Abstract
Background
Maximizing quality of life (QoL) is a major goal of care for people with dementia in nursing homes (NHs). Social determinants are critical for residents' QoL. However, similar to the United States and other countries, most Canadian NHs routinely monitor and publicly report quality of care, but not resident QoL and its social determinants. Therefore, we lack robust, quantitative studies evaluating the association of multiple intersecting social determinants with NH residents’ QoL. The goal of this study is to address this critical knowledge gap.
Methods
We will recruit a random sample of 80 NHs from 5 Canadian provinces (Alberta, British Columbia, Manitoba, Nova Scotia, Ontario). We will stratify facilities by urban/rural location, for-profit/not-for-profit ownership, and size (above/below median number of beds among urban versus rural facilities in each province). In video-based structured interviews with care staff, we will complete QoL assessments for each of ~ 4,320 residents, using the DEMQOL-CH, a validated, feasible tool for this purpose. We will also assess resident’s social determinants of QoL, using items from validated Canadian population surveys. Health and quality of care data will come from routinely collected Resident Assessment Instrument – Minimum Data Set 2.0 records. Knowledge users (health system decision makers, Alzheimer Societies, NH managers, care staff, people with dementia and their family/friend caregivers) have been involved in the design of this study, and we will partner with them throughout the study. We will share and discuss study findings with knowledge users in web-based summits with embedded focus groups. This will provide much needed data on knowledge users' interpretations, usefulness and intended use of data on NH residents’ QoL and its health and social determinants.
Discussion
This large-scale, robust, quantitative study will address a major knowledge gap by assessing QoL and multiple intersecting social determinants of QoL among NH residents with dementia. We will also generate evidence on clusters of intersecting social determinants of QoL. This study will be a prerequisite for future studies to investigate in depth the mechanisms leading to QoL inequities in LTC, longitudinal studies to identify trajectories in QoL, and robust intervention studies aiming to reduce these inequities.
Similar content being viewed by others
Background
Improving quality of life (QoL) – a person’s physical, emotional and social well-being – is a priority goal of care for people living with dementia [1,2,3,4]. In 2019, 55 million people worldwide were living with dementia, a number expected to increase to 139 million by 2050 [5]. Dementia is a progressive and irreversible syndrome, caused by a range of neurodegenerative, vascular, and other disorders that contribute to decline in cognitive and functional abilities, neuropsychiatric symptoms, and lead to death [6, 7]. Yet, even with profound impairment, people living with dementia can have good QoL with appropriate supports [8]. While communication difficulties, behavioral disturbances, and functional limitations can negatively affect QoL [9], they do not have to [6, 10]. People living with dementia, even those with severe cognitive and physical impairment, often have good QoL [11, 12].
Because appropriate supports are not consistently available, having dementia [13] is a major risk factor for poor QoL, especially for nursing home (NH) residents [14]. Of the 250,000 Canadian NH residents [15], 69% have a diagnosis of dementia, and 89% have some form of cognitive impairment [16]. NH policy prioritizes physical safety and security over QoL [17]. Current research and public reporting in Canada are largely based on the Resident Assessment Instrument – Minimum Data Set 2.0 (RAI) [18], which does not measure QoL [19]. The RAI provides objective indicators of care quality, such as inappropriate antipsychotics use, physical restraint use, pain, and depressive symptoms [20, 21]. These burdensome conditions and treatments negatively affect QoL [22, 23], but their absence does not guarantee good QoL [24]. RAI quality indicators do not include key aspects of QoL, such as social relationships, sense of purpose, or a resident’s feelings and worries [19, 24]. Measuring QoL directly, rather than relying on dementia severity as a poor proxy, is essential to accurately monitor a person’s well-being, and to enable design and evaluation of specific interventions to improve their QoL.
International research on NH residents’ QoL and its social determinants is limited. Social determinants are the non-medical conditions that shape people’s daily lives and affect their health and QoL [25]. They are the major drivers of health inequities, the unfair and avoidable differences in health and QoL among populations [26]. Intersecting identities, such as class, age, gender, race and ethnicity, disability, or religion combine to create various modes of privilege and discrimination, all of which can affect QoL [27, 28]. A recent systematic review and meta-analysis assessed factors associated with QoL in people with dementia [10]. Studies in NHs and assisted living suggested that lack of person-centered care and longer duration of stay decreased QoL. These studies did not assess any social determinants of QoL other than age and gender (both found to be unrelated to QoL) [10]. Studies in non-institutional settings found that being white, having good social relationships, being more socially engaged, being cared for by a spouse, being married, and having religious/spiritual beliefs were associated with better QoL [10]. Living alone decreased QoL [10]. US research suggests that racializedFootnote 1 NH residents or those who lived in a NH with high proportions of racialized residents had poorer QoL [29,30,31,32,33]. US research has also examined social determinants associated with inequities in quality of care and healthcare access [34], but we lack research assessing the association of social determinants other than racialization on the QoL of NH residents, especially those with dementia. Also, US research may not apply to Canada or other countries because NH systems [35], population structures [36], and historic, legal, political, and economic contexts differ.
A recent Canadian study found that non-English speaking NH residents had an increased risk of hospitalization [37]. Our work in the Canadian province of Alberta found lower QoL among racialized NH residents [38]. Canadian qualitative studies illustrate barriers encountered by racialized older adults in accessing healthcare services [39], and the multiple challenges they face in maintaining good QoL in assisted living [40]. The only Canadian study assessing QoL in NHs across provinces was conducted over a decade ago [41, 42]. However, this study did not assess social determinants of QoL, such as racialization, social supports, or financial situation. It also only included residents with no or low cognitive impairment who could self-report, excluding those whose QoL is probably most at risk. No cross-provincial comparisons were reported, even though NH care is regulated provincially in Canada and outcomes vary substantially across provinces [17, 43, 44]. A convenience sample of residents and NHs limited generalizability of findings. We lack large-scale quantitative evaluations of NH residents’ QoL and its social determinants (beyond racialization). We especially lack Canadian data, and data on how factors may intersect to influence QoL [10].
Our study aims to compare QoL among subgroups of older adults living with dementia in NHs, who experience multiple intersecting vulnerabilities – including residents at advanced stages of dementia who cannot self-report and who have no family member or friend to provide a proxy assessment. Three specific research objectives will address these pressing issues:
-
1.
Assess QoL and associated social determinants in a representative sample of NH residents in five Canadian provinces;
-
2.
Identify clusters of intersecting social determinants that perpetuate and reinforce QoL inequities among NH residents;
-
3.
Evaluate, through focus groups and knowledge users’ interpretations, the perceived usefulness and intended uses of data on NH residents’ QoL and its social determinants.
