Abstract
Objective
This scoping review describes the relationship between tooth retention, health, and quality of life in older adults.
Methods
Seven databases were searched for English language articles for subjects ≥ 65 y from 1981 to 2021. Exposure was tooth retention (≥ 20), and outcomes were general/systemic health and quality of life. Methodological quality was assessed using the Newcastle–Ottawa Scale and Cochrane Risk of Bias 2.0 tool.
Results
140 articles were included, only four were randomized trials. Inter-rater agreement (κ) regarding study inclusion was 0.924. Most were assessed with low risk of bias (n = 103) and of good quality (n = 96). Most studies were conducted in Japan (n = 60) and Europe (n = 51) and only nine in the US. Tooth retention was referred to as “functional dentition” in 132 studies and “shortened dental arch” in 19 studies. Study outcomes were broadly synthesized as (1) cognitive decline/functional dependence, (2) health status/chronic diseases, (3) nutrition, and (4) quality of life.
Discussion
There is a positive relationship between tooth retention, overall health, and quality of life. Older adults retaining ≥ 20 teeth are less likely to experience poorer health. Having < 20 teeth increases the likelihood for functional dependence and onset of disability, and may affect successful ageing. This review supports the general finding that the more teeth older adults retain as they age, the less likely they are to have adverse health outcomes. However, significant knowledge gaps remain which can limit decision-making affecting successful ageing for many older adults. This review highlights the need to consider, as an important marker of oral health and function, the retention of a functional minimum of a natural dentition, rather than a simple numeric score of missing teeth.
Similar content being viewed by others

Introduction
The aging of the global population is a hallmark of the twenty-first century with average lifespans projected to reach 100 years in some countries [1]. The world’s population is ageing rapidly with a projected doubling of the population by 2050, with those aged 80 and older expected to triple by 2050. In the US, by 2034 older adults will surpass children in population size for the first time and by 2060, they will comprise one-quarter of the population [2, 3]. Many of these older adults have retained much of their natural dentition and this trend is expected to continue. As recently as 1970, complete tooth loss (edentulism), affected half of the US older adult population. Today, the edentulism rate is 17% and is projected to decrease to < 3% by 2050 [4,5,6]. Globally, edentulism has decreased by about half among all persons, regardless of age, from 1990 to 2010 [7].
Tooth retention is considered an important indicator of a population’s oral health and is monitored by several countries. For example, the ‘8020’ campaign targeting elderly adults in Japan, which promotes the retention of ≥ 20 teeth by the time they reach the age of 80 years [8,9,10]. Research has shown an inverse correlation between masticatory function measured as number of remaining teeth and certain chronic systemic diseases [11,12,13,14,15,16,17,18,19]. Additional studies suggest cognitive and physical functioning may be poorer in edentulous older adults ≥ 65 years compared to their dentate counterparts [11, 20, 21]. There are also significant positive correlations between oral health status and overall/general health-related quality of life (HRQoL) [22,23,24], as well as the number of remaining teeth [25].
Quality of life (QoL) measures often include an objective and a subjective evaluation of life circumstances [26]. Fallowfield proposed psychological (e.g., depression), social (e.g., engagement in social and leisure activities), occupational (e.g., the ability to carry out paid or domestic work), and physical (e.g., pain, sleep, and mobility) core domains of QoL [27]. The definition of HRQoL varies, but the consensus identifies physical symptoms, perceptions of well-being and functional capacity as major dimensions [28]. Oral health contributes to QoL, and these dimensions are applied in dental research as number of dental symptoms, perception of oral well-being, and social and physical oral functioning [29,30,31,32].
Studying how tooth retention is related with health and QoL in aging populations is important because of the expected demographic shifts and tooth retention trends. Having a better understanding of the role tooth retention plays in health and wellbeing will help to inform how we can improve care for the increasing diversity and numbers of older adults whose oral health status and needs will be changing as well. Thus, our objective is to evaluate the literature using systematic methodology to ascertain the breadth of published information on tooth retention, health and QoL in older adults (≥ 65) using two common concepts, a functional dentition (FD) and a shortened dental arch (SDA), considered to be the minimal threshold of tooth retention needed to have a positive effect on well-being. This will help to identify gaps in knowledge and opportunities for research on the topics of tooth retention and health in older adults.
Methods
This study is a scoping review with the purpose of identifying knowledge and conceptual gaps and describing a body of literature on the topic. A protocol was written a priori for the review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [33]. We also used the PRISMA-ScR [33] to write this review.
Our primary research question was: What is the relationship between tooth retention defined as ≥ 20 teeth (characterized as either FD or SDA) on health and HRQoL in adults age ≥ 65? To guide this review, we established a set of a priori operational definitions:
Functional dentition: having ≥ 20 teeth regardless of position, location, or teeth type or ≥ 21 natural teeth [5, 34].
Shortened dental arch: is the presence of ≥ 20 teeth based on position and location on the dental arch dependent on author specific definitions focusing on the number of functional occlusal contacts in posterior teeth [35,36,37].
HRQoL: “An individual’s or group’s perceived physical and mental health over time” [38].
Successful aging: Having low probability of disease and disability, high cognitive and physical functioning, as well as productive activity and activity involving relations with others [39].
Well-being: Having positive outcomes that are meaningful including judgments of life satisfaction and feelings ranging from depression to joy. It’s what people think and feel about their lives, including quality of their relationships, their positive emotions and resilience, realization of their potential, and overall satisfaction with life [40].
Eligibility criteria
To assist with identifying studies eligible for inclusion in this scoping review, we used the following PECO framework:
Participants: Adults ≥ 65, with no geographic or other demographic restrictions.
Exposure: Tooth retention, presence of ≥ 20/≥ 21 teeth, characterized as a FD/SDA.
Comparators: Included studies must compare outcomes in a group with FD/SDA and a group without FD/SDA.
Outcomes: Included studies were required to report on outcomes in one or more of four major categories: (1) Cognitive decline/functional dependence, (2) Health status/chronic diseases, (3) Nutrition, and/or (4) Quality of Life.
