Abstract
Background
It has been suggested that tooth loss in later life might increase dementia incidence. The objective of this analysis is to systematically review the current evidence on the relationship between the number of remaining teeth and dementia occurrence in later life.
Methods
A search of multiple databases of scientific literature was conducted with relevant parameters for articles published up to March 25th, 2017. Multiple cohort studies that reported the incidence of dementia and residual teeth in later life were found with observation periods ranging from 2.4 to 32 years. Random-effects pooled odds ratios (OR) and 95% confidence intervals (CI) were estimated to examine whether high residual tooth number in later life was associated with a decreased risk of dementia. Heterogeneity was measured by I2. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system was used to assess the overall quality of evidence.
Results
The literature search initially yielded 419 articles and 11 studies (aged 52 to 75 at study enrollment, n = 28,894) were finally included for analysis. Compared to the low residual teeth number group, the high residual teeth number group was associated with a decreased risk of dementia by approximately 50% (pooled OR = 0.483; 95% CI 0.315 to 0.740; p < 0.001; I2 = 92.421%). The overall quality of evidence, however, was rated as very low.
Conclusion
Despite limited scientific strength, the current meta-analysis reported that a higher number of residual teeth was associated with having a lower risk of dementia occurrence in later life.
Similar content being viewed by others
Background
Dementia is a degenerative neuropsychological syndrome that affects not only a person’s ability to perform everyday activities, but also their cognitive skills including difficulties with memory, language, and problem-solving [1]. These difficulties occur because nerve cells in parts or most of the brain involved in cognitive function have been damaged or destroyed [2]. With the exception of cases of dementia caused by genetic abnormalities, dementia is thought to develop, like other common chronic diseases, as a result of multiple factors rather than a single cause [3]. Dementia is common as it affects 46.8 million older adults worldwide with an annual incidence of 9.9 million [4]. As life expectancy rises across the planet, most sharply in developing countries, the prevalence of dementia is expected to increase as well [4, 5]. Dementia has an enormous social and economic impact on patients, families, and government programs [6]. Thus, there is growing interest in identifying the risk factors for dementia, especially modifiable ones, which may play a pivotal role in preventing or at least delaying the progression of dementia.
Recently, a number of systematic reviews and meta-analyses examining longitudinal studies from Western and Asian countries have focused on the link between the number of teeth and cognitive status [7,8,9]. Despite the importance of examining the relationship between tooth loss and dementia in later life, only one meta-analysis, which was limited, was recently released [9]. Shen et al. [9] included cross sectional studies that might not accurately estimate dementia incidence and did not include important longitudinal studies in the analysis without readily apparent reasons [10, 11]. In the meta-analysis by Shen et al. [9], neither the process for the literature search nor for assessing the quality of evidence using standardized tools were presented. Therefore, there is an urgent need for a well-designed meta-analysis to examine the relationship between tooth loss and dementia incidence in later life.
Methods
Search strategy
A literature search was performed using the keywords “teeth”, “tooth”, “dental”, “tooth loss”, “teeth loss”, “missing teeth”, “oral health”, “dental care”, “elderly”, “later life”, “older adults”, “cognition”, “cognitive impairment”, “cognitive decline”, “dementia”, or in various combinations to identify every original study published in English from PubMed, EMBASE, Medline/Ovid, Cumulative Index to Nursing and Allied Health Literature, Web of Science, and Google Scholar databases up to March 25th, 2017. See Additional file 1 for more detailed information of systematic search strategy. Residual teeth number was defined as the count of natural teeth only and the division between a “high” and a “low” number of teeth in included studies ranged from 11 to 24 teeth (see Table 2). Studies that examined the association between residual teeth number and incidence of dementia in middle-age or older adults were included. Studies depicting high and low residual teeth groups at the time of study completion were given preference. Selected papers were restricted to cohort studies to prevent significant selection bias from cross-sectional studies in determining the incidence of dementia [12].