Methods and design
In this 3-year (April 2022 to March 2025) explanatory sequential mixed methods study [45], we will use an integrated knowledge translation (iKT) approach [46] to co-produce knowledge with knowledge users in all project phases. We will first collect quantitative data on nursing residents’ QoL and its social determinants from a representative sample of NHs in the Canadian provinces of Alberta (AB), British Columbia (BC), Manitoba (MB), Nova Scotia (NS), and Ontario (ON). After obtaining provincial ethics approvals and operational approvals (details in Objective 1: Assess QoL and its social determinants section, April to December 2022), we started with the recruitment of facilities (current phase of the project). Data collection started in November 2022 in the provinces and regions we received ethics/operational approvals first, and is scheduled to be completed in April 2024. We will then assess QoL and its health and social determinants (objective 1), as well as different clusters of intersecting factors in those with the highest and lowest QoL (objective 2). Finally, we will prepare feedback reports and conduct feedback webinars with embedded focus groups with knowledge users (objective 3) to help us interpret our findings, discuss how results can be used to enhance care practices, and identify strategies to maximize QoL and minimize QoL inequities among NH residents with dementia.
Theoretical framing
Our theoretical framework integrates 4 perspectives. 1) Social determinants of health – the idea that living conditions primarily shape the health and well-being of individuals, not just medical treatments or lifestyle choices [25]. 2) A health equity framework [47] that outlines important social factors supporting or impeding health equities. 3) Intersectionality – an analytical framework to understand how intersecting, overlapping social identities combine to create different modes of discrimination and privilege [48, 49]. 4) The Wilson & Cleary QoL framework [50] adapted for NHs [51], which guided our selection of social determinants and model covariates (Fig. 1). In alignment with our iKT approach, this study will be guided by a panel of 33 knowledge users, including 4 older adults in need of care and their family/friend caregivers, 7 representatives of advocacy organizations (CanAge, provincial Alzheimer Societies, Canadian Society of Palliative Care Physicians), 9 persons working in NHs (care aides, regulated nurses, managers), and 13 health system decision makers. These knowledge users participated in the conceptualization of this study and they will contribute to each step of the research process by sharing their lived experiences, guiding our priorities, and helping us contextualize our findings.
Objective 1: Assess QoL and its social determinants
In this observational survey study, we will use video calls to collect data on residents’ QoL and its social determinants from care staff who know residents well. We will obtain residents’ most recent, de-identified RAI assessment (completed by care staff in their routine practice) to assess resident health and function covariates. We will complete a survey with an administrator in each participating NH to assess home-level covariates. We will assign a random study identifier to each resident, so that we will not have to identify residents at any time. Therefore, the ethics boards who approved this study waived the requirement to obtain resident consent (Ethics approval and consent to participate section) .
Setting and sample
NHs will be eligible if they are publicly subsidized and licensed by the respective health authority, located in one of the participating health regions or zones, and have 15 beds or more. We will exclude congregate care settings for older adults, other than NHs, such as assisted/supportive/retirement living. In AB, all five Health Zones will participate (170 eligible homes, 15,191 beds [52]). In BC, 4 of 5 Health Regions will participate (260 eligible homes, 27,524 beds [53]). The BC Northern Health Region was excluded because it only has 15 eligible NHs, many of which serve primarily Indigenous populations, and our study team has not established the close, long-term relationships with Indigenous communities that are required to ethically conduct research including these populations. In MB, only the Winnipeg Regional Health Authority will participate (39 eligible homes, 5,640 beds [54]), since only homes in this region routinely collect the RAI data required for our analysis. In NS, all 4 health zones will participate (86 eligible homes, 6,862 beds). Ontario has a total of 617 eligible homes (79,197 beds) [55] and the province is not divided into health regions.
We aim to recruit 10% of all eligible NHs in each of AB (N = 17), BC (N = 26), Winnipeg (N = 4), and NS (N = 9). Ontario, Canada's largest province, has over 600 NHs, so recruiting a 10% sample is not feasible with the available resources. Therefore, we will recruit 24 homes in Ontario (slightly less than a 5% sample) for a total of 80 homes. We will randomly select sites, stratified by health region (geographic region in ON), urban/rural location, for-profit/not-for-profit status, and large/small size (using median number of beds for urban versus rural sites in each region as cut point). We chose these strata given their association with quality of care and QoL [56,57,58,59]. We aim to collect data from all eligible residents at each site. Residents will be included if they have cognitive impairment (a RAI Cognitive Performance Scale [CPS] score of 1 or higher; > 90% of all residents) and have been living in the home for at least 3 months, to ensure that care staff know residents well enough to assess their QoL and social determinants. Residents will be excluded if we cannot identify a suitable care aide. Care aides will be selected who have 1) cared for the resident on at least 4 days during the week before the QoL assessment (the DEMQOL-CH, our QoL assessment tool, assesses residents’ feelings/worries in the last 7 days); 2) worked morning and evening shifts (to ensure awareness of changes in residents’ feelings/worries that depend on time of the day); and 3) worked in the home for at least 3 months (to ensure familiarity with the resident over a longer time).
Sample Size
In our feasibility work [60], regression models on resident QoL suggested a medium effect size (f2 = 0.14) and a within-home intra-cluster correlation (ICC) of 0.211. QoL assessments of multiple residents provided by the same care aide were independent of the assessor (no significant clustering within care aides). To detect this medium effect, a linear multiple regression model with total DEMQOL-CH score as dependent variable, 30 covariates, α = 0.05, and power = 0.8 would require a sample size of 199 residents. Considering the nested structure of our data, we multiplied the required sample size by a variance inflation factor (VIF) [61]. VIF = 1 + (m-1)*ICC with m being cluster size (~ 50 participating residents/home). Our required sample size is 199*11.339 = 2,257 residents. Our feasibility study [60] found that QoL data could be collected from ~ 50% of the residents in participating homes. This corresponds to ~ 4,320 of the ~ 8,640 residents in our 80 NHs. This sample size is more than large enough to account for attrition, smaller effect sizes, and subgroup analyses.
Dependent variable – QoL
Systematic reviews [62,63,64,65,66,67] identified at least 22 tools to measure QoL for people with dementia. We chose the DEMQOL-CH (Additional file 1) [60, 68] because: 1) It is dementia-specific, assessing residents’ feelings and worries. Generic measures of QoL (e.g. EQ5D [69], SF-12 [70]) often work poorly for people with dementia. 2) It is among the most rigorously developed and validated dementia-specific QoL tools, with psychometric properties at least as good as those of other available tools [64, 71,72,73,74,75,76,77]. 3) It was developed and validated for completion by care aides [68]. 4) In our recent study [60] we found that this approach is highly feasible and robust (details below).
