Abstract
Background
Life-space mobility (LSM) is an important aspect of older adults’ real-life mobility. Studies have shown that restricted LSM is a risk factor for many adverse outcomes such as low quality of life and mortality. Therefore, an increasing number of interventions aim to enhance LSM. However, the intervention approaches differ in terms of their type/content, duration, targeted populations, but also in terms of their outcome measures and assessment tools. Especially the latter impairs the comparability of studies with otherwise similar interventional approaches and thus also the interpretation of their results. Therefore, this systematic scoping review aims to provide an overview of the intervention components, assessment tools, and effectiveness of studies aiming to improve LSM in older adults.
Methods
A systematic literature search was carried out in PubMed and Web of Science. We considered studies in older adults of any design that included an intervention approach and at least one outcome of LSM.
Results
27 studies were included in the review. These studies analyzed healthy community-dwelling as well as frail older adults in need of care or rehabilitation and nursing home residents with a mean age between 64 and 89. The percentage of female participants ranged from 3 to 100%. The types of interventions were of the following: physical, counseling, multidimensional, miscellaneous. Multidimensional interventions consisting of physical interventions plus any of the following or a combination of counseling/education/motivation/information appear to be most effective in increasing LSM. Older adults with mobility impairments were more responsive to these multidimensional interventions compared to healthy older adults. Most of the studies used the questionnaire-based Life-Space Assessment to quantify LSM.
Conclusions
This systematic scoping review provides a comprehensive overview of a heterogenous stock of literature investigating LSM-related interventions in older adults. Future meta-analyses are needed to provide a quantitative evaluation of the effectiveness of LSM interventions and recommendations.
Similar content being viewed by others
Background and objectives
Life-Space Mobility (LSM) is an important aspect of a person’s real-life mobility [1, 2]. Unlike mobility capacity and motor function, LSM is a more complex multifactorial construct [3], which addresses a person’s physical as well as social environment [4]. Therefore, it can be described as in- or out-of-home mobility defined by the space in which a person moves in her or his daily life, respectively by the distance of these spaces from home [3, 5, 6]. Assessment instruments to quantify life-space share that they depict various life-space zones spanning from an individual’s bedroom or home to places beyond an individual’s home town or even further [6].
Assessing LSM has proven to be highly relevant for many populations, especially for older adults. Before COVID, 12-13.5% of male and 27.1% of female older adults were found to have severely impaired LSM [7, 8], and during COVID, this number increased significantly [9]. A restricted life-space has been associated with higher subsequent healthcare costs and higher risks of subsequent submission in hospital or nursing care [10]. Thus, in older adults with difficulties walking ¼ mile, total annual healthcare costs have increased about $2773 [11]. What is more, it was shown that restricted LSM is a risk factor for numerous adverse health-related factors in older adults like poor physical health and functioning [12], cognitive impairment [7, 8, 13, 14], low quality of life [15, 16], restricted social participation [16, 17], nursing home admission [18], loss of independence and increased risk of mortality [17, 19,20,21]. What is more, a number of studies have identified several factors that can influence life-space mobility in older adults [22,23,24,25,26,27,28]. Webber et al. [3] categorized those influencing factors into five categories: (1) physical abilities, (2) cognitive abilities, (3) psychological factors, (4) environmental factors, and (5) financial factors with gender, culture and biography affecting each category. Identifying factors that can influence LSM is important because they can in turn serve as targets for the development of interventions to increase LSM or prevent age-related decline in LSM.
In the last years there has been an increase in the number of studies aiming to enhance LSM. Due to the complexity and multidisciplinary nature of factors influencing LSM, intervention approaches differ in terms of their type/content (e.g., exercise interventions targeting functional capacity versus consultations/behavioral modification techniques), duration (one-time session to regular sessions for months), targeted populations (e.g., healthy, frail, cognitively-impaired), but also in terms of their outcome measures and assessment tools (e.g., self-reported questionnaires, objective GPS-based tools). Especially the latter impairs the comparability of studies with otherwise similar/same interventional approaches and thus also the interpretation of their results.
Therefore, we aimed to provide a comprehensive overview of a potentially large and heterogenous stock of literature investigating LSM-related interventions in older adults. Consequently, this systematic scoping review investigated the following research questions:
1. Which intervention components are used to increase life-space mobility in older adults?
2. Which assessment tools are used to measure life-space mobility in intervention studies in older adults?
3. How effective are those interventions to increase life-space mobility in older adults?
Research design and methods
Scoping reviews have been defined as a “valuable resource for informing future systematic reviews (…) can be of use to researchers, policy-makers and practitioners, reducing duplication of effort and guiding future research” [29]. Correspondingly, we chose to conduct a scoping review to demonstrate the large variety of study designs of LSM-related intervention studies, the divers study populations, intervention methods, and outcome parameters and measures. Yet, we also aimed to cluster interventions and synthesize findings with respect to their effectiveness in order to identify the possible scope for a more precise systematic review and to define boundaries such as the definition of appropriate intervention types and outcomes and more specific research questions.
Protocol and registration
This systematic scoping review was conducted according to the PRISMA guidelines’ extension for scoping reviews (PRISMA-ScR, Supplementary Table 1, Additional File 1) [30], and registered on Prospero (registration ID: CRD42021236380) on March 27th 2021.
Search strategy
In February 2021 and May 2023, PubMed and Web of Science were systematically searched using a combination of keywords describing LSM and its synonyms, a variety of terms to describe intervention types, and various expressions to define the target population. For PubMed, this resulted in a search strategy presented in Table 1.
