Abstract
Background
Physical activity (PA) plays an important role in the process of several chronic diseases. It may be also associated with the incidence of sarcopenia. This study aimed to determine the association of PA from different components including frequency, duration, intensity, and volume with the incidence of sarcopenia in middle-aged and older adults.
Methods
This study used data from the China Health and Retirement Longitudinal Study in 2011 and 2015. A total of 3,760 individuals aged ≥ 40 years were involved in this study. Sarcopenia was diagnosed using muscle mass, strength and physical performance according to the Asian Working Group for Sarcopenia. PA information including frequency, duration, intensity, and volume was obtained by a self-reported questionnaire. Logistic regression analysis was employed to examine the association between PA and the incidence of sarcopenia at 4-year follow-up.
Results
The incidence of sarcopenia was 5.9% during the 4-year follow-up. Compared to sedentary individuals, those taking 1–2 days or more per week, or a minimum of 10 min each time on vigorous-intensity PA (VPA) had a lower incidence of sarcopenia. Adults spending 3 days or more each week, a minimum of 30 min each time, or 150 min or more per week on moderate-intensity PA (MPA) had a lower presence of sarcopenia than sedentary adults. Adults taking 3 days or more per week, at least 30 min each time, or 150 min or more each week on light-intensity PA (LPA) tended to have a lower incidence of sarcopenia than sedentary individuals. Sensitivity analyses confirmed the robustness of the findings after removing persons with hypertension, dyslipidemia, or diabetes.
Conclusions
These findings suggest that the frequency, duration, and volume of VPA or MPA are negatively associated with the presence of sarcopenia. Participation in LPA tends to have a lower incidence of sarcopenia in middle-aged and older adults.
Similar content being viewed by others
Introduction
Sarcopenia is a growing public health issue around the world. Sarcopenia is a common geriatric condition that is defined by an age-related loss of skeletal muscle mass, a drop in muscle strength and physical performance [1]. A previous study found that around the age of 40, muscle mass begins to diminish at a rate of 8% every decade [2]. Muscle strength and function are generally decreased alongside reductions in muscle mass. However, the decrease of muscle strength is far faster than the reduction of muscle mass [3]. Through a number of working group definitions, including the most recent one from the Asian Working Group on Sarcopenia in 2019 (AWGS 2019) [4], the definition of sarcopenia, which was formerly based on muscle mass loss, has been modified to highlight the deterioration in muscle strength and physical performance. A growing body of studies indicated that sarcopenia is linked to a range of adverse health outcomes, including frailty, functional disability, fractures, falls, morbidity, and mortality [5,6,7]. Sarcopenia poses a substantial impediment to healthy aging. As a result, it is critical to identify treatment targets for sarcopenia in order to avoid or delay its onset.
Inadequate physical activity (PA) is viewed as a primary contributor to sarcopenia. In a study of 162 older people between the ages of 60 and 80, Gianoudis et al. [8] discovered that spending more sedentary time is linked to a higher likelihood of sarcopenia, with the likelihood rising by 33% for every additional hour of sedentary behavior. Westbury and colleagues [9] indicated that older adults who engage in moderate-to-vigorous-intensity PA (MVPA) have a faster walking speed, a lower level of obesity, and a reduced chance of sarcopenia than those who engage in low-intensity PA (LPA). Physical exercise, especially resistance exercise can increase muscle mass and strength, as well as cardiovascular function and physical performance according to a range of studies [10,11,12], which can prevent or delay the development of sarcopenia in middle-aged and older adults.
PA is made up of four major components: frequency, duration, intensity, and weekly volume. There are specific guidelines on PA from a number of organizations. For example, the World Health Organization [13] recommends that older persons engage in 75 min or more per week of vigorous-intensity PA (VPA), 150 min or more per week of MPA, or an equivalent combination of MVP and VPA; the American College of Sports Medicine [14] further recommends that healthy individuals engage in at least 20 min per week of VPA each day on three different days, or at least 30 min per week of MPA on five different days. To the best of our knowledge, despite multiple publications on the link between PA, sarcopenia, and possible sarcopenia in middle-aged and older adults [15,16,17], the majority of previous studies used a cross-sectional design. Therefore, a longitudinal investigation is needed to determine the relationship between PA and sarcopenia. Moreover, to date, no research has investigated the association by taking into account all the four PA components such as frequency, duration, intensity, and weekly volume.