We limited the search to English language articles published from 1981 to 2021. In 1981, Kayser proposed the SDA concept [41], studies on FD followed later. Initial title/abstract (tiab) search included studies with participants ≥ 18, where exposure was tooth retention described as FD/SDA, and outcomes were general/systemic health and quality of life. Studies for full-text review were then limited to studies where participants age or age-groups were clearly defined as ≥ 65.
We included original observational research (cross-sectional, cohort, and case control studies) and interventional research (randomized and non-randomized controlled trials). Studies exclusively dealing with edentulous subjects with prostheses, in vitro studies, case series, case reports, non-peer reviewed studies, letters to the editor, editorials, commentaries, narrative syntheses, abstracts, personal communication as well as studies with both adults and children when data is not reported separately for adults ≥ 65 were excluded.
Information sources and search
A research librarian (AAL) independently performed searches in December 2019 and September 2021 of 7 databases: Ageline (EBSCOhost), Cochrane Library Database of Systematic Reviews (Wiley and Sons), Cumulative Index of Nursing and Allied Health Literature (EBSCOhost), Embase (Elsevier), PubMed/MEDLINE (US National Library of Medicine), Scopus (Elsevier), and Web of Science: Core Collection (Clarivate Analytics). A combination of controlled vocabulary terms (CINAHL Subject Headings, EMTREE, Medical Subject Headings), key words, and phrases for each of the concepts of interest were adapted for each database (see Additional file 2). Search results were exported into EndNote X9 (Clarivate Analytics) for citation management and removal of duplicates, and into Covidence (Veritas Health Innovation) for tiab and full-text screening.
Study selection, data collection, and risk of bias
Inter-rater reliability assessments were conducted between two main reviewers (AAA and SDL) and concordance was excellent before tiab and full-text screening (Kappa of 0.92 and 1.00 during tiab and full-text screening respectively). The main reviewers completed the initial tiab screen in February 2020 and the follow-up tiab in September 2021 when the review was updated, with another reviewer (SB) resolving disagreements from tiab screen using Covidence. Full-text articles were reviewed through September 2021 with two reviewers (SB, DW) serving as arbitrators.
Using Microsoft Excel, AAA and SDL independently extracted data into tables including author/year, objective, country, age, sample size, study design etc. Risk of bias and methodological quality was assessed using the Newcastle–Ottawa Scale (NOS) [42] for observational studies and the Cochrane Collaboration’s revised Risk of Bias 2.0 (RoB 2.0) for randomized trials [43] (Additional file 1: Table S3).
Results
Selection of sources
We retrieved 5044 citations after the database searches of which 1708 duplicates were removed resulting in 3336 unique citations for screening. After tiab screening, 575 studies were identified that met inclusion criteria. Following full-text screening, 435 were excluded (different age or age-groups, natural present teeth not grouped, different outcomes, inappropriate or incorrect study designs etc.) and 140 studies were included. See Fig. 1 for PRISMA flow diagram and full list of exclusion reasons.
Article characteristics
General characteristics of the 140 included studies are provided in Additional file 1: Tables S1 and S2. All were observational studies except for four randomized controlled clinical trials (RCT). Two observational studies were from a retrospective cohort, 23 from a prospective cohort, and 111 were cross-sectional studies. The majority were conducted in Japan (n = 60) and Europe (n = 51). Most European studies originated from the UK (n = 11) with Brazil (n = 12) and South Korea (n = 9) representing most of the non-European studies. Nine studies were conducted in the US.
There were 130 studies defining tooth retention in terms of a FD: 78 studies defined it as retention of ≥ 20 teeth, 18 defined it as retention of ≥ 21 teeth, and 36 assessed a FD in other ways (example, in terms of missing teeth or some other category of teeth present) (Additional file 1: Table S1). Researchers in 14 studies defined tooth retention in terms of a SDA (Additional file 1: Table S2). Nine studies defined tooth retention in terms of both FD and SDA. Specific information by tooth retention concept for all studies are in Additional file 1: Tables S1 and S2. Most outcomes evaluated were cognitive decline/functional dependence (n = 52), QoL (n = 45) and health status/chronic diseases (n = 43) (Table 1). The frequency of the more recent studies published substantially favored the use of FD (Fig. 2).
Risk of bias
Using the NOS and RoB 2.0 tools to assess risk of bias and methodological quality, 103 studies had a low risk of bias and the methodological quality of evidence in 96 studies was good (Additional file 1: Table S3). Only nine of the 140 articles included in this review had a sample size less than 100, indicating the majority were likely of adequate size (Additional file 1: Tables S1 and S2).
Synthesis of findings
Cognitive decline and functional dependence outcomes
The occurrence of severe cognitive impairment or lower mental status was associated with the presence of < 10 natural teeth in at least one dental arch (< 20 teeth total) [44, 45]. Having < 20 teeth is associated with lower hand-grip strength, leg extensor strength, isokinetic leg extensor power, and one-leg standing time, though the relationship tends to disappear after adjusting for confounders such as height, body weight, gender, smoking and alcohol, marital status, regular medical treatment, and regular exercise [46]. Activities of daily living/instrumental activities of daily living (ADL/IADL) problems were associated with < 20 teeth and loss of a FD was associated with severe locomotion impairments and difficulties with ADL/IADL [47,48,49,50,51,52,53,54,55,56,57]. In addition, having < 20 teeth was associated with functional dependence and was associated with onset of disability, declines in higher-level functional and mortality [47, 49, 53, 54, 58, 59]. Wearing dental prostheses mediated these effects (e.g., subjects having 19 or fewer teeth but not wearing dentures had a significantly increased risk for incident falls compared with those having FD, though wearing dentures alleviated this risk) [60].
Persons with FD were more active in leisure sports suggesting that the number of remaining teeth was associated with functional capacity, physical ability, and physical activity in elderly persons [50, 61,62,63]. A Higher Mini-Mental State Examination ‘MMSE’ scores (cognitive decline) were associated with FD compared to < 20 teeth after adjustment for demographics in a relationship also moderated/mediated by prostheses type [55, 56, 64,65,66,67,68,69]. Results on FD and psychological distress and depression are mixed. Self-rated poor oral health increased for individuals who had symptoms of psychological distress and < 20 teeth [70].
