Abstract
Background
Falls are a leading cause for emergency department (ED) visits in older adults. As a fall is associated with a high risk of functional decline and further falls and many falls do not receive medical attention, the ED is ideal to initiate secondary prevention, an opportunity generally not taken. Data on trajectories to identify patients, who would profit the most form early intervention and to examine the impact of a fall event, are lacking. To tailor interventions to the individual’s needs and preferences, and to address the whole scope of fall risks, we developed this longitudinal study using an extensive assessment battery including dynamic balance and aerobic fitness, but also sensor-based data. Additionally, participative research will contribute valuable qualitative data, and machine learning will be used to identify trips, slips, and falls in sensor data during daily life.
Methods
This is a mixed-methods study consisting of four parts: (1) an observational prospective study, (2) a randomized controlled trial (RCT) to explore whether a diagnostic to measure reactive dynamic balance influences fall risk, (3) machine learning approaches and (4) a qualitative study to explore patients’ and their caregivers’ views. We will target a sample size of 450 adults of 60 years and older, who presented to the ED of the Klinikum Oldenburg after a fall and are not hospitalized. The participants will be followed up over 24 months (within four weeks after the ED, after 6, 12 and 24 months). We will assess functional abilities, fall risk factors, participation, quality of life, falls incidence, and physical activity using validated instruments, including sensor-data. Additionally, two thirds of the patients will undergo intensive testing in the gait laboratory and 72 participants will partake in focus group interviews.
Discussion
The results of the SeFallED study will be used to identify risk factors with high predictive value for functional outcome after a sentinel fall. This will help to (1) establish a protocol adapted to the situation in the ED to identify patients at risk and (2) to initiate an appropriate care pathway, which will be developed based on the results of this study.
Trial registration
DRKS (Deutsches Register für klinische Studien, DRKS00025949). Prospectively registered on 4th November, 2021.
Similar content being viewed by others
Background
Falls are a main reason for emergency department (ED) visits in older adults [1]. Around 33% of community-dwelling older adults fall at least once a year with many of them becoming recurrent fallers [2, 3]. Falls diminish quality of life and increase mortality and morbidity [4]. As fall incidence and severity rise with age, falls will continue to be a burden for healthcare systems worldwide, especially in the context of the demographic change [3, 5].
Numerous risk factors for falls have been identified such as age, sex, cognitive decline, vertigo, muscle weakness, (dynamic) balance dysfunction, or polypharmacy [6,7,8,9]. Consequences of falls include physical as well as psychosocial sequelae. Physically, about 14% of falls lead to fractures, and around 10% of falls result in traumatic head injuries [10, 11]. Psychosocially, falls may cause fear of falling, which is a relevant fall risk factor itself, with prevalence ranging between 30 to 73% [12, 13]. Fear of falling may result in reduced physical activity [14], and affect social participation, thus, increasing the risk of social isolation and loss of independence [15, 16]. Therefore, the manifold consequences of falls do not only impair quality of life, but also increase the risk of further diseases and disorders such as depression and dementia [16,17,18], potentially forming a vicious circle.
Individuals presenting to the ED with a fall, who are directly discharged, are an easy to identify, but yet understudied high-risk group for further falls and functional decline [19, 20]. To optimize patient care, it is crucial to initiate secondary prevention programs for these individuals as they seek medical attention in the ED. Long term observation of this group may enable the identification of different functional trajectories [20, 21], thereby providing a solid basis for well-founded decision-making, and tailored falls prevention interventions in the future.
To identify functional trajectories, a comprehensive geriatric assessment is needed, whose informative value can be improved by modern sensor technology. Further, an in-depth analysis of fall risk factors is mandatory. As dynamic reactive balance and aerobic fitness are not only discussed to be relevant fall risk factors but may also present treatment targets for future trials, they should be included in such an assessment battery. Dynamic balance dysfunctions are known to increase fall risk [7,8,9]. However, previous research indicates that even a single perturbation-based dynamic balance session influences functional trajectories and fall risk positively [22]. Therefore, observational studies using perturbation to assess dynamic balance have to control for potentially confounding effects of such a diagnostic session. The role of aerobic fitness as a risk factor is less clear and its association with static balance mostly based on cross-sectional findings [23, 24], making it a promising research target for longitudinal studies.
The worrying sequelae of falls for the individual but also their societal impact, call for action to strengthen and establish effective prevention programs, promoting high compliance of the participants [25]. Here, it is essential to take the populations’ specific needs into account. Patient-centered approaches have gained importance to identify potential barriers and facilitators to ensure adherence to such programs [26]. Therefore, exploring patients’ and their caregivers’ views on falls prevention seems crucial to build a realistic foundation for tailored intervention programs [27, 28].
The SeFallED study aims to identify long-term trajectories of older adults, presenting to the ED without hospital admission, after a sentinel fall. The study will combine geriatric assessments, sensor data and machine learning approaches. Further, the prognostic value of different, so far rarely studied risk factors such as aerobic fitness and dynamic reactive balance in predicting the trajectories, while controlling for potentially confounding effects of the respective risk factor assessments will be analyzed. Finally, these results will be combined with information on individual barriers, preferences and needs from the patients’ and caregivers’ perspectives to select and evolve adequate fall prevention programs in the future.