Besides that, a hand-search was conducted in google scholar and other studies known to the authors were screened to ensure literature saturation.
Selection criteria
Inclusion criteria were (1) articles published in English, (2) study population consisting of older adults aged 60 years or older, (3) the study was conducted as an intervention study including a pre-post assessment, (4) outcomes explicitly included LSM - either subjectively determined (that is via questionnaires such as the University of Alabama Life-Space Assessment (LSA)) or objectively (e.g., via GPS). Studies focusing solely on physical activity-related outcomes (e.g., walking times) and articles published as registries, conference abstracts or editorials were excluded. As recommended for scoping reviews [29], inclusion and exclusion criteria were rather broad and study quality was not used as a filter in order to map all existing literature. Accordingly, there were no restrictions regarding health condition, type of interventions, control group characteristics or year of publication.
Study selection and organization
The resulting articles of both databases were imported into Mendeley citation manager, duplicates were removed. Subsequently, the remaining articles were imported into Rayyan [31], where in a first step, two reviewers (JS and SR) independently screened titles and abstracts. After discussing the results, the same two reviewers conducted a blinded full-text screening to evaluate the remaining studies in more detail. A third and, if necessary, a fourth reviewer (EG and CPJ) were consulted in case of any disagreements after both screening steps; decisions were discussed until consensus was reached.
To organize the articles, included studies were labelled using pre-specified terms relating to the following categories: (1) assessment tool to measure LSM, (2) intervention type, (3) population characteristics. Reasons for exclusion were also indicated using pre-defined labels provided by Rayyan in the following order: (1) wrong language, (2) wrong outcome, (3) wrong population, (4) wrong study design, and (5) wrong publication type. The first label of this order which was found to be applicable was indicated as reason for exclusion.
Data extraction and analysis
Next to the labels described above, more detailed information (number of participants, study design, intervention details, timeframe, other outcome measures, and results) was extracted and transferred to an excel spreadsheet. Details can be found in Supplementary Table 2 (Additional File 2). In case only study protocols were available, the authors were asked to provide the missing information to fill in the extraction table.
Risk of bias and quality assessment
Most commonly, scoping reviews do not include an assessment of the methodological quality of included studies, however, the lack of quality assessment is often mentioned as a limitation factor of scoping reviews [32]. Consequently, we incorporated a critical appraisal of included studies in order to overcome this limitation of scoping reviews and to provide guidance for treatments or future reviews. The “NIH Quality Assessment Tool for Controlled Intervention Studies”, respectively the “NIH Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group” were used [33]. The former includes items about randomization, blinding, similarity of groups at baseline, dropouts, adherence, outcome measures, power calculation, and type of analyses. Items of the latter tool comprise questions about the study question, eligibility criteria, study population, sample size, description of interventions, outcome measures, blinding, follow-up rate, statistical analyses, and group-level interventions. Concerning controlled intervention studies, each study was given a score out of 14 based on the number of “yes” given to each question. A score of 10–14 indicated a good, 5–9 a fair, and 0–4 a low quality. Regarding pre-post studies, the total score was 12 and 8–12 points meant a good quality, whereas 4–7 points indicated a fair, and 0–3 points a low quality.
Data synthesis
Results were grouped regarding the type of intervention and/or sample characteristics and/or outcome measures and/or time frame and/or study quality to form a clear descriptive summary of the included studies for specific intervention types and target groups. Subsequently, we performed a narrative synthesis to summarize the results.
Results
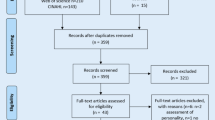
The search strategy resulted in 1479 articles including 221 duplicates, that is, n = 1258 articles were screened for title and abstract. Of these, 49 full texts were analyzed of which 23 met the inclusion criteria. Three further studies were only available as study protocols and have not to date been published as result papers which is why they are among the excluded studies. Finally, 4 further relevant articles [34,35,36,37] known to the authors were included. The final sample consisted of n = 27 articles (see Fig. 1). Details of each included study can be found in Supplementary Table 2 (Additional file 2).
Study characteristics and quality assessment
The 27 included studies were published between 2004 [38] and 2022 [37, 39] and most of them (n = 16) were randomized controlled studies (RCT). Only three studies were conducted as non-randomized controlled trials [37, 40, 41], one study as quasi-randomized [42], and seven further studies as pre-post intervention studies without a control group [35, 36, 38, 39, 43,44,45].
According to the quality assessment conducted via NIH Quality Assessment Tools, most included studies showed fair (n = 11) to good (n = 14) quality and only two studies demonstrated a poor study quality (Supplementary Tables 3 and 4, Additional File 3).
Intervention characteristics
Four groups of interventions have been identified which are described in the following. An overview is provided in Supplementary Table 5 (Additional File 4).
Multidimensional interventions
Almost half of the included studies (n = 12) applied multidimensional interventions, which mostly consisted of physical interventions combined with counseling (n = 10). Additionally, some of these ten studies also included care training/competence training of staff members and/or relatives (n = 2) [41, 46] or community improvements (n = 1) [34]. In most of these multidimensional interventions, the physical part was conducted as a physiotherapy treatment [35, 36, 46] or otherwise as walking interventions [34, 38, 47], mixed physical interventions [37, 41, 48, 49]. The counseling part mostly comprised the encouragement for physical activity and participation [34, 35, 41, 47], nutrition assessment/counseling [37, 38, 46, 49], motivational strategies [48] or ADL-techniques [36]. The remaining two studies which analyzed a multicomponent intervention applied occupational therapy combined with required repairs and home modifications by a handyman [50], or investigated a cognitive-motor group-based activity program [42].