Health status/chronic diseases outcomes
Older adults with < 20 teeth present had 2.5 times greater risk of cardiovascular disease, a relationship mediated by weight and BMI, suggesting that the number of missing teeth affects the quality of diet [71]. One study reported a relationship between tooth loss and chronic kidney disease, especially among older women [72]. Older adults with < 20 teeth had significantly increased risk of metabolic syndrome, higher serum lipid peroxide, and glycemic status [73,74,75]. However, the relationship was reversed in a study population of Medicaid patients for glycemic status [73].
Favorable lifestyles such as “no smoking” and “no alcohol drinking” show a strong association with > 20 teeth with the inverse being true for those with < 20 teeth or lacking a FD [76,77,78]. Similar relationships were reported where smoking and drinking status were used as confounders, though these results were mixed when the health outcome was hypertension [79,80,81]. Older Brazilian adults with ≥ 20 teeth had a lower chance of being frail than edentulous individuals, and elderly individuals with a need for dental prostheses were significantly more likely to be prefrail and frail [82]. Similar results were reported in Chinese, Japanese, and Danish cohorts though in a British cohort, this association was not significant [83,84,85,86,87]. In those ≥ 85 y, those with FD had a longer life expectancy and demonstrated successful ageing when compared with the edentulous participants [88]. Individuals with FD had more skeletal muscle mass than those with ≤ 20 teeth [89].
Nutrition outcomes
Older adults with a compromised FD (≤ 20 teeth) had higher odds of inadequate calorie intake, lower Healthy Eating Index (HEI) scores, and BMI outside of the normal range (obesity or being underweight) [52, 90,91,92,93,94,95]. In randomized, controlled clinical trials, conventional and functionally oriented tooth replacement strategies both showed significant improvement in mini-nutritional assessment scores though hematological markers did not provide a clear picture of improvement in either group [96, 97]. In general, people with FD were significantly more likely to be able to chew all foods, have a normal BMI, and consume more nutrients [98,99,100].
Quality of life outcomes
Sáez-Prado and colleagues showed a relationship between summary HRQoL variables in EuroQol- 5 Dimension (EQ-5D), visual analogue scale (VAS) and Oral Health Impact Profile (OHIP-14) scores [101]. Using the EQ-5D, those with ≤ 20 teeth were significantly less likely to have a good score in any of its five dimensions [102]. Dissatisfaction with daily life and an unfavorable face-scale score (negative mood) are more prevalent in those with < 20 teeth. However there was no consistent difference in prevalence of poor QoL status when comparing four groups defined by remaining numbers of teeth by regression analysis [103] though Wu et al. report that higher number of occluding tooth pairs were associated with better oral health-related quality of life (OHRQoL) (p < 0.001) [104]. Having ≤ 20 teeth mediates the association between living alone, measures of social relations, and coronal caries [105,106,107].
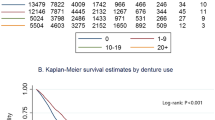
In general, social participation measures (travel, participation in leisure sports, cultural activity, neighborhood associations, or hobby clubs), were related to having ≥ 20 teeth [61, 106]. Using the Short Form Health Survey (SF-36), those with ≥ 20 teeth had higher physical component scores than did those with ≤ 19 teeth [26]. A SDA resulted in better or smaller OHIP-14 scores i.e. better OHRQoL compared to a removable partial denture group in one RCT [108].
Discussion
This scoping review describes the current state of knowledge regarding tooth retention, general/systemic health, and quality of life in older adults. Oral disease is a universal problem, but because it is rarely life-threatening, its prevention or treatment is often a low priority for health policy makers [31]. For instance, almost half of the world’s population is affected by an oral condition, accounting for 0.6% of all disability adjusted life-years (DALYs) [109]. DALYs increased 20.8% from 1990 to 2010 but mainly due to population growth and aging [109]. Continuing trends of improving tooth retention and increasing chronic disease co-morbidities, common in people as they age past 65 years, point towards future unmet dental and other healthcare needs when placed in the context of health professional shortages especially in the field of geriatric dentistry.
Of the 140 articles included in this review, most were cross-sectional, published in the last decade, described tooth retention in terms of FD, and examined cognitive decline, functional dependence, and general health/chronic disease outcomes in Japanese or European populations.
Given the broad nature of our research question, this scoping review is helpful for identifying areas where more work is needed. For example, within the cognitive decline and functional dependence domain, most research examined ADL/IADL. However, there appears to be a lack of research ascertaining dementia and other cognitive screening tools and their relationship with tooth retention. Such tools are increasingly being recommended for use in primary care [110]. Two Japanese studies in this review investigated differences between 8020 and non-8020 elderly [8, 9]. In general, 8020 achievers had good ADL/IADL levels and better satisfaction with life. Tooth loss is associated with onset of disability and mortality in old age and may be an early indicator of accelerated aging [49]. Maintenance of a FD is preventive against late-life cognitive declines in the aged population and associated with functional independence in nursing home residents [53, 55, 56]. Antunes and colleagues noted the complex interplay of factors resulting in a bidirectional relationship between dentition status and onset of functional disability [57]. For example, tooth brushing was reported to at least partially negate the increased risk of incident functional disability associated with having fewer remaining teeth [58], whereas Yamamoto and colleagues reported that in subjects with 19 or fewer teeth, the risk of falls was not significantly elevated as long as they wore dentures [60].
The relationship between tooth loss, numbers of remaining teeth, cognitive function, impairment or dementia, the direction of causality of the relationship between cognitive impairment and having poor oral health is poorly elucidated. Peres and colleagues reported a bidirectional association with effects particularly pronounced in older adults [44]. In Japan, where a sizable number of studies were conducted, dementia is a major cause of disruption of a healthy life expectancy. Kato et al. and Yoo et al. reported an association between number of teeth and cognitive function in community dwelling individuals [111]. Others report the use of artificial teeth, dentures, posterior teeth occlusion, socioeconomic status, educational level, smoking status, and systemic diseases, also influence this relationship [44, 69]. At least one study compared associations between dentate groups having FD, ≤ 19 teeth with dentures, and ≤ 19 teeth without dentures [69]. Participants with few teeth and without dentures had a nearly two-fold increased risk for dementia onset compared with those with 20 teeth or more [69].