Methods/design
Study design
This study protocol describes a mixed-methods study, consisting of four parts: (1) an observational prospective study to identify different trajectories of performance on activities of daily living, (2) a randomized controlled trial using a parallel group design (1:1) to explore whether a diagnostic to measure reactive dynamic balance influences fall risk, (3) machine learning a) to record data using inertial measurement units (IMU) and (depth-) cameras of human reactions to standardized perturbations in order to train classifiers and b) to identify slips, trips, and falls from IMU sensor data in real life, and (4) a qualitative study to explore patients’ and their caregivers’ views on falls prevention to identify facilitators and barriers for future interventions [29]. A patient advisory board consisting of older adults that have experienced fall(s) will accompany this study.
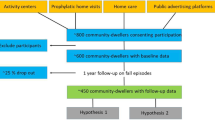
The study will be conducted at the Carl von Ossietzky University in Oldenburg, Germany from October 2021 until January 2024, in accordance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of the University of Oldenburg (number 2021 – 120). All participants will provide written informed consent to participate in the study. The consent forms are designed to be signed by either the participant or if needed by the participant and his / her legal guardian or family member. Ethical guidelines for research conducted with adults that lack the capacity to give consent will be followed and include the principle of group, the subsidiarity principle and the minimal risk standard [30]. Further, study information has been adapted to facilitate the participant’s understanding of the study, which will be provided in addition to the regular consent form, if necessary. Figure 1 shows the study design in a flow diagram.
Participants and recruitment
It is the aim to recruit 450 older adults, who meet the following inclusion criteria: 1) age 60 years or above, 2) presented to the ED of the Klinikum Oldenburg after a fall and were discharged within 72 h, 3) informed consent.
Exclusion criteria are as follows: 1) life expectancy of less than 3 months, 2) unstable medical, neurological or psychiatric condition, 3) bedridden or being unable to walk without support of another person, 4) residence more than 20 km away from the research center, 5) acute psychosis or social aggression, 6) inability to communicate verbally in German or English. Furthermore, participants that 1) are completely dependent on walking aids 2) or subjectively not able to walk 400 m in less than 5 min will be included in the observational part of the study but deemed ineligible for visiting the gait laboratory.
A study nurse will be present at the ED from Monday to Friday during regular working hours and address all suitable individuals to obtain written consent for further contact. These individuals will be contacted within a week of their visit to the ED to schedule an appointment for the first home assessment during which written consent for participation will be provided. The staff in the ED will hand out flyers with relevant information for participation and contact data outside regular working hours of the study nurse. Recruitment will be ongoing between October 2021 and January 2023.
Randomization and blinding
Two thirds of the 450 participants will take part in the tests in the gait laboratory. To control for the potential influence of assessing dynamic balance, these 300 participants will be randomly allocated to either a perturbation or no perturbation group using a 1:1 ratio block randomization. Randomization will be stratified in four different strata based on sex (male / female) and cognitive status (normal / impaired). We will stratify participants into cognitively normal and cognitively impaired using the result of the Montreal Cognitive Assessment (MoCA) at the first home visit. The chosen cutoff of ≤ 24 points increases sensitivity and specificity of the MoCA and reduces false positive results [31,32,33]. The randomization lists will be prepared by an independent statistician and will not be accessible by the persons enrolling the subjects into the study. The lists will be stored on a secured data server and protected by a password only known by the principal and co-investigators. Assessors of functional performance and falls risk factors will be blinded to allocation.
Data assessment
Data will be collected at the ED, in participants’ homes and at the gait laboratory. Furthermore, IMUs to measure physical activity as well as gait parameters will be worn by the participants during daily life over 7 days at each time point (T1 – T4). After the initial assessment, the researchers maintain contact with the participants through monthly phone calls, as part of the prospective falls recording in addition to fall calendars (Fig. 1). Within four weeks after presenting to the ED, participants will be visited at home for the first functional assessment (T1), which will be repeated after 6 (T2), 12 (T3) and 24 (T4) months. Besides the data collected during the home assessments, eligible participants will attend testing in the university’s gait laboratory. This appointment will preferably be scheduled a week after the respective home assessments.
Outcome measures
Emergency department
All older patients in the ED are regularly assessed with a geriatric screening ‘Geriatrisches Screening bei Klinikaufnahme’ (Supplementary file 1), which consists of six yes / no questions with a higher score predicting a poor outcome and the need for co-management or treatment by a geriatric team. Furthermore, all participants will be assessed for delirium using the Confusion Assessment Method (CAM) for Intermediate Care (CAM-IMC), which has shown better sensitivity and specificity in comparison to the widely used CAM for Intensive Care Unit (CAM-ICU) and includes the Richmond Agitation-Sedation Scale [34,35,36]. From the chart data chronic diseases and medication will be extracted to complement information given by the participant as soon as consent is provided. In addition, routinely drawn blood samples will be stored for further analyses of biomarkers.
Home assessment
After providing written consent to participate in the study, participants’ characteristics (age, sex, education, number and name of medications, pre-existing illnesses including joint replacements, smoking status, alcohol consumption, the use of hearing, seeing, and walking aids, and the living situation (e.g., alone, in a care facility) will be assessed. Additionally, the participants will be asked for detailed information on the recent fall that led to the visit at the ED, including time of the fall, location, and activity before falling, direction of the fall, and injuries. For a comprehensive geriatric assessment an extensive assessment battery will be used consisting of standardized, validated and widely used instruments. A detailed overview is given in Table 1.
