18]. Their cardiovascular disease risk factor history [including body mass index (BMI)] is known since midlife (mean age 40 years). In 2000, current residential addresses were retrieved from the Population Information System of Finland for surviving HBS participants, and a questionnaire survey was sent to them. The questionnaire included items about lifestyle (smoking, alcohol consumption, physical activity), social status (married/divorced/widowed/unmarried), body mass index (BMI), medications, prevalent physician-diagnosed diseases, question about subjective memory disturbances, and health-related quality of life (HRQoL, RAND-36/SF-36 instrument [https://www.rand.org/health/surveys_tools/mos/36-item-short-form.html, also including questions about mobility and Activities of Daily Living (ADL)] [19, 20].
Study groups in 2000
There is currently no consensus definition of the frailty syndrome, and various methods can be found in the literature. In the HBS, we have defined frailty phenotype using mainly questionnaire data and according to a modification of the Cardiovascular Health Study (CHS) frailty phenotype [21]. The following criteria were used: (1) Weight loss defined as > 5% weight loss from baseline in 1974, or having current calculated BMI under 21 kg/m2 in 2000. (2) evaluation of physical weakness based on self-reported difficulty (not at all = 0) in carrying or lifting a grocery bag (one of the questions of the Physical Function scale of RAND-36). (3) assessment of exhaustion based on reported low energy most or all of the time during the preceding 4 weeks (one of the questions of the Vitality scale of RAND-36). (4) evaluation of physical activity based on a question: “do you exercise regularly weekly?” the answer “no” was taken to denote low physical activity. Responders with 3–4, 1–2, and zero criteria were classified as frail, prefrail, and nonfrail, respectively. We have earlier demonstrated prognostic validity of this modification in our cohort [21].
In the literature there is no unequivocal definition of multimorbidity either [22], often defined as the presence of 2 or more diseases or clinical conditions. In the present study, our objective was to compare the independent effects of frailty phenotype (not based on diagnosed diseases and disabilities) and clinically meaningful, diagnosed diseases on mortality. Therefore, we defined multimorbidity as the reported presence of at least 2 out of 8 important chronic disease states: coronary artery disease (chronic or history of myocardial infarction), stroke, peripheral artery disease, heart failure, chronic pulmonary disease (including asthma and chronic obstructive pulmonary disease), diabetes (type not defined, but majority likely type 2), any cancer and musculoskeletal disease (including rheumatic diseases and osteoarthritis). We intentionally did not include hypertension, because it can be considered a risk factor rather than a disease. There were few cases of reported diagnosed psychiatric disorders (n = 55) or dementia (n = 6) among responders. Therefore, we used the Mental Health domain of RAND-36 and self-report of memory disturbances (‘Have you had problems with your memory?’) as proxies to reflect psychological and cognitive status, respectively.
We studied disability as a potential confounder. Using RAND-36 items, mobility disability was defined as ‘at least a lot of difficulty in walking ½ kilometer’ or ‘at least a lot of difficulty in climbing one flight of stairs’ [23], and ADL disability was defined as ‘a lot of difficulty in bathing or dressing oneself’. Smoking was categorised as current vs ex- or never smoker or as reported number of smoking years. Current and midlife BMI was calculated from the formula: weight in kg/height in m2. Alcohol consumption (grams of ethanol per week) was derived from responses to questions about participant’s consumption of different alcohol beverages in an average week.
Outcome
Total mortality of the whole HBS cohort up to 31 March 2018 was retrieved from the Finnish Population Information System, which is a registry of all Finnish citizens. The register's assessment of vital status is reliable for people who permanently reside in Finland (over 95% of the present cohort), irrespective of whether they die in Finland or abroad. Moreover, the assessment of vital status is also quite reliable for Finnish citizens living permanently abroad.
Statistical analysis
We used descriptive statistics, Armitage test for trend in proportions, and analysis of covariance (ANCOVA) to compare the study groups. The ANCOVA analyses were adjusted for age. For follow-up, proportionality requirements were met, and we used multivariable Cox hazards regression modelling to compare 10-year and 18-year mortality in various prefrailty/frailty and multimorbidity groups and calculated hazard ratios (HR) with 95% confidence intervals (CI). Schoenfeld residuals were inspected to confirm proportional hazards assumption. The group with no prefrailty/frailty and no multimorbidity was used as the reference category and variables were used for adjustments as follows: Age (continuous variable) in model 1; besides age variables significantly different between reference category and multimorbidity in model 2 (BMI, memory disturbance, regular drug use); besides age variables significantly different between reference category and frailty in model 3 (BMI, smoking years, memory disturbance, mental health, ADL disability, regular drug use). Model 3 was also the final model because it included all previous variables for adjustment. Although mobility disability in men with frailty was significantly different from reference category, it was not used in the analyses because of overlap with the definition of the frailty phenotype definition. To estimate selection bias, we also compared mortality among those men who were alive in 2000 but did not respond to the questionnaire survey, as well as those who responded but whose frailty/multimorbidity status in 2000 could not be assessed due to incomplete data. The role of attrition bias was assessed to be negligible, because the outcome (total mortality during follow-up) was retrieved from a reliable country-wide register.