Laurence Frank in 1946 presented two conflicting views of aging: one, an involutionary, largely pathological process; while the other describes a process of biological transformation [112]. The concept of successful ageing today is interconnected with QoL, a multidimensional construct that relates to the satisfaction of individual needs for growth, well-being, self-esteem, freedom and the pleasures of meaningful relationships and work [38, 40, 113, 114]. Based on the WHO model of health, Locker’s conceptualization of the impact of oral disease posits five consequences of oral disease: impairment, functional limitation, pain/discomfort, disability, and handicap [32, 115]. Implicit to Locker’s model is the assumption there is a relationship between poor oral health and impaired QoL. The medical model emphasizes the biological and pathological progression of oral health diseases and its irreversible endpoint, tooth loss; on the other hand, it uses measurable clinical indicators such as decayed, missing and filled teeth (DMFT), or numbers of remaining teeth as we do in this review.
Globally, 7 of the top 10 causes of mortality are ascribed to non-communicable diseases (NCDs) led by heart disease, stroke, and chronic obstructive pulmonary disease (COPD) [116]. In the US, non-communicable diseases (NCDs) account for 89% of all deaths and have surpassed infectious diseases as the main cause of death [117]. The top 5 NCDs are ischemic heart disease, Alzheimer’s, lung cancer, stroke, and COPD [117]. Yet, the paucity of longitudinal studies incorporating measures of tooth retention significantly limits our understanding of the relationship between tooth retention and chronic diseases. Within the nutrition domain, we note that studies generally focused on chewing ability and numbers of different types of foods/nutrients consumed rather using diet quality indices that are more appropriate for epidemiological studies. Within the QoL domain, few studies examined the relationship of tooth retention with social participation measures, which may be a significant oversight given the important esthetic and social considerations associated with tooth retention.
Only 20 articles described nutritional outcomes, suggesting the need for more, appropriately designed studies, conducted in the US and elsewhere to address this research gap. Within the nutritional outcome’s literature for instance, we also note that few used objective, diet quality measures of nutrition status like HEI, FDSK-11 or Diet Variety Score. Given that the US is becoming more diverse and aging rapidly, the lack of high-quality studies to inform evidence-based decision-making to improve oral health and related outcomes for older adults is a concern. Having > 20 teeth into old age played an important role in having a healthy diet rich in fruits and vegetables, a satisfactory nutritional status, and an acceptable BMI [98, 118, 119]. In the oldest old (80+ years), the presence of natural teeth, plus well-fitting dentures were associated with higher and more varied nutrient intakes and greater dietary quality [119]. The status of dentition should be a major consideration in nutritional counseling and assessment of older adults because tooth loss can affect ability to chew resulting in a lack of adequate nutrition intake [93].
Although we focused on FD/SDA and not edentulism, some of these articles reported a separate set of findings on edentulism and tooth loss or examined how having a denture or oral health behaviors like toothbrushing altered the relationship between tooth retention and the main outcomes considered in this review. For instance, severe cognitive impairment or a reduced mental status was associated with being edentulous [44, 45]. Edentulous subjects also had significantly increased risk of metabolic syndrome, higher serum lipid peroxide, and glycemic status [73,74,75], and Yamamoto and colleagues reported an association between edentulism and incident depressive symptoms [120]. While it may not be surprising that complete edentulism is associated with greater odds of self-rated “fair/poor” health in older diabetics, who also experienced additional physically unhealthy days in the past 30 days, it is also notable that the loss of any permanent teeth was also associated with these findings [121]. In addition, determinants of oral health behaviors were independently associated with edentulism [122], with tooth loss associated with self-limited food choices for example [12, 98, 99].
We encountered limitations common to reviews of the literature, for example difficulty in accessing literature not published in English, reporting on publication bias, and dependency on the rigor of methodological reporting in the included studies. In terms of strengths, most reviewed studies had a sample size > 100, had low risk of bias (n = 96) and were of good methodological quality (n = 103), as assessed using the NOS and RoB tools. This current review supersedes existing work in the following ways: (1) a focus solely on general/systemic health outcomes in older adults ≥ 65 rather than dental outcomes, (2) it uses common concepts that provide a threshold of tooth loss with minimal impact on well-being (FD/SDA), and (3) uses a longer timeframe for electronic database search. Although this review focused on numbers of remaining teeth, several studies described tooth retention in terms of tooth loss highlighting the need for a standardization of language that more appropriately describes the natural tooth retention trends we now see. This aligns with global efforts promoting retention of teeth as a healthcare policy goal.
Conclusion
The high global prevalence of oral disorders [123] and the new effort underway by the WHO to develop a global oral health strategy (resolution WHA74.5) to improve oral health and wellbeing that is aligned with NCD prevention strategies and universal health coverage [124] clearly points to the need for substantially more research to inform decision-making. As we move towards more integrated care models, cooperation among all health care providers will facilitate improved oral health among older adults, especially for those with multiple chronic conditions [50, 71]. With a “greying” global population, understanding how tooth retention patterns can affect successful aging among older adults, including where they live and work, is an important consideration for guiding evidence-based practice, including improving standards of care for those who are dependent on others for daily living, with the overall goal of promoting oral health and facilitating quality of life. Despite some uncertainty determining the direction of the cause and effect between tooth loss and overall health, insights from new research appear promising to facilitate clinical decision-making and caregiving, improve the framing of communication and health education strategies, and provide a guide for health policy makers who want to address the future oral health needs of older adults.
Abbreviations
- QoL:
-
Quality of life
- HRQoL:
-
Health-related quality of life
- FD:
-
Functional dentition
- SDA:
-
Shortened dental arch
- PRISMA-ScR:
-
Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews
- PECO:
-
Participants, exposure, comparators, outcomes
- NOS:
-
Newcastle–Ottawa Scale
- RoB2:
-
Cochrane collaboration’s revised risk of bias tool 2.0
- OHRQoL:
-
Oral health-related quality of life
References
Landefeld CS, Winker MA, Chernof B. Clinical care in the aging century—announcing “Care of the aging patient: from evidence to action.” JAMA. 2009;302(24):2703–4.
Aging NIo. World’s older population grows dramatically 2016. Available from: https://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically.
Mather M, Jacobsen LA, Pollard KM. Aging in the united states: population reference Bureau; 2015.