The DEMQOL-CH was developed to ensure that people with severe dementia can be included in evaluations. For those in NHs, the choice of proxy is family/friends or care staff. Unfortunately, many residents in Canadian NHs do not have family/friend proxies (up to 35% in some homes) [78]. Mixing family/friend and care staff proxy reports of QoL compromises comparability, because family/friend and care staff proxy reports differ systematically [67]. Family/friend ratings of resident QoL are not by default more accurate than care staff ratings. If a single measure is needed across severities of cognitive impairment and availability of family support (as in our study), staff proxy assessments are the only consistent source available to assess QoL.
Team member Banerjee and colleagues developed and validated the DEMQOL-CH [68]. It is based on the DEMQOL-Proxy [71, 72], an extensively validated tool [64, 65] that uses reports by a family/friend proxy to assess QoL in people with all levels of dementia severity. The 31 DEMQOL-CH items are rated on a 4-point scale (1 = Not At All to 4 = A Lot) and summed to create an overall score (possible range: 31–124). The DEMQOL-CH correlates well with Dementia Care Mapping, an established, robust, observation-based but highly time-consuming method to assess residents’ QoL [79]. Well-known predictors of QoL associate with DEMQOL-CH scores, internal consistency reliability is excellent (0.9), and test–retest reliability is acceptable (0.72) [68]. Inter-rater reliability was borderline-acceptable in the UK study (0.4) [68]. Our Canadian study [60] confirmed the excellent internal consistency reliability (0.83). We found much-improved inter-rater reliability (0.74) by asking administrators to select 2 care staff members for assessments who both knew the resident well. Care aides could complete the DEMQOL-CH within 5 min, and care staff and managers rated use of the DEMQOL-CH as highly feasible, acceptable, and valuable.
Independent variables – social determinants
For this first quantitative, large-scale evaluation of multiple intersecting social determinants of NH resident QoL in Canada, we will prioritize a focused set of social determinants that our knowledge users deemed highest priority. Data on these can be easily collected from residents and families by care teams, using a survey that includes items from validated Statistics Canada population surveys [80, 81] (Additional file 2). As outlined above, racialization is strongly associated with poor QoL [29,30,31,32,33]. We will also include a person’s immigrant status and primary language as variables. Visiting family/friend caregivers are essential to timely and appropriate care [82, 83]. They have critical roles as advocates [84] and legal decision makers for residents unable to clearly communicate their wishes or needs because of cognitive impairment [82, 83, 85]. We will include an item asking care staff and NH key contacts whether the resident is regularly visited by family or friends. Finally, a person’s socioeconomic situation is a strong predictor of their QoL. For example, recent immigrants face challenges accessing low-income supports, leading to longer wait times for NH placement [86]. While we cannot access a resident’s financial data, key contacts in participating homes will know whether a resident’s NH costs are fully covered publicly. In most Canadian provinces, NH costs are shared between authorities and care recipients unless the private share would cause the resident and their family serious financial hardship. Full public coverage of NH costs indicates a resident’s low income.
Resident covariates
These covariates will primarily be drawn from the RAI-MDS 2.0, a valid, reliable standard assessment of residents’ characteristics [18, 87]. Its 450 items capture physical and cognitive functioning and multiple symptoms. It is routinely administered at admission and quarterly in AB, BC, MB, and ON. In NS, a comparable version (RAI Long Term Care Facilities, LTCF) is collected [88, 89]. We will adjust our models for age, gender, education, physical and cognitive functioning, co-morbid conditions, pain, depression, anxiety, responsive behaviours, and length of stay [10]. Our team has established processes for obtaining de-identified RAI records from residents in participating NHs. Via date and resident identifiers, we can link RAI records collected in our survey time-period with resident QoL and social determinants data.
Care aide covariates
These covariates will be from a care aide demographic survey (Additional file 3) that we will complete with each participating care aide after the DEMQOL-CH assessment. The items are from a well-validated survey that our team has used extensively with care aides for decades [90]. We will include care aides’ age, gender, education, race/ethnicity, and primary language to control for possible care aide characteristics that may influence resident QoL or a care aide’s rating of resident QoL. Because care aides who are more distressed tend to rate residents’ QoL lower [67], we will also control for care aide burnout, using the well-validated 9-item Maslach Burnout Inventory [91,92,93].
NH covariates
Covariates will be from a NH survey (Additional file 4), completed with a key contact in each home. Items are based on a well-validated NH survey, used previously by our team [90]. We will include variables thought to be associated with NH residents’ QoL [10, 29,30,31, 33, 42, 56, 94, 95]: ownership model (public not-for-profit, voluntary not-for-profit, private for-profit), small vs large size based on the median bed size among urban vs rural homes in the respective region, health region (to account for regional differences in structures, regulations, and policies that may influence QoL), urban/rural location, staffing (care aide, licensed practical nurse, and registered nurse care hours per resident day based on a validated staffing measure [96]), and proportion of care aides and residents who are racialized, immigrants, or who speak English as an additional language.
Data collection
We will recruit NHs and work with a key contact in each site to identify eligible residents and care aides. Sites will receive a stipend of $500 for participation. Key contacts who help organize data collection will receive a $50 coffee gift card, and care aides completing the DEMQOL-CH will receive coffee gift cards ($5 for up to 5 residents assessed, increasing by $5 for every additional 1–5 residents assessed). Key contacts will complete a NH survey via structured phone or video interviews. Care aides will be interviewed via video or phone. De-identified RAI assessments (those completed within 8 weeks of the QoL assessment) will be obtained from the regional health authorities.
Data analyses
As per REporting of studies Conducted using Observational Routinely-collected Data (RECORD) [97] guidelines, we will conduct basic analyses to ensure that data are of high quality and comparable across jurisdictions. Our team has extensive cleaning protocols to ensure integrity and comparability of NH data. Analyses will apply multiple imputations as per best practices for managing missing data [98]. We will comprehensively describe resident QoL and other health and social characteristics, using summary statistics. We will stratify descriptive analyses of QoL scores by sampling strata (region, size, ownership, urban/rural location) and by resident (e.g., age category, gender, racialization/immigration status/language) and NH social determinants (e.g., above median proportion of racialized residents). We will then use hierarchical generalized linear mixed models [99] (Fig. 1) with QoL (DEMQOL-CH score) as the dependent variable to assess whether social determinants (independent variables) are associated with QoL. We will adjust all models for resident, care aide, and NH covariates. Models will also include a random home-level intercept to account for dependencies of residents living in the same home. We will account for regional differences by including region as a covariate in our models.