Gait Laboratory (RCT for effect of perturbation protocol)
Participants will visit the gait laboratory ideally one week after their home assessments. The time between fall and visit to the gait laboratory will be documented. At the lab participants will be equipped with an activity monitor (activPAL©, PAL Technologies Ltd, Glasgow UK) and six wirelessly synchronized IMU’s (Opal V1, Mobility Lab™ (ML), APDM, Inc., Portland, OR, USA) to measure gait characteristics during all the assessments in the laboratory. A flow chart of the assessments, conducted in the gait laboratory, is provided in Fig. 2.
To determine overground walking speed, which will be used for all further assessments at the gait laboratory, participants will walk 3 m twice with the instruction to walk as fast as they can without running, then twice with the instruction to walk with their preferred walking speed. The mean time of the two trials under the same instructions will be taken and used to calculate maximal and preferred overground walking speed in km/h, respectively. To minimize the effect of starting, stopping or turning, 1 m will be added at each end of the walk way.
Reactive dynamic balance
Reactive dynamic balance will be assessed on the M-Gait treadmill (Motek Medical B.V., Amsterdam, the Netherlands), which enables anterior–posterior, medio-lateral and pitch perturbations. The integrated split-belt of the treadmill with separate force plates allows to perturb either both legs or just one leg during walking. The participants are secured using a safety harness.
Familiarization on the treadmill will start at 50% of the preferred overground walking speed. Treadmill walking speed will be gradually increased by 5% every 30 s until the participants will reach either 100% of the previously measured overground walking speed or an individually more preferable walking speed. Familiarization will last 6 min, which is regarded to be sufficient according to previous research [58,59,60]. The final minute of the familiarization will be used to analyze the participants’ gait at the preferred gait speed with the aforementioned sensors (activPAL©, APDMs). Additionally, three Microsoft Kinect Azure cameras (Microsoft, USA) will be used as a motion capture system [61].
After a two-minute break, participants randomized to the no perturbation group will walk twice for 4 min and 30 s with the individually determined treadmill walking speed. Participants will have a two-minute break between the two trials.
Participants randomized to the perturbation group will complete a perturbation protocol with similar duration and break time. The perturbation protocol will start with 30 s of the preferred treadmill walking speed, followed by 9 perturbations randomly presented to the participants. Time between perturbations will vary between 20–30 s, which is deemed a sufficient washout period [62]. Perturbations will be triggered through the integrated force plates at initial foot contact through custom application (D-Flow version 3.34.2, Motek Medical BV, Amsterdam, The Netherlands). Using the split belt option, each leg will be perturbed in anterior–posterior direction twice, mimicking slips and trips. Slips will be simulated by an acceleration of 3 m∙s−2 to a maximum of 180% of treadmill walking speed for 0.42 s. Trips will be provoked similarly with a deceleration of 3 m∙s−2 to a minimum of 40% of treadmill walking speed, which is in line with previous research [58, 59, 63, 64]. Besides these single leg perturbations, an emergency stop as in public transport will be imitated with both belts decelerating by 9 m∙s−2 for 0.12 s [58, 65]. Further, the protocol will include two contralateral sways, perturbing each leg once by a 5-cm platform translation in 3 m∙s−2 [58, 59]. A pitch of + and—5° respectively, with a duration of 1.0 s will imitate small slope changes as present on sidewalks or at bus stops. Gait adaptations to these perturbations will be measured throughout the trials, using the aforementioned systems.
Aerobic fitness
All participants will complete a treadmill test, assessing cardiorespiratory kinetics as an indicator of aerobic fitness [66]. Participants will be equipped with a face mask connected to a mobile system (MetaMax3B, Cortex Biophysik GmbH, Leipzig, Germany) to measure breath-by-breath gas exchange and will wear an ECG belt (CustoGuard belt 3, Customed, Ottobrunn, Germany) to assess beat-to-beat heart rate. The work rate protocol on the treadmill consists of two pseudo random binary sequences [67,68,69] which will change between 50 and 100% of the preferred gait speed, as assessed during familiarization on the treadmill. The protocol to assess aerobic fitness is shown in Fig. 3.
Focus groups
In order to explore patients’ preferences, needs, facilitators and barriers of participating and adhering to falls prevention interventions and to support a patient centered intervention, focus group interviews will be established as part of the project [70]. 72 persons consisting of participants and caregivers will be recruited to join twelve focus groups (k = 6 with patients, k = 6 with caregivers).
Audio data from the focus group interviews will be transcribed verbatim with two multidisciplinary independent researchers analyzing the data. Content analysis according to Kuckartz will be applied with categories such as needs, preferences, barriers and facilitators deductively derived from the Theoretical Domains Framework [71]. Furthermore, categories can be derived inductively from the material recorded [72].
Sensor data acquisition and machine learning
Normal and reactive individual gait patterns are recorded via both, the two activity sensor systems (Inertial Measurement Unit consisting of accelerometer, gyroscopes, and magnetometers—activPAL©, APDM) and the three front-facing depth cameras (Kinect Azure). The camera data are used to identify the spatial–temporal gait parameters and to label the perturbations and the associated reaction strategy. Based on this data, the individual reaction of a subject is identified using the IMU data of the two sensor systems (activPAL©, APDM).
Depending on the degree of homogeneity of the reaction pattern, either general / inter-individual classifiers (high degree of uniformity) can be trained or individual classifiers (high individual characteristics) can be constructed. The derived classifiers will be used to recognize slip, trip, and fall patterns over the time in IMU data during daily life.