Apart from three studies [37, 38, 42], all multicomponent interventions demonstrated significant positive effects on life-space mobility compared to the respective control group and/or in pre-post-intervention comparison.
Physical interventions
Six studies [40, 44, 45, 51,52,53] investigated the effects of purely physical exercise-based interventions on LSM in older adults. These comprised multifaceted walking events/walking tasks [40], gait training [51], outdoor aerobic training [51], and physical exercises (strength, balance, postural exercises, walking, individual instruction, home-based program) [44, 45, 52, 53]. Only three of these studies [40, 44, 45] demonstrated significant between-, respectively within-group effects of physical interventions on LSM in older adults.
Counseling interventions
Four counseling, respectively educational or psychological interventions were conducted as well. The “Lifestyle Redesign” for instance is an occupational therapy intervention consisting of group sessions and individual meetings and is supposed to empower older adults to perform healthy and fulfilling activities. Levasseur et al. [43] investigated its effect on life-space mobility. They could show an increase in LSM between two out of four assessment points. Nonetheless, no significant improvement was detected over the whole study period. Further studies like Kamga et al. [54], who analyzed the influence of self-care tools such as audio tools and a notebook with written tools together with a coaching, and Siltanen et al. [55], who aimed at increasing self-selected out-of-home activities by counseling, did not find significant effects at all. In contrast, Uemura et al. [56] performed an active learning program regarding behavioral changes to promote a healthy lifestyle which they found to have a significant impact on life-space mobility.
Miscellaneous interventions
A final group of interventions (n = 6) dealt with very specific and special interventions. These combined breathing therapy with exercise advice, a handheld fan and a calming hand [57], or analyzed a driving cessation program [58], a rise-assisting robot [39], music therapy [59], a wheelchair adaption [60], and a horticulture activity program compared to a multicomponent physical exercise program (described in the section “physical interventions”) [53]. Only the first three types of interventions showed significant effects, while neither of the last three studies improved life-space mobility.
Sample characteristics
Together, the 27 studies included 2593 participants. The mean age of the populations under investigation ranged from 64 [38] to 89 [60], whereas the proportion of female participants varied from 3% [47] to 100% [44] with only four studies with male predominance [35, 42, 47, 57]. The sample sizes ranged from 3 [39] to 305 [34] participants. Four groups of participants have been identified:
Community-dwelling older adults without functional limitations
Seven studies investigated LSM in community-dwelling older adults without any specific functional limitations [34, 38, 45, 51, 55, 56, 58]. LSM improved in some of these studies in which a multidimensional intervention [34], counseling [56], or a driving program [58] were conducted. Purely physical exercises did not show an effect on LSM in healthy older adults [45, 51].
Community-dwelling older adults with functional limitations
Seven studies included community-dwelling older adults categorized as prefrail [37] or frail [45, 49, 59], respectively with disabilities [43, 44, 50]. Thereby, five showed an increase in LSM due to multidimensional interventions [50, 61], physical exercises [44, 45], or counseling [43].
Among this population group, two studies focused on older adults undergoing home-based rehabilitation [35, 36]. In both studies, a multidimensional intervention led to an increased LSM.
Finally, a multidimensional intervention also had a positive impact in cognitively impaired older adults recently discharged from rehabilitation [48].
Nursing home residents
Six studies included nursing home-residents, respectively older adults receiving nursing care [39, 41, 42, 46, 52, 60]. In three of these studies, LSM was improved by multidimensional interventions [41, 46], or by providing a rise-assisting robot [39].
Various patient populations
Two studies [47, 57] analyzed internal medicine patients, one study orthopedic patients [40], and depressive participants/participants with psychological problems were in the focus of two studies [53, 54]. The former two groups benefited from a multidimensional intervention [47], a walking intervention [40] and a breathing therapy [57], whereas in depressive participants neither physical interventions, nor counseling or horticulture improved LSM.
Timeframe
The length of the intervention period ranged from one single event of 90 min [40], to 12 months including 10 times 45 to 60-minute sessions and 3–5 times/week independent training [49]. However, no effect of length and frequency of the interventions on LSM was apparent since both short [40, 54] and long intervention periods [49, 55] showed positive as well as negative results.
LSM measures
The majority of studies (n = 18) used the Life-Space Assessment (LSA) to quantify the participants’ LSM [35,36,37,38, 40, 43,44,45, 47,48,49, 51,52,53,54,55,56, 59], whereas three studies applied the Nursing Home Life-Space Diameter (NHLSD) [42, 46, 60]. Other measurement tools were the Homebound Mobility Assessment (HBMA) [50], the Life-Space Questionnaire (LSQ) [57], GPS (Global Positioning System) and accelerometer [34], an indoor wireless sensor network used to measure the life space of nursing home residents [41], and a single question [39, 58].
LSM was the primary outcome in eighteen studies. Fifteen of these studies demonstrated a positive effect of the respective intervention on LSM [34,35,36, 39,40,41, 44,45,46,47,48,49,50, 57, 58]. In contrast, of the other nine studies that analyzed LSM as a secondary outcome, only one study indicated a significantly positive effect [56].
Discussion and implications
Research questions
The aim of this systematic scoping review was to create a comprehensive overview of the current status of interventions targeting LSM in older adults. Given that LSM is a rather holistic measure of mobility and related to a large number of beneficial health outcomes, this review is helpful to shed light on a currently growing body of research which is of high clinical value to the older population. Against this background, three research questions were posed regarding intervention components, assessment tools, and intervention effects.