Objective 2: Identify clusters of intersection social determinants of QoL
We will use survey data collected in objective 1 to 1) identify inequities in QoL and 2) assess if and how clusters (latent classes) of intersecting social determinants differ between residents with high and low QoL, using multi-level covariate-adjusted latent class analyses (LCAs) [100]. LCAs are widely used to identify subgroups in a population that are characterized by intersection of particular characteristics (in our case: clusters of intersecting social determinants) [101]. QoL inequities are unfair and avoidable differences in QoL [26]. Therefore, it is important to compare subsamples of residents with especially high and low QoL scores. Intersectionality means that social determinants such as racialization, class, or gender are interconnected, and embedded within systems and discourses of power that perpetuate structural inequities [48, 49]. Rather than modelling social determinants individually (or interactions of 2 social determinants) as in our regression models (objective 1), LCAs will allow us to identify which combinations (latent classes) of social determinants are present among residents with especially high and low QoL and which profiles are more common.
Sample and sample size
Analyses will include the 25% of residents (n = 1,080) in our sample with lowest QoL (25th percentile of DEMQOL-CH scores) and the 25% of residents with highest QoL (75th percentile of DEMQOL-CH scores). A simulation study of sample sizes required for multi-level LCA [102] suggests a minimum of 20 homes with at least 10 residents per home. Our total study sample will include ~ 50 residents in each of 80 homes. Therefore, our 25% subsamples will include ~ 12.5 residents per home, comfortably meeting sample size requirements. For sensitivity analysis and to mitigate any sample size issues, we will split the total sample based on the median DEMQOL-CH score and replicate our analyses. This will give us a total sample size of 2,160 residents in each of the 2 subsamples (high/low QoL) and ~ 25 residents per home.
Model variables
Models will include our main social determinants plus gender as latent class indicators. We will adjust the models for resident and care aide (level 1) and NH (level 2) covariates that are statistically significantly associated with resident QoL in our regression models (objective 1). Level 1 covariates predict an individual’s overall probability of being in a certain latent class. Level 2 covariates predict a NH’s probability that an individual will be in a certain latent class.
Data analyses
We will specify 2-level LCA models, adjusted for level 1 and level 2 covariates. Level 1 random class means are modelled as continuous level 2 latent variables that vary across homes (equivalent to a home-level random intercept) [100]. As in objective 1, we will include region as a model covariate rather than a random intercept. We will run separate series of LCA models in each of our 2 subsamples. In collaboration with our knowledge user experts and guided by our theoretical framework, we will pre-specify the expected number of classes, given the nature of social determinants included. We will then run models with 1, 2, and 3 more classes and with 1, 2, and 3 fewer classes than the number pre-specified [101]. We will compare the fit of each model to that of its predecessor using a significance test and model fit criteria [101]. We will select the final model based on theoretical and statistical considerations.
Objective 3: Evaluate knowledge user’s interpretations, usefulness, and intended use of data
Using a qualitative descriptive approach [103], we will share and discuss findings with our knowledge users to understand their perspectives on how social determinants are related to QoL. We will ask participants how useful they find such data, and if and how they intend to use it in their practice. We will discuss with relevant partners how such data may be used to develop and evaluate future NH policy. Our knowledge users are highly committed to prioritizing and improving QoL in their jurisdictions and care settings, and our iKT approach will expedite their uptake of our study findings. This study is an essential precursor to using these data in future audit and feedback work to improve resident QoL. We will also discuss existing promising practices and potential new strategies to maximize residents’ QoL and minimize QoL inequities, which could be further developed and evaluated in future studies. Our approach uses: 1) systematic feedback of study findings to participating care teams and other knowledge users, in an effective, feasible, theory-based feedback approach previously tested [104,105,106,107,108,109], 2) interactive, facilitated discussions of our findings with knowledge users in recorded video conference-based summits, and 3) focus groups of 5–6 knowledge users each, who can speak to experiences of immigrants, racialized, and low income older adults living with dementia.
Feedback reports to share findings with knowledge users
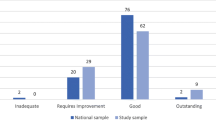
For each NH and health region, we will generate a tailored feedback report, structured and designed like the feedback reports our team has successfully generated, disseminated and discussed with knowledge users for decades [104,105,106,107,108,109]. We will develop reports in collaboration with our knowledge users for wider implementation. Each feedback report will include the QoL findings (rating of each DEMQOL-CH item and overall DEMQOL-CH score) for each resident in that facility that we collected QoL data for. We will also report the facility's overall (average) DEMQOL-CH score and compare it to the rest of the (de-identified) sample (by region, province and overall). Each facility's unique report will only be shared with that facility. For knowledge users who are not part of any of the participating facilities, we will generate overall summary reports.
Sample – feedback summit participants
We will invite participating care teams, our study's knowledge users, and additional knowledge users to web-based feedback summits (3 summits to maximize numbers of attendees, 20–30 attendees/summit). Integrated into the summits will be focus groups, each including ~ 5–10 participants for a total of ~ 10–15 focus groups (5 per summit).
Data collection
Reports will be shared with summit participants 2 weeks ahead of the summit and then presented to and discussed with participants at the summit. Duration of each summit will be 3 h. An experienced facilitator with strong skills in working with heterogeneous groups (including immigrants, racialized, and low-income individuals, and those living with dementia) and mitigating power differences will facilitate summits. Summits will follow our previously tested, theory-based, effective process of feeding back and discussing study findings [104,105,106,107,108,109].
In the first half of the summit, we will present and discuss QoL reports. Sessions will be recorded for data analyses (transcription purposes), using Zoom. We will then assign participants by role to focus groups (60–90 min, 5–10 people each). We will conduct separate focus groups with 1) decision makers, 2) NH managers, 3) nurses and other regulated care staff, 4) care aides, and 5) advocates (e.g., Alzheimer Societies), individuals in need of care and their family/friend caregivers. Each focus group will be facilitated by a research team member and video recorded (for transcription purposes). Focus groups following large panel discussions will create space for individual knowledge users to share their experiences and perspectives in detail and to raise issues that they may have decided not to raise in the large group.
Data analyses
We will transcribe summit and focus group recordings verbatim. Using thematic content analysis [110], we will deductively code transcripts, focusing on participants’ interpretations of results, perceived usefulness and intended uses of our data, promising practices, and new strategies to maximize QoL and minimize QoL inequities. Using the constant comparative method [111], we will inductively identify additional themes not captured by our focus group guide (Additional file 5). For rigour and trustworthiness, each of 2 team members will independently code texts and then reconcile coding together until consensus is reached.