In all analyses, two-sided P values < 0.05 were taken to denote statistical significance. Statistical analyses were performed using NCSS statistical software (Kaysville, UT, www.ncss.com, version 8).
Ethical statement
The follow-up complies with the Declaration of Helsinki, the research protocol has been approved by the ethical committee of the Department of Medicine, Helsinki University Central Hospital, and informed consent has been obtained from the subjects. The study is registered as ClinicalTrials.gov identifier: NCT02526082.
Results
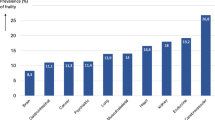
In 2000, the questionnaire was returned by 1863 men (81.5% of 2286 survivors), of them 98% were community-living with an age range from 66 to 81 years (median 74 years). Due to incomplete data in questionnaires, frailty phenotype and multimorbidity status could not be assessed in 498 men. Thus, the analytical sample consisted of 1365 men, of them 99% were community-living with an age range from 66 to 81 years (median 73 years). However, 18-year mortality follow-up was complete for all 2286 survivors in 2000. The flow chart of the study is shown in Fig. 1 and baseline data of various study groups are compared in Table 1. In the analytic sample, prevalencies of multimorbidity, prefrailty and frailty phenotype were 25.6% (n = 350), 51.4% (n = 701) and 10.8% (n = 147), respectively, while both mobility disability (6.1%, n = 83) and ADL disability (2.2%, n = 30) were less frequent.
Of the whole sample, 433 (31.7%) were nonfrail without multimorbity, 500 (36.6%) and 82 (6.0%) men had prefrailty or frailty, respectively, without multimorbidity; 84 (6.2%) men had multimorbidity only, and 201 (14.7%) and 65 (4.8%) men had prefrailty or frailty together with multimorbidity. Multimorbidity was mainly caused by cardiovascular and pulmonary diseases, cancer and diabetes, but musculoskeletal disorders were common also in men with frailty. The prevalence of hypertension was common and not statistically significantly different between the groups.
During the 18-year follow-up, 920 men died (67.4%). Unadjusted Kaplan-Maier curves for 18-year mortality in the study groups show the marked excess mortality associated with frailty phenotype with or without multimorbidity (Fig. 2). These observations were confirmed in the adjusted Cox analyses using men with no prefrailty/frailty and no multimorbidity as the reference category (Table 2).
In the final model frailty phenotype (HR 1.61, 95% CI 1.13–2.31) alone without multimorbidity was associated with similar mortality risk to multimorbidity alone (HR 1.55, 95% CI 1.17–2.06), also prefrailty alone was significant (HR 1.24, 95% CI 1.02–1.50).The presence of both frailty and multimorbidity indicated a strong mortality risk (HR 2.93, 95% CI 2.10–4.07).
In order to further separate a possible confounder, disability, from analyses, we rerun the fully adjusted analysis after excluding men with either ADL disability or mobility disability (n = 98). No prefrailty/frailty and no multimorbidity group as reference, the HRs (with 95% CI) were 1.24 (1.10–1.50), 1.57 (1.03–2.38), 1.57 (1.18–2.10), 1.56 (1.23–1.98), and 2.74 (1.86–4.03) for the prefrail or frail without multimorbidity, multimorbidity alone, and multimorbidity with prefrailty or frailty, respectively. We also analysed 18-year mortality among non-respondents (n = 423) and among those whose frailty/multimorbidity status could not be assessed in 2000 (n = 498). Mortality in these groups was similar to the average of the analytic sample (Fig. 1).
Finally, because the 18-year follow-up is very long for septuagenarian men, we also analysed HRs during the first 10 years or follow-up. In the final model with no prefrailty/frailty and no multimorbidity group as reference, the HRs (with 95% CI) were 1.42 (1.01–2.00), 1.99 (1.15–3.46), 1.78 (1.10–2.89), 2.53 (1.75–3.65), and 4.68 (2.94 to 7.43) for the prefrail or frail without multimorbidity, multimorbidity alone, and multimorbidity with prefrailty or frailty, respectively.