Regarding the interventions’ components, a wide range of approaches has been applied, whereby a large number of studies used a multidimensional approach mostly based on a combination of physical exercises and counseling. Physical exercise interventions, comprising strength training, balance training, and walking activities, followed by counseling interventions alone formed the other two major categories. The latter ones were without clear focus on LSM but mainly directed at activity encouragement, nutrition, and motivation. Finally, a last group of miscellaneous studies conducted very specific interventions targeted at equally specific populations, like a hand-held fan for patients with respiratory diseases, novel wheelchairs, rise-assisting robots, or horticulture programs.
To measure the effects of the interventions, apart from GPS-based analyzes, all but two studies used validated questionnaires such as the LSA.
Regarding the interventions’ effectiveness, the included studies revealed many differences which were based on several factors like intervention type, study quality, sample characteristics, and assessment instruments which will be discussed in the following.
Intervention type
LSM is a complex construct. According to previous studies, a large number of interdisciplinary factors affect life-space mobility in older adults [62,63,64,65]. These factors range from physical and cognitive abilities, over various psychological factors like fear of falling and self-efficacy, to diverse environmental factors. Thus, a single-dimension intervention approach does not seem to be appropriate to address the multifaceted nature of LSM. Thereby, it appears that the integration of physical exercises/physiotherapy is essential. This is consistent with other studies that have found physical factors to be most, but not solely associated with LSM [2, 12] and in agreement with this review’s findings that multidisciplinary approaches seem to be the most effective to increase LSM.
This positive effect of multidimensional interventions might, however, be dependent on the participants’ cognitive status. Tanaka et al. [42] analyzed people suffering from dementia who were apparently less responsive to such treatments. This is also indicated by Shaw et al. [66] and by “The American Geriatrics Society/British Society (AGS/BGS) guideline” [67], which does recommend multifactorial interventions, but regarding the components of the intervention, it clearly differentiates between community-dwelling older people, persons in long-term care, and persons in acute hospital settings.
Furthermore, differences were detected among the mono-factorial approaches, especially concerning physical exercise interventions. Studies like Matsuda et al. [44] and Nakagawa et al. [45] applied more complex physical exercise training, (i.e., a combination of muscle strengthening, balance training and/or stretching exercises and/or different walking tasks) and – unlike simpler physical activity programs [51, 52] - demonstrated significant effects on LSM. So again, multicomponent approaches targeting various physical skills showed more positive results emphasizing the complex physical challenges everyday mobility poses on older adults.
A systematic review by Ross et al. [68] attempted to investigate all possible interventions to maintain mobility, whereby they defined mobility as “any objective or self-report measure of every activity as it relates to the purposeful movement of an individual through physical space” – a definition which encompasses but does not focus on life-space mobility. Most importantly, similar to the findings of the current review, they found mixed results of physical activity intervention studies, but positive outcomes of multicomponent training interventions.
The same applied to purely counseling interventions. Two studies [43, 56] conducted interventions involving multiple components like group sessions, self-planning and counseling, which led to mixed, respectively positive results. On the contrary, interventions mainly based on only self-care tools [54] or phone calls plus supportive materials [55] did not show any effects. This matches again with the review of Ross et al. [68] who found mixed results concerning the effect of educational interventions on several mobility outcomes. They suggest that interventions tailored to specific participant characteristics are more likely to be effective. Another point to consider is obviously the social aspect and the group effect, which have proven to have a positive influence on adherence [69, 70].
Interventions designed for very specific target groups which involved wheelchair adaptions [60], a horticultural program [53], and music therapy [59] did not show significant effects on LSM. This indicates again that these specific interventions are not able to cover all relevant aspects of the complexity of LSM, especially considering that these topics do not or only vaguely touch LSM.
Correspondingly, a very strongly distinguishing factor is the assignment of LSM as either primary or secondary outcome of the respective study. It is striking that the vast majority of the studies analyzing LSM as primary outcome showed positive effects, whereas studies which treated LSM as a secondary outcome did not. The interventions of the latter group were not primarily designed for an improvement of LSM and were consequently too unspecific.
Study quality
Only seven studies [36, 45,46,47,48,49, 56] revealed both, a “good” quality and at the same time significant improvements in LSM. It is striking that all but two [45, 56] of these seven studies applied multidimensional treatments and that apart from Uemura et al. [56], all of them analyzed LSM as a primary outcome. Due to their good quality, these studies can be considered potentially the most effective and meaningful intervention approaches. Thus, the special role of multidimensional and outcome specific interventions is even more highlighted. Nevertheless, the number of good-quality studies is still too low to draw robust conclusions about statements regarding suitable interventions to increase LSM in older people.
Time frame
The duration of the intervention period did not seem to have an influence on LSM. Studies with both shorter (4 weeks) [46] and longer (12 month) [49] intervention periods brought forth significant improvements in LSM, which indicates that the intervention type rather than the duration of the intervention determines the older adults’ adherence to the programs and their responsiveness.
However, regardless of the duration of the intervention period and regardless of other factors like the type of intervention, the sustainability of positive outcomes is an occurring issue which needs to be addressed [41, 46, 48, 58]. For instance, a continuous therapeutical intervention program or a continuous supervision of home-based exercises after the intervention program must be offered to prevent a decline in LSM.
Sample characteristics
Only an insignificant number of studies (n = 4) had a male predominance. This is in line with a previous review observing a female predominance in intervention studies [71]. Therefore, no conclusions regarding an influence of gender in the effect of the interventions can be drawn. Previous research, however, suggests a relationship between gender and LSM in older adults with women having a more restricted LSM [72, 73]. Therefore, women may have more room for improvement and thus may be more likely to benefit from LSM interventions.