Study selection and data extraction
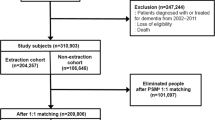
Two authors (X.L and C.C.) independently screened titles and abstracts. Full articles that met the criteria were pooled after an independent review, they extracted the data. Discrepancies were resolved in consultation with two other authors (B.O. and D.H.) every phase. Alternative search approach was performed by manually reviewing the references of eligible articles. Through alternative search, relevant twenty-three studies were added. The high or low teeth number groups were collected from tables and manuscript text in each study. When actual data was not presented in certain studies, two authors (K.H. and J.Y.) contacted the corresponding authors of the studies by either email or phone call in order to access data. Since the data originated from previously published studies, an institutional review board approval was waived. Finally, eleven studies were selected. Figure 1 presents the study selection process in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [13]. A summary of each study is shown in Table 1 and Table 2 presents patient specification for each study.
Quality assessment
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) [14] system to assess the overall quality of evidence for each outcome. Five domains (risk of bias, consistency, directness, precision, and publication bias) were considered to assess the overall quality of evidence. The GRADE system rates the quality of evidence as high, moderate, low, and very low [15]. Meta-analysis from observational studies start from a low quality of evidence. The quality of evidence may decrease when there are serious limitations of any of the five domains; therefore, optimal information size (OIS) calculations as an objective measure of imprecision for grading evidence were used. A priori assessment of risk showed an increase by 50% from low residual teeth number group with an alpha = 0.05 and beta = 0.80 compared to the dementia incidence risk from high residual teeth number group [10, 11, 15]. Publication bias was assessed by Egger’s regression analysis, which provides a more objective way to estimate the reliability of results, [16] and by funnel plot for visual inspection of publication bias. Table 3 presented the quality of evidence using the GRADEpro software [17].
Data synthesis and analysis
Individual study results were combined to calculate the pooled odds ratio (OR) and 95% confidence intervals (CI) using the random effects method [18]. Between-study heterogeneity was assessed using the I2 static values of 50%, representing an extensive statistical inconsistency. Subgroup analysis was performed to examine the effects of observation period, definition of high residual teeth number group, and study site. Meta-regression analysis was performed to predict whether age, gender, alcohol, smoking, diabetes, hypertension, depression, education attainment, denture use, regular dental care would be associated with the incidence of dementia. Studies were excluded one at a time and meta-analysis findings were individually analyzed against sensitivity analysis, which specifically analyzes to assess the robustness of the review results. For sensitivity analysis on publication bias, the “trim-and-fill” methods proposed by Duval and Tweedie [19] were used to further re-examine publication bias and to estimate corrected pooled ORs. Second order terms as sensitivity analysis of meta-regression results were used. All analyses were performed in Statistical Package for the Social Sciences version 24 (IBM Analytics Inc., Armonk, New York, USA, 2015) and Comprehensive Meta-Analysis version 3 (Biostat Inc., Englewood, New Jersey, USA, 2014). A 2-sided p-value < 0.05 was considered statistically significant.
Results
Study selection and participants characteristics
A total of 28,642 patients from 11 cohort studies were described in detail in Table 1 [10, 11, 20,21,22,23,24,25,26,27,28]. Observation periods ranged from 2.4 (Kim et al. [11]) to 32 years (Stewart et al. [24]). Age of enrollment ranged between ages of 52 and 75. High and low residual teeth group participants were 14,366 and 14,528, respectively. Between 9.6% (Yamamoto et al. [27]) and 32.8% (Paganini-Hill et al. [26]) of participants in each study were excluded from study enrollment or lost to follow-up during observation period. Table 2 presents each study’s cognitive assessment tool as well as dementia incidence rates per 100,000 persons by high/low residual teeth tooth groups. Stewart et al. [24] and Paganini-Hill et al. [26] demonstrated the highest rates of dementia incidence as well as the longest observation periods, 32 years and 18 years, respectively.
Meta-analyses
Figure 2 presents the meta-analysis results, which are the incidence of dementia between high and low residual teeth number groups. High residual teeth number group was associated with a decrease in the dementia occurrence risk (pooled OR = 0.483; 95% CI 0.315–0.740; p < .001). Heterogeneity was extensive (Q = 64.722, p < .001, I2 = 92.421%). Pooled incidence rates of dementia in low and high residual teeth group participants were 8415 and 7729 per 100,000 persons, respectively as presented in Table 3.