Discussion
QoL and its social determinants are essential aspects largely missing from routine data collected in NHs. US research has assessed disparities in NH care in general [34], and especially racial disparities in resident QoL [29,30,31,32,33]. However, we lack studies assessing multiple social determinants (and their complex interplay – their intersection) and their association with resident QoL directly (rather than focusing on quality of care or healthcare access). This study will contribute to addressing these important knowledge gaps. Our findings will create the prerequisites for developing and testing tailored strategies in future studies aimed at measuring and improving QoL for NH residents living with dementia and reducing inequities in QoL. Our intersectional approach will be a particular strength in informing complex improvement interventions. Our approach to QoL assessment provides a baseline assessment of QoL across several provinces in Canada. Used repeatedly, it can advance monitoring of the impact of diverse strategies and policy initiatives for QoL, improving their resource allocation. This study provides the foundational methods and data for evaluative work to investigate in depth the mechanisms leading to QoL inequities in NHs, and for longitudinal studies to identify trajectories in QoL. Our advanced skill-building for trainees will develop urgently needed Canadian capacity in research on QoL and its social determinants in vulnerable populations living with dementia. Our CIHR-funded project [112] will contribute to the science of sustaining, spreading, and scaling successful implementation of tailored strategies to improve QoL and reduce inequities in NHs. These learnings will be key to longitudinal work and to expanding our QoL work to other Canadian provinces and territories.
Availability of data and materials
All study data and analytical output will be held on a secure server at the University of Alberta, as required by the ethics and provincial data confidentiality requirements relevant to this study. As such, all study datasets will not be publicly available. Ethics approvals and provincial data confidentiality regulations require that access will be restricted to approved study investigators and research associates. Aggregate data and relevant statistical code will be available from the primary investigator (MH) on reasonable request. For additional information regarding the availability of data contact Dr. Matthias Hoben, email: mhoben@yorku.ca.
Notes
We base our understanding of the term ‘racialization’ on Hochman’s [113] comprehensive discussion and defence of this term. Specifically, racialization is defined “as the process through which groups come to be understood as major biological entities and human lineages, formed due to reproductive isolation, in which membership is transmitted through biological descent.” [113], p. 1246. The terminology related to race and ethnicity is highly heterogeneous and contested, and even the authors of the US studies cited above seem to vary the terminology they use from paper to paper [30,31,32,33,34]. In this paper, we refer to racialized residents as those who are perceived and grouped by others based on their appearance, behaviours, immigration background, ‘foreign’ accent, etc., and who often experience discrimination and inequities because of that.
Abbreviations
- LCA:
-
Latent class analyses
- NH:
-
Nursing home
- QoL:
-
Quality of life
References
Public Health Agency of Canada. A dementia strategy For Canada: Together we aspire. Ottawa, ON: public health agency of Canada; 2019.
Alzheimer’s Disease International. World Alzheimer Report 2018: The state of the art of dementia research: New frontiers. London: Alzheimer’s Disease International; 2018.
World Health Organization (WHO). Global action plan on the public health response to dementia 2017–2025. Geneva:WHO;2017.
Alzheimer Europe. Dementia in Europe Yearbook 2018: Comparison of national dementia strategies in Europe. Luxembourg: Alzheimer Europe; 2018.
World Health Organization. Global status report on the public health response to dementia. Geneva: World Health Organization; 2021.
Haaksma ML, Leoutsakos JS, Bremer JAE, Aalten P, Ramakers I, Verhey FRJ, et al. The clinical course and interrelations of dementia related symptoms. Int Psychogeriatr. 2018;30:859–66.
Kua EH, Ho E, Tan HH, Tsoi C, Thng C, Mahendran R. The natural history of dementia. Psychogeriatrics. 2014;14:196–201.
O’Rourke HM, Duggleby W, Fraser KD, Jerke L. Factors that affect quality of life from the perspective of people with dementia: a metasynthesis. J Am Geriatr Soc. 2015;63:24–38.
Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529–38.
Martyr A, Nelis SM, Quinn C, Wu YT, Lamont RA, Henderson C, et al. Living well with dementia: a systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychol Med. 2018;48:2130–9.
Banerjee S, Smith SC, Lamping DL, Harwood RH, Foley B, Smith P, et al. Quality of life in dementia: more than just cognition. An analysis of associations with quality of life in dementia. J Neurol Neurosurg Psychiatry. 2006;77:146–8.
Banerjee S, Samsi K, Petrie CD, Alvir J, Treglia M, Schwam EM, et al. What do we know about quality of life in dementia? A review of the emerging evidence on the predictive and explanatory value of disease specific measures of health related quality of life in people with dementia. Int J Geriatr Psychiatry. 2009;24:15–24.
Ydstebo AE, Bergh S, Selbaek G, Benth JS, Bronnick K, Vossius C. Longitudinal changes in quality of life among elderly people with and without dementia. Int Psychogeriatr. 2018;30:1607–18.
Jing W, Willis R, Feng Z. Factors influencing quality of life of elderly people with dementia and care implications: A systematic review. Arch Gerontol Geriatr. 2016;66:23–41.
Statistics Canada. Census of Population, 2021: Data tables - Type of collective dwelling, age and gender for the population in collective dwellings: Canada, provinces and territories. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810004501. Accessed 12 Apr 2023.
Canadian Institute for Health Information (CIHI). Dementia in long-term care. https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-long-term-care. Accessed 12 Apr 2023.
Hande MJ, Keefe J, Taylor D. Long-Term Residential Care Policy Guidance for Staff to Support Resident Quality of Life. Gerontologist. 2021. https://doi.org/10.1093/geront/gnaa176.
Morris JN, Hawes C, Mor V, Phillips C, Fries BE, Nonemaker S, et al. Resident Assessment Instrument (RAI) RAI-MDS 2.0 User’s Manual, Canadian Version, February 2012. Toronto, ON: Canadian Institute for Health Information (CIHI); 2012.
Armstrong H, Daly T, Choiniere JA. Policies and practices: The case of RAI-MDS in Canadian long-term care homes. J Can Stud. 2016;50:348–67.
Hutchinson AM, Draper K, Sales AE. Public reporting of nursing home quality of care: lessons from the United States experience for canadian policy discussion. Healthc Policy. 2009;5:87–105.
Hutchinson AM, Milke DL, Maisey S, Johnson C, Squires JE, Teare G, et al. The Resident Assessment Instrument-Minimum Data Set 2.0 quality indicators: a systematic review. BMC Health Serv Res. 2010;10:166.
Anderson K, Bird M, MacPherson S, Blair A. How do staff influence the quality of long-term dementia care and the lives of residents? A systematic review of the evidence. Int Psychogeriatr. 2016;28:1263–81.
Beerens HC, Zwakhalen SM, Verbeek H, Ruwaard D, Hamers JP. Factors associated with quality of life of people with dementia in long-term care facilities: a systematic review. Int J Nurs Stud. 2013;50:1259–70.