Looking at the different study populations, it is apparent that all groups benefited most from multidimensional interventions. Furthermore, the results of this review show a slight tendency that healthy and community-dwelling older adults are less responsive to the interventions than nursing home residents or older adults with severe mobility limitations. Nakagawa et al. [45], for instance, performed a simple physical exercise program combined with home training and compared non-frail and frail older people. Only the latter group could significantly enhance their LSM. One explanation why LSM did not improve in the healthy group might be a ceiling effect of the assessment tool (LSA). At baseline, the healthy older adults reached an average score of 74.4 ± 16.1 points, which was significantly higher than the average LSA score found in other studies. However, more likely, it indicates that physical performance was not the main mobility-limiting factor in the healthy group as it was in the frail group. Lifestyle interventions such as motivational training or knowledge-building aspects might have produced better results for the group without mobility impairments. All in all, the effect of interventions seems to be indirectly related to participants’ health status, degree of independence (e.g., institutionalized or community-dwelling), and mobility limitations.
Assessment tools
Objective measurement methods (GPS and indoor wireless sensor network) for surveying the effectiveness of interventions to increase LSM are severely underrepresented (n = 2) [34, 41]. Still, both studies using objective methods resulted in an improvement in LSM. Questionnaires like the LSA have the advantage of covering mobility independence respectively need for assistance which might be relevant for frail people. However, due to the potential “recall bias” and social desirability bias when answering questionnaires, objective survey methods have a higher validity [74, 75] and should theoretically be applied more often [76]. It must be considered, though, that devices that enable objective LSM mobility assessments usually come with higher costs than simple self-reported questionnaires and often show lower acceptance rates (especially in cases where additional devices need to be used for study purposes other than the ones participants already carry for their personal use,e.g., their own smartphones), hence their sparse use in intervention studies so far. Technological advancements will inevitably lead to more frequent use of objective assessment tools which will then enable a more fine-grained analysis of LSM [77] and it will be interesting to see whether the results of intervention approaches in the future will be in line with the results presented here.
External confounders
Some of the included studies [40, 47, 49, 50] adjusted for person-specific covariates like age, gender, BMI, race, and living situation. However, previous research could show that external factors like seasons and especially cold weather also have an important impact on life-space mobility which is even more pronounced in older adults [78]. Only a few studies included in this review such as Levasseur et al. [43] explicitly suspected a seasonal influence on the change of LSM in their participants. Some other studies [45, 55, 58] also highlighted the importance of considering seasonal and weather effects when analyzing LSM, however, none of them integrated these factors or other potential external confounders in their analyses.
Limitations
This systematic scoping review is of rather narrative nature and provides a more qualitative than quantitative evaluation of intervention effects on LSM. Scarcity of intervention studies aimed at improving LSM currently does not allow meta-analytical approaches but given that this field of work’s current increasing relevance, more studies can be expected. This will allow future meta-analysis to make a more robust statement regarding which interventions yield the best results for the increase of LSM in older adults. Although PubMed and Web of Science are very exhaustive and popular databases, it could still be that some studies were missed.
Conclusions
Interdisciplinary intervention approaches comprising physical exercise combined with counseling or educational interventions seem to have the highest potential for the improvement of LSM in older adults. As expected, individuals with poorer health and/or mobility limitations tend to profit more from such interventions compared to healthier individuals without mobility impairments. Considering that an increase in LSM is beneficial even for individuals without restricted LSM in order to build a reserve against a loss of mobility and the associated negative consequences, it remains interesting to see whether interventions targeting specifically high-functioning individuals would have additional advantages in their quality of life.
Naturally, the most effective interventions are the ones that are specifically designed to improve LSM. In addition, it has been shown that most effective interventions at least partly included physical performance training. However, according to the results of this review and to previous studies, physical factors are especially, but not solely associated with LSM, which is why counseling and educational interventions must also be regarded as an important part of multifactorial interventions for different target groups.
The current empirical evidence is still too small for profound recommendations concerning the most appropriate intervention strategies for the respective target groups, but future meta-analyses will be helpful to provide a quantitative evaluation of LSM enhancing interventions once possible.
Data availability
All data analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- GPS:
-
Global Positioning System
- HBMA:
-
Homebound Mobility Assessment
- LSA:
-
Life-Space Assessment
- LSM:
-
Life-Space Mobility
- LSQ:
-
Life-Space Questionnaire
- NIH:
-
National Institutes of Health
- NHLSD:
-
Nursing Home Life-Space Diameter
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews
- RCT:
-
Randomized Controlled Trial
References
Munch M, Weibel R, Sofios A, Huang H, Infanger D, Portegijs E, et al. MOBIlity assessment with modern TEChnology in older patients’ real-life by the General Practitioner: the MOBITEC-GP study protocol. BMC Public Health. 2019;19:1703.
Giannouli E, Fillekes MP, Mellone S, Weibel R, Bock O, Zijlstra W. Predictors of real-life mobility in community-dwelling older adults: an exploration based on a comprehensive framework for analyzing mobility. Eur Rev Aging Phys Act. 2019;16:1–13.
Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50:443–50.
Taylor JK, Buchan IE, van der Veer SN. Assessing life-space mobility for a more holistic view on wellbeing in geriatric research and clinical practice. Aging Clin Exp Res. 2018;31:439–45.
May D, Nayak USLSL, Isaacs B. The life-space diary: a measure of mobility in old people at home. Disabil Rehabil. 1985;7:182–6.