Safety
All serious adverse events / adverse events will be recorded on study specific adverse event forms. Overexertion during gait laboratory examinations will be avoided by using the preferred gait of the individual participant on the treadmill. Furthermore, breaks can be extended as needed and participants will be asked regularly if they feel fit to continue. If subjective or objective signs of fatigue or overexertion are seen, the protocol will be immediately interrupted. All adverse events will be reported to the principal investigator.
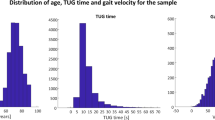
Sample size
The recruitment goal of 450 older adults for the observational part of the study is the result of an analysis of the hospital data base of the Klinikum Oldenburg from the year 2018, which revealed a total of 1.182 patients, presenting to the ED without admission, aged between 60 and 103 years. These patients were registered within the symptom-groups ‘problem of the extremities’, ‘head trauma’ or ‘fall’. We assume that 48% of these patients are ineligible due to in- and exclusion criteria as published by Barker and colleagues and expect a further drop out of 38% due to not giving consent for study participation [73].
An independent biostatistician calculated the sample size for the embedded randomized controlled trial (RCT). Sample size calculation was performed via computer simulations based on the study of Pai and colleagues [22]. The level of significance was set as α = 0.05. As we aim for a power of 80% a sample size of at least N = 245 is required. According to previous research, a dropout of 17% may be expected in this subgroup, which led to the decision to aim for 300 participants [73].
Statistical analysis
The endpoints will be compared between different home assessments: T1 (within 4 weeks), T2 (6 months), T3 (12 months), and the following yearly examinations after ED attendance. The association between multiple variables (e.g. age, time since recruitment etc.) and the trajectories of the different endpoints will be analyzed fitting a linear mixed model (LMM) / generalized linear mixed models, (GLMM, i. e. Logistic, Negative Binomial, Ordinal). For metric endpoints, we will check the normal distribution of the residuals in the corresponding LMM via Lilliefors-Test or descriptively via Skewness. We also plan to analyze stratified models (stratified e.g. by sex and / or initial physical fitness). Regarding the trajectories in the entire group, we will use the Friedman test for metric / ordinal data, if normal distribution of the residuals is not valid. The data obtained during the gait lab visit (gait analysis, aerobic capacity, physical activity) will be compared in a similar fashion. To identify simple predictors of declines in functional performance and physical activity as well as fall risks, that potentially can be obtained directly in the ED or at the general practitioner, regression analysis will be used. Setting parameters of the gait analysis and the cardiorespiratory fitness test as dependent variable and parameters of the home assessments as independent parameters, predictive factors for fall risks will be analyzed. Local significance level will be set to 5%. We will deal with missing value problems via complete Likelihood approach under the missing at random-assumption (MAR) in parametric models.
For the included RCT, we will analyze if a diagnostic perturbation session influences prospective fall risk. We will fit a logistic regression model, and will calculate p-values for coefficients plus estimates of the coefficients plus 95% confidence intervals.
Statistical analyses will be performed according to the ICH Guideline E9 ‘Statistical Principles for Clinical trials’ using validated statistical software (SAS, SPSS, R).
Data management
Data will be managed using unique study codes provided by an independent statistician. These will be used to code and file all electronic information that will be stored on secured university systems. Paper and pencil tests will be stored in a cabinet with a lock. Two different study nurses will enter the data collected from paper and pencil tests into a custom-made Research Electronic Data Capture (REDCap) database hosted at the Carl von Ossietzky University Oldenburg. REDCap is a secure, web-based software platform, designed to support data capture for research studies [74, 75].
Patient and public involvement
A participatory research team (PRT) will be involved as consultants, which was approved by the Medical Ethics Committee of the University of Oldenburg (2021 – 106). The PRT consists of six older adults (66 to 84 years old), who have experienced falls in the past. The group is heterogeneous with regard to sex, age, school education, living situation, and the use of mobility aids.
Approximately 30 meetings between researchers and the PRT will take place throughout the course of the SeFallED study. The PRT will provide feedback for example to the comprehensibility of consent forms, the burden of the assessment batteries, strategies of participant recruitment and the guidelines for the focus group interviews. Further, it is planned to engage the PRT in conducting and analyzing the focus group interviews. All meetings between the PRT and the researchers will be documented with focus on the remarks of the PRT. The PRT’s feedback, and whether and to what extent it will lead to changes in study procedures, will be documented [76, 77]. In addition, researchers and the PRT will fill in the Public and Patient Engagement Evaluation Tool every six months [76, 77]. Members of the PRT will receive an expense allowance of 20€ per hour according to documented working hours, which include meetings and working tasks between meetings.
Discussion
As falls are a major public health problem, the World Health Organization called for effective intervention strategies in their report ‘Step Safely’, published in 2021 [78]. The SeFallED study will aid in developing such strategies by systematically assessing the risk of older adults who presented to the ED after a fall, a group at high risk for further falls [79].
One strength of the SeFallED study is its long observation period (> 12 months), which may be increased by further funding, with yearly follow-up visits and monthly telephone calls. While fall research guidelines demand a prospective data collection for at least up to 12 months [80], it is likely that long-term consequences of a fall may either last well beyond this period or may only manifest after a certain time has passed [81]. Our long-term data will provide better insight and deepen our understanding of the consequences of falls in older adults, which is needed to design tailored interventions and to inform healthcare professionals and policy makers.