Thus, the aim of this prospective study was to explore the association of PA from different components including frequency, duration, intensity, and volume with the incidence of sarcopenia in middle-aged and older adults, using data from a national representative population-based sample in China.
Materials and methods
Study setting and participants
The data for this study came from the first and third waves of the China Health and Retirement Longitudinal Study (CHARLS), which were conducted in 2011 and 2015. The CHARLS survey aims to collect high-quality information on the demographic characteristics of non-institutionalized Chinese people in their middle and older years, as well as details on their families, health and functioning, lifestyle behaviors, health care, and employment and retirement. Detailed information regarding the CHARLS, as well as a description of its methodology, can be obtained on the official website (http://charls.pku.edu.cn/) and in published papers [18, 19].
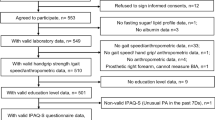
In the first wave of the survey in 2011, a total of 13,539 community-dwelling adults aged ≥ 40 years were enrolled. We removed 8,414 people for the following reasons: (a) without PA information (n = 6,773); (b) incomplete or missing data for defining sarcopenia (n = 1,108); (c) having sarcopenia at baseline (n = 533). There were in total 5,125 participants who did not have sarcopenia in the final study population. The third wave was conducted in 2015, nearly 4 years after the first wave. The exclusion criteria were as follows: (a) without follow-up data (n = 738); and (b) incomplete or missing data for defining sarcopenia (n = 627). Consequently, a total of 3,760 middle-aged and older people aged from 40 to 94 years were included in the final analysis (Fig. 1). To assess the potential selection bias caused by missing data, variables such as age, gender, education levels, smoking status, and hypertension were chosen to compare the observed data group and the missing data group (Additional file 1).
Assessment of PA
A modified version of the International Physical Activity Questionnaire (IPAQ) Short Form (Additional file 2) was used to measure PA. The modified questionnaire was structured and described similarly to the IPAQ. Previous studies have confirmed the validity and reliability of the IPAQ [20,21,22]. The procedure for evaluating the PA in our study was as follows: First, individuals were questioned about whether they had engaged in the intensity of PA for at least 10 min during a usual week continuously. The intensity of PA was specified as follows: (a) VPA: activities such as heavy lifting, digging, plowing, fast bicycling, cycling with a heavy load, and aerobics are examples of activities that cause a person to breathe much harder than usual; (b) MPA: activities such as carrying light loads, bicycling at a regular pace, and mopping the floor are examples of activities that cause a person to breathe somewhat harder than usual; (c) LPA: activities include walking at home or work, walking to get from one place to another, and any other walking done exclusively for sport, exercise, recreation or leisure. If the answer was “yes”, the participants were next asked how often (days/week, d/w) and how long (minutes/day, min/d) they engaged in the intensity of PA. The frequency of PA ranged from 0 to 7 d/w and was divided into three categories: sedentary, 1–2 d/w, and ≥ 3 d/w. The duration of PA was also divided into three scales: sedentary, 10–29 min/d, and ≥ 30–119 min/d. The weekly volume (minutes/week, min/w) of VPA/MPA/LPA was calculated using the following equation: Volume of VPA/MPA/LPA = Frequency of VPA/MPA/LPA × Duration of VPA/MPA/LPA. The weekly volume of VPA/MPA/LPA was divided into three groups: sedentary, < 150 min/w, and ≥ 150 min/w.
Diagnosis of sarcopenia
Sarcopenia was identified using a combination of the loss of muscle mass and the deterioration in muscle strength or physical performance based on the AWGS 2019 criteria [4]. Sarcopenia was assessed in our study by measuring appendicular skeletal muscle mass (ASMM), muscle strength, and physical function. To calculate the ASMM, we employed an anthropometric equation for the Chinese population that had previously been validated. A previous study has found strong agreement between the dual X-ray absorptiometry and the anthropometric equation [23]. ASMM can be calculated from the following anthropometric equation: ASMM = 0.193 × body weight (kg) + 0.107 × body height (cm) − 4.157 × gender (male = 1, female = 2) − 0.037 × age (years) − 2.631. We adjusted the ASMM by dividing it by the square of height (ASMM/Height2), as in earlier research [24]. We utilized the sex-specific lowest 20% of the ASMM/Height2 as the cut-off to determine the low muscle mass, which was 8.02 kg/m2 for males and 6.46 kg/m2 for females. Measures of muscle strength and physical performance included the 5-time chair stand test and handgrip strength, respectively. According to the AWGS 2019, we classified low physical performance as a time of ≥ 12 s for completing the 5-time chair stand test, and low muscle mass as handgrip strength of < 28 kg for males and < 18 kg for females. The measurement protocols for the 5-time chair stand test and handgrip strength can be found in our previous publications [18, 25].