Peel C, Sawyer Baker P, Roth DL, Brown CJ, Brodner EV, Allman RM, et al. Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85:1008–119.
Caldas V, Fernandes J, Vafaei A, Gomes C, Costa J, Curcio C, et al. Life-Space and Cognitive decline in older adults in different Social and Economic Contexts: longitudinal results from the IMIAS Study. J Cross Cult Gerontol. 2020;35:237–54.
Silberschmidt S, Kumar A, Raji MM, Markides K, Ottenbacher KJ, Al Snih S. Life-space mobility and cognitive decline among Mexican Americans aged 75 years and older. J Am Geriatr Soc. 2017;65:1514–20.
Perracini MR, de Amorim JSC, Lima CA, da Silva A, Trombini-Souza F, Pereira DS et al. Impact of COVID-19 pandemic on life-space mobility of older adults living in Brazil: REMOBILIZE Study. Front PUBLIC Heal. 2021;9.
Sheets KM, Kats AM, Langsetmo L, Mackey D, Fink HA, Diem SJ, et al. Life-space mobility and healthcare costs and utilization in older men. J Am Geriatr Soc. 2021;69:2262–72.
Hardy SE, Kang Y, Studenski SA, Degenholtz HB. Ability to walk 1/4 mile predicts subsequent disability, mortality, and health care costs. J Gen Intern Med. 2011;26:130–5.
Takemoto M, Carlson JA, Moran K, Godbole S, Crist K, Kerr J. Relationship between objectively measured transportation behaviors and health characteristics in older adults. Int J Environ Res Public Health. 2015;12:13923–37.
James BD, Boyle PA, Buchman AS, Barnes LL, Bennett DA. Life space and risk of alzheimer disease, mild cognitive impairment, and cognitive decline in old age. Am J Geriatric Psychiatry. 2011;19:961–9.
Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, Allman RM, et al. Life-space and cognitive decline in a community-based sample of african american and caucasian older adults. Journals Gerontol - Ser A Biol Sci Med Sci. 2008;63:1241–5.
Bentley JP, Brown CJ, McGwin G, Sawyer P, Allman RM, Roth DL. Functional status, life-space mobility, and quality of life: a longitudinal mediation analysis. Qual Life Res. 2013;22:1621–32.
Rantakokko M, Portegijs E, Viljanen A, Iwarsson S, Kauppinen M, Rantanen T. Changes in life-space mobility and quality of life among community-dwelling older people: a 2-year follow-up study. Qual Life Res. 2016;25.
Portegijs E, Rantakokko M, Viljanen A, Sipilä S, Rantanen T. Is frailty associated with life-space mobility and perceived autonomy in participation outdoors? A longitudinal study. Age Ageing. 2016;45:550–3.
Sheppard KD, Sawyer P, Ritchie CS, Allman RM, Brown CJ. Life-space mobility predicts nursing home admission over 6 years. J Aging Health. 2013;25:907–20.
Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older Population. J Am Geriatr Soc. 2000;48:493–8.
Boyle PA, Buchman AS, Barnes LL, James BD, Bennett DA. Association between life space and risk of mortality in advanced age. J Am Geriatr Soc. 2010;58:1925–30.
Mackey DC, Cauley JA, Barrett-Connor E, Schousboe JT, Cawthon PM, Cummings SR. Life-space mobility and mortality in older men: a prospective cohort study. J Am Geriatr Soc. 2014;62:1288–96.
Sverdrup K, Bergh S, Selbæk G, Røen I, Kirkevold Ø, Tangen GG. Mobility and cognition at admission to the nursing home - A cross-sectional study. BMC Geriatr. 2018;18:1–8.
Kuspinar A, Verschoor CP, Beauchamp MK, Dushoff J, Ma J, Amster E, et al. Modifiable factors related to life-space mobility in community-dwelling older adults: results from the canadian longitudinal study on aging. BMC Geriatr. 2020;20:1–12.
Saajanaho M, Rantakokko M, Portegijs E, Törmäkangas T, Eronen J, Tsai LT, et al. Personal goals and changes in life-space mobility among older people. Prev Med (Baltim). 2015;81:163–7.
Poranen-Clark T, Von Bonsdorff MB, Rantakokko M, Portegijs E, Eronen J, Pynnönen K, et al. The temporal association between executive function and life-space mobility in Old Age. Journals Gerontol - Ser A Biol Sci Med Sci. 2018;73:835–9.
Siltanen S, Portegijs E, Saajanaho M, Poranen-Clark T, Viljanen A, Rantakokko M, et al. The combined effect of lower extremity function and cognitive performance on Perceived walking ability among older people: a 2-Year follow-up study. JOURNALS Gerontol Ser A-BIOLOGICAL Sci Med Sci. 2018;73:1568–73.
Tsai LT, Portegijs E, Rantakokko M, Viljanen A, Saajanaho M, Eronen J, et al. The association between objectively measured physical activity and life-space mobility among older people. Scand J Med Sci Sport. 2015;25:e368–73.
Hayashi C, Tanaka H, Ogata S. Assessing timewise changes over 15 months in life-space mobility among community-dwelling elderly persons. BMC Geriatr. 2020;20:502.
Armstrong R, Hall BJ, Doyle J, Waters E. Scoping the scope” of a cochrane review. J Public Health (Bangkok). 2011;33:147–50.
Tricco AC, Lillie E, Zarin W, O´Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMAScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–73.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:1–10.
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, Mcewen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5:371–85.
National Institutes of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. 2014. https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort.