Quality assessment
The final quality of evidence was lowered to “very low” because serious limitations were found regarding inconsistency and publication bias of the GRADE [15] system as shown in Table 3. The quality of evidence started low because the analyzed studies were all observational [10, 11, 20,21,22,23,24,25,26,27,28]. There was evidence of publication bias found by the Egger’s regression test [16] (p = .009) and by the funnel plot as shown in Fig. 3. The total number of study participants (28,894) exceeded OIS (1471).
Subgroup and meta-regression analyses
In the subgroup analysis by length of observation period (≥ 5 years, < 5 years), high residual tooth number group was persistently associated with a decrease in dementia occurrence (OR = 0.545; 95% CI 0.343–0.864; p = .010) in ≥5 years [10, 20,21,22,23,24, 26, 28] and (OR = 0.358; 95% CI 0.185–0.693; p = .002) in < 5 years [11, 25, 27]. When the high residual tooth number group was defined as ≥20 [10, 22, 23, 27, 28], it was associated with a decrease in dementia occurrence (OR = 0.445; 95% CI 0.378–0.523; p < .001). However, this association was diminished (p = .264) in other definitions of high residual teeth group [11, 20, 21, 24,25,26]. In terms of study location, high residual teeth number group was associated with a decrease in dementia occurrence risk in Asian countries [11, 22, 23, 25, 27, 28] (OR = 0.381; 95% CI 0.271–0.536; p < .001), but this finding was not observed in Western countries [10, 20, 21, 24, 26] (OR = 0.646; 95% CI 0.364–1.146; p = .135).
Table 4 depicts meta-regression analysis results. Old age [10, 11, 20, 21, 23,24,25,26,27,28] (OR = 1.068; 95% CI 1.007–1.142; p < .001), diabetes [10, 22, 24, 25] (OR = 3.542; 95% CI 1.135–4.885; p = .037), and hypertension [22, 23, 25, 28] (OR = 3.146; 95% CI 1.071–4.610; p = .041) were predictors of dementia incidence. On the other hand, high-level education attainment [20, 22,23,24] (OR = 0.425; 95% CI 0.217–0.912; p = .015) and regular dental care [22, 23, 26, 27] (OR = 0.581; 95% CI 0.298–0.946; p = .027) were inversely associated with dementia incidence. Since the studies conducted by Stewart et al. [24] and Stein et al. [21] enrolled only female participants, these studies were excluded from meta-regression on age. The rest of the results from gender [10, 11, 20, 22, 23, 25,26,27,28], alcohol [10, 22, 23, 26], smoking [10, 22,23,24,25, 27], depression [23, 25, 27] and denture use [20, 22, 26,27,28] were not associated with dementia incidence.
Sensitivity analyses
The resulting estimate of the corrected OR was 0.469 (95% CI 0.307–0.718; p < .001) by the “trim-and-fill” method. While the corrected OR was increased, it did not change the essential thrust of pooled ORs on the effect of higher residual teeth number being associated with a lower incidence of dementia. The meta-analysis found that high residual teeth number group was robust in influencing the analysis. The results with pooled estimates of OR of dementia incidence with high residual tooth number group ranged from 0.315 to 0.740. With removal of individual studies and the lower limit of 95% CI, the results ranged from 0.277 to 0.364. The upper limits of 95% CI ranged from 0.603 to 0.792 with the removal of individual studies. The meta-regression results were confirmed even with sensitivity analyses using a second-order term.
Discussion
Tooth loss and dementia incidence in later life
To the best of our knowledge, the current study is the first well-designed meta-analysis that compares dementia occurrence risk among residual teeth number groups in later life. The current meta-analysis found that dementia occurrence risk in the high residual teeth number group was lowered by approximately half compared to the low residual teeth number group. However, wide variations in observation period, dementia definition, and high residual teeth group definition between studies may have led to greater heterogeneity among main findings. Despite significant dementia incidence rates between high/low residual teeth number groups as presented by pooled OR (0.483), the absolute difference of dementia incidence rates between these two groups was relatively narrow (+ 686 per 100,000 persons in low residual teeth number group). This effect can be explained by Paganini-Hill et al. [26], which had the largest number of study participants and yet had results, though with marginal significance, that ran counter to those of the meta-analysis (high residual tooth number group increased dementia incidence).
There are multiple possible mechanisms by which tooth loss can adversely affect cognitive function in later life. It has been suggested that masticatory stimulation with normal occlusion increases cerebral blood flow, activation of the cortical area, and increases levels of oxygen in blood [22, 29]. Reciprocally, poor mastication decreases orofacial sensorimotor activity, which eventually results in an overall cognitive decline [30].