Slade GD, Akinkugbe AA, Sanders AE. Projections of U.S. Edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93(10):959–65.
Dye BA, Weatherspoon DJ, Lopez MG. Tooth loss among older adults according to poverty status in the United States from 1999 through 2004 and 2009 through 2014. J Am Dent Assoc. 2019;150(1):9-23.e3.
Lin M, Griffin SO, Gooch BF, Espinoza L, Wei L, Li C-H, et al. Oral health surveillance report: trends in dental caries and sealants, tooth retention, and edentulism, United States: 1999–2004 to 2011–2016. 2019.
Kassebaum N, Bernabé E, Dahiya M, Bhandari B, Murray C, Marcenes W. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res. 2014;93(7_suppl):20S-28S.
Hashimoto M, Yamanaka K, Shimosato T, Furuzawa H, Tanaka H, Kato H, et al. Oral condition and health status of people aged 80–85 years. Geriatr Gerontol Int. 2006;6(1):60–4.
Hashimoto M, Yamanaka K, Shimosato T, Ozawa A, Takigawa T, Hidaka S, et al. Oral condition and health status of elderly 8020 achievers in Aichi Prefecture. Bull Tokyo Dent Coll. 2006;47(2):37–43.
Yamanaka K, Nakagaki H, Morita I, Suzaki H, Hashimoto M, Sakai T. Comparison of the health condition between the 8020 achievers and the 8020 non-achievers. Int Dent J. 2008;58(3):146–50.
Everman A. Genome-wide association study and meta-analysis of missing teeth and functional dentition: University of Pittsburgh; 2018.
Watson S, McGowan L, McCrum L-A, Cardwell CR, McGuinness B, Moore C, et al. The impact of dental status on perceived ability to eat certain foods and nutrient intakes in older adults: cross-sectional analysis of the UK National Diet and Nutrition Survey 2008–2014. Int J Behav Nutr Phys Act. 2019;16(1):43.
Bethene Ervin R, Dye BA. Number of natural and prosthetic teeth impact nutrient intakes of older adults in the United States. Gerodontology. 2012;29(2):e693–702.
Savoca MR, Arcury TA, Leng X, Chen H, Bell RA, Anderson AM, et al. Severe tooth loss in older adults as a key indicator of compromised dietary quality. Public Health Nutr. 2010;13(4):466–74.
Griffin SO, Barker LK, Griffin PM, Cleveland JL, Kohn W. Oral health needs among adults in the United States with chronic diseases. J Am Dent Assoc. 2009;140(10):1266–74.
Hung H-C, Joshipura KJ, Colditz G, Manson JE, Rimm EB, Speizer FE, et al. The association between tooth loss and coronary heart disease in men and women. J Public Health Dent. 2004;64(4):209–15.
Joshipura KJ, Douglass CW, Willett WC. Possible explanations for the tooth loss and cardiovascular disease relationship. Ann Periodontol. 1998;3(1):175–83.
Polzer I, Schwahn C, Völzke H, Mundt T, Biffar R. The association of tooth loss with all-cause and circulatory mortality. Is there a benefit of replaced teeth? A systematic review and meta-analysis. Clin Oral Investig. 2012;16(2):333–51.
Maupomé G, Gullion CM, White BA, Wyatt CCL, Williams PM. Oral disorders and chronic systemic diseases in very old adults living in institutions. Spec Care Dentist. 2003;23(6):199–208.
Tsakos G, Watt RG, Rouxel PL, de Oliveira C, Demakakos P. Tooth loss associated with physical and cognitive decline in older adults. J Am Geriatr Soc. 2015;63(1):91–9.
Fang W-L, Jiang M-J, Gu B-B, Wei Y-M, Fan S-N, Liao W, et al. Tooth loss as a risk factor for dementia: systematic review and meta-analysis of 21 observational studies. BMC Psychiatry. 2018;18(1):345.
Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NHJ. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8(1):126.
Schierz O, Baba K, Fueki K. Functional oral health-related quality of life impact: a systematic review in populations with tooth loss. J Oral Rehabil n/a(n/a)
Naito M, Yuasa H, Nomura Y, Nakayama T, Hamajima N, Hanada N. Oral health status and health-related quality of life: a systematic review. J Oral Sci. 2006;48(1):1–7.
Tan H, Peres KG, Peres MA. Retention of teeth and oral health-related quality of life. J Dent Res. 2016;95(12):1350–7.
Akifusa S, Soh I, Ansai T, Hamasaki T, Takata Y, Yohida A, et al. Relationship of number of remaining teeth to health-related quality of life in community-dwelling elderly. Gerodontology. 2005;22(2):91–7.
Fallowfield L. The quality of life: the missing measurement in health care. London: Souvenir Press; 1990.
Levine S. What constitutes quality of life? A conceptualization of dimensions of life quality in healthy populations and patients with cardiovascular disease. Assessment of quality of life in clinical trials of cardiovascular therapies. 1984:46–58.
Allen PF. Assessment of oral health related quality of life. Health Qual Life Outcomes. 2003;1(1):40.
Ansai T, Hamasaki T. Relationship between oral health and exercise function of elderly persons 80 years old in Fukuoka Prefecture. 2000.
Chen M-S, Hunter P. Oral health and quality of life in New Zealand: a social perspective. Soc Sci Med. 1996;43(8):1213–22.
Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5:3–18.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Chalub LLFH, Ferreira RC, Vargas AMD. Influence of functional dentition on satisfaction with oral health and impacts on daily performance among Brazilian adults: a population-based cross-sectional study. BMC Oral Health. 2017;17(1):112.
Käyser A. Shortened dental arches and oral function. J Oral Rehabil. 1981;8(5):457–62.
Wiener RC, Wiener MA, McNeil DW. Comorbid depression/anxiety and teeth removed: behavioral risk factor surveillance system 2010. Commun Dent Oral Epidemiol. 2015;43(5):433–43.
Witter DJ, van Palenstein Helderman WH, Creugers NH, Käyser AF. The shortened dental arch concept and its implications for oral health care. Commun Dent Oral Epidemiol. 1999;27(4):249–58.
Health-related Quality of Life Centers for Disease Control and Prevention website [updated October 31, 2018. Available from: https://www.cdc.gov/hrqol/index.htm.