Crist K, Jankowska MM, Schipperijn J, Rosenberg DE, Takemoto M, Zlatar ZZ et al. Change in GPS-assessed walking locations following a cluster-randomized controlled physical activity trial in older adults, results from the MIPARC trial. Heal Place. 2021;69 April:102573.
Kamioka Y, Miura Y, Matsuda T, Iijima Y, Suzuki A, Nakazato K, et al. Changes in social participation and life-space mobility in newly enrolled home-based rehabilitation users over 6 months. J Phys Ther Sci. 2020;32:375–84.
Todo E, Higuchi Y, Ueda T, Murakami T, Kozuki W. A 3-month multicomponent home-based rehabilitation program for older people with restricted life-space mobility: a pilot study. J Phys Ther Sci. 2021;33:158–63.
Tay L, Tay EL, Mah SM, Latib A, Ng YS. Intrinsic capacity rather than intervention exposure influences reversal to robustness among prefrail community-dwelling older adults: a non-randomized controlled study of a multidomain exercise and nutrition intervention. Front Med. 2022;9.
Jensen GL, Roy M-A, Buchanan AE, Berg MB. Weight loss intervention for obese older women: improvements in performance and function. Obes Res. 2004;12:1814–20.
Kato K, Yoshimi T, Aimoto K, Sato K, Itoh N, Kondo I. A rise-assisting robot extends life space and improves facial expressions of nursing home residents. BMC Health Serv Res. 2022;22:1588.
Hiyama Y, Kamitani T, Mori K. Effects of an intervention to Improve Life-Space mobility and self-efficacy in patients following total knee arthroplasty. J Knee Surg. 2019;32:966–71.
Jansen CP, Diegelmann M, Schilling OK, Werner C, Schnabel EL, Wahl HW, et al. Pushing the Boundaries: a physical activity intervention extends sensor-assessed life-space in nursing home residents. Gerontologist. 2018;58:979–88.
Tanaka S, Yamagami T, Yamaguchi H. Effects of a group-based physical and cognitive intervention on social activity and quality of life for elderly people with dementia in a geriatric health service facility: a quasi-randomised controlled trial. Psychogeriatrics. 2021;21:71–9.
Levasseur M, Filiatrault J, Larivière N, Trépanier J, Lévesque M-H, Beaudry M, et al. Influence of Lifestyle Redesign(®) on Health, Social Participation, Leisure, and mobility of older French-Canadians. Am J Occup Ther Off Publ Am Occup Ther Assoc. 2019;73:7305205030p1–18.
Matsuda K, Ikeda S, Nakahara M, Ikeda T, Okamoto R, Kurosawa K, et al. Factors affecting the coefficient of variation of stride time of the elderly without falling history: a prospective study. J Phys Ther Sci. 2015;27:1087–90.
Nakagawa K, Inomata N, Konno Y, Nakazawa R, Hagiwara K, Sakamoto M. The characteristic of a simple Exercise Program under the instruction of physiotherapists-for General Elderly People and Frail Elderly People. J Phys Ther Sci. 2008;20:197–203.
Crotty M, Killington M, Liu E, Cameron ID, Kurrle S, Kaambwa B, et al. Should we provide outreach rehabilitation to very old people living in nursing care Facilities after a hip fracture? A randomised controlled trial. Age Ageing. 2019;48:373–80.
Brown CJ, Foley KT, Lowman JDJ, MacLennan PA, Razjouyan J, Najafi B, et al. Comparison of posthospitalization function and community mobility in Hospital mobility program and Usual Care Patients: a Randomized Clinical Trial. JAMA Intern Med. 2016;176:921–7.
Ullrich P, Werner C, Bongartz M, Eckert T, Abel B, Schönstein A, et al. Increasing life-space mobility in community-dwelling older persons with cognitive impairment following rehabilitation: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2020. https://doi.org/10.1093/gerona/glaa254.
Fairhall N, Sherrington C, Kurrle SE, Lord SR, Lockwood K, Cameron ID. Effect of a multifactorial interdisciplinary intervention on mobility-related disability in frail older people: randomised controlled trial. BMC Med. 2012;10.
Liu M, Xue Q-LL, Gitlin LN, Wolff JL, Guralnik J, Leff B, et al. Disability Prevention Program improves Life-Space and Falls Efficacy: a Randomized Controlled Trial. J Am Geriatr Soc. 2021;69:85–90.
Collins KJ, Schrack JA, VanSwearingen JM, Glynn NW, Pospisil MC, Gant VE, et al. Randomized Controlled Trial of Exercise to improve walking energetics in older adults. Innov aging. 2018;2:1–10.
Hewitt J, Goodall S, Clemson L, Henwood T, Refshauge K. Progressive Resistance and Balance Training for Falls Prevention in Long-Term residential aged care: a Cluster Randomized Trial of the Sunbeam Program. J Am Med Dir Assoc. 2018;19:361–9.
Makizako H, Tsutsumimoto K, Doi T, Makino K, Nakakubo S, Liu-Ambrose T et al. Exercise and Horticultural Programs for older adults with depressive symptoms and memory problems: a Randomized Controlled Trial. J Clin Med. 2019;9.
Kamga H, McCusker J, Yaffe M, Sewitch M, Sussman T, Strumpf E, et al. Self-care tools to treat depressive symptoms in patients with age-related eye disease: a randomized controlled clinical trial. Clin Exp Ophthalmol. 2017;45:371–8.
Siltanen S, Portegijs E, Pynnönen K, Hassandra M, Rantalainen T, Karavirta L, et al. Effects of an individualized active aging counseling intervention on mobility and physical activity: secondary analyses of a Randomized Controlled Trial. J Aging Health. 2020;32:1316–24.