Another strength of the SeFallED study is its mixed methods approach, which combines both qualitative and quantitative data and includes machine learning aspects. Whereas quantitative data is needed to calculate risk scores that may facilitate decision making processes in the future, the qualitative approach, involving patients’ representatives, may enhance appropriateness and relevance of the research, and hence the quality of the study [26, 82]. Especially the collaboration with a PRT has shown promise to benefit the research process as well as its outcomes [83]. The potential of smart systems to enhance care for older adults, but also to detect falls or gait insecurities has been acknowledged in previous research [84, 85]. Therefore, adding machine learning to the observational data of older individuals after a sentinel fall, may offer a broad spectrum of innovative approaches in fall risk assessment, but also falls prevention.
The extensive assessment battery with its considerable number of outcome measures will result in a robust data set, and can be considered an additional strength of the SeFallED study. Researchers will work together with the PRT to deliver strategies such as splitting up home assessments into two days in highly vulnerable participants to reduce the participants’ burden, and successfully implement the extensive assessment battery. Furthermore, data collection will be done in the participants’ homes, which may help to alleviate discomfort and stress experienced particularly in laboratory settings. Nevertheless, data collection at home bears the risk of unplanned disturbances affecting the participants’ concentration such as the phone or door bell ringing. Such events will be noted by the assessors and discussed with the principal investigator.
Successful recruitment and adherence are key factors to the success of the study with drop out during the follow-ups presenting a major threat. Therefore, we decided that a study nurse is present in the ED to get into personal contact with potential participants. During the home assessments, the assessors will pay attention to promote a good atmosphere and allow questions and breaks in between assessments. To increase personal contact, which is important to minimize attrition [86], monthly phone calls are planned as part of the project. Furthermore, Christmas and thank you cards will be sent to the participants. Recruitment may be particularly challenging due to the ongoing COVID-19 situation, in which older adults are advised to reduce social contacts. Even though vaccination is available to the target population, the study team will undertake specific COVID-19 measures to increase participation in the study such as wearing FFP2 masks during the assessments, keeping a distance and communicating the vaccination status of the assessors.
The results of the SeFallED study will be used to identify risk factors with high predictive value for functional outcome after a sentinel fall. This will help to (1) establish a protocol adapted to the situation in the ED to identify patients at risk and (2) to initiate an appropriate care pathway, which will be developed based on the results of this study. (3) We will aim to select or (re)design existing interventions and / or develop effective interventions for older adults incorporating novel methods tailored to individual needs, barriers and preferences to lift fall prevention and individual compliance to a new level. (4) Automated falls detection based on machine learning algorithms may be integrated in devices used during daily life such as smart phones or wrist worn activity trackers, and will potentially play a major role in fall related research as well as for patient security in the future.
Availability of data and materials
Not applicable.
Abbreviations
- AG:
-
Aerobic fitness and gait analysis
- AGP:
-
Aerobic fitness, gait analysis, and perturbation based dynamic balance
- CAM:
-
Confusion assessment Method
- DIA-S:
-
Depression in old age scale
- DRKS:
-
Deutsches Register für klinische Studien
- ED:
-
Emergency department
- FES-I:
-
Falls efficacy scale
- FIT:
-
Participants with sufficient walking ability
- GLMM:
-
Generalized linear mixed models
- ICU:
-
Intensive care unit
- IMC:
-
Intermediate care
- IMU:
-
Inertial measurement unit
- LMM:
-
Linear mixed model
- LSA-D:
-
German life space questionnaire
- LUCAS – FI:
-
Longitudinal urban cohort ageing study functional ability index
- MAR:
-
Missing at random
- MoCA:
-
Montreal cognitive assessment
- MoCA-MIS:
-
Montreal cognitive assessment – memory index score
- PRBS:
-
Pseudo random binary sequences
- PRT:
-
Participatory research team
- REDCap:
-
Research electronic capture
- RCT:
-
Randomized controlled trial
- SPPB:
-
Short physical performance battery
- TMT:
-
Trail making test
References
Shankar KN, Liu SW, Ganz DA. Trends and characteristics of emergency department visits for fall-related injuries in older adults, 2003–2010. West J Emerg Med. 2017;18(5):785.
Moreland J, Richardson J, Chan D, O’Neill J, Bellissimo A, Grum R, Shanks L. Evidence-based guidelines for the secondary prevention of falls in older adults. Gerontology. 2003;49(2):93–116.
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl 2:ii37–41.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61.
Houry D, Florence C, Baldwin G, Stevens J, McClure R. The CDC Injury Center’s response to the growing public health problem of falls among older adults. Am J Lifestyle Med. 2016;10(1):74–7.
Zhao YL, Alderden J, Lind BK, Kim H. A Comprehensive Assessment of Risk Factors for Falls in Community-Dwelling Older Adults. J Gerontol Nurs. 2018;44(10):40–8.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–68.
Zhang L, Ding Z, Qiu L, Li A. Falls and risk factors of falls for urban and rural community-dwelling older adults in China. BMC Geriatr. 2019;19(1):379.
Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta-analysis. Arch Gerontol Geriatr. 2013;56(3):407–15.
Rupp M, Walter N, Pfeifer C, Lang S, Kerschbaum M, Krutsch W, Baumann F, Alt V. The Incidence of Fractures Among the Adult Population of Germany - and Analysis From 2009 through 2019. Dtsch Arztebl Int. 2021;118(40):665–9 (Forthcoming).
Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54(10):1590–5.