Martin P, Kelly N, Kahana B, Kahana E, Willcox BJ, Willcox DC, et al. Defining successful aging: a tangible or elusive concept? Gerontologist. 2014;55(1):14–25.
Well-Being Concepts [updated October 31, 2018]. Available from: Centers for Disease Control and Prevention website
Fernandes V, Chitre V. The shortened dental arch concept: a treatment modality for the partially dentate patient. J Indian Prosthodontic Soc. 2008;8(3):134–9.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle–Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http//www.ohri.ca/programs/clinical_epidemiology/oxford.asp. 2012. Accessed; 2021.
Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (Clin Res Ed). 2019; 366.
Peres MA, Bastos JL, Watt RG, Xavier AJ, Barbato PR, D’Orsi E. Tooth loss is associated with severe cognitive impairment among older people: findings from a population-based study in Brazil. Aging Ment Health. 2015;19(10):876–84.
Wang T-F, Chen Y-Y, Liou Y-M, Chou C. Investigating tooth loss and associated factors among older Taiwanese adults. Arch Gerontol Geriatr. 2014;58(3):446–53.
Takata Y, Ansai T, Awano S, Hamasaki T, Yoshitake Y, Kimura Y, et al. Relationship of physical fitness to chewing in an 80-year-old population. Oral Dis. 2004;10(1):44–9.
Saintrain MVDL, Saintrain SV, Sampaio EGM, Ferreira BSP, Nepomuceno TC, Frota MA, et al. Older adults’ dependence in activities of daily living: Implications for oral health. Public Health Nurs. 2018;35(6):473–81.
Takata Y, Ansai T, Awano S, Sonoki K, Fukuhara M, Wakisaka M, et al. Activities of daily living and chewing ability in an 80-year-old population. Oral Dis. 2004;10(6):365–8.
Holm-Pedersen P, Schultz-Larsen K, Christiansen N, Avlund K. Tooth loss and subsequent disability and mortality in old age. J Am Geriatr Soc. 2008;56(3):429–35.
Mollaoglu N, Alpar R. The effect of dental profile on daily functions of the elderly. Clin Oral Invest. 2005;9(3):137–40.
Montero J, Bravo M, Hernandez L, Dib A. Effect of arch length on the functional well-being of dentate adults. J Oral Rehabil. 2009;36(5):338–45.
Inomata C, Ikebe K, Kagawa R, Okubo H, Sasaki S, Okada T, et al. Significance of occlusal force for dietary fibre and vitamin intakes in independently living 70-year-old Japanese: from SONIC Study. J Dent. 2014;42(5):556–64.
Komiyama T, Ohi T, Miyoshi Y, Murakami T, Tsuboi A, Tomata Y, et al. Relationship between status of dentition and incident functional disability in an elderly Japanese population: prospective cohort study of the Tsurugaya project. J Prosthodont Res. 2018;62(4):443–8.
Aida J, Kondo K, Hirai H, Nakade M, Yamamoto T, Hanibuchi T, et al. Association between dental status and incident disability in an older Japanese population. J Am Geriatr Soc. 2012;60(2):338–43.
Takeuchi K, Izumi M, Furuta M, Takeshita T, Shibata Y, Kageyama S, et al. Association between posterior teeth occlusion and functional dependence among older adults in nursing homes in Japan. Geriatr Gerontol Int. 2017;17(4):622–7.
Takeuchi K, Izumi M, Furuta M, Takeshita T, Shibata Y, Kageyama S, et al. Posterior teeth occlusion associated with cognitive function in nursing home older residents: a cross-sectional observational study. PLOS ONE. 2015;10(10):e0141737.
Antunes JLF, de Andrade FB, Peres MA. How functional disability relates to dentition in community-dwelling older adults in Brazil. Oral Dis. 2017;23(1):97–101.
Bando S, Tomata Y, Aida J, Sugiyama K, Sugawara Y, Tsuji I. Impact of oral self-care on incident functional disability in elderly Japanese: the Ohsaki Cohort 2006 study. BMJ Open. 2017;7(9):e017946.
Sato Y, Aida J, Kondo K, Tsuboya T, Watt RG, Yamamoto T, et al. Tooth loss and decline in functional capacity: a prospective cohort study from the Japan Gerontological Evaluation Study. J Am Geriatr Soc. 2016;64(11):2336–42.
Yamamoto T, Kondo K, Misawa J, Hirai H, Nakade M, Aida J, et al. Dental status and incident falls among older Japanese: a prospective cohort study. BMJ Open. 2012;2(4):e001262.
Tada A, Watanabe T, Yokoe H, Hanada N, Tanzawa H. Relationship between the number of remaining teeth and physical activity in community-dwelling elderly. Arch Gerontol Geriatr. 2003;37(2):109–17.
Shimazaki Y, Soh I, Saito T, Yamashita Y, Koga T, Miyazaki H, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res. 2001;80(1):340–5.
Komiyama T, Ohi T, Miyoshi Y, Murakami T, Tsuboi A, Tomata Y, et al. Association between tooth loss, receipt of dental care, and functional disability in an elderly Japanese population: the Tsurugaya project. J Am Geriatr Soc. 2016;64(12):2495–502.
Kato H, Takahashi Y, Iseki C, Igari R, Sato H, Sato H, et al. Tooth loss-associated cognitive impairment in the elderly: a community-based study in Japan. Internal Med. 2019;58:1411–6.
Patcharawan Srisilapanan D, Jai-Ua C. Oral health status of dementia patients in Chiang Mai Neurological Hospital. J Med Assoc Thai. 2013;96(3):351–7.
Okamoto N, Morikawa M, Okamoto K, Habu N, Iwamoto J, Tomioka K, et al. Relationship of tooth loss to mild memory impairment and cognitive impairment: findings from the Fujiwara-kyo study. Behav Brain Funct. 2010;6(1):77.
Cocco F, Campus G, Strohmenger L, Ardizzone VC, Cagetti MG. The burden of tooth loss in Italian elderly population living in nursing homes. BMC Geriatr. 2018;18(1):76.
Nilsson H, Berglund J, Renvert S. Tooth loss and cognitive functions among older adults. Acta Odontol Scand. 2014;72(8):639–44.