Kane RA. Long-term care and a good quality of life: bringing them closer together. Gerontologist. 2001;41:293–304.
Raphael D, Bryant T, Mikkonen J, Raphael A. Social determinants of health: The Canadian facts. 2nd edition. Oshawa and Toronto: Ontario Tech University, Faculty of Health Sciences and York University, School of Health Policy and Management;2020.
Braveman P, Gruskin S. Defining equity in health. J Epidemiol Commun Health. 2003;57:254–8.
Sirgy MJoseph. The psychology of quality of life hedonic well-being, life satisfaction, and eudaimonia. 2nd edition. Dordrecht: Springer; 2012.
Land KC, Michalos AC, Sirgy MJ. Handbook of social indicators and quality of life research. Dordrecht: Springer; 2012.
Shippee TP, Henning-Smith C, Rhee TG, Held RN, Kane RL. Racial differences in Minnesota nursing home residents’ quality of life: The importance of looking beyond individual predictors. J Aging Health. 2016;28:199–224.
Shippee TP, Ng W, Bowblis JR. Does living in a higher proportion minority facility improve quality of life for racial/ethnic minority residents in nursing homes? Innov Aging. 2020;4:igaa014.
Shippee TT, Ng W, Duan Y, Woodhouse M, Akosionu O, Chu H, et al. Changes over time in racial/ethnic differences in quality of life for nursing home residents: Patterns within and between facilities. J Aging Health. 2020;32:1498–509.
Shippee TP, Akosionu O, Ng W, Woodhouse M, Duan Y, Thao MS, et al. COVID-19 Pandemic: Exacerbating racial/ethnic disparities in long-term services and supports. J Aging Soc Policy. 2020;32:323–33.
Bowblis JR, Ng W, Akosionu O, Shippee TP. Decomposing racial and ethnic disparities in nursing home quality of life. J Appl Gerontol. 2020;733464820946659.
Carlson E, Selassie G. Racial Disparities in Nursing Facilities— and How to Address Them. Washington, DC: Justice in Aging; 2022.
Ridic G, Gleason S, Ridic O. Comparisons of health care systems in the United States Germany and Canada. Mater Sociomed. 2012;24:112–20.
IndexMundi. Canada vs. United States. https://www.indexmundi.com/factbook/compare/canada.united-states. Accessed 12 Apr 2023.
Jeong A, Lapenskie J, Talarico R, Hsu AT, Tanuseputro P. Health outcomes of immigrants in nursing homes: A population-based retrospective cohort study in Ontario. Canada J Am Med Dir Assoc. 2020;21:740–746.e5.
Hoben M, Dymchuk E, Corbett K, Devkota R, Shrestha S, Lam J, et al. Factors associated with the quality of life of nursing home residents during the COVID-19 pandemic: A cross-sectional study. J Am Med Dir Assoc. 2023;24:876–84.
Koehn S. Negotiating candidacy: ethnic minority seniors’ access to care. Ageing Soc. 2009;29:585–608.
Koehn SD, Mahmood AN, Stott-Eveneshen S. Quality of life for diverse older adults in assisted living: The centrality of control. J Gerontol Soc Work. 2016;59:512–36.
Kehyayan V, Hirdes JP, Tyas SL, Stolee P. Residents’ self-reported quality of life in long-term care facilities in Canada. Can J Aging. 2015;34:149–64.
Kehyayan V, Hirdes JP, Tyas SL, Stolee P. Predictors of long-term care facility residents’ self-reported quality of life with individual and facility characteristics in Canada. J Aging Health. 2016;28:503–29.
Hoben M, Chamberlain SA, Gruneir A, Knopp-Sihota JA, Sutherland JM, Poss JW, et al. Nursing home length of stay in in three Canadian health regions: temporal trends, jurisdictional differences and associated factors. J Am Med Direct Assoc. 2019;20 In press.
Hoben M, Heninger A, Holroyd-Leduc J, Knopp-Sihota J, Estabrooks C, Goodarzi Z. Depressive symptoms in long term care facilities in Western Canada: a cross sectional study. BMC Geriatr. 2019;19:335.
Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Third Edition. SAGE;2018.
Bowen SJ, Graham ID. From knowledge translation to engaged scholarship: promoting research relevance and utilization. Arch Phys Med Rehabil. 2013;94(1 Suppl):S3–8.
Peterson A, Charles V, Yeung D, Coyle K. The Health Equity Framework: A science- and justice-based model for public health researchers and practitioners. Health Promot Pract. 2020;1524839920950730.
Crenshaw K, Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics," : Vol. Article 8. Univ Chic Leg Forum. 1989;1989(1989):139–67.
Holman D, Walker A. Understanding unequal ageing: towards a synthesis of intersectionality and life course analyses. Eur J Ageing. 2020. https://doi.org/10.1007/s10433-020-00582-7.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: A conceptual model of patient outcomes. JAMA. 1995;273:59–65.
Zubritsky C, Abbott KM, Hirschman KB, Bowles KH, Foust JB, Naylor MD. Health-related quality of life: expanding a conceptual framework to include older adults who receive long-term services and supports. Gerontologist. 2013;53:205–10.
Alberta Health Services. Annual report 2018–19: A healthier future together. Edmonton, AB: Alberta Health Services;2019.
Office of the Seniors Advocate British Columbia. British Columbia long-term care facilities quick facts directory: Summary report. Vancouver, BC: Office of the Seniors Advocate British Columbia; 2020.
Long Term & Continuing Care Association of Manitoba. List of personal care homes in MB. 2021. https://www.ltcam.mb.ca/pch-mblist.htm. Accessed 13 Apr 2023.
ServiceOntario. Reports on Long-Term Care Homes: Search for LTC Homes By Home Name. https://publicreporting.ltchomes.net/en-ca/Search_Selection.aspx. Accessed 10 Sep 2023.
Shippee TP, Henning-Smith C, Kane RL, Lewis T. Resident- and facility-level predictors of quality of life in long-term care. Gerontologist. 2015;55:643–55.
Beeber AS, Zimmerman S, Reed D, Mitchell CM, Sloane PD, Harris-Wallace B, et al. Licensed nurse staffing and health service availability in residential care and assisted living. J Am Geriatr Soc. 2014;62:805–11.
Poss J, McGrail K, McGregor MJ, Ronald LA. Long-term care facility ownership and acute hospital service use in British Columbia, Canada: A retrospective cohort study. J Am Med Dir Assoc. 2020;21:1490–6.