Potential covariates
Our study’s covariates, which were chosen based on published papers [25,26,27], included sociodemographic characteristics, lifestyle-related factors, and health-related variables. The sociodemographic characteristics included age (40–49, 50–59, 60–69, and ≥ 70 years), gender (male and female), education levels (illiteracy, ≤primary school, middle school, and ≥ high school), and marital status (married and living with spouse, widowed, and others). Lifestyle-related factors encompassed alcohol drinking frequency (> 1/month, ≤1/month, and never drank) and smoking status (current smokers, former smokers, and never smoked). Health-related variables covered major chronic diseases (e.g., hypertension, dyslipidemia, and diabetes).
Statistical analysis
The study participants’ characteristics were reported as numbers with percentages. To compare these characteristics between the non-sarcopenia and sarcopenia groups, we performed Chi-square tests. The incidence of sarcopenia at the follow-up years was investigated using logistic regression analysis, both with and without adjusting for age, gender, education levels, marital status, alcohol consumption frequency, smoking status, hypertension, dyslipidemia, and diabetes. In the logistic regression analysis, each VPA, MPA, and LPA used “sedentary” (no activity) as the reference group. The odds ratios (OR) and 95% confidence intervals (CI) were computed. We ran sensitivity analyses for major chronic disease-free participants, excluding people with hypertension, dyslipidemia, or diabetes, to confirm the robustness of our findings. In our study, Chi-square tests and logistic regression analyses were performed using SPSS Statistics version 26.0 (IBM Corp., Chicago, IL, USA).
Results
The final analysis included 3,760 participants, and 221 of them had sarcopenia, with an incidence of 5.9% at 4-year follow-up. Table 1 depicts the differences in sociodemographic characteristics, lifestyle-related factors, and health-related variables between the non-sarcopenia and sarcopenia groups at the first wave. Compared to those without sarcopenia at baseline, those with new-onset sarcopenia are more likely to be older (28.9% vs. 42.1% for 60–69 years, 9.0% vs. 34.4% for ≥ 70 years, p < 0.001), widowed (8.1% vs. 17.2%, p < 0.001), and illiterate (26.2% vs. 41.2%, p < 0.001). However, we did not find significant differences in smoking status, alcohol consumption frequency, and major chronic diseases between the non-sarcopenia and sarcopenia groups.
Regarding PA frequency, it was found that taking 1–2 d/w or more (OR: 0.30, 95% CI: 0.10–0.88 for 1–2 d/w; OR: 0.45, 95% CI: 0.27–0.73 for ≥ 3 d/w) on VPA, or taking ≥ 3 d/w (OR: 0.59, 95% CI: 0.38–0.92) on MPA was negatively associated with the incidence of sarcopenia, even after adjustment with covariates. Spending ≥ 3 d/w (OR: 0.66, 95% CI: 0.43–1.01) on LPA tended to have a lower incidence of sarcopenia (Table 2). In terms of PA duration, we noticed that taking 10–29 min/d or more (OR: 0.39, 95% CI: 0.16–0.95 for 10–29 min/d; OR: 0.46, 95% CI: 0.28–0.74 for ≥ 30 min/d) on VPA, or spending ≥ 30 min/d (OR: 0.60, 95% CI: 0.38–0.93) on MPA was negatively associated with the progression of sarcopenia after adjustments. Taking ≥ 30 min/d (OR: 0.67, 95% CI: 0.43–1.03) on LPA tended to have a lower presence of sarcopenia (Table 3). When it comes to PA volume, we observed that taking < 150 min/w (OR: 0.48, 95% CI: 0.25–0.94) or ≥ 150 min/w (OR: 0.42, 95% CI: 0.25–0.69) on VPA, or taking ≥ 150 min/w (OR: 0.59, 95% CI: 0.38–0.92) on MPA was negatively associated with the presence of sarcopenia after adjustments. Spending ≥ 150 min/w (OR: 0.62, 95% CI: 0.43–1.02) on LPA tended to have a lower incidence of sarcopenia (Table 4).