Uemura K, Yamada M, Okamoto H. The effectiveness of an active learning program in promoting a healthy lifestyle among older adults with low health literacy: a Randomized Controlled Trial. Gerontology. 2021;67:25–35.
Swan F, English A, Allgar V, Hart SP, Johnson MJ. The hand-held fan and the calming hand for people with chronic breathlessness: a feasibility trial. J Pain Symptom Manage. 2019;57:1051–1061e1.
Liddle J, Haynes M, Pachana NA, Mitchell G, McKenna K, Gustafsson L. Effect of a Group intervention to promote older adults’ Adjustment to Driving Cessation on Community mobility: a Randomized Controlled Trial. Gerontologist. 2014;54:409–22.
Murabayashi N, Akahoshi T, Ishimine R, Saji N, Takeda C, Nakayama H, et al. Effects of Music Therapy in Frail Elderlies: controlled crossover study. Dement Geriatr Cogn Dis Extra. 2019;9:87–99.
Brienza DM, Karg PE, Bertolet M, Schmeler M, Poojary-Mazzotta P, Vlachos H, et al. A Randomized Clinical Trial of Wheeled mobility for pressure Injury Prevention and better function. J Am Geriatr Soc. 2018;66:1752–9.
Fairhall N, Sherrington C, Lord SR, Kurrle SE, Langron C, Lockwood K, et al. Effect of a multifactorial, interdisciplinary intervention on risk factors for falls and fall rate in frail older people: a randomised controlled trial. Age Ageing. 2014;43:616–22.
Zijlstra W, Giannouli E. Mobility in community-dwelling older adults; what are its determinants? BMC Geriatr. 2021;21:228.
Giannouli E, Bock O, Mellone S, Zijlstra W. Mobility in Old Age: Capacity Is Not Performance. Biomed Res Int. 2016;2016.
Giannouli E, Bock O, Zijlstra W. Cognitive functioning is more closely related to real-life mobility than to laboratory-based mobility parameters. Eur J Ageing. 2018;15:57–65.
Seinsche J, Zijlstra W, Giannouli E. Motility in Frail older adults: operationalization of a New Framework and First Insights into its relationship with physical activity and life-space mobility: an exploratory study. Int J Environ Res Public Health. 2020;17.
Shaw FE, Bond J, Richardson DA, Dawson P, Nicholas Steen I, McKeith IG, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: Randomised controlled trial. Br Med J. 2003;326:73–5.
American Geriatrics Society, Society BG, American Academy of Orthopaedic Surgeons Panel on Fall Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49:664–72.
Ross LA, Schmidt EL, Ball K. Interventions to maintain mobility: what works? Accid Anal Prev. 2013;61:167–96.
Killingback C, Tsofliou F, Clark C. Older people’s adherence to community-based group exercise programmes: a multiple-case study. BMC Public Health. 2017;17:1–12.
Brawley LR, Rejeski WJ, Lutes L. A group-mediated cognitive-behavioral intervention for increasing adherence to physical activity in older adults. J Appl Biobehav Res. 2000;5:47–65.
van der Bij AK, Laurant MGH, Wensing M. Effectiveness of physical activity - A review. Am J Prev Med. 2002;22.
Snih S, Al, Peek KM, Sawyer P, Markides KS, Allman RM, Ottenbacher KJ. Life-space mobility in Mexican Americans aged 75 and older. J Am Geriatr Soc. 2012;60:532–7.
Choi M, O’Connor ML, Mingo CA, Mezuk B. Gender and racial disparities in life-space constriction among older adults. Gerontologist. 2016;56:1153–60.
Birenboim A, Shoval N. Mobility research in the age of the smartphone. Ann Am Assoc Geogr. 2016;106:283–91.
Blanchard RA, Myers AM, Porter MM. Correspondence between self-reported and objective measures of driving exposure and patterns in older drivers. Accid Anal Prev. 2010;42:523–9.
Fillekes MP, Kim EK, Trumpf R, Zijlstra W, Giannouli E, Weibel R. Assessing older adults’ daily mobility: a comparison of GPS-derived and self-reported mobility indicators. Sens (Switzerland). 2019;19.
Fillekes MP, Giannouli E, Kim E-K, Zijlstra W, Weibel R. Towards a comprehensive set of GPS-based indicators reflecting the multidimensional nature of daily mobility for applications in health and aging research. Int J Heal Geogr 2019 181. 2019;18:17.
Portegijs E, Iwarsson S, Rantakokko M, Viljanen A, Rantanen T. Life-space mobility assessment in older people in finland; measurement properties in winter and spring. BMC Res Notes. 2014;7:1–9.
Acknowledgements
Not applicable.
Funding
Open access funding provided by Swiss Federal Institute of Technology Zurich. This work was supported by the Velux Stiftung [Project No. 1155], to [TH], and institutional budget of [WZ].
Author information
Authors and Affiliations
Contributions
EG conceptualized the study. EG, CPJ, WZ and TH created the methodology. JS and SR were responsible for study screening, data extraction and analysis. JS and EG prepared the original draft. EG, CPJ, WZ and TH performed the writing-review and editing. EG supervised the study. TH and WZ were responsible for funding. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Seinsche, J., Jansen, CP., Roth, S. et al. Multidimensional interventions to increase life-space mobility in older adults ranging from nursing home residents to community-dwelling: a systematic scoping review. BMC Geriatr 23, 412 (2023). https://doi.org/10.1186/s12877-023-04118-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04118-3