Tanuseputro P, Chalifoux M, Bennett C, Gruneir A, Bronskill SE, Walker P, et al. Hospitalization and mortality rates in long-term care facilities: Does for-profit status matter? J Am Med Dir Assoc. 2015;16:874–83.
Hoben M, Banerjee S, Beeber AS, Chamberlain SA, Hughes L, O’Rourke HM, et al. Feasibility of routine quality of life measurement for people living with dementia in long-term care. J Am Med Dir Assoc. 2022;23:1221–6.
Hsieh FY, Lavori PW, Cohen HJ, Feussner JR. An overview of variance inflation factors for sample-size calculation. Eval Health Prof. 2003;26:239–57.
Hughes LJ, Farina N, Page TE, Tabet N, Banerjee S. Psychometric properties and feasibility of use of dementia specific quality of life instruments for use in care settings: a systematic review. Int Psychogeriatr. 2019;Published online ahead of print:1–15.
Aspden T, Bradshaw SA, Playford ED, Riazi A. Quality-of-life measures for use within care homes: a systematic review of their measurement properties. Age Ageing. 2014;43:596–603.
Bowling A, Rowe G, Adams S, Sands P, Samsi K, Crane M, et al. Quality of life in dementia: a systematically conducted narrative review of dementia-specific measurement scales. Aging Ment Health. 2015;19:13–31.
Dichter MN, Schwab CGG, Meyer G, Bartholomeyczik S, Halek M. Linguistic validation and reliability properties are weak investigated of most dementia-specific quality of life measurements - A systematic review. J Clin Epidemiol. 2016;70:233–45.
Yang F, Dawes P, Leroi I, Gannon B. Measurement tools of resource use and quality of life in clinical trials for dementia or cognitive impairment interventions: A systematically conducted narrative review. Int J Geriatr Psychiatry. 2018;33:e166–76.
Robertson S, Cooper C, Hoe J, Lord K, Rapaport P, Marston L, et al. Comparing proxy rated quality of life of people living with dementia in care homes. Psychol Med. 2020;50:86–95.
Hughes LJ, Farina N, Page TE, Tabet N, Banerjee S. Adaptation of the DEMQOL-Proxy for routine use in care homes: reliability and validity of DEMQOL-CH. BMJ Open. 2019;9: e028045.
EQ-5D. https://euroqol.org/. Accessed 27 Feb 2020.
12-Item Short Form Survey (SF-12). https://www.rand.org/health-care/surveys_tools/mos/12-item-short-form.html. Accessed 27 Feb 2020.
Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al. Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology. Health Technol Assess (Winchester, England). 2005;9(1–93):iii–iv.
Smith SC, Lamping DL, Banerjee S, Harwood RH, Foley B, Smith P, et al. Development of a new measure of health-related quality of life for people with dementia: DEMQOL. Psychol Med. 2007;37:737–46.
Aguirre E, Kang S, Hoare Z, Edwards RT, Orrell M. How does the EQ-5D perform when measuring quality of life in dementia against two other dementia-specific outcome measures? Qual Life Res. 2016;25:45–9.
Banerjee S, Willis R, Matthews D, Contell F, Chan J, Murray J. Improving the quality of care for mild to moderate dementia: an evaluation of the Croydon Memory Service Model. Int J Geriatr Psychiatry. 2007;22:782–8.
Chua KC, Brown A, Little R, Matthews D, Morton L, Loftus V, et al. Quality-of-life assessment in dementia: the use of DEMQOL and DEMQOL-Proxy total scores. Qual Life Res. 2016;25:3107–18.
Hendriks AAJ, Smith SC, Chrysanthaki T, Black N. Reliability and validity of a self-administration version of DEMQOL-Proxy. Int J Geriatr Psychiatry. 2017;32:734–41.
Hendriks AAJ, Smith SC, Chrysanthaki T, Cano SJ, Black N. DEMQOL and DEMQOL-Proxy: a Rasch analysis. Health Qual Life Outcomes. 2017;15:164.
Chamberlain SA, Duggleby W, Fast J, Teaster PB, Estabrooks CA. Incapacitated and alone: Prevalence of unbefriended residents in Alberta long-term care homes. SAGE Open. 2019;9:2158244019885127.
Barbosa A, Lord K, Blighe A, Mountain G. Dementia Care Mapping in long-term care settings: a systematic review of the evidence. Int Psychogeriatr. 2017;29:1609–18.
Statistics Canada. 2021 Census: 2A-L. https://www.statcan.gc.ca/eng/statistical-programs/instrument/3901_Q2_V6. Accessed 13 Apr 2023.
Statistics Canada. Canadian Community Health Survey (CCHS) - 2016. https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&lang=en&Item_Id=260675. Accessed 14 Mar 2021.
Port CL, Zimmerman S, Williams CS, Dobbs D, Preisser JS, Williams SW. Families Filling the Gap: Comparing Family Involvement for Assisted Living and Nursing Home Residents With Dementia. Gerontologist. 2005;45 suppl_1:87–95.
Zimmerman S, Cohen LW, Reed D, Gwyther LP, Washington T, Cagle JC, et al. Comparing families and staff in nursing homes and assisted living: implications for social work practice. J Gerontol Soc Work. 2013;56:535–53.
Baumbusch J, Phinney A. Invisible hands: the role of highly involved families in long-term residential care. J Fam Nurs. 2014;20:73–97.
Brown EE, Kumar S, Rajji TK, Pollock BG, Mulsant BH. Anticipating and mitigating the impact of the COVID-19 Pandemic on Alzheimer’s Disease and Related Dementias. Am J Geriatr Psychiatry. 2020;28:712–21.
Qureshi D, Schumacher C, Talarico R, Lapenskie J, Tanuseputro P, Scott M, et al. Describing differences among recent immigrants and long-standing residents waiting for long-term care: A population-based retrospective cohort study. J Am Med Dir Assoc. 2021;22:648–55.
Poss JW, Jutan NM, Hirdes JP, Fries BE, Morris JN, Teare GF, et al. A review of evidence on the reliability and validity of Minimum Data Set data. Healthc Manage Forum. 2008;21:33–9.
Kim H, Jung Y-I, Sung M, Lee J-Y, Yoon J-Y, Yoon J-L. Reliability of the interRAI Long Term Care Facilities (LTCF) and interRAI Home Care (HC). Geriatr Gerontol Int. 2015;15:220–8.
Norman KJ, Hirdes JP. Evaluation of the predictive accuracy of the interRAI Falls clinical assessment protocol, scott fall risk screen, and a supplementary falls risk assessment tool used in residential long-term care: a retrospective cohort study. Can J Aging. 2020;39:521–32.
Estabrooks CA, Squires JE, Cummings GG, Teare GF, Norton PG. Study protocol for the translating research in elder care (TREC): building context - an organizational monitoring program in long-term care project (project one). Implement Sci. 2009;4:52.