We conducted sensitivity analyses for participants without major chronic diseases by excluding those who had diabetes, dyslipidemia, or hypertension (Additional file 3). The findings of the sensitivity analyses, which reveal an association between PA volume and the progression of sarcopenia, were found to be similar to the findings in Table 4.
Discussion
To our knowledge, this is the first longitudinal study to determine the association of PA from different components including intensity, frequency, duration, and weekly volume with the progression of sarcopenia. Results indicated that the incidence of sarcopenia was 5.9% during the period between baseline and 4-year follow-up. Compared to sedentary individuals, those taking 1–2 days or more per week, or a minimum of 10 min each time on VPA had a lower incidence of sarcopenia. Adults spending 3 days or more each week, a minimum of 30 min each time, or 150 min or more per week on MPA had a lower presence of sarcopenia than sedentary adults. Adults taking 3 days or more per week, at least 30 min each time, or 150 min or more each week on LPA were inclined to have a lower incidence of sarcopenia than sedentary individuals.
Sarcopenia was shown to have a 5.9% incidence between baseline and the 4-year follow-up, according to the current study. The finding is comparable with earlier prospective studies, which found that sarcopenia incidence was 1.14% annually among the older population in English [28] and 1.06% annually among older persons living in communities in Japan [29]. In a population of 65 years of age and older, Yu and colleagues [30] observed a 4-year incidence of the proportion of 7.8% sarcopenia. Additionally, we did not find significant differences in the incidence of sarcopenia between genders in our study, which is consistent with a previous study that found no statistical differences in the prevalence of sarcopenia between males and females in the Vietnamese population [31].
Previous research has shown an association between MVPA and sarcopenia or its components. Marini et al. [32] performed a cross-sectional study to examine the role of PA level and sitting time as predictors of sarcopenia odds, discovering that time spent in MPA can prevent sarcopenia in community-dwelling older women. By using accelerometers to measure PA to explore its association with sarcopenia, Scott and colleagues [33] discovered that regardless of the length of amounts or bouts of sedentary behavior, a greater level of MVPA is consistently associated with a lower risk of sarcopenia and its components. A longitudinal study conducted by Mijnarends et al. [34] showed that although MVPA does not affect the rate of decline in muscle mass and function, it can delay the presence of sarcopenia in adults aged 66–93 years. Our findings support these previous results but additionally show what frequency, duration, and weekly volume of MVPA may decrease the incidence of sarcopenia in middle-aged and older adults. Specifically, spending 3 days or more each week, a minimum of 30 min each time, or 150 min or more each week on MPA, or taking 1–2 days or more each week, a minimum of 10 min each time, or 10–149 min or more each week on VPA associated with a lower incidence of sarcopenia. Compared to only providing information about PA intensity like previous studies, our study’s specific recommendation including PA intensity, frequency, duration, and weekly volume may be more practicable in preventing or treating sarcopenia.
It has been reported that not only MVPA, but LPA is also associated with a lower rate of sarcopenia or decreased sarcopenia risk such as low muscle mass, strength, and physical performance [25, 35,36,37]. However, there have also been previous studies suggesting that no significant relationship exists between LPA and sarcopenia in middle-aged and older individuals [33, 38, 39]. In the present study, although no statistical significance was detected, we observed that individuals taking 3 days or more per week, a minimum of 30 min each time, or 150 min or more per week on LPA were inclined to have a lower incidence of sarcopenia than sedentary adults. Additionally, it should be emphasized that LPA has been demonstrated to affect a range of health outcomes, including cognitive health, cardiovascular diseases, and mortality [40, 41]. Based on the above results, we believe that it may be helpful to increase LPA to prevent and treat sarcopenia and other chronic conditions, especially for older adults who have difficulty participating in MVPA.
PA plays an important role in the process of various chronic diseases. The findings of the present study suggest that increasing VPA or MPA may benefit in the prevention of sarcopenia. Resistance training may be useful in achieving this goal since it can successfully improve muscle mass, strength, and physical function, thereby decreasing the risk of sarcopenia [42,43,44]. In light of these, practitioners should be aware of the relationship between MVPA and sarcopenia and consider formulating resistance training strategies for sedentary people or those who only participate in LPA to aid in sarcopenia prevention. Future research should examine the PA-sarcopenia mechanism, as well as whether increasing MVPA for sedentary people or those who only take part in LPA can lead to a lower risk of sarcopenia onset.