Discussion
Our 18-year follow-up suggests impact of both prefrailty and frailty phenotype as defined in this study on mortality risk in 70 + , community-living men, independently of chronic, clinically meaningful diseases or disability. Especially the presence of both multimorbidity and frailty phenotype was a very strong indicator of mortality risk. Although men with frailty had more memory complaints and worse general psychological health than men without frailty, the mortality results remained significant after various adjustments, also with variables related to mental and cognitive state.
Strengths and limitations
The strengths of the study include its long follow-up and reliable assessment of mortality from national registers. The response rate was also satisfactory and analyses of the mortality among non-respondents suggest that a major bias is unlikely. A further strength of this homogenous male population from the highest social strata is that socioeconomic factors are not likely to affect the results. Hazard ratios of mortality were relatively insensitive to several adjustments suggesting that residual confounding is not likely.
At the same time, the homogeneity is also an obvious limitation for generalisability. Furthermore, the cohort mainly represents functional older men, because almost all were home-dwelling and assessed proportions of ADL- or mobility disability were only 2% and 6%, respectively.
Long follow-up is also a limitation, because clinical status was defined at baseline and potential changes in frailty and morbidity status during follow-up is not known. This may lead to underestimation of relationships with mortality, which is supported by higher HRs during the 10-year vs 18-year follow-up.
Self-report of diseases is a limitation, but a recent analysis suggested that self-report of many chronic conditions can provide a reliable estimate [24], and comparison of the disease prevalencies with national statistics largely supports this. Moreover, reliability is probably better in this type of cohort with high social status.
Currently there is no consensus definition of frailty, and various modifications of the CHS frailty phenotype [8] have been used in different studies. For our modification, prognostic validation has been shown earlier [21]. Moreover, questionnaire data without clinical strength measurement have also been used to define frailty in other cohorts. The simplified Women's Health Initiative (sWHI) frailty score, for example, showed high correlations with the standard CHS frailty phenotype [25]. Whether weight loss in our cohort was intentional or unintentional is not known.
Assessment of cognitive and mental status were also based on self-report. However, the RAND-36 Mental Health domain has been used to determine the presence of general psychological disorder [26], and its score was significantly lower among those who reported mental disorder. Although self-reported memory disturbance alone is not sufficient for general screening of dementia, its presence in 2000 significantly predicted incident dementia during a 14-year follow-up (unpublished observation, types of dementia were certified from death certificates as described in Ref. [27]).
A final limitation is that in an observational study causal inferences cannot be made.
Comparison to previous studies
Multimorbidity has received a lot of attention during the last decade for several reasons. It has suggested to be more than the sum of its parts, it leads to polypharmacy and complicated care with possibilities of adverse effects, and may predispose to intervening diseases like infections. Accordingly, it is considered to be a major burden for healthcare in ageing societies. Because various definitions of multimorbidity can also include conditions of less serious nature [22], in the present study we chose to include only clinically meaningful chronic diseases, such as major cardiovascular- and cerebrovascular disease, diabetes, chronic pulmonary disease, cancer, and musculoskeletal disease including rheumatic diseases and osteoarthritis.
Disability has been shown to exert a higher mortality risk than multimorbidity in an older population with frequent (32%) prevalence of disability [16]. In the present study we specifically wished to evaluate the independent and clinically meaningful effect of the concept of frailty over traditional diseases and also disabilities on prognosis. Therefore, we defined frailty as a phenotype, not as cumulative deficits which usually include also diagnosed diseases and disabilities. In addition, we assessed the impact of prefrailty, which is a less homogenous and more controversial condition and with a potential of reversal to non-frailty [28]. Our findings from this long follow-up show that prefrailty alone has prognostic significance, suggesting that it could be considered as an earlier target of prevention. Indeed, it is surprising that according to cumulative hazard function the effect of prefrailty on mortality appears to be similar to multimorbidity at least for the first 12–15 years of follow-up (Fig. 2). The combination of prefrailty and multimorbidity conferred a stronger mortality risk.