Estabrooks CA, Squires JE, Hayduk L, Morgan D, Cummings GG, Ginsburg L, et al. The influence of organizational context on best practice use by care aides in residential long-term care settings. J Am Med Dir Assoc. 2015;16(537):e1–10.
Beckstead JW. Confirmatory factor analysis of the Maslach Burnout Inventory among Florida nurses. Int J Nurs Stud. 2002;39:785–92.
Barnett RC, Brennan RT, Gareis KC. A closer look at the measurement of burnout. J Appl Biobehav Res. 1999;4:65–78.
Kehyayan V. Relationships between quality of life and selected resident and facility characteristics in long term care facilities in Canada: PhD thesis. 2011. https://uwspace.uwaterloo.ca/bitstream/handle/10012/6058/Kehyayan_Vahe.pdf?sequence=1&isAllowed=y. Accessed 25 Mar 2021.
Shippee TP, Hong H, Henning-Smith C, Kane RL. Longitudinal changes in nursing home resident-reported quality of life: the role of facility characteristics. Res Aging. 2015;37:555–80.
Cummings GG, Doupe M, Ginsburg L, McGregor MJ, Norton PG, Estabrooks CA. Development and Validation of A Scheduled Shifts Staffing (ASSiST) measure of unit-level staffing in nursing homes. Gerontologist. 2017;57:509–16.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12: e1001885.
Graham JW. Missing data: analysis and design. New York, NY: Springer; 2012.
Hox J, Moerbeek M, van de Schoot R. Multilevel Analysis: Techniques and Applications. 3rd ed. New York: Routledge; 2017.
Bakk Z, Di Mari R, Oser J, Kuha J. Two-stage multilevel latent class analysis with covariates in the presence of direct effects. Struct Equ Modeling. 2022;29:267–77.
Dziak JJ, Lanza ST, Tan X. Effect size, statistical power and sample size requirements for the bootstrap likelihood ratio test in latent class analysis. Struct Equ Modeling. 2014;21:534–52.
Park J, Yu HT. Recommendations on the sample sizes for multilevel latent class models. Educ Psychol Meas. 2018;78:737–61.
Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: A systematic review. Res Nurs Health. 2017;40:23–42.
Hoben M, Ginsburg LR, Easterbrook A, Norton PG, Anderson RA, Andersen EA, et al. Comparing effects of two higher intensity feedback interventions with simple feedback on improving staff communication in nursing homes—the INFORM cluster-randomized controlled trial. Implement Sci. 2020;15:75.
Estabrooks CA, Teare GF, Norton PG. Should we feed back research results in the midst of a study? Implement Sci. 2012;7:87.
Boström A-M, Cranley LA, Hutchinson AM, Cummings GG, Norton PG, Estabrooks CA. Nursing home administrators’ perspectives on a study feedback report: a cross sectional survey. Implement Sci. 2012;7:88.
Hutchinson AM, Batra-Garga N, Cranley L, Bostrom A-M, Cummings G, Norton P, et al. Feedback reporting of survey data to healthcare aides. Implement Sci. 2012;7:89.
Cranley LA, Birdsell JM, Norton PG, Morgan DG, Estabrooks CA. Insights into the impact and use of research results in a residential long-term care facility: a case study. Implement Sci. 2012;7:90.
Ginsburg LR, Hoben M, Easterbrook A, Andersen E, Anderson RA, Cranley L, et al. Examining fidelity in the INFORM trial: a complex team-based behavioral intervention. Implement Sci. 2020;15:78.
Mayring P. Qualitative Content Analysis: A Step-by-Step Guide. Thousand Oaks, CA: Sage; 2022.
Glaser BG. The constant comparative method of qualitative analysis. Soc Probl. 1965;12:436–45.
Berta WB, Wagg A, Cranley L, Doupe MB, Ginsburg L, Hoben M, et al. Sustainment, Sustainability, and Spread Study (SSaSSy): protocol for a study of factors that contribute to the sustainment, sustainability, and spread of practice changes introduced through an evidence-based quality-improvement intervention in Canadian nursing homes. Implement Sci. 2019;14:109.
Hochman A. Racialization: a defense of the concept. Ethn Racial Stud. 2019;42:1245–62.
Acknowledgements
We would like to thank Cathy McPhalen for professional editing services of the original funding proposal that led to this manuscript. We would also like to thank our knowledge users for their ongoing dedication to our project, their valuable guidance and support, and their assistance with navigating ethics approvals, operational approvals, data sharing agreements and recruitment of NHs and participants. Our particular gratitude goes to the NHs and care staff that have participated in our study so far and that have committed to participating in our feedback summits and focus groups. We know these are challenging times for NH providers and staff, and their support despite these adversities cannot be appreciated enough.
Funding
This study is funded by a Canadian Institutes of Health Research (CIHR) Project Grant (funding # 180541), and a CIHR Yves Joanette Award of Excellence in Research in Aging (funding # 179756), both held by MH.
Author information
Authors and Affiliations
Contributions
Study concept and design (MH, MBD, JK, KA, CK, KS, SB, HMO, CH, AB, JS, PJ, AA, CAE); obtaining ethics approvals, operational approvals, data sharing agreements (MH, ED, MBD, JK, KA, KS, KC); recruitment and data collection (MH, ED, MBD, JK, KA, KS, AA, KC, RD, MR, SS); drafting of initial manuscript (MH); critical revision of manuscript for important intellectual content (all authors); obtained research funding (research leads: MH, CAE, PJ); administrative, technical, or material support (ED, KC). “The author(s) read and approved the final manuscript.”
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study obtained ethics clearance from the University of Alberta (Pro00117476), the Mount Saint Vincent University (2021–230), York University (2022–240), University of Victoria (H22-00783), and the University of Manitoba (HS25536 (H2022:191)), and we have obtained operational approvals from regional health authorities and NH operators as needed. Key contacts in each NH (directors of care or facility administrators) will provide verbal informed consent for their home to participate. Care staff in participating homes will provide verbal provide verbal informed consent to participate. Researchers were not aware of resident names or other identifying details at any time. Therefore, the requirement to obtain resident consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
DEMQOL-CH.
Additional file 2.
Nursing home resident social determinants.
Additional file 3.
Care aide demographics.
Additional file 4.
Nursing home characteristics.
Additional file 5.
Focus group guide – feedback summit participants.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hoben, M., Dymchuk, E., Doupe, M.B. et al. Counting what counts: assessing quality of life and its social determinants among nursing home residents with dementia. BMC Geriatr 24, 177 (2024). https://doi.org/10.1186/s12877-024-04710-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04710-1