The current study had some drawbacks. First, a modified version of IPAQ was used to gather data on PA rather than objective tools. A previous study has shown that when compared to objective PA measuring tools like accelerometers, the subjective IPAQ overrates levels of PA [45]. Moreover, the modified version of IPAQ defined LPA as activities such as walking at home or work, walking to get from one place to another, and any other walking done exclusively for sport, exercise, recreation or leisure. The definition might cause participants to misclassify brisk walking during sport and exercise that belongs to MVPA as LPA to some extent. Third, despite controlling for a range of relevant covariates, our study did not control for other potential factors such as dietary status and nutritional supplements, which could influence the relationship between PA and sarcopenia. Fourth, rather than using dual X-ray absorptiometry or bioelectrical impedance analysis to assess muscle mass, we used an anthropometric equation that had previously been validated in the Chinese population [23]. Fifth, the 4-year follow-up in our study was a relatively short period, which could have led to a minimal change in health status during the short observation period. Finally, more than half of the participants (8,414 of 13,539) were eliminated due to missing data at baseline, which might cause some selection bias. However, sensitivity analyses confirmed the findings’ robustness after excluding individuals with hypertension, dyslipidemia, or diabetes.
Conclusions
In summary, the current study indicated that the incidence of sarcopenia was 5.9% during the period between baseline and 4-year follow-up. We found that individuals taking 1–2 days or more each week, a minimum of 10 min each time, or 10–149 min or more each week on VPA had a lower incidence of sarcopenia than sedentary persons; adults spending 3 days or more each week, a minimum of 30 min each time, or 150 min or more each week on MPA had a lower incidence of sarcopenia when compared to sedentary people; adults taking 3 days or more per week, at least 30 min each time, or 150 min or more per week on LPA were inclined to have a lower incidence of sarcopenia from baseline to 4-year follow-up.
These findings suggest that the frequency, duration, and volume of VPA or MPA are negatively associated with the presence of sarcopenia. Participation in LPA tends to have a lower incidence of sarcopenia in middle-aged and older adults.
Data availability
The data that support the findings of this study are available in Peking University Open Research Data at http://charls.pku.edu.cn/en/index.htm.
Abbreviations
- ASMM:
-
Appendicular Skeletal Muscle Mass
- AWGS:
-
Asian Working Group on Sarcopenia
- CHARLS:
-
China Health and Retirement Longitudinal Study
- CI:
-
Confidence Intervals
- IPAQ:
-
International Physical Activity Questionnaire
- LPA:
-
Light-intensity Physical Activity
- MPA:
-
Moderate-intensity Physical Activity
- MVPA:
-
Moderate-to-Vigorous-intensity Physical Activity
- OR:
-
Odds Ratios
- PA:
-
Physical Activity
- VPA:
-
Vigorous-intensity Physical Activity
References
Sayer AA, Cruz-Jentoft A. Sarcopenia definition, diagnosis and treatment: consensus is growing. Age Ageing. 2022;51(10):afac220. https://doi.org/10.1093/ageing/afac220.
Rier HN, Jager A, Sleijfer S, Maier AB, Levin MD. The prevalence and prognostic value of low muscle mass in cancer patients: a review of the literature. Oncologist. 2016;21(11):1396–409. https://doi.org/10.1634/theoncologist.2016-0066.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on Sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56. https://doi.org/10.1016/j.jamda.2011.01.003.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian working group for Sarcopenia: 2019 consensus update on Sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–e72. https://doi.org/10.1016/j.jamda.2019.12.012.
Batsis JA, Haudenschild C, Crow RS, Gilliam M, Mackenzie TA. Sarcopenia definition outcome consortium - defined weakness and risk of falls: the National Health and Aging trends Survey. Geriatr Gerontol Int. 2023;23(3):213–20. https://doi.org/10.1111/ggi.14548.
Pereira CC, Pagotto V, de Oliveira C, Silveira EA. Sarcopenia and mortality risk in community-dwelling Brazilian older adults. Sci Rep. 2022;12(1):17531. https://doi.org/10.1038/s41598-022-22153-9.
Zhao X, Zhang H, Yu J, Wang J. Association of possible sarcopenia with major chronic diseases and multimorbidity among middle-aged and older adults: findings from a national cross-sectional study in China. Geriatr Gerontol Int. 2023;23(12):925–31. https://doi.org/10.1111/ggi.14720.