Li F, Fisher KJ, Harmer P, McAuley E, Wilson NL. Fear of falling in elderly persons: association with falls, functional ability, and quality of life. J Gerontol B Psychol Sci Soc Sci. 2003;58(5):P283-290.
Schoene D, Heller C, Aung YN, Sieber CC, Kemmler W, Freiberger E. A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls? Clin Interv Aging. 2019;14:701–19.
Liu M, Hou T, Li Y, Sun X, Szanton SL, Clemson L, Davidson PM. Fear of falling is as important as multiple previous falls in terms of limiting daily activities: a longitudinal study. BMC Geriatr. 2021;21(1):350.
Hajek A, Konig HH. The association of falls with loneliness and social exclusion: evidence from the DEAS German Ageing Survey. BMC Geriatr. 2017;17(1):204.
Sundstrom A, Adolfsson AN, Nordin M, Adolfsson R. Loneliness Increases the Risk of All-Cause Dementia and Alzheimer’s Disease. J Gerontol B Psychol Sci Soc Sci. 2020;75(5):919–26.
Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. Am J Geriatr Psychiatry. 2013;21(5):484–92.
Rogers NT, Steptoe A, Cadar D. Frailty is an independent predictor of incident dementia: Evidence from the English Longitudinal Study of Ageing. Sci Rep. 2017;7(1):15746.
Russell MA, Hill KD, Blackberry I, Day LL, Dharmage SC. Falls risk and functional decline in older fallers discharged directly from emergency departments. J Gerontol A Biol Sci Med Sci. 2006;61(10):1090–5.
Close JC, Lord SR, Antonova EJ, Martin M, Lensberg B, Taylor M, Hallen J, Kelly A. Older people presenting to the emergency department after a fall: a population with substantial recurrent healthcare use. Emerg Med J. 2012;29(9):742–7.
Jonkman NH, Del Panta V, Hoekstra T, Colpo M, van Schoor NM, Bandinelli S, Cattelani L, Helbostad JL, Vereijken B, Pijnappels M, et al. Predicting Trajectories of Functional Decline in 60- to 70-Year-Old People. Gerontology. 2018;64(3):212–21.
Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69(12):1586–94.
Donath L, Kurz E, Roth R, Hanssen H, Schmidt-Trucksass A, Zahner L, Faude O. Does a single session of high-intensity interval training provoke a transient elevated risk of falling in seniors and adults? Gerontology. 2015;61(1):15–23.
Nagano H, James L, Sparrow WA, Begg RK. Effects of walking-induced fatigue on gait function and tripping risks in older adults. J Neuroeng Rehabil. 2014;11:155.
Liddle J, Lovarini M, Clemson L, Mackenzie L, Tan A, Pit SW, Poulos R, Tiedemann A, Sherrington C, Roberts C, et al. Making fall prevention routine in primary care practice: perspectives of allied health professionals. BMC Health Serv Res. 2018;18(1):598.
Bethell J, Commisso E, Rostad HM, Puts M, Babineau J, Grinbergs-Saull A, Wighton MB, Hammel J, Doyle E, Nadeau S, et al. Patient engagement in research related to dementia: A scoping review. Dementia (London). 2018;17(8):944–75.
Tzeng HM, Yin CY. Patient Engagement in Hospital Fall Prevention. Nurs Econ. 2015;33(6):326–34.
Radecki B, Reynolds S, Kara A. Inpatient fall prevention from the patient’s perspective: A qualitative study. Appl Nurs Res. 2018;43:114–9.
Creswell JW, Creswell JD. Research design: Qualitative, Quantitative, and Mixed Methods approaches. 4th Edition, Sage, Newbury Park. 2017.
Scholten M, Gieselmann A, Gather J, Vollmann J. Advance Research Directives in Germany A Proposal for a Disclosure Standard. Geropsych J Gerontopsychology Geriatr Psychiatry. 2018;31(2):77–86.
Dautzenberg G, Lijmer J, Beekman A. Diagnostic accuracy of the Montreal Cognitive Assessment (MoCA) for cognitive screening in old age psychiatry: Determining cutoff scores in clinical practice. Avoiding spectrum bias caused by healthy controls. Int J Geriatr Psychiatry. 2020;35(3):261–9.
Milani SA, Marsiske M, Cottler LB, Chen X, Striley CW. Optimal cutoffs for the Montreal Cognitive Assessment vary by race and ethnicity. Alzheimers Dement (Amst). 2018;10:773–81.
Thomann AE, Berres M, Goettel N, Steiner LA, Monsch AU. Enhanced diagnostic accuracy for neurocognitive disorders: a revised cut-off approach for the Montreal Cognitive Assessment. Alzheimers Res Ther. 2020;12(1):39.
Guenther U, Wolke M, Hansen HC, Feldmann N, Diers A, Dewald O, et al. [Disorientation and delirium assessment: A secondary analysis of a prospective, observational study]. Med Klin Intensivmed Notfmed. 2021. German. https://doi.org/10.1007/s00063-021-00850-z. Epub ahead of print. PMID: 34432084.
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703–10.
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–44.
Dias N, Kempen GI, Todd CJ, Beyer N, Freiberger E, Piot-Ziegler C, Yardley L, Hauer K. The German version of the Falls Efficacy Scale-International Version (FES-I). Z Gerontol Geriatr. 2006;39(4):297–300.
Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K, Todd C. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008;37(1):45–50.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Julayanont P, Brousseau M, Chertkow H, Phillips N, Nasreddine ZS. Montreal Cognitive Assessment Memory Index Score (MoCA-MIS) as a predictor of conversion from mild cognitive impairment to Alzheimer’s disease. J Am Geriatr Soc. 2014;62(4):679–84.
Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19(2):203–14.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86.
Heuschmann PU, Kolominsky-Rabas PL, Nolte CH, Hunermund G, Ruf HU, Laumeier I, Meyrer R, Alberti T, Rahmann A, Kurth T, et al. The reliability of the german version of the barthel-index and the development of a postal and telephone version for the application on stroke patients. Fortschr Neurol Psychiatr. 2005;73(2):74–82.
Dapp U, Minder CE, Anders J, Golgert S, von Renteln-Kruse W. Long-term prediction of changes in health status, frailty, nursing care and mortality in community-dwelling senior citizens-results from the Longitudinal Urban Cohort Ageing Study (LUCAS). BMC Geriatr. 2014;14:141.
Huy C, Schneider S. Instrument for the assessment of middle-aged and older adults’ physical activity: design, eliability and application of the German-PAQ-50+. Z Gerontol Geriatr. 2008;41(3):208–16.
Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52(7):643–51.
Mumken SA, Gellert P, Stollwerck M, O’Sullivan JL, Kiselev J. Validation of the German Life-Space Assessment (LSA-D): cross-sectional validation study in urban and rural community-dwelling older adults. BMJ Open. 2021;11(7): e049926.
Stalvey BT, Owsley C, Sloane ME, Ball K. The Life Space Questionnaire: A Measure of the Extent of Mobility of Older Adults. J Appl Gerontol. 2016;18(4):460–78.
Heidenblut S, Zank S. Screening for Depression with the Depression in Old Age Scale (DIA-S) and the Geriatric Depression Scale (GDS15). GeroPsych. 2014;27(1):41–9.
Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell scale for depression in dementia. Biol Psychiat. 1988;23(3):271–84.
Ludwig K. Graf von der Schulenburg JM, Greiner W: German Value Set for the EQ-5D-5L. Pharmacoeconomics. 2018;36(6):663–74.
Konig HH, Brettschneider C, Luhmann D, Kaduszkiewicz H, Oey A, Wiese B, Werle J, Weyerer S, Fuchs A, Pentzek M, et al. EQ-5D-3L health status and health state utilities of the oldest-old (85 +) in Germany: results from the AgeCoDe-AgeQualiDe study. Qual Life Res. 2020;29(12):3223–32.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, Sayer AA. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40(4):423–9.
Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther. 2007;30(1):8–15.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–61.
Morris R, Stuart S, McBarron G, Fino PC, Mancini M, Curtze C. Validity of Mobility Lab (version 2) for gait assessment in young adults, older adults and Parkinson’s disease. Physiol Meas. 2019;40(9): 095003.
Sankarpandi SK, Baldwin AJ, Ray J, Mazza C. Reliability of inertial sensors in the assessment of patients with vestibular disorders: a feasibility study. BMC Ear Nose Throat Disord. 2017;17:1.
Rieger MM, Papegaaij S, Steenbrink F, Pijnappels M, van Dieen JH. Development of a Balance Recovery Performance Measure for Gait Perturbation Training Based on the Center of Pressure. Front Sports Act Living. 2021;3: 617430.
Roeles S, Rowe PJ, Bruijn SM, Childs CR, Tarfali GD, Steenbrink F, Pijnappels M. Gait stability in response to platform, belt, and sensory perturbations in young and older adults. Med Biol Eng Comput. 2018;56(12):2325–35.
Meyer C, Killeen T, Easthope CS, Curt A, Bolliger M, Linnebank M, Zorner B, Filli L. Familiarization with treadmill walking: How much is enough? Sci Rep. 2019;9(1):5232.
Albert JA, Owolabi V, Gebel A, Brahms CM, Granacher U, Arnrich B. Evaluation of the Pose Tracking Performance of the Azure Kinect and Kinect v2 for Gait Analysis in Comparison with a Gold Standard: A Pilot Study. Sensors (Basel). 2020;20(18):5104.
Kurz I, Gimmon Y, Shapiro A, Debi R, Snir Y, Melzer I. Unexpected perturbations training improves balance control and voluntary stepping times in older adults - a double blind randomized control trial. BMC Geriatr. 2016;16:58.
McCrum C, Karamanidis K, Grevendonk L, Zijlstra W, Meijer K. Older adults demonstrate interlimb transfer of reactive gait adaptations to repeated unpredictable gait perturbations. Geroscience. 2020;42(1):39–49.
Rieger MM, Papegaaij S, Pijnappels M, Steenbrink F, van Dieen JH. Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin Biomech (Bristol, Avon). 2020;75: 104988.
Kirchner M, Schubert P, Haas CT. Characterisation of Real-World Bus Acceleration and Deceleration Signals. J Signal Inf Process. 2014;05(01):8–13.
Poole DC, Jones AM. Oxygen Uptake Kinetics. Compr Physiol. 2012;2(2):933–96.
Beltrame T, Gois MO, Hoffmann U, Koschate J, Hughson RL, Moraes Frade MC, Linares SN, da Silva Torres R, Catai AM. Relationship between maximal aerobic power with aerobic fitness as a function of signal-to-noise ratio. J Appl Physiol (1985). 2020;129(3):522–32.