Meta-regression and factors associated with dementia in later life
The association between tooth loss and dementia occurrence may be confounded by biological and healthcare system factors. Advanced age is the strongest predictor of incidence for any type of dementia as replicated by the current analysis. This finding has been identified from an early meta-analysis, which also noted that elderly women had a higher rate of dementia incidence [31]. However, recent studies on the progression from mild cognitive impairment to Alzheimer disease present conflicting results [32, 33]. A gender difference was not identified in dementia incidence in our analysis.
A recent meta-analysis by Xu et al. [34] found a dose-response relationship between alcohol use and dementia incidence. Modest alcohol consumption was associated with a decreased risk of dementia incidence while high alcohol consumption was associated with an increased risk of dementia incidence. Data collection of alcohol intake for the analyzed studies was not quantified except for Batty et al. [10]; therefore, the lack of association between alcohol intake and dementia occurrence found in this meta-analysis could be explained by the mixed effects of modest and high-amount of alcohol consumption. Previous studies have supported that smoking is associated with dementia incidence [35, 36]. The magnitude of the relationship between smoking and dementia incidence was effaced to the point of marginal non-significance in this analysis, but potential selection bias from heterogeneous data may have occurred.
Diabetes and hypertension are cardiovascular risk factors and, when these are uncontrolled over a long-period, they may lead to atherosclerosis, which in turn may reduce cerebral blood flow. This has been the main explanation for the wide spectrum of cognitive impairment, from mild cognitive impairment to vascular and Alzheimer’s dementia [10, 37, 38].
Chewing with a removable denture is at least 30% to 40% less efficient than chewing with natural teeth [39]. Denture use might not restore the entire masticatory function in elderly patients with tooth loss as much as implants do. Therefore, denture use may not maintain cerebral blood flow in patients with tooth loss [40].
Regular dental care was associated with a decreased risk of dementia occurrence in meta-regression from 4 analyzed studies [22, 23, 26, 27]. More than half of adults in the US faced at least partial tooth loss and had not received regular dental care [41]. Except for Paganini-Hill et al. [26], which found no association between regular dental care and dementia incidence, three studies were conducted in Japan. These studies found that regular dental care reduced dementia incidence. The different lifestyle and health care systems between Paganini-Hill et al. [26] and the other three Japanese studies [22, 23, 27] may explain the different effects of regular dental care on dementia incidence [42]. For example, older Japanese adults might have more access to dental care through the Japanese Ministry of Health and Welfare initiated nationwide dental policy, the “80–20” campaign in effect since 1989 [43], as well as through a universal long-term care insurance implementation that has been happening since 2001 [44], which promotes regular dental care in later life. In a subgroup analysis, Asian studies found a greater association between tooth loss and dementia incidence while in Western studies, this association was diminished. This finding could be interpreted as possible interactions between healthcare systems (universal vs. non-universal delivery systems) and dental care access. Therefore, future comparative studies are urgently needed, to see whether a link between regular dental care and dementia incidence can be replicated in countries where different health care systems, universal vs. non-universal, have been adopted.
Education itself could create an additional reserve against clinical manifestations of dementia or educational attainment may be the result of having a greater reserve to begin with [45]. This hypothesis has been proven by a serial of cohort [46] and meta-analyses [47]. Temporal trends in developed countries, higher levels of education attainment, and better control of cardiovascular risk factors are considered likely contributors to the declining dementia risk [48, 49]. Although educational attainment is a powerful determinant of health among older adults, participation in lifelong learning, especially with a community-based approach, has a great potential to attenuate the relationship between tooth loss and dementia incidence [50]. Community-based lifelong learning programs could enhance social networks, active engagement, and encourage regular participation in intellectually stimulating activities, which may delay the progression of cognitive decline even in older adults whose cognition has already started to decline [51].
Strengths and limitations
A strength of the current study is that the analysis was based on cohort studies which are better able to feasibly explain dementia occurrence when compared to cross-sectional studies. Another strength is the application of a structured approach to literature search and quality assessment.