Gianoudis J, Bailey CA, Daly RM. Associations between sedentary behaviour and body composition, muscle function and sarcopenia in community-dwelling older adults. Osteoporos Int. 2015;26(2):571–9. https://doi.org/10.1007/s00198-014-2895-y.
Westbury LD, Dodds RM, Syddall HE, Baczynska AM, Shaw SC, Dennison EM, et al. Associations between objectively measured physical activity, body composition and sarcopenia: findings from the hertfordshire Sarcopenia study (HSS). Calcif Tissue Int. 2018;103(3):237–45. https://doi.org/10.1007/s00223-018-0413-5.
van Waart H, Stuiver MM, van Harten WH, Geleijn E, Kieffer JM, Buffart LM, et al. Effect of low-intensity physical activity and moderate- to high-intensity physical exercise during adjuvant chemotherapy on physical fitness, fatigue, and chemotherapy completion rates: results of the PACES randomized clinical trial. J Clin Oncol. 2015;33(17):1918–27. https://doi.org/10.1200/jco.2014.59.1081.
Eriksen CS, Garde E, Reislev NL, Wimmelmann CL, Bieler T, Ziegler AK, et al. Physical activity as intervention for age-related loss of muscle mass and function: protocol for a randomised controlled trial (the LISA study). BMJ Open. 2016;6(12):e012951. https://doi.org/10.1136/bmjopen-2016-012951.
Martín-Valero R, Cuesta-Vargas AI, Labajos-Manzanares MT. Effectiveness of the physical activity promotion programme on the quality of life and the cardiopulmonary function for inactive people: randomized controlled trial. BMC Public Health. 2013;13:127. https://doi.org/10.1186/1471-2458-13-127.
World Health Organization. Physical activity. 2022 [cited 2023 September 28]. Available from: https://www.who.int/initiatives/behealthy/physical-activity.
American College of Sports Medicine. Trending topic| Physical activity guidelines. 2022 [cited 2023 September 28]. Available from: https://www.acsm.org/education-resources/trending-topics-resources/physical-activity-guidelines.
Jacob L, Gyasi RM, Oh H, Smith L, Kostev K, López Sánchez GF, et al. Leisure-time physical activity and sarcopenia among older adults from low- and middle-income countries. J Cachexia Sarcopenia Muscle. 2023;14(2):1130–8. https://doi.org/10.1002/jcsm.13215.
Kitamura M, Izawa KP, Ishihara K, Matsuda H, Okamura S, Fujioka K. Physical activity and Sarcopenia in community-dwelling older adults with long-term care insurance. Eur J Investig Health Psychol Educ. 2021;11(4):1610–8. https://doi.org/10.3390/ejihpe11040114.
Ko YC, Chie WC, Wu TY, Ho CY, Yu WR. A cross-sectional study about the relationship between physical activity and Sarcopenia in Taiwanese older adults. Sci Rep. 2021;11(1):11488. https://doi.org/10.1038/s41598-021-90869-1.
Zhao X, Chen S, Liu N, Hu F, Yu J. Handgrip strength is positively associated with successful aging in older adults: a national cross-sectional study in China. J Affect Disord. 2023;333:30–7. https://doi.org/10.1016/j.jad.2023.04.041.
Zhao X, Yu J, Zhou Z. Separate and combined associations of obesity and handgrip strength with cognitive function in older adults: a national cross-sectional study in China. J Sports Sci. 2024;1–7. https://doi.org/10.1080/02640414.2024.2321420. Epub ahead of print.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95. https://doi.org/10.1249/01.mss.0000078924.61453.fb.
Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. https://doi.org/10.1186/1479-5868-8-115.
Guo X, Mao H, Liu T, Zhang Y, Shen P, Xie D, et al. Validity of the international physical activity questionnaire and bouchard diary in Chinese adults. Wei Sheng Yan Jiu. 2021;50(3):435–41. https://doi.org/10.19813/j.cnki.weishengyanjiu.2021.03.015. (in Chinese).
Wen X, Wang M, Jiang CM, Zhang YM. Anthropometric equation for estimation of appendicular skeletal muscle mass in Chinese adults. Asia Pac J Clin Nutr. 2011;20(4):551–6.