Hoffmann U, Drescher U, Benson AP, Rossiter HB, Essfeld D. Skeletal muscle VO(2) kinetics from cardio-pulmonary measurements: assessing distortions through O(2) transport by means of stochastic work-rate signals and circulatory modelling. Eur J Appl Physiol. 2013;113(7):1745–54.
Koschate J, Drescher U, Thieschafer L, Heine O, Baum K, Hoffmann U. Cardiorespiratory Kinetics Determined by Pseudo-Random Binary Sequences - Comparisons between Walking and Cycling. Int J Sports Med. 2016;37(14):1110–6.
Morse JM. Critical issues in qualitative research methods. Thousand Oaks: Sage Publications; 1994.
Kuckartz U: Qualitative Inhaltsanalyse. Methoden, Praxis, Computerunterst¸tzung. 2016.
French SD, Green SE, O’Connor DA, McKenzie JE, Francis JJ, Michie S, Buchbinder R, Schattner P, Spike N, Grimshaw JM. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38.
Barker A, Cameron P, Flicker L, Arendts G, Brand C, Etherton-Beer C, Forbes A, Haines T, Hill AM, Hunter P, et al. Evaluation of RESPOND, a patient-centred program to prevent falls in older people presenting to the emergency department with a fall: A randomised controlled trial. PLoS Med. 2019;16(5): e1002807.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95: 103208.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Abelson J, Li K, Wilson G, Shields K, Schneider C, Boesveld S. Supporting quality public and patient engagement in health system organizations: development and usability testing of the Public and Patient Engagement Evaluation Tool. Health Expect. 2016;19(4):817–27.
Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, Altman DG, Moher D, Barber R, Denegri S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ. 2017;358: j3453.
Step safely: strategies for preventing and managing falls across the life-course. In. Geneva: World Health Organization; 2021: Licence: CC BY-NC-SA 3.0 IGO.
Morello RT, Soh SE, Behm K, Egan A, Ayton D, Hill K, Flicker L, Etherton-Beer CD, Arendts G, Waldron N, et al. Multifactorial falls prevention programmes for older adults presenting to the emergency department with a fall: systematic review and meta-analysis. Inj Prev. 2019;25(6):557–64.
Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Prevention of Falls Network E, Outcomes Consensus G: Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–22.
Peeters GM, Jones M, Byles J, Dobson AJ. Long-term Consequences of Noninjurious and Injurious Falls on Well-being in Older Women. J Gerontol A Biol Sci Med Sci. 2015;70(12):1519–25.
Howard Wilsher S, Brainard J, Loke Y, Salter C. Patient and public involvement in health literacy interventions: a mapping review. Res Involv Engagem. 2017;3:31.
Baldwin JN, Napier S, Neville S, Wright-St Clair VA. Impacts of older people’s patient and public involvement in health and social care research: a systematic review. Age Ageing. 2018;47(6):801–9.
Alaraj R, Alshammari R. Utilizing Machine Learning to Recognize Human Activities for Elderly and Homecare. Acta Inform Med. 2020;28(3):196–201.
Mrozek D, Koczur A, Małysiak-Mrozek B. Fall detection in older adults with mobile IoT devices and machine learning in the cloud and on the edge. Inf Sci. 2020;537:132–47.
Robiner WN. Enhancing adherence in clinical research. Contemp Clin Trials. 2005;26(1):59–77.
Acknowledgements
We want to thank all doctors and nurses involved, particularly our study nurses Sabine Ehlers and Ann-Kathrin Wolter for their help with informing subjects about the study. Further, we want to express our gratitude to the participatory research team for their valuable input and feedback. We would also like to acknowledge all colleagues, who have assisted and supported us during the grant proposal: Lena Ansmann, Rebecca Diekmann, Falk Hoffmann, Mark Schweda, Merle Weßel.
Funding
Open Access funding enabled and organized by Projekt DEAL. The project has been funded by the Federal Ministry of Education and Research (BMBF, grant number: 01GY2021). The BMBF did not contribute to the study design or in writing the manuscript nor will it be involved in data collection, analysis and interpretation.
Author information
Authors and Affiliations
Contributions
TS is the coordinating researcher and is involved in writing the manuscript and data collection. JK was a major contributor in writing the manuscript and in the conception of the research project. NR and ED have revised the work and are involved in data collection. MH has revised the work, organized and installed the assessments in the gait laboratory. SL has revised the draft and contributed to the conception of the research project. ALB, SH and AH will supervise the qualitative and machine learning parts of the study and have provided input for writing the manuscript. RK is responsible for the statistical design and analysis of the study and provided feedback to an earlier version of the draft. TZ is the principal investigator, played a major role in the conception of the research project, supervises the research project and provided substantial feedback to the study protocol. All authors were involved in the design of this study protocol and have approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study will be performed in accordance with the Declaration of Helsinki. The Medical Ethics Committee of the University of Oldenburg gave their approval (number: 2021 – 120 and 2021 – 106). All participants in this study will provide written informed consent. Important modifications to the protocol will be implemented after approval by the Medical Ethics Committee and communicated to subjects as well as trial registries.
Consent for publcation
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary file 1.
‘Geriatrisches Screening bei Klinikaufnahme‘; unofficial English translation of the German version.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stuckenschneider, T., Koschate, J., Dunker, E. et al. Sentinel fall presenting to the emergency department (SeFallED) – protocol of a complex study including long-term observation of functional trajectories after a fall, exploration of specific fall risk factors, and patients’ views on falls prevention. BMC Geriatr 22, 594 (2022). https://doi.org/10.1186/s12877-022-03261-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03261-7