What may be the reason for quite moderate effect of multimorbidity (without frailty) on mortality prognosis in our cohort? Many of the diseases included are nevertheless frequent causes of death. The participants had high socioeconomic status and can be seen as a population subgroup nested within the Finnish population at large. They may represent a group which is likely to be treated early, to have high adherence to treatments and a better prognosis for chronic conditions than the general population. For example, almost half of the of the responding men were using statins in the 2015 survey when median age was 85 years [29], and statin treatment has been shown to improve prognosis also in old age [30]. On the other hand, frailty alone does not necessarily lead to medical treatments, although it is possible that frail men have subclinical disease worsening their prognosis. Midlife CVD risk factors have been shown to associate with development of frailty [31]. In geriatrics, polypharmacy is often seen as a general threat, but further research is clearly warranted of the effects of specific drugs on prognosis. We are presently conducting detailed analyses of long-term drug effects in the HBS cohort.
To conclude: Although multimorbidity is generally considered a substantial health problem, our long-term observational study emphasises that frailty phenotype alone may confer a higher risk, and a combination of multimorbidity and frailty is an especially strong predictor of mortality. The results highlight identification of frailty and potentially also prefrailty as a clinically meaningful and feasible method to more effectively assess patient prognosis at older ages.
References
Tinetti ME, Fried TR, Boyd CM (2012) Designing health care for the most common chronic condition–multimorbidity. JAMA 307:2493–2494. https://doi.org/10.1001/jama.2012.5265
Rocca WA, Boyd CM, Grossardt BR, Bobo WV, Finney Rutten LJ, Roger VL et al (2014) Prevalence of multimorbidity in a geographically defined American population: patterns by age, sex, and race/ethnicity. Mayo Clin Proc 89:1336–1349. https://doi.org/10.1016/j.mayocp.2014.07.010
Forman DE, Maurer MS, Boyd C, Brindis R, Salive ME, Horne FM et al (2018) Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol 71(19):2149–2161. https://doi.org/10.1016/j.jacc.2018.03.022
Tran J, Norton R, Conrad N, Rahimian F, Canoy D, Nazarzadeh M et al (2018) Patterns and temporal trends of comorbidity among adult patients with incident cardiovascular disease in the UK between 2000 and 2014: A population-based cohort study. PLoS Med 15(3):e1002513. https://doi.org/10.1371/journal.pmed.1002513
Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-Mañas L, Fried LP et al (2019) Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging 23:771–787. https://doi.org/10.1007/s12603-019-1273-z
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP (2019) Frailty: implications for clinical practice and public health. Lancet 394:1365–1375. https://doi.org/10.1016/S0140-6736(19)31786-
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD (2019) Management of frailty: opportunities, challenges, and future directions. Lancet 394:1376–1386. https://doi.org/10.1016/S0140-6736(19)31785-4
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Cardiovascular Health Study Collaborative Research Group et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:146–156
Rockwood K, Mitnitski A (2007) Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 62:722–727
Woo J, Leung J (2014) Multi-morbidity, dependency, and frailty singly or in combination have different impact on health outcomes. Age 36:923–931
Jackson CA, Jones M, Tooth L, Mishra GD, Byles J, Dobson A (2015) Multimorbidity patterns are differentially associated with functional ability and decline in a longitudinal cohort of older women. Age Ageing 44:810–816
Aarts S, Patel KV, Garcia ME, Van den Akker M, Verhey FR, Metsemakers JF et al (2015) Co-presence of multimorbidity and disability with frailty: an examination of heterogeneity in the frail older population. J Frailty Aging 4:131–138. https://doi.org/10.14283/jfa.2015.45
Villacampa-Fernández P, Navarro-Pardo E, Tarín JJ, Cano A (2017) Frailty and multimorbidity: two related yet different concepts. Maturitas 95:31–35
Cesari M, Perez-Zepeda MU, Marzetti E (2017) Frailty and multimorbidy: different ways of thinking about geriatrics. JAMDA 18:361–364
Espinoza SE, Quiben M, Hazuda HP (2018) Distinguishing comorbidity, disability, and frailty. Curr Geriatr Rep 7:201–209
Landi F, Liperoti R, Russo A, Capoluongo E, Barillaro C, Pahor M et al (2010) Disability, more than multimorbidity, was predictive of mortality among older persons aged 80 years and older. J Clin Epidemiol 63(7):752–759