There are several limitations in this study. The oral cavity, particularly in chronic periodontal disease, can affect tooth loss [20, 21, 52] and cognitive impairment [53,54,55] by multiple plausible explanations [7, 53]. Chronic inflammation as measured by blood inflammatory markers are, in turn, thought to play a central role in altering the inflammatory state within the brain via various microbial or cytokines activities [54, 56,57,58,59]. The mediator role of chronic periodontal disease has not been measured in the original studies, therefore, the mediator effect of chronic periodontal disease between tooth loss and dementia could not be presented in the current analysis. Heterogeneity from differing observation times, cognitive assessments, and definitions of high and low residual teeth number groups could raise concerns of overgeneralization when these findings are applied to real practice. There is potential reverse causality due to long prodromal phase of dementia. Time-person analysis might adjust an issue resulting from potential reverse causality. In addition, a time-person analysis could not be applied due to the lack of data from studies except for the most recently published study, Takeuchi et al. [22]. This analysis relied on counting residual teeth at the completion of each study. A mid-point analysis that may have provided more information of time-variable analysis could not be performed.
Conclusions
These findings support a link between tooth loss and dementia occurrence in later life. Further studies are needed to evaluate the effects of chronic periodontitis on cognitive function in multi-point longitudinal studies. In addition, further developments in restorative dental prostheses by oral health scientists as well as optimizing lifelong community education programs for local older adults by community leaders and health policymakers may defer or reduce negative outcomes associated with tooth loss and cognitive decline.
Abbreviations
- CI:
-
Confidence Intervals
- GRADE:
-
Grading of recommendations assessment, development, and evaluation
- OIS:
-
Optimal information size
- OR:
-
Odds ratio
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 2nd ed. Arlington, VA: American Psychiatric Association; 2013.
Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC, et al. National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease. Alzheimers Dement. 2012;8(1):1–13.
Kapasi A, DeCarli C, Schneider JA. Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol. 2017;134(2):171–86.
World Alzheimer Report. Improving healthcare for people living with dementia: Coverage, quality and costs now and in the future. 2016. Available at https://www.alz.co.uk/research/world-report-2016. Accessed 26 May 2017.
Wu YT, Beiser AS, Breteler MMB, Fratglioni L, Helmer C, Hendrie HC, et al. The changing prevalence and incidence of dementia over time - current evidence. Nat Rev Neurol. 2017;13(6):327–39.
Hurd MD, Martolle P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326–34.
Tonsekar PP, Jiang SS, Yue G. Periodontal disease, tooth loss and dementia: is there a link? A systematic review. Gerodontology. 2017;34(2):151–63.
Wu B, Fillenbaum GG, Plassman BL, Guo L. Association between oral health and cognitive status: a systematic review. J Am Geriatr Soc. 2016;64(4):739–51.
Shen T, Lv J, Wang L, Wang W, Zhang D. Association between tooth loss and dementia among older people: a meta-analysis. Int J Geriatr Psychiatry. 2015;31(8):953–5.
Batty G, Li Q, Huxley R, Zoungas S, Taylor BA, Neal B, et al. Oral disease in relation to future risk of dementia and cognitive decline: prospective cohort study based on the action in diabetes and vascular disease: Preterax and Diamicron modified-release controlled evaluation (ADVANCE) trial. Eur Psychiat. 2013;28(1):49–52.
Kim JM, Stewart R, Prince M, Kim SW, Yang SJ, Shin IS, et al. Dental health, nutritional status and recent-onset dementia in a Korean community population. Int J Geriatr Psychiatry. 2007;22(9):850–5.
Hernán MA, Alonso A, Logroscino G. Cigarette smoking and dementia: potential selection bias in the elderly. Epidemiology. 2008;19(3):448–50.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011;64(12):1283–93.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE working group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Cochrane Collaboration: GradePRO. Available at: https://gradepro.org. Accessed 4 Apr 2017.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Arrivé E, Letenneur L, Matharan F, Laporte C, Helmer C, Barberger-Gateau P, et al. Oral health condition of French elderly and risk of dementia: a longitudinal cohort study: a longitudinal cohort study. Community Dent Oral Epidemiol. 2011;40(3):230–8.
Stein P, Desrosiers M, Donegan SJ, Yepes JF, Kryscio RJ. Tooth loss, dementia and neuropathology in the nun study. J Am Dent Assoc. 2007;138(10):1314–22.