Gao K, Cao LF, Ma WZ, Gao YJ, Luo MS, Zhu J, et al. Association between Sarcopenia and cardiovascular disease among middle-aged and older adults: findings from the China health and retirement longitudinal study. EClinicalMedicine. 2022;44:101264. https://doi.org/10.1016/j.eclinm.2021.101264.
Zhao X, Zhang H, Yu J, Zhou Z, Wang J. Physical activity intensity, frequency, duration, volume and the risk of possible Sarcopenia in middle-aged and older adults. Geroscience. 2023;1–15. https://doi.org/10.1007/s11357-023-00848-9. Epub ahead of print.
Sallfeldt ES, Mallmin H, Karlsson MK, Mellström D, Hailer NP, Ribom EL. Sarcopenia prevalence and incidence in older men - a MrOs Sweden study. Geriatr Nurs. 2023;50:102–8. https://doi.org/10.1016/j.gerinurse.2023.01.003.
Sri-On J, Fusakul Y, Kredarunsooksree T, Paksopis T, Ruangsiri R. The prevalence and risk factors of Sarcopenia among Thai community-dwelling older adults as defined by the Asian Working Group for Sarcopenia (AWGS-2019) criteria: a cross-sectional study. BMC Geriatr. 2022;22(1):786. https://doi.org/10.1186/s12877-022-03471-z.
Veronese N, Smith L, Cereda E, Maggi S, Barbagallo M, Dominguez LJ, et al. Multimorbidity increases the risk for Sarcopenia onset: longitudinal analyses from the English Longitudinal Study of Ageing. Exp Gerontol. 2021;156:111624. https://doi.org/10.1016/j.exger.2021.111624.
Matsumoto H, Tanimura C, Kushida D, Osaka H, Kawabata Y, Hagino H. FRAX score and recent fall history predict the incidence for Sarcopenia in community-dwelling older adults: a prospective cohort study. Osteoporos Int. 2020;31(10):1985–94. https://doi.org/10.1007/s00198-020-05447-4.
Yu R, Wong M, Leung J, Lee J, Auyeung TW, Woo J. Incidence, reversibility, risk factors and the protective effect of high body mass index against Sarcopenia in community-dwelling older Chinese adults. Geriatr Gerontol Int. 2014;14(Suppl 1):15–28. https://doi.org/10.1111/ggi.12220.
Pham LT, Nguyen BT, Huynh DT, Nguyen BLT, Tran PN, Van Vo T, et al. Community-based prevalence and associated factors of Sarcopenia in the Vietnamese elderly. Sci Rep. 2024;14(1):17. https://doi.org/10.1038/s41598-023-50979-4.
Marini JAG, Abdalla PP, Bohn L, Mota J, Duncan M, Dos Santos AP, et al. Moderate physical activity reduces the odds of Sarcopenia in community- dwelling older women: a cross-sectional study. Curr Aging Sci. 2023;16(3):219–26. https://doi.org/10.2174/1874609816666230330171930.
Scott D, Johansson J, Gandham A, Ebeling PR, Nordstrom P, Nordstrom A. Associations of accelerometer-determined physical activity and sedentary behavior with Sarcopenia and incident falls over 12 months in community-dwelling Swedish older adults. J Sport Health Sci. 2021;10(5):577–84. https://doi.org/10.1016/j.jshs.2020.01.006.
Mijnarends DM, Koster A, Schols JM, Meijers JM, Halfens RJ, Gudnason V, et al. Physical activity and incidence of Sarcopenia: the population-based AGES-Reykjavik Study. Age Ageing. 2016;45(5):614–20. https://doi.org/10.1093/ageing/afw090.
Veen J, Montiel-Rojas D, Kadi F, Nilsson A. Effects of reallocating time spent in different physical activity intensities on Sarcopenia risk in older adults: an isotemporal substitution analysis. Biology (Basel). 2022;11(1):111. https://doi.org/10.3390/biology11010111.
Ohtsubo T, Nozoe M, Kanai M, Ueno K, Nakayama M. Association of objectively measured physical activity with physical function in patients with sarcopenia during hospitalized rehabilitation. Nutrients. 2022;14(20):4439. https://doi.org/10.3390/nu14204439.
Osuka Y, Yabushita N, Kim M, Seino S, Nemoto M, Jung S, et al. Association between habitual light-intensity physical activity and lower-extremity performance: a cross-sectional study of community-dwelling older Japanese adults. Geriatr Gerontol Int. 2015;15(3):268–75. https://doi.org/10.1111/ggi.12268.