Yamamoto T, Kondo K, Hirai H, Nakade M, Aida J, Hirata Y. Association between self-reported dental health status and onset of dementia: a 4-year prospective cohort study of older Japanese adults from the Aichi Gerontological Evaluation Study (AGES) Project. Psychosom Med. 2012;74(3):241–8.
Dahl KE, Calogiuri G, Jönsson B. Perceived oral health and its association with symptoms of psychological distress, oral status and socio-demographic characteristics among elderly in Norway. BMC Oral Health. 2018;18(1):93.
De Angelis F, Basili S, Giovanni F, Dan Trifan P, Di Carlo S, Manzon L. Influence of the oral status on cardiovascular diseases in an older Italian population. Int J Immunopathol Pharmacol. 2018;31:0394632017751786.
Shin H-S. Number of existing permanent teeth is associated with chronic kidney disease in the elderly Korean population. Korean J Intern Med. 2018;33(6):1150.
Northridge ME, Chakraborty B, Salehabadi SM, Metcalf SS, Kunzel C, Greenblatt AP, et al. Does medicaid coverage modify the relationship between glycemic status and teeth present in older adults? J Health Care Poor Underserved. 2018;29(4):1509.
Sonoki K, Takata Y, Ansai T, Fujisawa K, Fukuhara M, Wakisaka M, et al. Number of teeth and serum lipid peroxide in 85-year-olds. Community Dent Health. 2008;25(4):243.
Saito M, Shimazaki Y, Nonoyama T, Tadokoro Y. Number of teeth, oral self-care, eating speed, and metabolic syndrome in an aged Japanese population. J Epidemiol. 2019;29(1):26–32.
Laguzzi PN, Schuch HS, Medina LD, de Amores AR, Demarco FF, Lorenzo S. Tooth loss and associated factors in elders: results from a national survey in U ruguay. J Public Health Dent. 2016;76(2):143–51.
Ando A, Ohsawa M, Yaegashi Y, Sakata K, Tanno K, Onoda T, et al. Factors related to tooth loss among community-dwelling middle-aged and elderly Japanese men. J Epidemiol. 2013;23(4):301–6.
Yoshioka M, Hinode D, Yokoyama M, Fujiwara A, Sakaida Y, Toyoshima K. Relationship between subjective oral health status and lifestyle in elderly people: a cross-sectional study in Japan. ISRN dentistry. 2013; 2013.
Darnaud C, Thomas F, Pannier B, Danchin N, Bouchard P. Oral health and blood pressure: the IPC cohort. Am J Hypertens. 2015;28(10):1257–61.
Lee H-K, Lee K-D, Merchant AT, Lee S-K, Song K-B, Lee SG, et al. More missing teeth are associated with poorer general health in the rural Korean elderly. Arch Gerontol Geriatr. 2010;50(1):30–3.
Tramini P, Montal S, Valcarcel J. Tooth loss and associated factors in long-term institutionalised elderly patients. Gerodontology. 2007;24(4):196–203.
de Andrade FB, Lebrão ML, Santos JLF, de Oliveira Duarte YA. Relationship between oral health and frailty in community-dwelling elderly individuals in Brazil. J Am Geriatr Soc. 2013;61(5):809–14.
Gu Y, Wu W, Bai J, Chen X, Chen X, Yu L, et al. Association between the number of teeth and frailty among Chinese older adults: a nationwide cross-sectional study. BMJ Open. 2019;9(10):e029929.
Iwasaki M, Yoshihara A, Sato M, Minagawa K, Shimada M, Nishimuta M, et al. Dentition status and frailty in community-dwelling older adults: a 5-year prospective cohort study. Geriatr Gerontol Int. 2018;18(2):256–62.
Watanabe Y, Hirano H, Arai H, Morishita S, Ohara Y, Edahiro A, et al. Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc. 2017;65(1):66–76.
Ramsay SE, Papachristou E, Watt RG, Tsakos G, Lennon LT, Papacosta AO, et al. Influence of poor oral health on physical frailty: a population-based cohort study of older British men. J Am Geriatr Soc. 2018;66(3):473–9.
Avlund K, Schultz-Larsen K, Christiansen N, Holm-Pedersen P. Number of teeth and fatigue in older adults. J Am Geriatr Soc. 2011;59(8):1459–64.
Matsuyama Y, Aida J, Watt R, Tsuboya T, Koyama S, Sato Y, et al. Dental status and compression of life expectancy with disability. J Dent Res. 2017;96(9):1006–13.
Kim S, Min J-Y, Lee HS, Kwon K-R, Yoo J, Won CW. The association between the number of natural remaining teeth and appendicular skeletal muscle mass in Korean older adults. Ann Geriatr Med Res. 2018;22(4):194–9.
Iwasaki M, Taylor GW, Manz MC, Yoshihara A, Sato M, Muramatsu K, et al. Oral health status: relationship to nutrient and food intake among 80-year-old Japanese adults. Commun Dent Oral Epidemiol. 2014;42(5):441–50.
Nakamura M, Ojima T, Nakade M, Ohtsuka R, Yamamoto T, Suzuki K, et al. Poor oral health and diet in relation to weight loss, stable underweight, and obesity in community-dwelling older adults: a cross-sectional study from the JAGES 2010 project. J Epidemiol. 2016;26(6):322–9.
Östberg A-L, Bengtsson C, Lissner L, Hakeberg M. Oral health and obesity indicators. BMC Oral Health. 2012;12(1):50.
Sahyoun NR, Lin C-L, Krall E. Nutritional status of the older adult is associated with dentition status. J Am Diet Assoc. 2003;103(1):61–6.
Seman K, Abdul Manaf H, Ismail A. Association between functional dentition with inadequate calorie intake and underweight in elderly people living in" Pondok" in Kelantan. Arch Orofac Sci. 2007;2:10–9.
Shinkai R, Hatch J, Sakai S, Mobley C, Saunders M, Rugh JD. Oral function and diet quality in a community-based sample. J Dent Res. 2001;80(7):1625–30.
McKenna G, Allen PF, Flynn A, O’Mahony D, DaMata C, Cronin M, et al. Impact of tooth replacement strategies on the nutritional status of partially-dentate elders. Gerodontology. 2012;29(2):e883–90.