Takeuchi K, Ohara T, Furuta M, Takeshita T, Shibata Y, Hata J, et al. Tooth loss and risk of dementia in the community: the Hisayama study. J Am Geriatr Soc. 2017;65(5):e95-e100.
Komiyama T, Ohi T, Miyoshi Y, Murakami T, Tsuboi A, Tomata Y, et al. Association between tooth loss, receipt of dental care, and functional disability in an elderly Japanese population: the Tsurugaya project. J Am Geriatr Soc. 2016;64(12):2495–502.
Stewart R, Stenman U, Hakeberg M, Hagglin C, Gustafson D, Skoog I, Associations. Between oral health and risk of dementia in a 37-year follow-up study: the prospective population study of women in Gothenburg. J Am Geriatr Soc. 2015;63(1):100–5.
Luo J, Wu B, Zhao Q, Guo Q, Meng H, Yu L, et al. Association between tooth loss and cognitive function among 3063 Chinese older adults: a community-based study. PLoS One. 2015;10(3):e0120986.
Paganini-Hill A, White S, Atchison K. Dentition, dental health habits, and dementia: the leisure world cohort study. J Am Geriatr Soc. 2012;60(8):1556–63.
Yamamoto T, Kondo K, Hirai H, Nakade M, Aida J, Hirata Y. Association between self-reported dental health status and onset of dementia: a 4-year prospective cohort study of older Japanese adults from the Aichi Gerontological evaluation study (AGES) project. Psychosom Med. 2012;74(3):241–8.
Shimazaki Y, Soh I, Saito T, Yamashita Y, Koga T, Miyazaki H, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res. 2001;80(1):340–5.
Hirano Y, Obata T, Kashikura K, Nonaka H, Tachibana A, Ikehira H, et al. Effects of chewing in working memory processing. Neurosci Lett. 2008;436(2):189–92.
De Cicco V, Barresi M, Tramonti Fantozzi MP, Cataldo E, Parisi V, Manzoni D. Oral implant-prostheses: new teeth for a brighter brain. PLoS One. 2016;11(2):e0148715.
Gao S, Hendrie HC, Hall KS, Hui S. The relationship between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis. Arch Gen Psychiatry. 1999;55(9):809–15.
Lin KA, Choudhury KR, Rathakrishnan BG, Marks DM, Petrella JR, Doraiswamy PM, et al. Marked gender differences in progression of mild cognitive impairment over 8 years. Alzheimers Dement (N Y). 2015;1(2):103–10.
Kim S, Kim MJ, Kang HS, Lim SW, Myung W, Lee Y, et al. Gender differences in risk factors for transition from mild cognitive impairment to Alzheimer’s disease: a CREDOS study. Compr Psychiatry. 2015;62:114–22.
Xu W, Wang H, Wan Y, Tan C, Li J, Tan L, et al. Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2017;32(1):31–42.
Reitz C, den Heijer T, van Duijn C, Hofman A, Breteler M. Relation between smoking and risk of dementia and Alzheimer disease: the Rotterdam study. Neurology. 2007;69(10):998–1005.
Ohara T, Ninomiya T, Hata J, Ozawa M, Yoshida D, Mukai N, et al. Midlife and late-life smoking and risk of dementia in the community: the Hisayama study. J Am Geriatr Soc. 2015;63(11):2332–9.
Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012;42(5):484–91.
Nagai M, Hoshide S, Kario K. Hypertension and dementia. Am J Hypertens. 2010;23(2):116–24.
Idowu AT, Handelman SL, Graser GN. Effect of denture stability, retention, and tooth form on masticatory function in the elderly. Gerodontics. 1987;3(4):161–4.
von der Gracht I, Derks A, Haselhuhn K, Wolfart S. EMG correlations of edentulous patients with implant overdentures and fixed dental prostheses compared to conventional complete dentures and dentates: a systematic review and meta-analysis. Clin Oral Implants Res. 2017;28(7):765–73.
Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102(3):411–8.
Lee JL, Liu X, Yoo JW. Education and healthcare system effects on tooth loss and dementia incidence in later life. J Am Geriatr Soc 2017 June 12 [Epub ahead print].
Ministry of Health, Labour and Welfare Japan. Overview 8020 Campaign. Available at: http://www.mhlw.go.jp/english/wp/wp-hw3/dl/2-075.pdf. Accessed 14 May 2017.