Alkahtani S, Aljuhani O, Alhussain M, Habib SS. Association between physical activity patterns and Sarcopenia in arab men. J Int Med Res. 2020;48(4):300060520918694. https://doi.org/10.1177/0300060520918694.
Kwan RYC, Liu JYW, Yin YH, Lee PH, Ng SY, Cheung DSK, et al. Sarcopenia and its association with objectively measured life-space mobility and moderate-to-vigorous physical activity in the oldest-old amid the COVID-19 pandemic when a physical distancing policy is in force. BMC Geriatr. 2022;22(1):250. https://doi.org/10.1186/s12877-022-02861-7.
Zhou XX, Liao SM, Qi L, Wang RX. Physical activity and its association with cognitive function in middle- and older-aged Chinese: evidence from China Health and Retirement Longitudinal Study, 2015. Eur J Sport Sci. 2022;22(6):937–47. https://doi.org/10.1080/17461391.2021.1897164.
Länsitie M, Kangas M, Jokelainen J, Venojärvi M, Timonen M, Keinänen-Kiukaanniemi S, et al. Cardiovascular disease risk and all-cause mortality associated with accelerometer-measured physical activity and sedentary time – a prospective population-based study in older adults. BMC Geriatr. 2022;22(1):729. https://doi.org/10.1186/s12877-022-03414-8.
Silva AC, Pereira MA, Peixoto LM, Rosse IC, Júnior JBF, de Oliveira EC, et al. 12 weeks of resistance training with progressive intensity improves the diagnostic parameters of Sarcopenia in individuals of advanced age. Geriatr Nurs. 2023;54:60–5. https://doi.org/10.1016/j.gerinurse.2023.08.015.
Mori H, Tokuda Y. De-training effects following leucine-enriched whey protein supplementation and resistance training in older adults with Sarcopenia: a randomized controlled trial with 24 weeks of follow-up. J Nutr Health Aging. 2022;26(11):994–1002. https://doi.org/10.1007/s12603-022-1853-1.
Zhao D, Shi W, Bi L, Qi Y, Hu S, Li C, et al. Effect of short-term acute moderate-intensity resistance exercise on blood glucose in older patients with type 2 diabetes mellitus and sarcopenia. Geriatr Gerontol Int. 2022;22(8):653–9. https://doi.org/10.1111/ggi.14437.
Wijndaele K, Westgate K, Stephens SK, Blair SN, Bull FC, Chastin SFM, et al. Utilization and harmonization of adult Accelerometry data: review and expert consensus. Med Sci Sports Exerc. 2015;47(10):2129–39. https://doi.org/10.1249/MSS.0000000000000661.
Acknowledgements
The authors thank the CHARLS research team for their sharing of the data. The authors are also grateful to all the subjects who participated in this study.
Funding
This work was supported by the Zhejiang Provincial Philosophy and Social Science Planning Project (24NDJC070YB), and the Ningbo Public Welfare Science and Technology Project (2022S070). The funding bodies had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Xiaoguang Zhao: Conceptualization; formal analysis; investigation; methodology; resources; writing – original draft preparation. Dongxue Liu: Formal analysis; investigation; methodology. Hongjun Zhang: Formal analysis; methodology. Shaoshuai Shen: Conceptualization; formal analysis; writing – review & editing. Naipeng Zhang: Formal analysis; methodology. Yihan Pan: Formal analysis; writing – original draft preparation. Chao Fu: Data curation; formal analysis; methodology. Wenjiao Wang: Investigation; methodology; resources. Hang Ren: Investigation; methodology. Xiaopeng Pan: Formal analysis; resources. All Authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The participants provided written, informed consent before the start of the study. The study was conducted in accordance with the Declaration of Helsinki and was approved by the research committee at Peking University (registration number: IRB00001052-11015).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
The characteristics of study participants at baseline in 2011 according to the missing data
Supplementary Material 2:
The modified IPAQ short form
Supplementary Material 3:
Association between PA volume and the presence of sarcopenia in disease-free people
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, X., Liu, D., Zhang, H. et al. Associations of physical activity intensity, frequency, duration, and volume with the incidence of sarcopenia in middle-aged and older adults: a 4-year longitudinal study in China. BMC Geriatr 24, 258 (2024). https://doi.org/10.1186/s12877-024-04873-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04873-x