McKenna G, Allen PF, O’Mahony D, Cronin M, DaMata C, Woods N. Impact of tooth replacement on the nutritional status of partially dentate elders. Clin Oral Invest. 2015;19(8):1991–8.
Marcenes W, Steele JG, Sheiham A, Walls AWG. The relationship between dental status, food selection, nutrient intake, nutritional status, and body mass index in older people. Cad Saude Publica. 2003;19:809–15.
Sheiham A, Steele J. Does the condition of the mouth and teeth affect the ability to eat certain foods, nutrient and dietary intake and nutritional status amongst older people? Public Health Nutr. 2001;4(3):797–803.
Sheiham A, Steele J, Marcenes W, Lowe C, Finch S, Bates C, et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 2001;80(2):408–13.
Sáez-Prado B, Haya-Fernández M-C, Sanz-García M-T. Oral health and quality of life in the municipal senior citizen s social clubs for people over 65 of Valencia, Spain. Med Oral Patol Oral Cir Bucal. 2016;21(6):e672.
Cho MJ, Kim EK. Subjective chewing ability and health-related quality of life among the elderly. Gerodontology. 2019;36(2):99–106.
Takata Y, Ansai T, Awano S, Fukuhara M, Sonoki K, Wakisaka M, et al. Chewing ability and quality of life in an 80-year-old population. J Oral Rehabil. 2006;33(5):330–4.
Wu L, Cheung K, Lam P, Gao X. Oral health indicators for risk of malnutrition in elders. J Nutr Health Aging. 2018;22(2):254–61.
Avlund K, Holm-Pedersen P, Morse DE, Viitanen M, Winblad B. Social relations as determinants of oral health among persons over the age of 80 years. Commun Dent Oral Epidemiol. 2003;31(6):454–62.
Takeuchi K, Aida J, Kondo K, Osaka K. Social participation and dental health status among older Japanese adults: a population-based cross-sectional study. PLOS ONE. 2013;8(4):e61741.
Koyama S, Aida J, Saito M, Kondo N, Sato Y, Matsuyama Y, et al. Community social capital and tooth loss in Japanese older people: a longitudinal cohort study. BMJ Open. 2016;6(4):e010768.
McKenna G, Allen PF, O’Mahony D, Cronin M, DaMata C, Woods N. The impact of rehabilitation using removable partial dentures and functionally orientated treatment on oral health-related quality of life: a randomised controlled clinical trial. J Dent. 2015;43(1):66–71.
Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 2013;92(7):592–7.
Barnes DE, Beiser AS, Lee A, Langa KM, Koyama A, Preis SR, et al. Development and validation of a brief dementia screening indicator for primary care. Alzheimer’s Dementia. 2014;10(6):656-665.e1.
Yoo J-J, Yoon J-H, Kang M-J, Kim M, Oh N. The effect of missing teeth on dementia in older people: a nationwide population-based cohort study in South Korea. BMC Oral Health. 2019;19(1):61.
Frank LK. Gerontology. J Gerontol. 1946;1(11):1–12.
The Quality of American Life in the Eighties: Report of the Panel on the Quality of American Life. Washington DC (USA): President's Commission for a National Agenda for the Eighties; 1981.
McLeod S. Maslow’s hierarchy of needs. Simply Psychol. 2007;1:1–8.
Slade GD. Measuring oral health and quality of life. Chapel Hill. 1997;3.
World Health Organization. The top 10 causes of death 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
Chen S, Kuhn M, Prettner K, Bloom DE. The macroeconomic burden of noncommunicable diseases in the United States: estimates and projections. PLOS ONE. 2018;13(11):e0206702.
Natapov L, Kushnir D, Goldsmith R, Dichtiar R, Zusman S. Dental status, visits, and functional ability and dietary intake of elderly in Israel. Israel J Health Policy Res. 2018;7(1):1–5.
Marshall TA, Warren JJ, Hand JS, Xie X-J, Stumbo PJ. Oral health, nutrient intake and dietary quality in the very old. J Am Dent Assoc. 2002;133(10):1369–79.
Yamamoto T, Aida J, Kondo K, Fuchida S, Tani Y, Saito M, et al. Oral health and incident depressive symptoms: JAGES project longitudinal study in older Japanese. J Am Geriatr Soc. 2017;65(5):1079–84.
Huang DL, Chan KCG, Young BA. Poor oral health and quality of life in older US adults with diabetes mellitus. J Am Geriatr Soc. 2013;61(10):1782–8.
Hugo FN, Hilgert JB, De Sousa MDLR, Da Silva DD, Pucca GA Jr. Correlates of partial tooth loss and edentulism in the Brazilian elderly. Community Dent Oral Epidemiol. 2007;35(3):224–32.
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–60.
World Health Organization. Global strategy on tackling oral diseases 2021. Available from: https://www.who.int/teams/noncommunicable-diseases/governance/gaporalhealth.
Acknowledgements
We thank Dr. Elisa Ghezzi, University of Michigan and Dr. Paul Fontelo, National Library of Medicine, National Institutes of Health, for their support reviewing the protocol and early drafts of this manuscript.
Funding
This research was supported by the National Institutes of Health (NIH), National Institute of Dental and Craniofacial Research, and National Library of Medicine (NLM). Some authors were paid a salary by the NIH.
Author information
Authors and Affiliations
Contributions
AAA, SB and BAD conceived and designed the study. AAL created the search strategy, performed database searches, and retrieved articles. AAA and SDL reviewed all studies, extracted, and interpreted the data. SB and DW served as tiebreakers. TJI helped assess methodological quality and risk of bias. AAA drafted the manuscript, which was critically revised for important intellectual content by AAL, SDL, SB, DW and BAD. All authors read and approved the final article and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Tables 1-3 (Outcomes by Tooth Retention Concept, Risk of Bias and Quality/Strength of Cumulative Evidence).
Additional file 2:
Supplementary Information. Search Strategy for Seven Databases.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Atanda, A.J., Livinski, A.A., London, S.D. et al. Tooth retention, health, and quality of life in older adults: a scoping review. BMC Oral Health 22, 185 (2022). https://doi.org/10.1186/s12903-022-02210-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02210-5