Houde SC, Gautam R, Kai I. Long-term Care insurance in Japan: implications for U.S. long-term care policy. J Gerontol Nurs 2007;33(1):7–13.
Ngandu T, von Strauss E, Helkala EL, Winblad B, Nissinen A, Tuomilehto J, et al. Education and dementia: what lies behind the association? Neurology. 2007;69(14):1442–50.
Bachkati K, Mortensen E, Brønnum-Hansen H, Holm-Pedersen P. Midlife cognitive ability, education, and tooth loss in older Danes. J Am Geriatr Soc. 2017;65(1):194–9.
Meng X, D’Arcy C. Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS One. 2012;7(6):e38268.
Langa KM, Larson EB, Crimmins EM, Faul JD, Levine DA, Kabeto MU, et al. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177(1):51–8.
Matthews FE, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, et al. Medical Research Council cognitive function and ageing collaboration. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the cognitive function and ageing study I and II. Lancet. 2013;382(9902):1405–12.
Narushima M. More than nickels and dimes: the health benefits of a community-based lifelong learning programme for older adults. Int J Lifelong Edu. 2008;27(6):673–92.
Ramscar M, Hendrix P, Shaoul C, Milin P, Baayen H. The myth of cognitive decline: non-linear dynamics of lifelong learning. Top Cogn Sci. 2014;6(1):5–42.
Kaye EK, Valencia A, Baba N, Spiro A, Dietrich T, Garcia RI. Tooth loss and periodontal disease predict poor cognitive function in older men. J Am Geriatr Soc. 2010;58(4):713–8.
Lee YT, Lee HC, Hu CJ, Huang LK, Chao SP, Lin CP, et al. Periodontitis as a modifiable risk factor for dementia: a nationwide population-based cohort study. J Am Geriatr Soc. 2017;65(2):301–5.
Weijenberg RA, Scherder EJ, Lobbezoo F. Mastication for the mind-the relationship between mastication and cogitation in ageing and dementia. Neurosci Biobehav Rev. 2011;35(3):483–97.
Shin SH, Shin MS, Ahn YB, Choi BY, Nam JH, Kim HD. Periodontitis is associated with cognitive impairment in elderly Koreans: results from the Yangpyeong cohort study. J Am Geriatr Soc. 2016;64(1):162–7.
Kamer AR, Craig RG, Dasanayake AP, Brys M, Glodzik-Sobanska L, de Leon MJ. Inflammation and Alzheimer’s disease: possible role of periodontal disease. Alzheimers Dement. 2008;4(4):242–50.
Sochocka M, Sobczynski M, Sender-Janeczek AM, Zwolinska K, Blachowicz O, Tomcyk T, et al. Association between periodontal health status and cognitive abilities: the role of cytokine profile and systemic inflammation. Curr Alzeimer Res. 2017;14(7):731–41.
Gill-Montoya JA, Barrios R, Santana S, Sanchez-Lara I, Pardo CC, Fornieles-Rubio F, et al. Association between periodontitis and amyloid β-peptide in elderly people with and without cognitive impairment. J Periodontol. 2017;88(10):1051–8.
Noble JM, Scarmeas N, Celenti RS, Elkind MS, Wright CB, Schupf N, et al. Serum IgG antibody levels to periodontal microbiota are associated with incident Alzheimer disease. PLoS One. 2014;9(12):e114959.
Acknowledgements
Not applicable.
Funding
University of Nevada School of Medicine Faculty Career Development funded this research. (Number: 16–016).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to different ownership of data results from original studies, but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
BO designed and conducted the study, interpreted the results, and helped write the manuscript. DHH and JWY conceived and designed the study, helped obtain funding, analyzed the data, and wrote sections of the manuscript. K-TH provided methodological support, screened citations and full-text articles, and edited the manuscript. XL, JU, CC and KD screened citations and full-text articles, abstracted data, appraised quality, and helped conceive the study and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Supplement (DOCX 12 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Oh, B., Han, DH., Han, KT. et al. Association between residual teeth number in later life and incidence of dementia: A systematic review and meta-analysis. BMC Geriatr 18, 48 (2018). https://doi.org/10.1186/s12877-018-0729-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-018-0729-z