Strandberg TE, Salomaa V, Strandberg AY, Vanhanen H, Sarna S, Pitkälä K et al (2016) Cohort Profile: The Helsinki Businessmen Study (HBS). Int J Epidemiol 45:1074–1074h
Huohvanainen E, Strandberg AY, Stenholm S, Pitkälä KH, Tilvis RS, Strandberg TE (2016) Association of self-rated health in midlife with mortality and old age frailty: a 26-year follow-up of initially healthy men. J Gerontol A Biol Sci Med Sci 71:923–928
Hays RD, Morales LS (2001) The RAND-36 measure of health-related quality of life. Ann Med 33:350–357
Aalto AM, Aro AR, Teperi J (1999) RAND-36 as a measure of health-related quality of life. Reliability, construct validity and reference values in the Finnish general population. Helsinki, Finland: Stakes, Research Reports; No. 101
Sirola J, Pitkala KH, Tilvis RS, Miettinen TA, Strandberg TE (2011) Definition of frailty in older men according to questionnaire data (RAND-36/SF-36): The Helsinki Businessmen Study. J Nutr Health Aging 15:783
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M (2009) Defining comorbidity: implications for understanding health and health services. Ann Fam Med 7:357–363. https://doi.org/10.1370/afm.983
Chaudhry SI, McAvay G, Ning Y, Allore HG, Newman AB, Gill TM (2010) Geriatric impairments and disability: the Cardiovascular Health Study. J Am Geriatr Soc 58:1686–1692
Najafi F, Moradinazar M, Hamzeh B, Rezaeian S (2019) The reliability of self-reporting chronic diseases: how reliable is the result of population-based cohort studies. J Prev Med Hyg 60:E349–E353. https://doi.org/10.15167/2421-4248/jpmh2019.60.4.1118
Zaslavsky O, Zelber-Sagi S, LaCroix AZ, Brunner RL, Wallace RB, Cochrane BB et al (2017) Comparison of the simplified sWHI and the standard CHS frailty phenotypes for prediction of mortality, incident falls, and hip fractures in older women. J Gerontol A Biol Sci Med Sci 72:1394–1400
Pfoh ER, Chan KS, Dinglas VD, Cuthbertson BH, Elliott D, Porter R et al (2016) The SF-36 offers a strong measure of mental health symptoms in survivors of acute respiratory failure: a tri-national analysis. Ann Am Thorac Soc 13:1343–1350
Rantanen K, Strandberg AY, Salomaa V, Pitkälä K, Tilvis RS, Tienari P et al (2017) Cardiovascular risk factors and glucose tolerance in midlife and risk of cognitive disorders in old age up to a 49-year follow-up of the Helsinki Businessmen Study. Ann Med 49(6):462–469
Romero-Ortuno R, Scarlett S, O’Halloran AM, Kenny RA (2019) Is phenotypical prefrailty all the same? A longitudinal investigation of two prefrailty subtypes in TILDA. Age Ageing 49:39–45. https://doi.org/10.1093/ageing/afz129
Strandberg TE, Urtamo A, Kähärä J, Strandberg AY, Pitkälä KH, Kautiainen H (2018) Statin treatment is associated with a neutral effect on health-related quality of life among community-dwelling octogenarian men: the Helsinki Businessmen Study. J Gerontol A Biol Sci Med Sci 73:1418–1423. https://doi.org/10.1093/gerona/gly073
Gencer B, Marston NA, Im KA, Cannon CP, Sever P, Keech A et al (2020) Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet 396:1637–1643
Strandberg TE, Sirola J, Pitkälä KH, Tilvis RS, Strandberg AY, Stenholm S (2012) Association of midlife obesity and cardiovascular risk with old age frailty: a 26-year follow-up of initially healthy men. Int J Obes (Lond) 36:1153–1157. https://doi.org/10.1038/ijo.2012.8
Acknowledgements
This work was supported by VTR-funding of the Helsinki University Hospital (TYH 2014245; 2015211); and the Academy of Finland (grant number 311492). MK was additionally supported by the US National Institute on Aging, National Institutes of Health (NIH, R01AG056477), the UK Medical Research Council (MR/S011676/1), NordForsk (75021), and Finnish Work Environment Fund (190424). The sponsors had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Funding
Open access funding provided by University of Helsinki including Helsinki University Central Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TES reports various cooperation (educational, research, consultation) with several companies including Amgen, Boehringer, Merck, OrionPharma, Servier, and Zora. Other authors declare no conflict of interest related to this paper.
Ethical approval
The follow-up complies with the Declaration of Helsinki, the research protocol has been approved by the ethical committee of the Department of Medicine, Helsinki University Central Hospital.
Informed consent
Informed consent has been obtained from the subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Strandberg, T.E., Lindström, L., Jyväkorpi, S. et al. Phenotypic frailty and multimorbidity are independent 18-year mortality risk indicators in older men. Eur Geriatr Med 12, 953–961 (2021). https://doi.org/10.1007/s41999-021-00472-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00472-w